Abstract
Pulmonary rehabilitation (PR) is a non-pharmacological intervention addressed to chronic obstructive pulmonary disease (COPD) and non-COPD patients, a key management strategy scientifically demonstrated to improve exercise capacity, dyspnoea, health status and psychological wellbeing. The main body of literature comes from COPD patients, as they provide the core evidence for PR programmes. PR is recommended even to severe patients having chronic hypercapnic respiratory failure; their significant psychological impairment and potential for greater instability during rehabilitation need to be carefully considered by the multidisciplinary team. Optimizing medical management (e.g., inhaled bronchodilators, oxygen therapy, noninvasive ventilation) may enhance the results of exercise training. Patients who already receive long-term domiciliary noninvasive ventilation (NIV) for chronic respiratory failure might exercise with NIV during physical training if acceptable and tolerable to the patient. It is not advisable to offer long-term domiciliary NIV with the only aim to improve outcomes during PR course. Chest physiotherapy and cough augmentation techniques enhance mucus clearance. Long-term adherence to exercise is an important goal of PR programmes and teams, targeting to translate all-domain gains of PR into increased physical activity and participation to real life.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic obstructive pulmonary disease
- Pulmonary rehabilitation
- Noninvasive ventilation
- Chest physiotherapy
- Bilevel positive airway pressure
1 Brief Introduction to the Concept of Pulmonary Rehabilitation
Pulmonary rehabilitation is described as a “comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behaviour change, designed to improve the physical and psychological condition of people with chronic respiratory disease, and to promote the long-term adherence to health-enhancing behaviours” [1]. The main goal for PR programmes is to enhance physical activity towards normal levels, to return the patient to the highest possible capacity in order to achieve the maximum level of independence and functioning in the community [2]. Despite being a cost-beneficial intervention, only approximately two-fifth of chronic respiratory patients have been informed by their health care provider about PR and its positive results. This might be an explanation why <2% of the patients are referred to one of the available PR programmes.
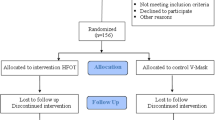
The main body of evidences comes from COPD patients, but PR is effective in many others obstructive and restrictive conditions. COPD patients are referred to PR due to persistent respiratory symptoms and/or limited activities of daily living and an unsatisfactory response to the medical treatment offered in primary care. It is recommended to all symptomatic patients, regardless the severity of disease, but recommendations are stronger in moderate-to-severe COPD. PR is addressed to stable patients, after an acute exacerbation, in intensive care unit, in the perioperative period after a lung transplantation, before and after lung cancer surgery, and before endobronchial lung volume reduction [3]. It can be offered in a hospital-based outpatient setting, in an inpatient setting (Fig. 49.1), a community-based setting and at the patient home [1].
Exercise training is the cornerstone in PR programmes and the best approach for increasing muscle strength, decreasing symptoms, reducing mood abnormalities, improving cardiovascular function and the motivation for physical activity [3]. Exercise training (upper and lower limb endurance aerobic exercise, resistance training, flexibility training, inspiratory muscle training—Fig. 49.2) should be completed by education (information about disease, bronchial hygiene and mobilization of secretions by cough managing, breathing techniques, relaxation, energy conservation, stress management, coping techniques and education of relatives), psychological and nutritional support [3, 4]. Typical modes of aerobic exercise are walking or cycling. In stable COPD patients, a combination of endurance and resistance training should be performed to maximize improvement in limb muscle function and whole-body exercise capacity [1].
Breathing training consists of purse-lipped, controlled and diaphragmatic breathing [5]. Airway clearance during chest infections through intensive physiotherapy consists in a modified active cycle of breathing technique accompanied by physical procedures such as percussions and shaking, and manually assisted cough; however, standard or intensive physiotherapy might be tiring for the patients and can precipitate episodic oxygen desaturation [6]. There are some cough augmentation techniques like: cough after inspiration supported by a NIV ventilator type bi-level positive airway pressure (BiPAP); exsufflation-assisted cough with delivery of negative pressure initiated manually at the end of inspiration; insufflation (given manually during inspiratory phase) and exsufflation-assisted cough with delivery of the negative pressure immediately preceding the cough effort via a facial mask [6].
2 Noninvasive Ventilation: Why to Think About It?
In advanced stages of respiratory diseases, patients frequently develop chronic hypercapnic respiratory failure (CHRF). NIV is the standard treatment for patients with CHRF due to COPD and restrictive lung disease, and a major indication for home mechanical ventilation (HMV) in Europe [7]. COPD patients benefit from NIV once they have COPD GOLD stage III or IV and CHRF (arterial partial pressure for carbon dioxide >6.0 kPa) in a stable clinical condition. In patients with CHRF, long-term noninvasive positive pressure ventilation (NPPV) improves important physiological variables such as blood gases and lung hyperinflation. Results from clinical studies have shown that NPPV improves exercise capacity, exercise-related dyspnoea, pulmonary cachexia, sleep quality and health-related quality of life (QRQoL). Moreover, NPPV treatment might be associated with fewer hospital admission and lower overall treatment costs [8]. The best results with long-term NPPV have been noted in studies using more intensive forms of NPPV, with higher inspiratory pressures and high back-up frequencies that have improved or even normalised hypercapnia [7]. They have been reported two disadvantages of high-intensity NPPV: patients need more days in hospital to acclimatise and there is an increased expiratory leakage comparing to low-intensity NPPV. In high-pressure NIV may develop a haemodynamic compromise due to reduced venous return from high intra-thoracic pressures. These factors may affect results of NIV in NIV-naïve patients or in those with compromised cardiac performance.
It was hypothesized that a substantial reduction in hypercapnia may lead to the benefits of NIV, including survival, but this is not entirely true. A survival benefit was shown without a change in daytime hypercapnia, and not all studies showing a reduction in hypercapnia could demonstrate improvements in survival [7]; consecutively, chronic NIV may lead to above mentioned benefits through different mechanisms [7] like resting the respiratory muscles at night [3]. Moreover, NIV might prevent exacerbations in a subgroup of frail severe persistent hypercapnic patients, an effect that might also affect survival [7]. Nevertheless, it is still unclear how and why chronic NIV improves survival [7]. Recent pulmonary rehabilitation BTS guidelines suggest that NIV during exercise training should be offered to patients who already receive domiciliary NIV [4]. With increased use of high-pressure NIV for home therapy, the use of NIV during PR would become more feasible.
Köhnlein et al. have conducted a study in 2014 with the intention to assess survival in chronic hypercapnic COPD patients using NPPV (ResMed, Martinsried, Germany; Weinmann, Hamburg, Germany; and Tyco Healthcare, Neuburg, Germany ventilators) in addition to standard treatment for at least 6 h at night and anytime during daytime. The results provided evidence that NPPV addition in a group of stable COPD patients reduces hypercapnia, improves overall survival, exercise capacity and HRQoL over 1 year when comparing with guideline-oriented COPD treatment without NPPV [8]. In the study conducted by Raveling et al. in 2018, NIV was initiated in COPD patients in a stable condition and after an episode of acute respiratory failure using BiPAP (Synchrony and A30 Respironics, Murrysville, PA, USA) [7]. After 3 months results have shown that a higher body mass index and forced expiratory volume in 1 s, a lower bicarbonate before NIV initiation, younger age and NIV initiated in stable conditions were independently associated with better survival [7]. A higher level of bicarbonate before NIV initiation, the use of higher inspiratory ventilatory pressures, the presence of anxiety symptoms, and NIV initiated after an exacerbation compared with NIV initiated in stable disease were associated with a better reduction in arterial partial pressure of carbon dioxide, as NPPV improves respiratory centre’s sensitivity to carbon dioxide.
3 Types of NIV Useful in Association with Pulmonary Rehabilitation
3.1 Negative Airway Pressure Devices
Techniques to deliver ventilatory support have developed in nineteenth century and became popular during the polio epidemic in early twentieth century [9]. There are two types of negative pressure ventilation (NPV). One is tank ventilation that provides intermittent sub-atmospheric pressure around the whole body. The other one is cuirass ventilator that provides negative pressure around the chest only and creates a gradient pressure between thorax and lower body, which may increase intrathoracic venous return, right cardiac output and lung perfusion [5]. Breathing pattern undergoing cuirass ventilator is a real approximation of the normal physiological breathing, with more natural distribution of air in the lungs. Hence, NPV does not restrict the patients’ activities and they can be more comfortable [5].
3.2 Positive Airway Pressure Devices
Positive airway pressure (PAP) devices offer today a consistent solution; they unload respiratory system and increase its capacity, with a consecutive reduction in neural respiratory drive and breathlessness [9]. Limitations of negative pressure devices promoted development of PAP devices to deliver continuous positive airway pressure (CPAP) and bi-level pressure support. CPAP delivers a fixed level of positive airway pressure during the whole respiratory cycle [9].
Bi-level pressure support, known as NIV, delivers a positive pressure during expiration and a higher positive pressure during inspiration to support inspiratory effort. PAP devices deliver respiratory support through oronasal or nasal mask interfaces, and not through endotracheal tube or tracheostomy, thus being considered as non-invasive devices [9]. PAP devices have well established benefits in acute and chronic respiratory failure in a large range of conditions, including COPD, obstructive sleep apnoea, obesity-related respiratory failure, progressive neuromuscular disease and cardiogenic pulmonary oedema, through restoring respiratory muscles load-capacity balance, promoting alveolar ventilation and improving gas exchange [9].
3.3 Non-invasive Ventilation as an Adjunct to Pulmonary Rehabilitation
NIV may be used as an adjunctive therapy to PR that unloads the respiratory muscles with the aim to increase the intensity of exercise training in selected patients with severe chronic respiratory diseases who have a suboptimal response to exercise [1]. The benefits appear to be more marked in patients with severe COPD, and higher tolerated positive pressure may lead to greater improvements, with improved exercise performance and reduced breathlessness [1]. COPD is characterized by recurrent exacerbations leading to episodes of severe clinical deterioration requiring hospitalization and ventilatory support. Persistent hypercapnia after an episode of acute exacerbation of COPD (AECOPD) is associated with excess mortality and early hospitalization. That means extra costs for caring same patients; therefore, it is an urgent need for measures to prevent readmissions in this area. Non-invasive PAP interventions applied during exercise, at rest and in the end-of-life setting, can be used to restore the balance of respiratory muscle load and capacity, with reducing neural respiratory drive and dyspnoea [9]. Table 49.1 summarises the use of NIV and chest physiotherapy along to PR in different stages of COPD.
Long-term oxygen therapy (LTOT) and non-invasive ventilation (NIV) are potentially valuable therapeutic options, especially in COPD patients with severe lung hyperinflation and exercise-induced desaturation noticed during exercise training as part of a comprehensive PR programme [1]. For patients with COPD and chronic hypoxia LTOT is crucial in terms of improving survival. In these cases, use of supplemental oxygen during exercise may be associated with reduced exertional pulsoximetric arterial oxygen saturation (SpO2) and increased exercise performance. The addition of nasal positive pressure ventilation to LTOT in hypercapnic patients has been shown to improve arterial blood gases, dyspnoea, quality of life and survival. Oxygen supplementation in moderate to severe COPD patients can acutely increase exercise capacity, the amount of training they can undertake, and thus the benefits of PR. Alleviation at a certain extend of ventilatory limitation will allow greater cardiac and muscular stress, with further beneficial effects on stroke volume and oxygen extraction [4]. SpO2 should be >88% during exercise; if SpO2 is ≤88% while breathing room air, supplemental oxygen should be used to maintain SpO2 at >88% or >90% according to different authors [5].
3.4 Pulmonary Rehabilitation and Noninvasive Ventilation in Acute Exacerbation of COPD
COPD exacerbations are known to deteriorate life quality, to enhance disease progression and increase mortality [3]. Acute respiratory failure leading to acute or acute-on-chronic respiratory acidosis, develops when the respiratory muscles fall to achieve adequate alveolar ventilation despite high levels of diaphragmatic activity [10] and when appear alterations in central ventilatory control [8]. The official American Thoracic Society/European Respiratory Society clinical practice guidelines suggest to consider bi-level NIV in patients with AECOPD in three clinical settings: to prevent acute respiratory acidosis; to prevent endotracheal intubation and invasive mechanical ventilation in patients with mild to moderate acidosis and respiratory distress; and as an alternative to invasive ventilation in patients with severe acidosis and more severe respiratory distress [10]. Bi-level NIV is known to improve related symptoms, and to reduce the length of hospital stay, intubation rate and mortality rate [10]. Applying of noninvasive positive pressure ventilation in these cases will correct acute respiratory acidosis and relieve dyspnoea, will lower the rate of ventilatory associated pneumonia and extend hospital stays, that often results in mortality. NPPV is a life support intervention that does not require sedation, allowing the patients to communicate with the family and caregivers during the interruptions, to eat, to drink and to take decisions regarding their care. The outcomes were more favourable in COPD patients with strong cough and awake.
British Thoracic Society recommends the initiation of early PR within 1 month of hospital discharge after exacerbation, consisting of a minimum of twice a week supervised session, lasting between 6 and 12 weeks [4]. PR can be delivered late post-exacerbation, that is 6 months after COPD exacerbations, the majority flare ups requiring hospitalisation or hospital at home services [4]. More recently, a reliable group of experts have strongly recommended the initiation of PR during and shortly after an exacerbation-related hospitalisation, as this results in clinically relevant improvements in exercise performance, lower-limb muscle function, balance and quality of life compared to usual care [2]. The integrated peri-exacerbation PR programme must be tailored carefully to the patients’ physical and psychological status, making it safe and effective for patients with a spectrum of illnesses, even in mechanically ventilated, critically ill patients [2]. NIV can improve exercise tolerance with less desaturation in patients admitted to hospital with an exacerbation of chronic respiratory disease, but participation is limited in older populations; it is more suitable in younger patients with fewer comorbidities.
Early mobilisation and exercise therapy within the intensive care unit target the goals of enhancing the functional outcome, health-related quality of life and reducing of healthcare utilization [2]. In these cases, specifically, exercise should combine progressive muscle resistance and aerobic training [3]. Moss et al. proposed a graduate manner to increase the physical training programme, for 30 min while in intensive care unit up to 60 min when the patient was in a regular ward, in an outpatient setting or at home, with five components: techniques for proper breathing during exercise; progressive range of motion; therapeutic exercises addressed to the muscle strength; exercises designed to improve core mobility and strength; and functional mobility retraining including bed mobility, transfers, gait and balance [11]. Unfortunately, an intensive physical therapy programme did not improve long-term physical functioning compared with a standard-of-care physical therapy programme [11].
3.5 Pulmonary Rehabilitation and Noninvasive Ventilation in Stable COPD Patients
Exercise capacity is significantly reduced in patients with COPD and chronic hypercapnia. Reduced ventilatory capacity combined with an increased ventilatory load leads to intolerable dyspnoea at low level of exercise. However, severe COPD patients have strong recommendations to follow a PR course and to perform a specific exercise training, but these individuals have difficulties in performing exercise training at a sufficiently high training intensity to achieve physiological and clinical benefits due to severe breathlessness. Therefore, NIV was proposed has an adjunct to PR in patients with severe COPD in order to allow the patients to exercise at a higher training intensity and to obtain a greater effect compared to exercise training without NIV, with both improvement in physical functions and exercise performance [12]. In majority of studies have been used relatively low to moderate levels of inspiratory pressure during exercise, and the optimal mode and settings in a population with very severe lung disease is still unknown [12]. A Cochrane review performed in 2014 by Menadue et al. has shown that NIV during exercise training may allow COPD patients to exercise at a higher training intensity and to achieve a greater physiological training effect compared with exercise training alone or exercise training with sham NIV [12]. It is currently unknown if the demonstrated benefit of NIV during exercise training is clinically worthwhile or cost-effective [12].
NIV delivered during exercise enables patients with severe COPD to exercise at higher intensity, to increase their exercise endurance time and walking distance [8, 9]. NPPV is a feasible and beneficial tool in hospital-based PR [8], but clinical application of NIV during physical exercise is limited by time consuming NIV setup, need for specialist supervision, limited portability of devices and the ventilator model, battery duration and poor patient tolerance [9]. Another recommendation is at night in patients with chronic respiratory failure, to improve their clinical status during the exercise programme, functional capacity, HRQoL and sleep quality [8, 9]. The benefits are achieved through optimization of the respiratory muscle load-capacity-drive relationship [9].
NIV prolongs endurance during exercise in COPD, but routine use is difficult. Recently, handheld, battery operated and portable NIV (pNIV) devices, providing pressure support ventilation, require the patient to inspire and expire through a mouthpiece, are intended to be applied at the end of exercise to reduce the time to return at baseline respiratory status in COPD patients, thus acting as dyspnoea-relief tools. They provide an accessible and acceptable method to improve exercise capacity and relieve exertional breathlessness by reducing dynamic hyperinflation and leg discomfort, together with improving cardiac output, systemic oxygen delivery and exercise endurance time [9, 13]. The pNIV device (VitaBreath, Philips, Respironics, Morrisville, PA, USA) delivers 18 cmH2O inspiratory and 8 cmH2O expiratory pressures, and it is used only during recovery periods interspersing bouts of moderate or high-intensity physical activity [13]. The fixed pressures may be sub-optimal in some patients; therefore, the future devices should have the ability to adjust expiratory positive airway pressure, making the pressure support more desirable and potentially automated [13]. Future studies should investigate the additive effect of oxygen supplementation to intermittent NIV support during conventional PR [13].
Less practical in daily life but providing a greater improvement in exercise tolerance are the continuous positive pressure support devices like CPAP, inspiratory pressure support including proportional assist ventilation (PAV), and noninvasive “open” ventilation (NIOV) [13]. All these ventilation support strategies provide continuous unloading of the respiratory muscles and reduce the work of breathing, thus reducing dyspnoea and enhancing exercise tolerance in COPD patients [13, 14]. Portable CPAP devices, light-weighted and battery-powered, are very useful in cases with excessive dynamic airway collapse where they provide a pneumatic stent to maintain airway patency, reduce expiratory resistance and improve expiratory airflow [9]. After providing PAV to a group of patients with more severe COPD during a supervised high-intensity out-patients cycle exercise programme, mean training and peak work rate was higher in this group. PAV is a mode of ventilation that matches ventilator output to patient effort, allowing the patients to prolong exercises and to achieve greater improvements in exercise performance [14]. NIOV system (BT-V2S Breath Technologies) operating in conjunction with a portable oxygen tank was found to decrease respiratory muscle activation and dyspnoea, and to improve cycle ergometer exercise tolerance; it is a light, wearable 1-lb ventilator, practical for facilitating activities of everyday living [15].
Some centres use Assist Pressure Control Ventilation (APCV) mode with a high backup rate, intending to achieve controlled ventilation. The use of APCV mode during exercise implies to best set up a minimum mandatory backup rate along with a fixed inspiratory time for both patient and machine-triggered breaths [12]. Negative pressure ventilation (NPV), when used as an adjuvant to PR, improves lung function, increases exercise capacity, prolongs survival and reduces exacerbations in COPD patients with exercise desaturation, who have an increased mortality risk compared with non-desaturating COPD patients. The NPV group had a slower yearly decline in lung function and in 6-min walking distance, irrespective of exercise desaturation [5]. Maintenance of NPV reduces long-term mortality in COPD patients, irrespective of the presence of desaturation during the 6-min walking test.
3.6 Pulmonary Rehabilitation and Noninvasive Ventilation at Home
After successfully completing a course of PR, the only way to maintain the achieved improvements is to continue with a home-based exercise programme and participate to follow-up visits in the PR centre. The scope is to make chronic respiratory patients to become more active in daily living life and to preserve endurance capacity, psychological and cognitive benefits [3]. NIV can be used for long-term treatment of chronic respiratory failure at home. High-pressure NIV is addressed to the patients who have persistent hypercapnia for 2–4 weeks after resolution of respiratory acidemia that has required acute NIV. In COPD patients, long-term NIV decreases arterial partial pressure of carbon dioxide and improves mortality [2]. NIV may be initiated by using nasal, oronasal or total face masks according to the patient preference. The aim is to achieve control over nocturnal hypoventilation with a high-pressure ventilation strategy. After 12 weeks of use at home the pNIV devices, patients reported reduced anxiety and recovery time from breathlessness, as well as improvement in the speed, duration and confidence to undertake activities of daily living [13]. Another treatment option would be the use of NIV in addition to oxygen therapy in home setting, at least for 6 h per night.
Manual techniques, including postural drainage, percussion and vibration, and breathing pattern exercises can be implemented to assist airway clearance [9]. Mechanical insufflation-exsufflation technique is not an alternative for secretion clearance but can be vital for expulsing secretions from central airways for patients with weak respiratory muscles and a partially preserved bulbar (laryngeal intrinsic) muscle function [6]. This new technique of secretion management reduces airway resistance and respiratory muscle load, with increased lung volumes and improved ventilatory capacity; it produces a higher peak cough flow than a voluntary unassisted cough or a cough assisted by NIV [6, 9]. Mechanical insufflation-exsufflation technique is well tolerated and should be considered as an adjunct to manual airway clearance techniques for patients with a peak cough flow less than 160 L/min [9].
3.7 Pulmonary Rehabilitation and Noninvasive Ventilation in Palliative Care Services
In advanced chronic patients admitted to palliative care services, it is essential to reduce breathlessness and improve survival, quality of life and function. The use of PAP devices in end-stage hypercapnic disease is frequently implemented in clinical practise, as suggested by international guidelines. Notably, timing of its initiation remains controversial because of potential side-effects as mask discomfort and limited communication with caregivers and family [9]. NPPV is a mean of potentially ensuring the highest quality of life during the final hours, allowing to reduce the dose of morphine necessary to palliate dyspnoea, maintaining better cognitive function and with a similar rate of acceptance by patients compared with oxygen therapy [10]. The American Thoracic Society/European Respiratory Society guidelines suggest offering NIV to dyspnoeic patients for palliation in the setting of terminal cancer or other terminal conditions [10].
4 Conclusions
Pulmonary rehabilitation is a unique non-pharmacological therapy addressed to symptomatic COPD and non-COPD patients with a poor HRQoL due to breathlessness and fatigue. Because of dyspnoea, patients become more socially isolated and finally housebound. PR, LTOT and NIV bring hope in this difficult and long-term fight with a chronic respiratory disease, encouraging patients to meet other people with same disability and fear from illness and death, to exercise together and to continue their lives in a better condition.
Questions and Answers
-
1.
Pulmonary rehabilitation is a non-pharmacological intervention addressed to chronic respiratory patients that improves:
-
(a)
Exercise capacity
-
(b)
Survival
-
(c)
Dyspnoea
-
(d)
Health-related quality of life
-
(e)
Muscle performance
Answers: (a), (c), (d)
-
(a)
-
2.
Standard medical management in chronic respiratory conditions might be optimized through:
-
(a)
Thoracic taping
-
(b)
Pulmonary rehabilitation
-
(c)
Oxygen therapy
-
(d)
Saline therapy
-
(e)
Non-invasive ventilation
Answers: (b), (c), (e)
-
(a)
-
3.
Non-invasive positive pressure ventilation used in chronic hypercapnic respiratory failure conditions improves:
-
(a)
Blood gases
-
(b)
Survival
-
(c)
Lung hyperinflation
-
(d)
Cardiac fitness
-
(e)
Exercise capacity
Answers: (a), (c), (e)
-
(a)
-
4.
The disadvantages of using high-intensity non-invasive positive pressure ventilation are:
-
(a)
Face wounds
-
(b)
Bronchial epithelial damage
-
(c)
More days to stay in hospital to acclimatise
-
(d)
Increased expiratory leakage
-
(e)
Developing of a haemodynamic compromise
Answers: (c), (d), (e)
-
(a)
Abbreviations
- AECOPD:
-
Acute exacerbation of chronic obstructive pulmonary disease
- APCV:
-
Assist pressure control ventilation
- BiPAP:
-
Bi-level positive airway pressure
- CHRF:
-
Chronic hypercapnic respiratory failure
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- FEV1:
-
Forced expiratory volume in 1 s
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- HRQoL:
-
Health-related quality of life
- LTOT:
-
Long-term oxygen therapy
- NIOV:
-
Noninvasive “open” ventilation
- NIV:
-
Noninvasive ventilation
- NPPV:
-
Noninvasive positive pressure ventilation
- NPV:
-
Negative pressure ventilation
- PAP:
-
Positive airway pressure
- PAV:
-
Proportional assist ventilation
- pNIV:
-
Portable noninvasive ventilation
- PR:
-
Pulmonary rehabilitation
- SpO2:
-
Pulsoximetric arterial oxygen saturation
References
Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64.
Houben-Wilke S, Augustin IM, Vercoulen JH, et al. COPD stands for complex obstructive pulmonary disease. Eur Respir Rev. 2018;27:180027.
Candemir I. Advances in pulmonary rehabilitation for chronic obstructive pulmonary disease and associated conditions. In: McCarthy C, editor. COPD – an update in pathogenesis and clinical management. Rijeka: Intech Open; 2018. p. 131–51.
Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax. 2013;68:ii1–ii30.
Huang HY, Chou PC, Joa WC, et al. Pulmonary rehabilitation coupled with negative pressure ventilation decreases decline in lung function, hospitalizations, and medical cost in COPD. Medicine (Baltimore). 2016;95(41):e5119.
Chatwin M, Ross E, Hart N, et al. Cough augmentation with mechanical insufflation/exsufflation in patients with neuromuscular weakness. Eur Respir J. 2003;21:502–8.
Raveling T, Bladder G, Vonk JM, et al. Improvement in hypercapnia does not predict survival in COPD patients on chronic noninvasive ventilation. Int J COPD. 2018;13:3625–34.
Köhnlein T, Windisch W, Köhler D, et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med. 2014;2:698–705.
D’Cruz RF, Kaltsakas G, Suh ES, et al. Positive airway pressure devices for the management of breathlessness. Curr Opin Support Palliat Care. 2018;12:246–52.
Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426.
Moss M, Nordon-Craft A, Malone D, et al. A randomised trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med. 2016;193(10):1101–10.
Menadue C, Piper AJ. Pressuring stable patients with hypercapnic COPD to exercise. Respirology. 2019;24:195–6.
Vogiatzis I, Chynkiamis N, Armstrong M, et al. Intermittent use of portable NIV increases exercise tolerance in COPD: a randomized, cross-over trial. J Clin Med. 2019;8:94.
Hawkins P, Johnson LC, Nikoletou D, et al. Proportional assist ventilation as an aid to exercise training in severe chronic obstructive pulmonary disease. Thorax. 2002;57:853–9.
Porszasz J, Cao R, Morishige R, et al. Physiologic effect of an ambulatory ventilation system in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(3):334–42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ciobanu, L.D. (2022). Non Invasive Ventilation, Pulmonary Rehabilitation and Chest Physiotherapy-2. In: Esquinas, A.M. (eds) Teaching Pearls in Noninvasive Mechanical Ventilation. Springer, Cham. https://doi.org/10.1007/978-3-030-71298-3_49
Download citation
DOI: https://doi.org/10.1007/978-3-030-71298-3_49
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71297-6
Online ISBN: 978-3-030-71298-3
eBook Packages: MedicineMedicine (R0)