Abstract
Limb sparing surgery for tumors of the acetabulum is notoriously difficult. The tumor defect is often extensive, and restoration of a functional and painless hip joint after an Enneking type 2 or type 2–3 pelvic resection is difficult due to the complex anatomy and biomechanics. Stemmed acetabular cups offer a reconstructive option for the majority of these resections. Various stemmed cups have been introduced, and modular designs have gained popularity during recent years because of their versatility and because they allow for relatively easy and quick reconstruction. In this chapter, we present a case of a patient with a primary tumor of the acetabulum who was treated with computer-assisted en bloc tumor resection and direct reconstruction with a modular stemmed acetabular cup.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pelvic resection
- Acetabular reconstruction
- LUMiC
- Stemmed acetabular cup
- Computer-assisted surgery
- Navigated resection
1 Brief Clinical History
A 57-year-old patient, with no relevant medical history, presented with progressive weakness and pain of the right hip. On imaging, a primary bone malignancy was suspected. Biopsy confirmed an osteosarcoma of the right acetabulum. Following neo-adjuvant chemotherapy, she was scheduled for an Enneking type 2–3 internal hemipelvectomy.
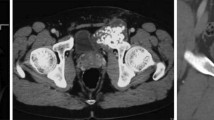
2 Preoperative Imaging
Preoperative imaging and planning are not only used to assess the tumor extension in bone, the hip joint, and surrounding soft tissues (muscles and neurovascular structures) but should also be part of the preoperative surgical planning and optimal margin assessment to increase the possibility of performing a R0 resection leaving as optimal reconstruction options in place. See Fig. 10.1.
Preoperative radiograph showing a large lesion of the right acetabulum with cortical destruction, expanding into the right iliac wing and superior pubic ramus. There is a soft tissue mass on both sides of the iliac wing, growing into the gluteus minimus and the iliacus muscle. Moreover, the direct and indirect head of the rectus femoris muscle are involved
3 Problem List
-
(a)
There is a large tumor of the periacetabular bone with a significant soft-tissue mass. The tumor needs to be resected with clear margins, while preferably sparing the femoral vessels and both the femoral and sciatic nerve, to maintain a functional limb.
-
(b)
After tumor resection, there is a considerable bony defect that needs to be reconstructed. Resection of hip musculature impairs stability of the neo-joint, and these reconstructions therefore carry a substantial risk of instability and prosthetic dislocation. Additionally, resection leads to significant bone loss and therefore, there is limited bone stock for prosthetic fixation.
-
(c)
The extent of surgery, complex three-dimensional anatomy, and substantial soft tissue resection together result in lengthy surgical procedures with significant blood loss and a large dead space. These factors all contribute to the high risk of infection.
4 Treatment Strategy
-
(a)
A pre-planned and computer navigated en bloc tumor resection of the periacetabulum and superior pubic ramus (Enneking type 2–3) is performed. As far as possible, vital neurovascular structures are carefully preserved to maintain a functional limb. Obturator nerve resection, and, therefore, adductor functional loss, is commonly unavoidable because of the resection of the obturator canal and both pubic rami.
-
(b)
Reconstruction of a functional hip joint with appropriate soft tissue coverage and restoration of the anatomical center of rotation using a modular stemmed acetabular cup and a conventional femoral component.
-
(c)
In this case an “extra articular” resection (acetabulum + proximal femur) is performed because reconstruction of the proximal femur is also required. It is not mandated for oncologic reasons, but may prove very helpful in performing the osteotomy of the
sciatic orinferior ramus using the space of the osteotomy through the femoral neck.
5 Basic Principles
-
(a)
Computed tomography (CT) and magnetic resonance (MR) images are used to assess the extent of osseous and extra-osseous tumor involvement, and to determine the level of the three osteotomies (supra-acetabular, superior pubic ramus, and infra-acetabular).
-
(b)
The patient is positioned in the lateral decubitus position, which allows the patient to be rotated to nearly prone and supine positions.
-
(c)
A single-incision approach is utilized, running from posteriorly to anteriorly across the iliac crest and then distally along the lateral border of the rectus femoris. To prevent wound healing complications, medial extension of the approach should be avoided. When needed, the approach can be extended subcutaneously toward the pubic symphysis, via the anterior distal extension.
-
(d)
Dissection follows the iliac wing, releasing the gluteus maximus and, if possible, the gluteus medius on the lateral side, toward the greater gluteal vascularization in the sciatic notch. The sartorius and rectus femoris muscles anteriorly are commonly released, and the psoas muscle medially with femoral nerve is kept intact. The iliac wing is used to place the navigation tree fixed to two 2.5 mm pins. An envelope of muscles is left to cover the tumor, often resulting in resection of the iliacus muscle, while the femoral nerve can be spared. The rectus femoris muscle is cut distally from the tumor, as was determined on preoperative MR imaging. The superior gluteal, iliac, femoral, and obturator vessels are spared when the inferior ramus is left in situ.
-
(e)
The tumor grows within the subchondral bone of the acetabulum on preoperative imaging, but the joint itself appeared unaffected. The hip capsule is dissected from its surrounding tissues and released from the femoral neck. An osteotomy is made through the femoral neck using an oscillating saw, and this provides space for the navigated osteotomy of the inferior pubic ramus.
-
(f)
The three osteotomies are performed using a navigated chisel. The specimen is released from the remaining musculature using LigaSure Precise™ (Covidien, Dublin, Ireland) to prevent blood loss. Next, the specimen is removed from the patient.
-
(g)
First, the femoral component is inserted. In this case, the proximal femur was unaffected and therefore, a femoral component designed for conventional hip replacement can be used. If part of the proximal femur has to be resected, a modular proximal femoral endoprosthesis is used to restore sufficient femoral length.
-
(h)
Next, a guidewire for the iliac stem is inserted in the direction of the posterior superior iliac spine with use of computer-assisted navigation. Alternatively, the guidewire can be inserted under image intensifier control, or with use of patient-specific jigs. Following insertion of the guidewire, the ilium is prepared over the guidewire.
-
(i)
Subsequently, the trial iliac stem is inserted. The length of the iliac stem is dictated by the supra-acetabular resection height. The iliac stem has two fin slots, which are used to prepare the fins for the definitive stem using a fin chisel.
-
(j)
A trial cup is connected to the trial stem and a trial reconstruction is performed to assess implant size, reconstruction length and offset, soft tissue tension, and acetabular cup anteversion, which can be adjusted in five-degree increments. This may aid to reduce the risk of postoperative instability.
-
(k)
The definitive iliac stem is inserted. Be cautious not to fracture the anterior or posterior wall of the iliac wing, as this impairs initial stem fixation. When the stem is inserted to the appropriate depth, the acetabular cup is connected to the iliac stem.
-
(l)
Stability of the reconstruction is again assessed. Optionally, an attachment tube may be used to reinforce the neo-joint and to re-attach soft tissues. This is done to obtain optimal coverage of implants, and it is thought to reduce the risk of prosthetic dislocation.
-
(m)
The wound is thoroughly irrigated. Gentamycin-containing resorbable sponges are optionally used as a local antibiotic treatment. The wound is closed in layers. If sufficient soft tissue coverage is lacking, the vastus lateralis muscle can be released distally and used to obtain proximal coverage of the prosthesis.
-
(n)
Starting on the third postoperative day, partial weight-bearing with two crutches is allowed until 6 weeks postoperatively. Then, patients are allowed to mobilize with one crutch.
7 Technical Pearls
-
(a)
Three-dimensional planning software may be used to fuse the CT and MR images. An intraoperative CT scan is obtained to allow for navigated bone resection using a computer-assisted surgery (CAS) system with a navigated chisel. This has been shown to reduce the risk of contaminated margins. Also, in experienced hands, CAS reduces operative time [1].
-
(b)
With three-dimensional planning software and digital templating, the position and size of the iliac stem may be determined preoperatively. Based on this, the trajectory for the guidewire can be determined and inserted in the CAS system. This allows for quick and reliable implant positioning, which is essential during these lengthy surgical procedures.
-
(c)
The stemmed acetabular cup (LUMiC, implantcast GmbH, Buxtehude, Germany) is designed to seat in the medial ilium, along the natural weight-bearing axis, where dense bone is encountered. It is essential that the iliac stem is inserted to the right depth, in order to obtain adequate primary fixation and to allow for bony on growth on the uncemented hydroxyapatite-coated stem. This enables long-term stable fixation of the iliac stem [2]. Stem depth is therefore more important than restoration of the initial center of rotation. Also, the largest possible stem should be inserted to ensure maximum tight fitting.
-
(d)
The attachment tube should not be fixed to the iliac stem or acetabular cup but rather, a trans-osseous fixation to the remaining ilium should be performed, using non-absorbable sutures, to further reinforce the reconstruction.
8 Outcome Photos and Imaging
See Fig. 10.6.
9 Avoiding and Managing Complications
-
(a)
The use of a dual-mobility cup with the largest possible diameter is advised, as this is shown to reduce the risk of dislocation [2].
-
(b)
Avoid the use of star-shaped incisions, even in Enneking type 2–3 resections, as these incisions are associated with a higher risk of wound healing complications.
-
(c)
The use of silver coating may aid to reduce the risk of deep infection, or at least improve the chance of successful debridement in case the implant gets infected [3].
-
(d)
Infections of pelvic endoprostheses are often polymicrobial and caused by gram-negative micro-organisms. The prophylactic antibiotic regimen should be aimed at these micro-organisms [4]. Also, poor penetration of systemic antibiotics in the dead space and the significant morbidity associated with deep infection presumably justify the use of local antibiotics.
References
Laitinen MK, Parry MC, Albergo JI, Grimer RJ, Jeys LM. Is computer navigation when used in the surgery of iliosacral pelvic bone tumours safer for the patient? Bone Joint J. 2017;99-B(2):261–6.
Bus MP, Szafranski A, Sellevold S, Goryn T, Jutte PC, Bramer JA, et al. LUMiC® endoprosthetic reconstruction after periacetabular tumor resection: short-term results. Clin Orthop Relat Res. 2017;475(3):686–95.
Wafa H, Grimer RJ, Reddy K, Jeys L, Abudu A, Carter SR, et al. Retrospective evaluation of the incidence of early periprosthetic infection with silver-treated endoprostheses in high-risk patients: case-control study. Bone Joint J. 2015;97-B(2):252–7.
Sanders PTJ, Bus MPA, Scheper H, van der Wal RJP, van de Sande MAJ, Bramer JAM, et al. Multiflora and gram-negative microorganisms predominate in infections affecting pelvic endoprostheses following tumor resection. J Bone Joint Surg Am Vol. 2019;101(9):797–803.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bus, M.P.A., van de Sande, M.A.J. (2022). Implant Reconstruction of the Pelvis: II: Modular Pedestal Cup Prosthesis. In: Özger, H., Sim, F.H., Puri, A., Eralp, L. (eds) Orthopedic Surgical Oncology For Bone Tumors . Springer, Cham. https://doi.org/10.1007/978-3-030-73327-8_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-73327-8_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73326-1
Online ISBN: 978-3-030-73327-8
eBook Packages: MedicineMedicine (R0)