Abstract
Urothelial cancer (UC) is a molecularly and clinicopathologically heterogeneous disease. Recent advances in the genetic studies of UC have expanded our knowledge of the disease from a poorly understood aggregate of pathologies to more specific and molecularly characterized subtypes. This may effectively enable the implementation of personalized therapies and better patient management. The current section summarizes the contemporary understanding of the molecular pathology of bladder cancer, including its molecular pathways and biomarkers.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Urinary bladder
- Urothelial carcinoma
- Molecular pathology
- Pathogenesis
- Pathways
- Mutation
- Epigenetic
- Micro-RNA
- Biomarker
- Progression
- Targeted therapy
- CDKN2A
- TP53
- RB1
- TP53
- MDM2
- FGFR3
- RAS
- TERT
- PTEN
- PIK3/AKT/MTOR
Mutational Frame
Development and progression of bladder UC occur mainly through genomic modifications affecting almost all chromosomes. All types of genetic changes that include aneusomies, epigenetic alterations, activating or silencing mutations, amplifications, and deletions are commonly seen in this disease [1, 2].
Numerical Chromosomal Alterations
The most frequently detected copy number aberrations in UC are on chromosomes 1, 8, 9, 10, 11, 13, and 14 [3]. These changes offer the necessary setting of genetic instability that in turn allows for the accumulation of succeeding genetic defects. Although most non-muscle invasive bladder cancer (NMIBC) are diploid or near diploid, loss of specific regions is common and associated with higher recurrence [4,5,6]. A study comparing genetic deviations between Ta and T1 tumors has found that losses of 9q (54%), 9p (39%), and Y (28%) and gain of 1q (14%) were more prevalent in Ta tumors, whereas deletions at 2q (36%), 8p (32%), and 11p (21%) and gains at 1q (54%), 8q (32%), 3p, 3q, 5p, 6p, and 10p (18% each) were more common in T1 neoplasia [6]. Notably, loss of 9q has also been shown in normal surface epithelium adjacent to tumor. Loss of 9q appears to be an early marker of local genomic instability and may act in the initiation of bladder cancer [5, 7]. NOTCH1 and TSC1 are the candidate tumor suppressor genes on chromosome 9q that may factor in the cancer pathogenesis. Gains of chromosomes 3q, 7p, and 17q and 9p21 deletions (p16 locus) are of special note which give them potential diagnostic and prognostic significance [8] (see Urovysion below).
Mutations
Mutations in bladder cancer (BC) mainly involve the genes responsible for neoplastic transformation, signal transduction, cell cycle regulation, DNA damage repair, transcription, and chromatin remodeling. Overall mutation rates in muscle invasive bladder carcinoma (MIBC) are very high (mean 8.2 and median 5.8 per megabase in coding regions according to The Cancer Genome Atlas (TCGA) data, only slightly fewer than lung cancer and melanoma [9, 10]). Recurrent genetic alterations include mutations in the coding region of many genes such as FGFR3, PIK3CA, KDM6A, STAG2, and TP53 [10, 11] as well as in numerous non-coding regions such as TERT, PLEKHS1, WDR74, TBC1D1, LEPROTL1, and GPR126 [12, 13].
High mutation load in invasive UC is mainly thought to be driven by the APOBEC (apolipoprotein B mRNA editing enzyme catalytic polypeptide-like) mutagenesis. APOBEC is a member of the evolutionary conserved family of cytidine deaminases that are involved in the intrinsic response to infection, modification, and clearance of viral DNA. TCGA Bladder Cancer Group has shown that the somatic mutations in UC are dominated by a C:G → T:A [9]. This is characteristic of mutations caused by the APOBEC family [14]. APOBEC-a and APOBEC-b mutation signatures account for 67% of all single nucleotide variants (SNVs) within MIBC. A second frequent mutational signature is associated with ERCC2 mutations and thought to be responsible for ~20% of all SNVs. ERCC2 encodes a DNA helicase that has a central role in the nucleotide excision DNA repair pathway. A third signature in the TCGA analysis is likely related to 5-methylcytosine deamination and has been associated with 8% of SNVs.
The most frequently mutated gene in the bladder cancer is the TERT (telomerase reverse transcriptase) promoter [13, 15, 16]. TERT encodes the catalytic subunit of the telomerase complex which is upregulated in the majority of cancers and is essential for vanquishing senescence and apoptosis by maintaining the 3′ telomere length at the ends of chromosomes [17]. Somatic TERT promoter mutations occur early in the process of bladder carcinogenesis [16, 18, 19]. Mutations generate consensus binding motifs for ETS transcription factors, increasing TERT expression and activity. Given that telomere shortening acts as a mitotic clock, the activation of telomerase elongates telomeres at the ends of chromosomes, which is essential for the continued growth of cancer cells [20].
Activating mutations of FGFR3 , a gene located at chromosome 4p16.3, are common in bladder UC, particularly in the subset of low-grade and low-stage tumors, where their frequency reaches up to 70–80% [18]. They map to three mutation hotspots in exons 7 (codons 248 and 249), 10 (codons 372, 373, 375, 382, and 393), and 15 (codon 653) [21].
One of the most frequently mutated gene is TP53 in muscle-invasive UCs and has been detected in nearly 50% of the cases [9]. Mouse double minute 2 homolog (MDM2) is another gene functioning in cell cycle regulation. MDM2 amplification and overexpression are seen in 7% of UCs and mutually exclusive with TP53 mutation. RB1 mutation is a frequent accompaniment of TP53 mutation, is observed in 17% of cases, and is mutually exclusive with CDKN2A deletion.
Mixed-lineage leukemia 2 (MLL2) gene belongs to the group of chromatin remodeling genes involved in epigenetic regulation. It is another frequently mutated gene and found in around 28% of UCs. Other frequently mutated genes include lysine (K)-specific methyltransferase 2C (KMT2C) , ataxia telangiectasia mutation (ATM) , FAT atypical cadherin 1 (FAT1) , CREB-binding protein (CREBBP) , ERBB2, spectrin alpha non-erythrocytic 1 (SPTAN1) , and lysine (K)-specific methyltransferase 2A (KMT2A).
The recurrent gene fusions are rarely observed in UC [10]. Less than 5% of bladder cancers harbor FGFR3-TACC3 (transforming acidic coiled-coil containing protein 3) fusions and even less frequently TSEN2 (tRNA splicing endonuclease subunit 2) -PPARG (peroxisome proliferator-activated receptor gamma) and MKRN2 (makorin ring finger protein 2) -PPARG translocations [22].
Epigenetic Alterations
Aberrant DNA methylation and histone modification play a role in regulating gene expression and may contribute to carcinogenesis. Several groups have documented that hypermethylation of RARB, RASSF1, and DAPK is linked to aggressiveness in UC [23].
Chromatin-modifying genes (CMGs) are the regulators of gene expression and commonly mutated in the malignancies [10, 24]. It was found that the two most commonly mutated CMGs in NMIBC were KDM6A (38%) and ARID1A (28%) [25]. KDM6A mutation frequency is 52% in low grade (LG) Ta, 38% in high grade (HG) Ta, 32% in HGT1, and 24% in MIBC, whereas ARID1A mutation frequency is 9% in LGTa, 28% in HGTa, 18% in HGT1, and 24% in MIBC cases. Frequency of KDM6A mutations was found elevated in the female patients with Ta tumors (72%) compared to men (42%). ARID1A has been associated with increased risk of recurrence, which may be linked to increased aggressiveness or BCG resistance [25].
Molecular Pathways
Bladder UC is believed to develop via a field effect that involves multiple sites in the mucosa, leading to multifocal and metachronous tumorigenesis [18, 26]. Urothelial cells in the affected field gain additional genetic alterations and become malignant by clonal evolution.
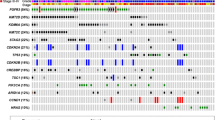
UC develops along two oncogenic tracks: papillary (~80% of bladder cancers) and nonpapillary (~20% of bladder cancers), with some overlapping molecular profile (Fig. 14.1). Low-grade (LG) papillary tumors are superficial, and they arise from premalignant lesions referred to as urothelial dysplasia (low-grade intraurothelial neoplasia), whereas nonpapillary lesions are generally high grade (HG) and develop from urothelial dysplasia that progresses to carcinoma in situ (high-grade intraurothelial neoplasia). Low-grade papillary UCs have high propensity for recurrence after transurethral resections, but they usually do not penetrate the basement membrane of surface epithelium to invade the bladder wall. On the other hand, urothelial CIS is notorious for frequent transformation to invasive and metastatic cancer. It is also known that some of the low-grade papillary tumors (~10 to 15%) may progress to the noninvasive high-grade papillary UC and subsequently invasive UC. The MIBC cohort in The Cancer Genome Atlas (TCGA) study has demonstrated the mutual exclusiveness of alterations between CDKN2A and TP53, CDKN2A and RB1 , TP53 and MDM2 , and FGFR3 and RB1 gene pairs. Similar analyses showed the co-occurrence of mutations in the TP53 and RB1 genes and in the FGFR3 and CDKN2A genes [10]. It has now been widely accepted that the Ras pathway is a major driver of the papillary track, whereas the p53/RB1 and PTEN-related pathways contribute to the aggressive and invasive phenotype [2, 18, 27, 28]. Most CIS lesions gain TP53 mutations early in evolution and do not acquire FGFR3 mutations [29]. On the other hand, some low-grade papillary tumors with FGFR3 mutation may acquire additional mutations of the TP53 gene and chromosomal losses of 9p21 (the locus that includes CDKN2A ) and may progress to high-grade and invasive carcinoma [29,30,31].
Low-Grade Tumors
FGFR3/RAS Pathway: The FGFR3/RAS pathway is active mainly in low-grade noninvasive papillary UC. FGFR3 signals through Ras (RAS-MAPK-ERK pathway) and regulates cell cycle entry and proliferation. The most common FGFR3 mutations facilitate ligand-independent receptor dimerization, leading to transphosphorylation and downstream signaling. Activating point mutation in FGFR3 is most common in Ta tumors (~80%), with decreased frequency in high-grade Ta (59%), T1 (10–34%), and MIBC (10–20%) [25, 32, 33]. FGFR3 mutations have been associated with a higher risk of recurrence in noninvasive papillary bladder cancer and favorable clinical outcomes in pT1 tumors [18, 27, 34, 35]. Approximately 10% of low-grade bladder carcinomas harbor mutations in RAS genes (HRAS, KRAS, or NRAS) [36] which do not co-occur with FGFR3 mutations [37]. FGFR3 fusion proteins are also implicated in bladder cancer pathogenesis, with in-frame FGFR3-TACC3 fusions being the most common [10]. TACC3 is upstream of FGFR3 signaling, and fusion protein causes constitutive activation of the MAPK-ERK pathway [38]. FGFR3-TACC3 fusions appear more commonly associated with MIBC.
High-Grade Tumors
TP53/RB1 Pathway: The TP53/RB1 pathway is an important regulator of cell cycle progression and plays an important role in the development of aggressive UCs [18, 39]. The mutation or deletion of TP53 has been observed predominantly in CIS and MIBC. According to TCGA cohort data [10], 89% of MIBCs have an inactivated TP53 cell cycle pathway, with TP53 mutations in 48%, MDM2 amplification in 6%, and MDM2 overexpression in 19% of cases. Seventeen percent of MIBCs harbor RB1 mutations often with concurrent TP53 mutations [40]. CDKN2A (p16), which functions as a negative regulator of the RB1 pathway, is found to be mutated (7%) or deleted (22%).
Evidence suggests LG noninvasive papillary UC, which classically has a high frequency of FGFR3 mutation, progresses to high-grade and invasive carcinoma through mutations in TP53 and chromosomal losses of 9p21, the locus that includes CDKN2A [30, 31]. In contrast, most CIS lesions develop TP53 mutations early and do not acquire FGFR3 mutations [29].
PIK3/AKT/MTOR Pathway: In vitro studies show that the ablation of p53 in a background of mutant Ras induces superficial papillary tumors but is insufficient to trigger cancer invasion, suggesting that additional complex genetic events are needed to induce a thoroughly aggressive and invasive phenotype [41]. Up to 40% of bladder UCs show the activation of the phosphoinositide 3-kinase/protein kinase B (or AKT)/mechanistic target of rapamycin (PI3K/AKT/mTOR) pathway. The PIK3/AKT/MTOR pathway regulates important steps in tumorigenesis and tumor progression. This pathway is activated by receptor tyrosine kinases including ERBB2, ERBB3, and FGFR3. The upstream pathway activator ERBB2 encodes human epidermal growth factor receptor 2 (Her2), which is mitogenic for cell growth. It is amplified, mutated, or overexpressed in 12% of MIBCs or a subset of high-grade NMIBC cases [9, 25, 28]. When present in NMIBC, ERBB2 amplification is associated with high risk of progression and concomitant CIS [42,43,44]. ERBB2 mutations are commonly found in the extracellular domain and are likely reflect APOBEC mutational signature [10]. PIK3CA (cancer-associated phosphatidylinositol 3-kinase) encodes the catalytic subunit of PI3K, and its mutations are seen more frequently in NMIBC than in MIBC (Ta, 40–50%; T1, 6–20%; MIBC, 22%) [10, 13, 45]. They are more commonly located in the helical domain than in the kinase domain, likely due to the mutagenic activity of APOBEC. PIK3CA mutations appear to be associated with a favorable outcome in patients who undergo radical cystectomy [46]. The reduced expression of phosphatase and tensin homolog (PTEN) is a negative regulator of the PIK3/AKT/MTOR pathway. Inactivating deletions or mutations of the PTEN gene has been observed in many MIBC cases. Loss of PTEN was significantly associated with non-papillary, high-grade and invasive tumors, supporting that the involvement of the PI3K/AKT/mTOR pathway might be a potential driver of an invasive phenotype. AKT1 and TSC1 are other tumor suppressor genes and negative regulators of this pathway. However, they are not as frequently mutated [18].
Urothelial Proliferation of Unknown Malignant Potential (Urothelial Hyperplasia) and Dysplasia
The deletion of chromosome 9 is prevalent in urothelial hyperplasia and dysplasia [40, 47, 48], suggesting that this deletion occurs in the early stage of bladder cancer. In one study, chromosome 9 deletions were detected in 37% of cases of flat urothelial hyperplasia with or without associated papillary lesions, in addition to chromosome 8 deletions in 10% and FGFR3 mutations in 23% of the cases [49]. The FGFR3/HRAS mutations are frequently found during the development of urothelial hyperplasia [2, 27, 28, 50, 51]. FGFR3/RAS pathway enables tumors to progress from urothelial hyperplasia to noninvasive papillary tumors with high recurrence rates. Expression of ectopic mutant FGFR3 in normal urothelial cells has been shown to induce aberrant activation of the MAPK and PLCg1 signaling pathways and increase cell proliferation [21]. In animal models the activating mutations of the Ras gene caused the development of urothelial dysplasia and low-grade superficial papillary UC [50, 52]. The dose of activated Ras was related to phenotypic change. A low copy number of mutant Ras induced urothelial dysplasia, whereas a high copy number led to the development of low-grade superficial papillary tumors.
Tumor Progression
Approximately, 15–20% of patients with NMIBC progress to muscle invasive disease [53] which is referred to as secondary MIBC. Two of the candidate genes proposed in tumor progression are E2F1 and CDKN2A. E2F1 is a regulator of cellular apoptosis that has been linked to tumor invasion and metastasis in various cancer types [53, 54]. Upregulation of E2F1 and its downstream targets, EZH2 and SUZ12, have been shown in patients with NMIBC progressing to muscle-invasive disease [55]. CDK2NA is a cell cycle regulator involved in G1-S arrest. CDKN2A is lost in the invasive portion of NMIBCs, and only tumors with progression lose both TP53 and CDK2NA [56].
Urothelial Papilloma (UP)
Results of molecular studies in UPs are variable. Rates of reported TERT promoter mutations vary from 46% to 0% [57, 58]. Similarly range of FGFR3 mutations varies from 75% [59] to 0% [58]. In a recent study, 10 of 11 UPs had oncogenic mutations in the RAS/ERK signaling pathway (seven KRAS, one HRAS, one KRAS plus HRAS and one BRAF mutations) [58]. Only one case harbored oncogenic FGFR3 or TERT promoter mutations. This lesion was likely a recurrent carcinoma despite papilloma histology as the tumor also had oncogenic PIK3CA, KMT2D, and CDKN1A mutations and arose in a patient who had history of several low-grade noninvasive papillary urothelial carcinomas, prior and subsequent to UP.
Inverted Urothelial Papilloma (IUP)
There is variability in the reported results of molecular studies in inverted papillomas. Some groups report FGFR3 mutations in 9.8–45% (a mean of 18%) of inverted papillomas [60, 61], but others have found no change in FGFR3 gene [62]. Similarly, some tumors have been reported to harbor 9p deletions (in 3.9% of cases), 9q deletions (in 13.2%), and 17p deletions (in 51%) [60]. The most common molecular alterations in IUP appear in the MAP kinase/ERK pathway, HRAS and KRAS mutations being predominant. Recurrent HRAS mutations (Q61R) have been reported in 60% to over 90% of cases [57, 62].
TERT promoter mutations are rare in inverted urothelial papilloma, with most studies showing inverted papillomas lack these mutations [57, 60,61,62,63]. This information and the benign behavior and frequent mutations in the MAP kinase/ERK pathway in these lesions have been taken as evidence that IUPs are a distinct type of indolent low-grade urothelial neoplasia that does not progress to carcinoma [64].
Urothelial Carcinoma with Variant Histology
Urothelial Carcinoma with Divergent Differentiation
The literature on the molecular characteristics of divergent (glandular and/or squamous) differentiation in UC is scant, but it is very likely that there is overlap with those of UC, particularly in the presence of high rates of TERT promoter mutations [65, 66].
Plasmacytoid Urothelial Carcinoma (PUC)
PUCs are characterized by loss of E-cadherin expression similar to lobular or diffuse carcinomas of the breast and stomach. Somatic CDH1 truncating mutations are mostly responsible from E-cadherin loss as they have been identified in 84% of PUC; CDH1 promoter hypermethylation occurs less frequently [67]. Aside from CDH1 alterations, the genomic landscape of PUC is generally similar to that of coexistent conventional UC, suggesting that both histologic subtypes potentially evolve from a common cell of origin [67, 68]. No germline CDH1 mutations have been reported in PUC.
Micropapillary Urothelial Carcinoma (MPUC)
Genomic expression profile of micropapillary cancer reveals that more than 6000 genes are aberrantly expressed when compared to conventional UC [69]. The micropapillary expression signature is also present in conventional UC component accompanying MPUC, suggesting that micropapillary variant arises from a unique subset of conventional UCs.
Consistently higher rates of ERBB2 amplification have been reported in MPUC than in conventional UC [70]. ERBB2 amplification is associated with a worse outcome following radical cystectomy in some series [71]. A study has shown that ERBB2 amplification is more commonly identified in the micropapillary variant than conventional UC when both components are present [72] although the rate of ERBB2 amplification in the conventional urothelial component in these mixed (micropapillary + conventional urothelial) tumors is much higher than the reported rates in UC not containing micropapillary component [10, 73, 74].
It has been reported that in MPUC there is common downregulation of miR-296 and activation of chromatin-remodeling complex RUVBL1, with overexpression of its downstream target genes such as lysine-specific demethylase 4B (KDM4B), insulin-like growth factor-binding protein 3 (IGFBP3) , and disintegrin and metalloproteinase domain-containing protein 15 (ADAM15) [75, 76]. These are known to be involved in cell growth, DNA damage repair, and metastasis.
Sarcomatoid Urothelial Carcinoma
The sarcomatous and urothelial components within the same tumor share common clonal origin. More recently, it has been shown that sarcomatoid UC is enriched with mutations in TP53, RB1 , and PIK3CA and is associated with overexpression of epithelial-mesenchymal transition markers [77,78,79,80].
Nested Variant of Urothelial Carcinoma
Up to now, only a few molecular findings have been reported related to this tumor type, the most common being the high rate of TERT promoter mutations as well as occasional mutations in TP53, JAK3, and CTNNB1. These findings suggest that this UC subtype harbors molecular alterations similar to those of UC in general [81, 82]. Documentation of TERT promoter mutation can be beneficial in difficult cases such as small biopsies as it is not found in benign mimickers of nested UC.
Small Cell/Neuroendocrine Carcinoma of the Bladder (SmCC)
One of the most common findings in SmCC is the near ubiquitous presence of loss-of-function co-alterations of TP53 and RB1. One study reported mutations of TP53 and RB1 in 90% and 87% of cases, respectively (80% of tumors displaying co-alterations of both) [83]. Even in tumors with no loss-of-function mutations in RB1 gene, RB protein expression was lost immunohistochemically, suggesting an alternative mechanism for RB suppression, such as epigenetic silencing.
Small cell carcinoma has a high somatic mutational burden driven predominantly by an APOBEC-mediated mutational process [84]. Genes that are commonly mutated in UC are also found mutated in bladder SmCC, including TERT promoter mutations (95%) and truncating alterations in genes involved in chromatin modification such as CREBBP, EP300, ARID1A, and KMT2D in ~75% of cases [83, 84]. Unlike UC, there is near absence of KDM6A truncating mutations, CDKN2A deletion, and CCND1 amplifications in SmCC [83]. SmCC is associated with a high level of chromosomal instability, and whole genome duplication is seen in 72% of tumors. RNA sequencing reveals novel fusion transcripts, including an in-frame Pvt1 oncogene (PVT1)-ERBB2 fusion, which is associated with aberrant ERBB2 expression.
Studies investigating the clonal connection between the small cell and urothelial components within the same tumor have shown that there are shared changes between the two components as well as different alterations in each component. These findings further support the common clonal origin for SmCC and coexisting conventional UC [83].
Micro-RNA (miRNA)
Over 200 miRNAs or miRNA families/clusters are aberrantly expressed in UC [85]. The downregulated miRNAs may serve as tumor suppressors. miR-145 appears to be the most frequently downregulated miRNA in bladder cancer. The upregulated miRNAs may contribute to tumor progression. miR-21 has been shown to be upregulated in the tissues, plasma, and urinary exosomes of patients with bladder carcinoma, but its role in UC still needs further investigation. Circulating miRNAs in body fluids, especially in urine, constitute an important cancer signature and carry the potential to be the useful molecular markers for diagnosis, prognosis, classification, and recurrence of UC. miR-146a-5p is frequently overexpressed in the urine of UC patients, which indicates its potential as a novel biomarker for the rapid and early diagnosis.
Inheritance
Upper tract UC is a characteristic tumor of Lynch syndrome (an autosomal dominant disorder caused by a defect in a DNA mismatch repair (MMR) gene). Invasive upper tract UCs are MSI-high/MMR-deficient in ∼20% of cases [86]. Emerging evidence suggests an increased (but smaller) risk of urothelial neoplasia in the bladder as well [87]. The 10-year risk for urothelial cancer in patients already diagnosed with Lynch syndrome is 2%. The patients with Lynch syndrome seem to develop urothelial tumors mainly when MSH2 is affected by a germline mutation [88].
Bladder cancer has been reported in patients with hereditary retinoblastoma, possibly related to radiation and/or cyclophosphamide therapy. Bladder cancer can be a component of Costello syndrome. Patients with this syndrome have been reported to develop papillary UC during childhood [87].
Molecular Biomarkers for Tumor Detection and Surveillance
Analysis of desquamated urothelial cells in urine is a valuable source for noninvasive detection of bladder cancer. Urine cytology is an important tool in this respect for both diagnosis and follow-up of UC. However, its overall low sensitivity, especially in low-grade tumors, limits its utility. By the help of accumulating data about pathogenesis and molecular background of urothelial neoplasia, several urine-based noninvasive assays have now become available for early detection and surveillance of the disease with higher sensitivity and specificity.
- The Urovysion assay: This test is multitarget, multicolor fluorescence in situ hybridization (FISH) assay and explores four common chromosomal alterations (aneuploidy of chromosomes 3, 7, and 17 and losses in 9p21) in high-grade UC cells shed to the urine [89]. It was reported that almost all invasive tumors including pT1 as well as a large fraction of the noninvasive bladder tumors were identified by this assay. Most studies also claim that adding this test to standard urine cytology increases sensitivity for detecting recurrence [90].
- Mutation detection assays: Urine-based mutational tests performed on cellular DNA have higher sensitivity than urine cytology and can detect low-grade tumor, an advantage over FISH. They mainly evaluate the genes altered in bladder cancer, such as TERT promoter and FGFR3, with focus on mutational hotspots [91, 92]. The noninvasive test may be useful for monitoring patients and triage cystoscopy. A positive result may serve as a warning of future recurrence if the subsequent cystoscopy is unable to show a tumor. Mutations in the TERT promoter occur early and are very common in UC regardless of grade, stage, and morphologic variants including papillary urothelial neoplasm of low malignant potential [93, 94]. TERT promotor mutations do not occur in reactive urothelial proliferations. Thus, they also have great diagnostic utility in distinguishing UC from its benign mimics. FGFR3 mutations in the cell-free DNA obtained from blood were identified in 68% of patients with advanced or metastatic UC in one study [95].
- UroSEEK: This is a urine-based molecular assay recently developed for the detection and surveillance of urothelial neoplasms [96]. It is designed to detect alterations in 11 genes (TERT, FGFR3, PIK3CA, TP53, HRAS, KRAS, ERBB2, CDKN2A , MET, MLL, and VHL) commonly mutated in bladder cancer and copy number changes on 39 chromosome arms. Combined with cytology, the test detects 95% of bladder UC, 75% of upper tract UC, and 68% of recurrent bladder carcinoma. The advantage of the assay over cytology is more evident in low-grade tumors as UroSEEK detects 67% of these cases whereas cytology does none.
Molecular Markers for Treatment
The potential therapeutic molecular targets have been identified overall in 70% of the bladder cancers; however, none of them has been integrated into clinical practice, waiting for the results of ongoing studies and clinical trials.
FGFR Inhibitors: A very high proportion of bladder tumors are characterized by FGFR3 dysregulation. Activating point mutations of FGFR3 are found in up to 80% of low-grade and low-stage UC of the bladder. Upregulated expression of FGFR3 protein is also found in a significant number of tumors which lack point mutations and are predominantly muscle invasive [21]. Thus, FGFR3 may be an important therapeutic target in both noninvasive and invasive UC. Several studies have shown in preclinical models that silencing or inhibition of FGFR3 has a profound inhibitory effect on some UC cells leading to decreased proliferation, reduced anchorage-independent growth, and enhanced apoptosis [97,98,99]. Therefore, FGFR inhibitors have been proposed as novel therapeutic agents in the treatment of bladder tumors [100], and clinical trials of such agents have been initiated. In a phase II trial of erdafitinib (an FGFR inhibitor) for metastatic UC with FGFR3 alterations, the overall response rate was 40% [101]. The study of BGJ398 and erdafitinib showed significant clinical activity in patients with refractory metastatic cancers whose tumors contained activating FGFR3 mutations or fusions, which led to the recent US Food and Drug Administration (FDA) approval of erdafitinib. The US FDA also approved a companion diagnostic test for FGFR3 mutations and fusions. Given the high frequency of FGFR3 mutation in NMIBC, FGFR3 may be a rational target in NMIBC as well.
DNA Damage Response (DDR) Gene Alterations and Treatment: ERCC2 is among the DDR-related genes, and its alterations are detected in 10–15% of MIBCs. Mutations in ERCC2 and other genes involved in DNA damage response and repair have recently been shown to be associated with improved response not only to cisplatin-based chemotherapy but also to immune checkpoint blockade and radiation therapy for advanced UC [102,103,104]. Forty percent of responders to neoadjuvant chemotherapy (NAC) have been seen to have nonsynonymous ERCC2 gene alteration versus 7% in non-responders [105]. Other DDR genes such as ATM, RB1, and FANCC appear as potential biomarkers for response to NAC as well [106, 107].
Mammalian Target of Rapamycin (mTOR) Inhibitors: The potential therapeutic vulnerabilities also include the targets in the PI-3 kinase/AKT/mTOR and in the receptor tyrosine kinase (RTK)/mitogen-activated protein kinase (MAPK) pathways. Patients with mutations that activate mTOR pathway may benefit from mTOR inhibitors. TSC1 is the negative regulator of mTOR, and its loss may be associated with increased cell growth and survival in high-risk NMIBC [4]. mTOR inhibitors may be an effective therapy to prevent recurrence of tumors with TSC1 loss.
Other Potential Targets: Urothelial carcinoma with carcinogenesis by EGFR, ERBB2, ERBB3, PIK3CA, or RAS alterations may benefit from targeted therapy. Chromatin regulatory genes have been found more frequently mutated in UC than other common cancers, further supporting additional therapeutic options [10]. Long non-coding RNAs (lncRNAs) are long RNA transcripts greater than 200 nucleotides in length that do not code for any proteins. The lncRNA urothelial cancer-associated 1 (UCA1) has been associated with cisplatin chemotherapy resistance through activation of Wnt signaling [108].
Bacillus Calmette-Guérin (BCG) Responsiveness
Certain glutathione pathway genomic variations and immune system gene single nucleotide polymorphisms reveal potential to predict recurrence and progression-free survival after BCG therapy [109,110,111]. IL-8 (−251 T > A) polymorphism has been associated with an increased recurrence-free survival (RFS) in BCG-treated patients [112]. Gene polymorphisms in XPA, XPC, XPD, XPG, XPF, ERCC1, ERCC2, XRCC1, XRCC4, APEX1, GSTM1, CCNB1, PON1, and SLCO1B have been linked to reduced RFS or increased recurrence risk after BCG treatment. High tumor mutation burden and loss of CDK2NA may predict progression to MIBC in high-risk NMIBC treated with BCG [56]. ARID1A mutation has been associated with increasing stage and aggressiveness and may serve as a predictive biomarker of resistance in patients undergoing BCG therapy or a potential therapeutic target to enhance BCG response [25].
Conclusions
The discovery of the molecular changes and pathways involved in bladder cancer is fundamental to understand its biological heterogeneity. Analysis of specific alterations can be used to plan targeted therapies, and predict clinical outcomes and responsiveness to personalized therapies.
References
Sandberg AA. Cytogenetics and molecular genetics of bladder cancer: a personal view. Am J Med Genet. 2002;115(3):173–82. https://doi.org/10.1002/ajmg.10693.
Wu XR. Urothelial tumorigenesis: a tale of divergent pathways. Nat Rev Cancer. 2005;5(9):713–25. https://doi.org/10.1038/nrc1697.
Matsuyama H, Ikemoto K, Eguchi S, et al. Copy number aberrations using multicolour fluorescence in situ hybridization (FISH) for prognostication in non-muscle-invasive bladder cancer (NIMBC). BJU Int. 2014;113(4):662–7. https://doi.org/10.1111/bju.12232.
Hurst CD, Alder O, Platt FM, et al. Genomic subtypes of non-invasive bladder cancer with distinct metabolic profile and female gender bias in KDM6A mutation frequency. Cancer Cell. 2017;32(5):701–715.e7. https://doi.org/10.1016/j.ccell.2017.08.005.
Granberg-Ohman I, Tribukait B, Wijkström H. Cytogenetic analysis of 62 transitional cell bladder carcinomas. Cancer Genet Cytogenet. 1984;11(1):69–85. https://doi.org/10.1016/0165-4608(84)90100-6.
Richter J, Jiang F, Görög JP, et al. Marked genetic differences between stage pTa and stage pT1 papillary bladder cancer detected by comparative genomic hybridization. Cancer Res. 1997;57(14):2860–4.
Hurst CD, Knowles MA. Mutational landscape of non-muscle-invasive bladder cancer [published online ahead of print, 2018 Nov 13]. Urol Oncol. 2018;S1078-1439(18)30398-3.; https://doi.org/10.1016/j.urolonc.2018.10.015.
Kawauchi S, Sakai H, Ikemoto K, et al. 9p21 index as estimated by dual-color fluorescence in situ hybridization is useful to predict urothelial carcinoma recurrence in bladder washing cytology. Hum Pathol. 2009;40(12):1783–9. https://doi.org/10.1016/j.humpath.2009.06.011.
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature. 2014;507(7492):315–22. https://doi.org/10.1038/nature12965.
Robertson AG, Kim J, Al-Ahmadie H, et al. Comprehensive molecular characterization of muscle-invasive bladder cancer [published correction appears in Cell. 2018 Aug 9;174(4):1033]. Cell. 2017;171(3):540–556.e25. https://doi.org/10.1016/j.cell.2017.09.007.
Ward DG, Gordon NS, Boucher RH, et al. Targeted deep sequencing of urothelial bladder cancers and associated urinary DNA: a 23-gene panel with utility for non-invasive diagnosis and risk stratification. BJU Int. 2019;124(3):532–44. https://doi.org/10.1111/bju.14808.
Jeeta RR, Gordon N, Baxter L, Goel A, Noyvert B, Ott S, Boucher R, Humayun-Zakaria N, Arnold R, James N, Zeegers M, Cheng K, Bryan R, Ward D. Non-coding mutations in urothelial bladder cancer: biological and clinical relevance and potential utility as biomarkers. Bladder Cancer. 2019;5:263–72. https://doi.org/10.3233/BLC-190251.
Hurst CD, Knowles MA. Mutational landscape of non-muscle-invasive bladder cancer [published online ahead of print, 2018 Nov 13]. Urol Oncol. 2018;S1078-1439(18)30398-3; https://doi.org/10.1016/j.urolonc.2018.10.015.
Lawrence MS, Stojanov P, Polak P, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499(7457):214–8. https://doi.org/10.1038/nature12213.
Liu X, Wu G, Shan Y, Hartmann C, von Deimling A, Xing M. Highly prevalent TERT promoter mutations in bladder cancer and glioblastoma. Cell Cycle. 2013;12(10):1637–8. https://doi.org/10.4161/cc.24662.
Allory Y, Beukers W, Sagrera A, et al. Telomerase reverse transcriptase promoter mutations in bladder cancer: high frequency across stages, detection in urine, and lack of association with outcome. Eur Urol. 2014;65(2):360–6. https://doi.org/10.1016/j.eururo.2013.08.052.
Colebatch AJ, Dobrovic A, Cooper WA. TERT gene: its function and dysregulation in cancer. J Clin Pathol. 2019;72(4):281–4. https://doi.org/10.1136/jclinpath-2018-205653.
Moch H, Humphrey PA, Ulbright TM, Reuter VE. WHO classification of tumours of the urinary system and male genital organs. 4th ed. Lyon: IARC Press; 2016.
Wang CC, Huang CY, Jhuang YL, Chen CC, Jeng YM. Biological significance of TERT promoter mutation in papillary urothelial neoplasm of low malignant potential. Histopathology. 2018;72(5):795–803. https://doi.org/10.1111/his.13441.
Günes C, Rudolph KL. The role of telomeres in stem cells and cancer. Cell. 2013;152(3):390–3. https://doi.org/10.1016/j.cell.2013.01.010.
di Martino E, Tomlinson DC, Knowles MAA. Decade of FGF receptor research in bladder cancer: past, present, and future challenges. Adv Urol. 2012;2012:429213. https://doi.org/10.1155/2012/429213.
Guo CC, Czerniak B. Bladder cancer in the genomic era. Arch Pathol Lab Med. 2019;143(6):695–704. https://doi.org/10.5858/arpa.2018-0329-RA.
Netto GJ, Cheng L. Emerging critical role of molecular testing in diagnostic genitourinary pathology. Arch Pathol Lab Med. 2012;136(4):372–90. https://doi.org/10.5858/arpa.2011-0471-RA.
Guo G, Sun X, Chen C, et al. Whole-genome and whole-exome sequencing of bladder cancer identifies frequent alterations in genes involved in sister chromatid cohesion and segregation. Nat Genet. 2013;45(12):1459–63. https://doi.org/10.1038/ng.2798.
Pietzak EJ, Bagrodia A, Cha EK, et al. Next-generation sequencing of nonmuscle invasive bladder cancer reveals potential biomarkers and rational therapeutic targets. Eur Urol. 2017;72(6):952–9. https://doi.org/10.1016/j.eururo.2017.05.032.
Jones TD, Wang M, Eble JN, et al. Molecular evidence supporting field effect in urothelial carcinogenesis. Clin Cancer Res. 2005;11(18):6512–9. https://doi.org/10.1158/1078-0432.CCR-05-0891.
Knowles MA, Hurst CD. Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity. Nat Rev Cancer. 2015;15(1):25–41. https://doi.org/10.1038/nrc3817.
Sanli O, Dobruch J, Knowles MA, et al. Bladder cancer. Nat Rev Dis Primers. 2017;3:17022. Published 2017 Apr 13. https://doi.org/10.1038/nrdp.2017.22.
Amin MB, Eble JN. Urological pathology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014.
Rebouissou S, Hérault A, Letouzé E, et al. CDKN2A homozygous deletion is associated with muscle invasion in FGFR3-mutated urothelial bladder carcinoma. J Pathol. 2012;227(3):315–24. https://doi.org/10.1002/path.4017.
Downes MR, Weening B, van Rhijn BW, Have CL, Treurniet KM, van der Kwast TH. Analysis of papillary urothelial carcinomas of the bladder with grade heterogeneity: supportive evidence for an early role of CDKN2A deletions in the FGFR3 pathway. Histopathology. 2017;70(2):281–9. https://doi.org/10.1111/his.13063.
Billerey C, Chopin D, Aubriot-Lorton MH, et al. Frequent FGFR3 mutations in papillary non-invasive bladder (pTa) tumors. Am J Pathol. 2001;158(6):1955–9. https://doi.org/10.1016/S0002-9440(10)64665-2.
Kimura T, Suzuki H, Ohashi T, Asano K, Kiyota H, Eto Y. The incidence of thanatophoric dysplasia mutations in FGFR3 gene is higher in low-grade or superficial bladder carcinomas [published correction appears in Cancer 2002 Apr 1;94(7):2117]. Cancer. 2001;92(10):2555–61. https://doi.org/10.1002/1097-0142(20011115)92:10<2555::aid-cncr1607>3.0.co;2-m.
Hernández S, López-Knowles E, Lloreta J, et al. Prospective study of FGFR3 mutations as a prognostic factor in nonmuscle invasive urothelial bladder carcinomas. J Clin Oncol. 2006;24(22):3664–71. https://doi.org/10.1200/JCO.2005.05.1771.
van Rhijn BW, van der Kwast TH, Liu L, et al. The FGFR3 mutation is related to favorable pT1 bladder cancer. J Urol. 2012;187(1):310–4. https://doi.org/10.1016/j.juro.2011.09.008.
Kompier LC, Lurkin I, van der Aa MN, van Rhijn BW, van der Kwast TH, Zwarthoff EC. FGFR3, HRAS, KRAS, NRAS and PIK3CA mutations in bladder cancer and their potential as biomarkers for surveillance and therapy. PLoS One. 2010;5(11):e13821. Published 2010 Nov 3. https://doi.org/10.1371/journal.pone.0013821.
Jebar AH, Hurst CD, Tomlinson DC, Johnston C, Taylor CF, Knowles MA. FGFR3 and Ras gene mutations are mutually exclusive genetic events in urothelial cell carcinoma. Oncogene. 2005;24(33):5218–25. https://doi.org/10.1038/sj.onc.1208705.
Glaser AP, Fantini D, Shilatifard A, Schaeffer EM, Meeks JJ. The evolving genomic landscape of urothelial carcinoma [published online ahead of print, 2017 Feb 7]. Nat Rev Urol. 2017;14(4):215–29. https://doi.org/10.1038/nrurol.2017.11.
Hartmann A, Schlake G, Zaak D, et al. Occurrence of chromosome 9 and p53 alterations in multifocal dysplasia and carcinoma in situ of human urinary bladder. Cancer Res. 2002;62(3):809–18.
Kim J, Akbani R, Creighton CJ, et al. Invasive bladder cancer: genomic insights and therapeutic promise. Clin Cancer Res. 2015;21(20):4514–24. https://doi.org/10.1158/1078-0432.CCR-14-1215.
Hedegaard J, Lamy P, Nordentoft I, et al. Comprehensive transcriptional analysis of early-stage urothelial carcinoma. Cancer Cell. 2016;30(1):27–42. https://doi.org/10.1016/j.ccell.2016.05.004.
Kiss B, Wyatt AW, Douglas J, et al. Her2 alterations in muscle-invasive bladder cancer: Patient selection beyond protein expression for targeted therapy. Sci Rep. 2017;7:42713. Published 2017 Feb 16. https://doi.org/10.1038/srep42713.
Chen PC, Yu HJ, Chang YH, Pan CC. Her2 amplification distinguishes a subset of non-muscle-invasive bladder cancers with a high risk of progression. J Clin Pathol. 2013;66(2):113–9. https://doi.org/10.1136/jclinpath-2012-200944.
Breyer J, Otto W, Wirtz RM, et al. ERBB2 expression as potential risk-stratification for early cystectomy in patients with pT1 bladder cancer and concomitant carcinoma in situ. Urol Int. 2017;98(3):282–9. https://doi.org/10.1159/000453670.
López-Knowles E, Hernández S, Malats N, et al. PIK3CA mutations are an early genetic alteration associated with FGFR3 mutations in superficial papillary bladder tumors. Cancer Res. 2006;66(15):7401–4. https://doi.org/10.1158/0008-5472.CAN-06-1182.
Kim PH, Cha EK, Sfakianos JP, et al. Genomic predictors of survival in patients with high-grade urothelial carcinoma of the bladder. Eur Urol. 2015;67(2):198–201. https://doi.org/10.1016/j.eururo.2014.06.050.
Obermann EC, Junker K, Stoehr R, et al. Frequent genetic alterations in flat urothelial hyperplasias and concomitant papillary bladder cancer as detected by CGH, LOH, and FISH analyses. J Pathol. 2003;199(1):50–7. https://doi.org/10.1002/path.1259.
Chow NH, Cairns P, Eisenberger CF, et al. Papillary urothelial hyperplasia is a clonal precursor to papillary transitional cell bladder cancer. Int J Cancer. 2000;89(6):514–8.
Adar R, Monsonego-Ornan E, David P, Yayon A. Differential activation of cysteine-substitution mutants of fibroblast growth factor receptor 3 is determined by cysteine localization. J Bone Miner Res. 2002;17(5):860–8. https://doi.org/10.1359/jbmr.2002.17.5.860.
Mo L, Zheng X, Huang HY, et al. Hyperactivation of Ha-ras oncogene, but not Ink4a/Arf deficiency, triggers bladder tumorigenesis. J Clin Invest. 2007;117(2):314–25. https://doi.org/10.1172/JCI30062.
van Oers JM, Adam C, Denzinger S, et al. Chromosome 9 deletions are more frequent than FGFR3 mutations in flat urothelial hyperplasias of the bladder. Int J Cancer. 2006;119(5):1212–5. https://doi.org/10.1002/ijc.21958.
Zhang ZT, Pak J, Huang HY, et al. Role of Ha-ras activation in superficial papillary pathway of urothelial tumor formation. Oncogene. 2001;20(16):1973–80. https://doi.org/10.1038/sj.onc.1204315.
Chamie K, Litwin MS, Bassett JC, et al. Recurrence of high-risk bladder cancer: a population-based analysis. Cancer. 2013;119(17):3219–27. https://doi.org/10.1002/cncr.28147.
Pützer BM, Engelmann D. E2F1 apoptosis counterattacked: evil strikes back. Trends Mol Med. 2013;19(2):89–98. https://doi.org/10.1016/j.molmed.2012.10.009.
Lee SR, Roh YG, Kim SK, et al. Activation of EZH2 and SUZ12 regulated by E2F1 predicts the disease progression and aggressive characteristics of bladder cancer. Clin Cancer Res. 2015;21(23):5391–403. https://doi.org/10.1158/1078-0432.CCR-14-2680.
Meeks JJ, Carneiro BA, Pai SG, et al. Genomic characterization of high-risk non-muscle invasive bladder cancer. Oncotarget. 2016;7(46):75176–84. https://doi.org/10.18632/oncotarget.12661.
Isharwal S, Hu W, Sarungbam J, et al. Genomic landscape of inverted urothelial papilloma and urothelial papilloma of the bladder. J Pathol. 2019;248(3):260–5. https://doi.org/10.1002/path.5261.
Wang X, Lopez-Beltran A, Osunkoya AO, et al. TERT promoter mutation status in sarcomatoid urothelial carcinomas of the upper urinary tract. Future Oncol. 2017;13(8):705–14. https://doi.org/10.2217/fon-2016-0414.
van Rhijn BW, Montironi R, Zwarthoff EC, Jöbsis AC, van der Kwast TH. Frequent FGFR3 mutations in urothelial papilloma. J Pathol. 2002;198(2):245–51. https://doi.org/10.1002/path.1202.
Collomp K, Ahmaidi S, Audran M, Chanal JL, Préfaut C. Effects of caffeine ingestion on performance and anaerobic metabolism during the Wingate Test. Int J Sports Med. 1991;12(5):439–43. https://doi.org/10.1055/s-2007-1024710.
Lott S, Wang M, Zhang S, et al. FGFR3 and TP53 mutation analysis in inverted urothelial papilloma: incidence and etiological considerations. Mod Pathol. 2009;22(5):627–32. https://doi.org/10.1038/modpathol.2009.28.
McDaniel AS, Zhai Y, Cho KR, et al. HRAS mutations are frequent in inverted urothelial neoplasms. Hum Pathol. 2014;45(9):1957–65. https://doi.org/10.1016/j.humpath.2014.06.003.
Cheng L, Davidson DD, Wang M, et al. Telomerase reverse transcriptase (TERT) promoter mutation analysis of benign, malignant and reactive urothelial lesions reveals a subpopulation of inverted papilloma with immortalizing genetic change. Histopathology. 2016;69(1):107–13. https://doi.org/10.1111/his.12920.
Akgul M, MacLennan GT, Cheng L. Distinct mutational landscape of inverted urothelial papilloma. J Pathol. 2019;249(1):3–5. https://doi.org/10.1002/path.5307.
Brown NA, Lew M, Weigelin HC, et al. Comparative study of TERT promoter mutation status within spatially, temporally and morphologically distinct components of urothelial carcinoma. Histopathology. 2018;72(2):354–6. https://doi.org/10.1111/his.13318.
Vail E, Zheng X, Zhou M, et al. Telomerase reverse transcriptase promoter mutations in glandular lesions of the urinary bladder. Ann Diagn Pathol. 2015;19(5):301–5. https://doi.org/10.1016/j.anndiagpath.2015.06.007.
Al-Ahmadie HA, Iyer G, Lee BH, et al. Frequent somatic CDH1 loss-of-function mutations in plasmacytoid variant bladder cancer. Nat Genet. 2016;48(4):356–8. https://doi.org/10.1038/ng.3503.
Palsgrove DN, Taheri D, Springer SU, et al. Targeted sequencing of plasmacytoid urothelial carcinoma reveals frequent TERT promoter mutations. Hum Pathol. 2019;85:1–9. https://doi.org/10.1016/j.humpath.2018.10.033.
Guo CC, Dadhania V, Zhang L, et al. Gene expression profile of the clinically aggressive micropapillary variant of bladder cancer. Eur Urol. 2016;70(4):611–20. https://doi.org/10.1016/j.eururo.2016.02.056.
Tschui J, Vassella E, Bandi N, et al. Morphological and molecular characteristics of HER2 amplified urothelial bladder cancer. Virchows Arch. 2015;466(6):703–10. https://doi.org/10.1007/s00428-015-1729-4.
Schneider SA, Sukov WR, Frank I, et al. Outcome of patients with micropapillary urothelial carcinoma following radical cystectomy: ERBB2 (HER2) amplification identifies patients with poor outcome. Mod Pathol. 2014;27(5):758–64. https://doi.org/10.1038/modpathol.2013.201.
Isharwal S, Huang H, Nanjangud G, et al. Intratumoral heterogeneity of ERBB2 amplification and HER2 expression in micropapillary urothelial carcinoma. Hum Pathol. 2018;77:63–9. https://doi.org/10.1016/j.humpath.2018.03.015.
Iyer G, Al-Ahmadie H, Schultz N, et al. Prevalence and co-occurrence of actionable genomic alterations in high-grade bladder cancer. J Clin Oncol. 2013;31(25):3133–40. https://doi.org/10.1200/JCO.2012.46.5740.
Fleischmann A, Rotzer D, Seiler R, Studer UE, Thalmann GN. Her2 amplification is significantly more frequent in lymph node metastases from urothelial bladder cancer than in the primary tumours. Eur Urol. 2011;60(2):350–7. https://doi.org/10.1016/j.eururo.2011.05.035.
Vaira V, Faversani A, Dohi T, et al. miR-296 regulation of a cell polarity-cell plasticity module controls tumor progression. Oncogene. 2012;31(1):27–38. https://doi.org/10.1038/onc.2011.209.
Gentili C, Castor D, Kaden S, et al. Chromosome missegregation associated with RUVBL1 deficiency. PLoS One. 2015;10(7):e0133576. Published 2015 Jul 22. https://doi.org/10.1371/journal.pone.0133576.
Sanfrancesco J, McKenney JK, Leivo MZ, Gupta S, Elson P, Hansel DE. Sarcomatoid Urothelial carcinoma of the bladder: analysis of 28 cases with emphasis on clinicopathologic features and markers of epithelial-to-mesenchymal transition. Arch Pathol Lab Med. 2016;140(6):543–51. https://doi.org/10.5858/arpa.2015-0085-OA.
Sung MT, Wang M, MacLennan GT, et al. Histogenesis of sarcomatoid urothelial carcinoma of the urinary bladder: evidence for a common clonal origin with divergent differentiation. J Pathol. 2007;211(4):420–30. https://doi.org/10.1002/path.2129.
Guo CC, Majewski T, Zhang L, et al. Dysregulation of EMT drives the progression to clinically aggressive sarcomatoid bladder cancer. Cell Rep. 2019;27(6):1781–1793.e4. https://doi.org/10.1016/j.celrep.2019.04.048.
Genitsch V, Kollár A, Vandekerkhove G, et al. Morphologic and genomic characterization of urothelial to sarcomatoid transition in muscle-invasive bladder cancer. Urol Oncol. 2019;37(11):826–36. https://doi.org/10.1016/j.urolonc.2019.09.025.
Weyerer V, Weisser R, Moskalev EA, et al. Distinct genetic alterations and luminal molecular subtype in nested variant of urothelial carcinoma. Histopathology. 2019;75(6):865–75. https://doi.org/10.1111/his.13958.
Zhong M, Tian W, Zhuge J, et al. Distinguishing nested variants of urothelial carcinoma from benign mimickers by TERT promoter mutation. Am J Surg Pathol. 2015;39(1):127–31. https://doi.org/10.1097/PAS.0000000000000305.
Chang MT, Penson A, Desai NB, et al. Small-cell carcinomas of the bladder and lung are characterized by a convergent but distinct pathogenesis. Clin Cancer Res. 2018;24(8):1965–73. https://doi.org/10.1158/1078-0432.CCR-17-2655.
Shen P, Jing Y, Zhang R, et al. Comprehensive genomic profiling of neuroendocrine bladder cancer pinpoints molecular origin and potential therapeutics. Oncogene. 2018;37(22):3039–44. https://doi.org/10.1038/s41388-018-0192-5.
Li Q, Wang H, Peng H, et al. MicroRNAs: key players in bladder Cancer. Mol Diagn Ther. 2019;23(5):579–601. https://doi.org/10.1007/s40291-019-00410-4.
Rouprêt M, Fromont G, Azzouzi AR, et al. Microsatellite instability as predictor of survival in patients with invasive upper urinary tract transitional cell carcinoma. Urology. 2005;65(6):1233–7. https://doi.org/10.1016/j.urology.2005.01.019.
Mueller CM, Caporaso N, Greene MH. Familial and genetic risk of transitional cell carcinoma of the urinary tract. Urol Oncol. 2008;26(5):451–64. https://doi.org/10.1016/j.urolonc.2008.02.016.
Engel C, Loeffler M, Steinke V, et al. Risks of less common cancers in proven mutation carriers with lynch syndrome. J Clin Oncol. 2012;30(35):4409–15. https://doi.org/10.1200/JCO.2012.43.2278.
Bubendorf L, Grilli B, Sauter G, Mihatsch MJ, Gasser TC, Dalquen P. Multiprobe FISH for enhanced detection of bladder cancer in voided urine specimens and bladder washings. Am J Clin Pathol. 2001;116(1):79–86. https://doi.org/10.1309/K5P2-4Y8B-7L5A-FAA9.
Hajdinjak T. UroVysion FISH test for detecting urothelial cancers: meta-analysis of diagnostic accuracy and comparison with urinary cytology testing. Urol Oncol. 2008;26(6):646–51. https://doi.org/10.1016/j.urolonc.2007.06.002.
Kandimalla R, Masius R, Beukers W, et al. A 3-plex methylation assay combined with the FGFR3 mutation assay sensitively detects recurrent bladder cancer in voided urine. Clin Cancer Res. 2013;19(17):4760–9. https://doi.org/10.1158/1078-0432.CCR-12-3276.
Beukers W, van der Keur KA, Kandimalla R, et al. FGFR3, TERT and OTX1 as a urinary biomarker combination for surveillance of patients with bladder cancer in a large prospective multicenter study. J Urol. 2017;197(6):1410–8. https://doi.org/10.1016/j.juro.2016.12.096.
Rodriguez Pena MDC, Tregnago AC, Eich ML, et al. Spectrum of genetic mutations in de novo PUNLMP of the urinary bladder. Virchows Arch. 2017;471(6):761–7. https://doi.org/10.1007/s00428-017-2164-5.
Wang CC, Huang CY, Jhuang YL, Chen CC, Jeng YM. Biological significance of TERT promoter mutation in papillary urothelial neoplasm of low malignant potential. Histopathology. 2018;72(5):795–803. https://doi.org/10.1111/his.13441.
Pal SK, Rosenberg JE, Hoffman-Censits JH, et al. Efficacy of BGJ398, a fibroblast growth factor receptor 1-3 inhibitor, in patients with previously treated advanced urothelial carcinoma with FGFR3 alterations. Cancer Discov. 2018;8(7):812–21. https://doi.org/10.1158/2159-8290.CD-18-0229.
Springer SU, Chen CH, Rodriguez Pena MDC, et al. Non-invasive detection of urothelial cancer through the analysis of driver gene mutations and aneuploidy [published correction appears in Elife. 2018 Nov 12;7:]. Elife. 2018;7:e32143. Published 2018 Mar 20. https://doi.org/10.7554/eLife.32143
Bernard-Pierrot I, Brams A, Dunois-Lardé C, et al. Oncogenic properties of the mutated forms of fibroblast growth factor receptor 3b. Carcinogenesis. 2006;27(4):740–7. https://doi.org/10.1093/carcin/bgi290.
Tomlinson DC, Hurst CD, Knowles MA. Knockdown by shRNA identifies S249C mutant FGFR3 as a potential therapeutic target in bladder cancer. Oncogene. 2007;26(40):5889–99. https://doi.org/10.1038/sj.onc.1210399.
Lamont FR, Tomlinson DC, Cooper PA, Shnyder SD, Chester JD, Knowles MA. Small molecule FGF receptor inhibitors block FGFR-dependent urothelial carcinoma growth in vitro and in vivo. Br J Cancer. 2011;104(1):75–82. https://doi.org/10.1038/sj.bjc.6606016.
Knowles MA. Novel therapeutic targets in bladder cancer: mutation and expression of FGF receptors. Future Oncol. 2008;4(1):71–83. https://doi.org/10.2217/14796694.4.1.71.
Loriot Y, Necchi A, Park SH, et al. Erdafitinib in locally advanced or metastatic urothelial carcinoma. N Engl J Med. 2019;381(4):338–48. https://doi.org/10.1056/NEJMoa1817323.
Teo MY, Bambury RM, Zabor EC, et al. DNA damage response and repair gene alterations are associated with improved survival in patients with platinum-treated advanced urothelial carcinoma. Clin Cancer Res. 2017;23(14):3610–8. https://doi.org/10.1158/1078-0432.CCR-16-2520.
Teo MY, Seier K, Ostrovnaya I, et al. Alterations in DNA damage response and repair genes as potential marker of clinical benefit from PD-1/PD-L1 blockade in advanced urothelial cancers. J Clin Oncol. 2018;36(17):1685–94. https://doi.org/10.1200/JCO.2017.75.7740.
Desai NB, Scott SN, Zabor EC, et al. Genomic characterization of response to chemoradiation in urothelial bladder cancer. Cancer. 2016;122(23):3715–23. https://doi.org/10.1002/cncr.30219.
Liu D, Plimack ER, Hoffman-Censits J, et al. Clinical validation of chemotherapy response biomarker ERCC2 in muscle-invasive urothelial bladder carcinoma. JAMA Oncol. 2016;2(8):1094–6. https://doi.org/10.1001/jamaoncol.2016.1056.
Plimack ER, Dunbrack RL, Brennan TA, et al. Defects in DNA repair genes predict response to neoadjuvant cisplatin-based chemotherapy in muscle-invasive bladder cancer. Eur Urol. 2015;68(6):959–67. https://doi.org/10.1016/j.eururo.2015.07.009.
Lotan Y, Woldu SL, Sanli O, Black P, Milowsky MI. Modelling cost-effectiveness of a biomarker-based approach to neoadjuvant chemotherapy for muscle-invasive bladder cancer. BJU Int. 2018;122(3):434–40. https://doi.org/10.1111/bju.14220.
Fan Y, Shen B, Tan M, et al. Long non-coding RNA UCA1 increases chemoresistance of bladder cancer cells by regulating Wnt signaling. FEBS J. 2014;281(7):1750–8. https://doi.org/10.1111/febs.12737.
Ke HL, Lin J, Ye Y, et al. Genetic variations in glutathione pathway genes predict cancer recurrence in patients treated with transurethral resection and Bacillus Calmette-Guerin instillation for non-muscle invasive bladder cancer. Ann Surg Oncol. 2015;22(12):4104–10. https://doi.org/10.1245/s10434-015-4431-5.
Kim YJ, Ha YS, Kim SK, et al. Gene signatures for the prediction of response to Bacillus Calmette-Guerin immunotherapy in primary pT1 bladder cancers. Clin Cancer Res. 2010;16(7):2131–7. https://doi.org/10.1158/1078-0432.CCR-09-3323.
Kiselyov A, Bunimovich-Mendrazitsky S, Startsev V. Treatment of non-muscle invasive bladder cancer with Bacillus Calmette-Guerin (BCG): Biological markers and simulation studies. BBA Clin. 2015;(4):27–34. Published 2015 Jun 10. https://doi.org/10.1016/j.bbacli.2015.06.002.
Ahirwar DK, Mandhani A, Mittal RD. IL-8 -251 T > A polymorphism is associated with bladder cancer susceptibility and outcome after BCG immunotherapy in a northern Indian cohort. Arch Med Res. 2010;41(2):97–103. https://doi.org/10.1016/j.arcmed.2010.03.005.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ertoy Baydar, D. (2021). Molecular Pathology. In: Zhou, H., Guo, C.C., Ro, J.Y. (eds) Urinary Bladder Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-71509-0_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-71509-0_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71508-3
Online ISBN: 978-3-030-71509-0
eBook Packages: MedicineMedicine (R0)