Abstract
This chapter presents evidence for a key role of inflammation in schizophrenia. In animal models, an immune response during the pre- or perinatal phase has been shown to affect lifelong immune function. Furthermore, levels of cytokines and other pro-inflammatory compounds are higher in people with schizophrenia than in healthy controls. Evidence from epidemiological and clinical studies shows that certain infections increase the risk for psychosis, in particular schizophrenia. The so-called vulnerability-stress-inflammation model has been proposed to explain how inflammation is involved in schizophrenia. According to this model, schizophrenia is related to risk genes for inflammation, alterations in the immune system, and exposure to environmental stress factors. Stress is known to increase cytokine levels and may play a role in a chronic proinflammatory state. The proposed involvement of low-level neuroinflammation in schizophrenia is supported by several findings: altered neurotransmission is a typical feature of both neuroinflammation and schizophrenia; patients with schizophrenia have a loss of volume in central nervous system structures and activated microglia; anti-inflammatory drugs have positive effects in schizophrenia; and antipsychotics have anti-inflammatory and immunomodulatory effects. Together, these findings indicate that the immune system may be a potential target for novel treatments for schizophrenia.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Inflammation
- Schizophrenia
- Psychosis
- Psychoneuroimmunology
- Cytokines
- Anti-inflammatory drugs
- Microglia
- Celecoxib
- Infection
- Stress
1 Introduction
Well-regulated inflammation is an essential protective mechanism, for example, to eliminate bacterial and viral infections; however, excessive inflammatory processes can cause harm, as in autoinflammatory diseases such as multiple sclerosis. In the central nervous system (CNS), inflammation can also be either neuroprotective or neurotoxic [1]. The outcome of inflammation depends on interactions between environmental factors and the inflammatory response; genetics; and whether the inflammation is acute or chronic [2]. For example, acute inflammation in the CNS, such as encephalitis, can be fatal within a few hours or days, but a chronic, harmful inflammatory state can also continue over months or even years, such as in multiple sclerosis. In acute CNS inflammation, macrophages and B- and T-cells from the peripheral immune system are assumed to cross the blood-brain barrier. In contrast, chronic CNS inflammation is hypothesized to be related to the activity of the CNS-based immune system. In multiple sclerosis, for example, this local immune activity in the CNS is seen as disseminated activation of microglia [3]. Researchers have referred to these differences between THE involvement of the peripheral and central immune systems as “compartmentalization” [2, 4].
The pathogenetic mechanisms of multiple sclerosis and schizophrenia may show similarities because both affect the CNS, can be chronic, and are characterized by phases of active disease interspersed with phases of remission [5]. However, the inflammatory mechanisms in these two diseases differ. For example, a general neuroinflammatory state is typical for schizophrenia [6], whereas multiple sclerosis shows focal areas of neuroinflammation [3]. This chapter will review possible inflammatory mechanisms of schizophrenia and potential immune-based treatments.
2 CNS Inflammation
Various components of the immune system are involved in inflammation in the CNS, including microglia, astrocytes, cytokines, and cells of the peripheral immune system, such as monocytes, macrophages, and T- and B-lymphocytes. These different parts of the immune system can be affected by a range of factors, including not only environmental toxins and pathogens but also genetics and secondary reactions to neuronal lesions resulting from trauma.
2.1 Microglia
Microglia make up 15% of cells in the CNS and are the most important component of the local immune defense system. They are activated in case of neuroinflammation, for example, resulting from injury or infection in the CNS [7]. Systemic infection also activates microglia, which contribute to the synthesis of proinflammatory cytokines in the CNS that cause so-called sickness behavior and other illness-related mental states [8, 9]. Although initially produced in response to an acute signal, proinflammatory cytokines may then continue to be released for up to 10 months; this finding led to the hypothesis that microglia may be involved in chronic inflammation [7]. In schizophrenia, in addition to activated microglia some studies found higher levels of pro-inflammatory cytokines and lower levels of anti-inflammatory cytokines (see below). As a caveat, one must note that the subdivision of cytokines into pro- and anti-inflammatory is an oversimplification because certain cytokines can show both properties; the respective activity of such cytokines depends on several factors, including the activating signal, timing, and type of target cell [10]. However, this topic is beyond the scope of this chapter.
2.2 Sensitization of the Immune System and the Effects of Stress
Microglia can also be “sensitized” or “primed” by various low-level stimuli [11], including ageing-related processes [12], neurodegeneration [13], and stress [14]. After sensitization, the response of microglia to a low-level stimulus such as minor infection is exaggerated and they show greater pro-inflammatory reactivity [15], perhaps leading to an exacerbation or re-exacerbation of a CNS immune response and affecting behavior. This process of sensitization is also seen in the peripheral immune system. As with microglia, an initial immune response to a stimulus, e.g., stress, strengthens the subsequent immune response or lowers the threshold for a response upon re-exposure to the same stimulus [16]. On the basis of earlier studies, researchers hypothesized that this process is related to a memory function in the acquired immune system [14, 17]. For example, later re-exposure to a stimulus that caused an early childhood infection can result in increased cytokine release and associated neurotransmitter disturbances [18]. Furthermore, in rats stress-related release of the cytokine interleukin-6 (IL-6) reactivated (prenatally) conditioned processes [19].
In addition to infections and trauma, stressful events can evoke a pro-inflammatory immune response [20]. Stress increases the levels of corticosterone, which activates the N-methyl-d-aspartate (NMDA) receptor, and this receptor activation causes microglia to proliferate [21]. The increased cytokine levels associated with this response can present as psychopathological symptoms and behavioral changes [22]. After an acute stressful event, the immune response is normally downregulated; however, studies have shown that chronic stress or repeated stressful events can lower the threshold for the physiological reactions to stress, including the immune system response or neurotransmitter changes [23]. Furthermore, the brains of aged animals were found to be in a proinflammatory state that sensitized them to peripheral infection and stress, so that they showed a greater cytokine response to these stimuli than younger animals [14]. In other animal studies, neurotransmitter responses to a cytokine, for example, tumor necrosis factor-alpha (TNF-α), were greater upon re-exposure [24, 25].
3 The Vulnerability-Stress-Inflammation Model of Schizophrenia
The vulnerability-stress model of schizophrenia was first proposed by Zubin and Spring over four decades ago [26]. The authors hypothesized that physical or mental stress can cause a psychotic episode. Because stress is known to be a cause of inflammation, and inflammation is known to be involved in schizophrenia, the model was further developed into the so-called vulnerability-stress-inflammation model. Evidence for the validity of this model is provided by animal studies, which show that offspring are more vulnerable to developing schizophrenia if an inflammatory response of the mother is stimulated in the second trimester or in the young offspring soon after birth [27]. Besides sensitization (see above), vulnerability to stress is also influenced by genetic factors, as proposed in the pathogen host defense hypothesis of depression [28]. Inflammatory markers and the effects of inflammation on neurotransmitter systems in schizophrenia are further elucidated.
3.1 Inflammatory Markers
An inflammatory process is hypothesized to be involved in the pathophysiology of at least a subgroup of patients with schizophrenia [29, 30], a theory that is supported by a range of findings. First, postmortem studies in schizophrenia have found degradation products of fibrin (a protein involved in coagulation and inflammation) in the brain [31] and cerebrospinal fluid (CSF) [32]. Furthermore, untreated patients with schizophrenia have a blunted type 1 cytokine response and an increased type 2 cytokine response [33]. Meta-analyses of studies in schizophrenia found higher levels of pro-inflammatory cytokines in the peripheral blood in patients with a first episode of the disease and those who had relapsed [34], including the inflammation-marker C-reactive protein [35]; in contrast, levels of some anti-inflammatory cytokines were lower than in healthy controls [34]. The results of a meta-analysis of studies on cytokines in the CSF were similar [36]. When examining these findings, however, one must consider the potential effects of confounding factors such as smoking, body mass index, sex, sleep, and medication. Moreover, blood levels of cytokines may not appropriately reflect their function because several cytokines have a primarily paracrine effect. Lastly, the brain is protected from peripheral inflammation by the blood-brain barrier, and an immune activation with increased pro-inflammatory cytokines in the blood does not necessarily reflect the situation in the brain [37].
3.2 Inflammation and Neurotransmitters
For a long time, research on the neurobiology of schizophrenia has focused mainly on disturbances in dopaminergic neurotransmission. Studies have clearly shown that the dopamine system is altered in schizophrenia [38], but the exact relationship remains unclear and results of studies on antidopaminergic drugs have been disappointing. At least two cytokines may be involved in the changes in neurotransmitter systems seen in schizophrenia: IL-1ß, which has been shown to cause rat mesencephalic progenitor cells to be converted into a dopaminergic phenotype [39,40,41], and IL-6, which shortens the survival of serotonergic neurons in the fetal brain [42].
The interaction between cytokines and neurotransmitters in certain brain regions and in particular during brain development has been shown to contribute to the pathophysiology of schizophrenia. In a mouse model, Winter et al. [43] found a significant increase in the dopamine levels in fetal brains after eliciting an immune response in the pregnant dams with a viral mimetic (poly I:C). The authors suggested that the poly I:C-induced immune response caused an excess of dopamine in the midbrain, a structure that is affected in patients with schizophrenia [43]. However, chronic administration of the cytokine interferon-alpha in animals was associated with a reduction in striatal dopamine release and with anhedonia [44]. Anhedonia is a characteristic negative symptom of schizophrenia, and negative symptoms are often found in chronic schizophrenia [45]. Other authors have proposed that latent persistent infections may result in imbalanced immune reactions [46]. Thus, inflammation may have diverse effects on dopaminergic neurotransmission and may be involved in the chronification of schizophrenia.
Another key neurotransmitter in the pathophysiology of schizophrenia is glutamate, the most abundant neurotransmitter in the CNS, which is involved in cytokine-directed tryptophan/kynurenine metabolism. Kynurenic acid, one of three or more intermediate neuroactive products in the kynurenine pathway, is the only known naturally occurring NMDA receptor antagonist in the human CNS [47]. In schizophrenia, a predominant type 2 immune response is proposed to inhibit indoleamine 2,3-dioxygenase (IDO), resulting in increased kynurenic acid production; kynurenic acid acts as an antagonist at NMDA receptors, which in turn decreases glutamate neurotransmission [48, 49]. Support for this hypothesis is provided by studies that found NMDA receptor antibodies in about 10% of untreated patients with acute schizophrenia [50, 51]. Some studies found higher kynurenic acid levels in the CSF [52, 53] and brains of patients with schizophrenia [54, 55] and in animal models of schizophrenia [56], and others found no changes in levels in the peripheral blood of patients with first-episode schizophrenia [57] or in other groups of schizophrenia patients [58]. Antipsychotic medication affects kynurenine metabolites and thus may be a confounder in studies [57,58,59].
4 Infection and Schizophrenia
Studies in animal models have shown that pre- and perinatal infections increase the likelihood of schizophrenia in offspring [60, 61]. For example, after prenatal exposure to viral agents animal offspring show symptoms typical of schizophrenia, including cognitive deficits and abnormalities in the startle reflex [62, 63]. The relationship between exposure to infections and a higher risk for schizophrenia appears to hold true in humans, too, and has been shown for prenatal or childhood viral exposure [64,65,66,67], respiratory infections [68], genital or reproductive tract infections [68, 69], Toxoplasma gondii infection [70], and other infections [71,72,73,74]. Findings on virus antibody titers in patients with schizophrenia are inconsistent [75], although this may be because the studies did not control for potential confounders, such as medication [76]. In an earlier study, we found higher titers of antibodies to various pathogens in patients with schizophrenia than in healthy controls, a phenomenon we named the “infectious index” [77]. Another study showed that the mothers of people with schizophrenia spectrum disorders had higher second-trimester levels of the pro-inflammatory cytokine IL-8 than controls [78].
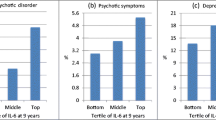
Possible mechanisms of the association between early life infection and schizophrenia are of interest because schizophrenia is a disease of late adolescence/early adulthood. Many studies in animal models have shown that early infection or immune activation influences several neurodevelopmental processes, including dopaminergic and glutamatergic neurotransmission [40, 79]. In humans, studies on some infections [80] and a cohort study of bacterial infection are examples that support this explanation [68]. Furthermore, increased levels of cytokines or CRP in childhood predict an increased risk for schizophrenia [81].
Infection in adulthood also increases the risk of developing schizophrenia. A large epidemiological register study in Denmark found a higher risk for schizophrenia and schizophrenia spectrum disorders in people hospitalized for autoimmune disorders or severe infections, particularly in patients with both diseases [82]. However, the study found no evidence that early exposure to infections, including prenatal exposure, increased the risk for schizophrenia [82, 83].
5 Inflammation and CNS Volume Loss
Neuroimaging studies have not shown marked inflammation-related changes in schizophrenia, although they have found CNS volume reductions in first-episode schizophrenia and progressive volume loss in the further disease course [84,85,86,87]. People with schizophrenia showed decreased brain volume, i.e., lower volumes of the right posterior cingulum and left entorhinal cortex and higher volumes of the ventricles, after prenatal exposure to higher maternal IL-8 levels (measured in assays from archived prenatal sera) [88], and volume loss in schizophrenia was found to be associated with an increased genetic risk for greater production of the immune marker IL-1β [89].
The peripheral benzodiazepine receptor is expressed on microglia and is upregulated in inflammation [90]. Positron emission tomography (PET) studies therefore used radiolabeled PK11195, a ligand for the receptor, to estimate microglial activation in the CNS and found that binding of PK11195 is higher in schizophrenia, indicating neuroinflammation [91,92,93]. Another PET study used DAA1106, another marker of microglial activation, to investigate the brains of people with chronic schizophrenia and found a correlation between binding of the marker and positive symptoms, as well as the duration of the disease [94].
6 Anti-Inflammatory Treatment in Schizophrenia
Treatment with anti-inflammatory drugs, such as celecoxib (a cyclooxygenase-2 [COX-2] inhibitor) and acetyl salicylic acid, has positive effects in schizophrenia and schizophrenia spectrum disorders [95, 96], providing support for an involvement of inflammation in the disease. In a 6-week prospective, double-blind, randomized controlled trial in patients receiving risperidone for an acute schizophrenic episode, outcome was significantly better in the add-on celecoxib group (n = 25) than in the add-on placebo group (n = 25) [97]. Cognition also improved significantly more in the celecoxib group [98]. A pooled analysis (n = 90) of the data from this and another 6-week study of celecoxib add-on to risperidone found that the duration of illness influenced the effects of celecoxib; i.e., the drug was beneficial in patients with a duration of illness <2 years but not superior to placebo in case of a longer illness duration [99] (see Fig. 14.1).
Comparison of disease duration on the effects of celecoxib add-on therapy to risperidone. Patients with a disease duration <2 years and celecoxib treatment had a better outcome than patients with a disease duration >2 years and placebo and both groups of patients with a disease duration of more than 2 years (results not statistically significant). Reprinted from [100] by permission of Oxford University Press and [101] Copyright © 2017 Karger Publishers, Basel, Switzerland. Cox celecoxib, PANSS Positive and negative syndrome scale
Other studies also provided support for the hypothesis that duration of illness is an important factor in the efficacy of anti-inflammatory treatment in schizophrenia. In a 6-week study of celecoxib add-on treatment in patients with first-manifestation schizophrenia being treated with amisulpride, the Positive and Negative Syndrome Scale (PANSS) positive, negative, total, and general psychopathology scores improved more in the celecoxib add-on group than in the placebo add-on group [102]. However, an 8-week double-blind study comparing celecoxib and placebo augmentation in continuously ill outpatients with schizophrenia receiving stable antipsychotic treatment found no benefit of celecoxib [103]. In addition, a meta-analysis of eight studies (six of celecoxib and two of acetylsalicylic acid) found significant effects in first-episode but not chronic schizophrenia [104].
A possible explanation for the importance of the duration of illness for the efficacy of anti-inflammatory agents may be neuroprogression (Müller 2017). We know from studies of first- and second-generation antipsychotics that the efficacy of these treatments is worse in chronic schizophrenia than in acute schizophrenia. However, so far anti-inflammatory treatment in schizophrenia has been studied for a maximum of 8 weeks (see above). Furthermore, short-term anti-inflammatory treatment also has poor efficacy in chronic inflammatory diseases. Therefore, longer studies are needed to evaluate anti-inflammatory treatment in chronic schizophrenia [105].
Studies are also needed to investigate potential predictors of treatment response to anti-inflammatory treatment. Earlier studies found that a higher amount of inflammation is associated with worse response to antipsychotics [106,107,108,109]. The question remains open whether higher levels of inflammation predict a better outcome to anti-inflammatory treatment, as was shown for anti-TNF treatment and celecoxib in major depression [28, 110]. So far, no immune-related predictive markers for anti-inflammatory treatment have been identified.
7 Other Potential Inflammation-Related Treatments in Schizophrenia
As mentioned earlier, microglia play a role in CNS inflammation, and CNS inflammation is hypothesized to be involved in schizophrenia. Thus, studies have examined whether agents that can cross the blood-brain barrier and inhibit microglia activation may be useful in schizophrenia. One such drug is the antibiotic minocycline. Minocycline was studied in animal models of schizophrenia, where it was shown to have positive effects on cognition [111]. In a double-blind, placebo-controlled study, add-on minocycline improved negative symptoms of schizophrenia [112, 113]. In addition, case reports described positive effects on the overall symptom spectrum [114].
Studies have also found some positive effects of other anti-inflammatory substances, such as acetylcysteine and omega-3 fatty acids [115] and interferon-gamma, a cytokine that stimulates the monocytic type 1 immune response [116]. Interferon-gamma may not be a viable treatment option, though, because it can have adverse effects on the immune system and is thus probably a “double-edged sword” in psychiatric diseases, as it is in cancer [117].
Monoclonal antibodies to pro-inflammatory cytokines have also been proposed as a potential treatment for schizophrenia, and treatment appears to be feasible and potentially efficacious, warranting further research [118].
8 Conclusion
In the context of research on the immune system and inflammation, it is important to note that drug treatment, smoking, stress levels, sleep patterns, etc., can affect results. Nevertheless, research appears to support a role of immunological and inflammatory processes in the pathogenesis of schizophrenia. Data have been obtained from a range of approaches, including studies on the role of proinflammatory cytokines in the disease; the effects of cytokines on tryptophan/kynurenine metabolism and glutamatergic neurotransmission; the binding of markers of inflammation in imaging studies; genetics; and the effects of anti-inflammatory drugs. Further research is required, particularly into a potential association of inflammation with volume loss in the CNS and the importance of the duration of illness for treatment outcome. However, findings so far, in particular on the positive effects of anti-inflammatory treatment in schizophrenia, are encouraging.
References
Hohlfeld R, Kerschensteiner M, Meinl E. Dual role of inflammation in CNS disease. Neurology. 2007;68:S58–63; discussion S91–6
Kerschensteiner M, Meinl E, Hohlfeld R. Neuro-immune crosstalk in CNS diseases. Neuroscience. 2009;158:1122–32.
Elkjaer ML, Frisch T, Reynolds R, et al. Molecular signature of different lesion types in the brain white matter of patients with progressive multiple sclerosis. Acta Neuropathol Commun. 2019;7:205.
Meinl E, Krumbholz M, Derfuss T, et al. Compartmentalization of inflammation in the CNS: a major mechanism driving progressive multiple sclerosis. J Neurol Sci. 2008;274:42–4.
Hanson DR, Gottesman II. Theories of schizophrenia: a genetic-inflammatory-vascular synthesis. BMC Med Genet. 2005;6:7.
Anderson G, Berk M, Dodd S, et al. Immuno-inflammatory, oxidative and nitrosative stress, and neuroprogressive pathways in the etiology, course and treatment of schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiatry. 2013;42:1–4.
Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996;19:312–8.
van Dam AP. Diagnosis and pathogenesis of CNS lupus. Rheumatol Int. 1991;11:1–11.
Dantzer R. Cytokine-induced sickness behavior: where do we stand? Brain Behav Immun. 2001;15:7–24.
Cavaillon JM. Pro-versus anti-inflammatory cytokines: myth or reality. Cell Mol Biol (Noisy-le-Grand). 2001;47:695–702.
Perry VH. Stress primes microglia to the presence of systemic inflammation: implications for environmental influences on the brain. Brain Behav Immun. 2007;21:45–6.
Godbout JP, Johnson RW. Age and neuroinflammation: a lifetime of psychoneuroimmune consequences. Immunol Allergy Clin N Am. 2009;29:321–37.
Cunningham C, Wilcockson DC, Campion S, et al. Central and systemic endotoxin challenges exacerbate the local inflammatory response and increase neuronal death during chronic neurodegeneration. J Neurosci. 2005;25:9275–84.
Sparkman NL, Johnson RW. Neuroinflammation associated with aging sensitizes the brain to the effects of infection or stress. Neuroimmunomodulation. 2008;15:323–30.
Frank MG, Baratta MV, Sprunger DB, et al. Microglia serve as a neuroimmune substrate for stress-induced potentiation of CNS pro-inflammatory cytokine responses. Brain Behav Immun. 2007;21:47–59.
Schedlowski M, Pacheco-Lopez G. The learned immune response: Pavlov and beyond. Brain Behav Immun. 2010;24:176–85.
Furukawa H, del Rey A, Monge-Arditi G, et al. Interleukin-1, but not stress, stimulates glucocorticoid output during early postnatal life in mice. Ann N Y Acad Sci. 1998;840:117–22.
Krusche J, Basse S, Schaub B. Role of early life immune regulation in asthma development. Semin Immunopathol. 2020;42:29–42.
Zhou D, Kusnecov AW, Shurin MR, et al. Exposure to physical and psychological stressors elevates plasma interleukin 6: relationship to the activation of hypothalamic-pituitary-adrenal axis. Endocrinology. 1993;133:2523–30.
Muller N, Krause D, Barth R, et al. Childhood adversity and current stress are related to pro- and anti-inflammatory cytokines in major depression. J Affect Disord. 2019;253:270–6.
Nair A, Bonneau RH. Stress-induced elevation of glucocorticoids increases microglia proliferation through NMDA receptor activation. J Neuroimmunol. 2006;171:72–85.
Lovelock DF, Deak T. Acute stress imposed during adolescence yields heightened anxiety in Sprague Dawley rats that persists into adulthood: sex differences and potential involvement of the medial amygdala. Brain Res. 2019;1723:146392.
Korte SM, Straub RH. Fatigue in inflammatory rheumatic disorders: pathophysiological mechanisms. Rheumatology (Oxford). 2019;58:v35–50.
Anisman H, Merali Z. Cytokines, stress and depressive illness: brain-immune interactions. Ann Med. 2003;35:2–11.
Hayley S, Wall P, Anisman H. Sensitization to the neuroendocrine, central monoamine and behavioural effects of murine tumor necrosis factor-alpha: peripheral and central mechanisms. Eur J Neurosci. 2002;15:1061–76.
Zubin J, Spring B. Vulnerability: a new view of schizophrenia. J Abnorm Psychol. 1977;86:103–26.
Khandaker GM, Zimbron J, Lewis G, et al. Prenatal maternal infection, neurodevelopment and adult schizophrenia: a systematic review of population-based studies. Psychol Med. 2013;43:239–57.
Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiat. 2013;70:31–41.
Muller N, Schwarz MJ. Immune system and schizophrenia. Curr Immunol Rev. 2010;6:213–20.
Potvin S, Stip E, Sepehry AA, et al. Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry. 2008;63:801–8.
Korschenhausen DA, Hampel HJ, Ackenheil M, et al. Fibrin degradation products in post mortem brain tissue of schizophrenics: a possible marker for underlying inflammatory processes. Schizophr Res. 1996;19:103–9.
Wildenauer DB, Korschenhausen D, Hoechtlen W, et al. Analysis of cerebrospinal fluid from patients with psychiatric and neurological disorders by two-dimensional electrophoresis: identification of disease-associated polypeptides as fibrin fragments. Electrophoresis. 1991;12:487–92.
Muller N, Schwarz MJ. Neuroimmune-endocrine crosstalk in schizophrenia and mood disorders. Expert Rev Neurother. 2006;6:1017–38.
Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–709.
Miller BJ, Culpepper N, Rapaport MH. C-reactive protein levels in schizophrenia: a review and meta-analysis. Clin Schizophr Relat Psychoses. 2014;7:223–30.
Wang AK, Miller BJ. Meta-analysis of cerebrospinal fluid cytokine and tryptophan catabolite alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder, and depression. Schizophr Bull. 2017.
Muller N, Bechter K. The mild encephalitis concept for psychiatric disorders revisited in the light of current psychoneuroimmunological findings. Neurol Psychiatry Brain Res. 2013;19:87–101.
Carlsson A. The current status of the dopamine hypothesis of schizophrenia. Neuropsychopharmacology. 1988;1:179–86.
Ling ZD, Potter ED, Lipton JW, et al. Differentiation of mesencephalic progenitor cells into dopaminergic neurons by cytokines. Exp Neurol. 1998;149:411–23.
Kabiersch A, Furukawa H, del Rey A, et al. Administration of interleukin-1 at birth affects dopaminergic neurons in adult mice. Ann N Y Acad Sci. 1998;840:123–7.
Potter ED, Ling ZD, Carvey PM. Cytokine-induced conversion of mesencephalic-derived progenitor cells into dopamine neurons. Cell Tissue Res. 1999;296:235–46.
Jarskog LF, Xiao H, Wilkie MB, et al. Cytokine regulation of embryonic rat dopamine and serotonin neuronal survival in vitro. Int J Dev Neurosci. 1997;15:711–6.
Winter C, Djodari-Irani A, Sohr R, et al. Prenatal immune activation leads to multiple changes in basal neurotransmitter levels in the adult brain: implications for brain disorders of neurodevelopmental origin such as schizophrenia. Int J Neuropsychopharmacol. 2009;12:513–24.
Felger JC, Mun J, Kimmel HL, et al. Chronic interferon-alpha decreases dopamine 2 receptor binding and striatal dopamine release in association with anhedonia-like behavior in nonhuman primates. Neuropsychopharmacology. 2013;38:2179–87.
Muller N, Ackenheil M. Immunoglobulin and albumin content of cerebrospinal fluid in schizophrenic patients: relationship to negative symptomatology. Schizophr Res. 1995;14:223–8.
Nikolich-Zugich J. Ageing and life-long maintenance of T-cell subsets in the face of latent persistent infections. Nat Rev Immunol. 2008;8:512–22.
Stone TW. Neuropharmacology of quinolinic and kynurenic acids. Pharmacol Rev. 1993;45:309–79.
Muller N, Schwarz MJ. The immunological basis of glutamatergic disturbance in schizophrenia: towards an integrated view. J Neural Transm Suppl. 2007:269–80.
Muller N, Myint AM, Schwarz MJ. Kynurenine pathway in schizophrenia: pathophysiological and therapeutic aspects. Curr Pharm Des. 2011;17:130–6.
Steiner J, Walter M, Glanz W, et al. Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: specific relevance of IgG NR1a antibodies for distinction from N-methyl-D-aspartate glutamate receptor encephalitis. JAMA Psychiat. 2013;70:271–8.
Vincent A, Bien CG. Anti-NMDA-receptor encephalitis: a cause of psychiatric, seizure, and movement disorders in young adults. Lancet Neurol. 2008;7:1074–5.
Erhardt S, Blennow K, Nordin C, et al. Kynurenic acid levels are elevated in the cerebrospinal fluid of patients with schizophrenia. Neurosci Lett. 2001;313:96–8.
Linderholm KR, Skogh E, Olsson SK, et al. Increased levels of kynurenine and kynurenic acid in the CSF of patients with schizophrenia. Schizophr Bull. 2012;38:426–32.
Schwarcz R, Rassoulpour A, Wu HQ, et al. Increased cortical kynurenate content in schizophrenia. Biol Psychiatry. 2001;50:521–30.
Sathyasaikumar KV, Stachowski EK, Wonodi I, et al. Impaired kynurenine pathway metabolism in the prefrontal cortex of individuals with schizophrenia. Schizophr Bull. 2011;37:1147–56.
Olsson SK, Andersson AS, Linderholm KR, et al. Elevated levels of kynurenic acid change the dopaminergic response to amphetamine: implications for schizophrenia. Int J Neuropsychopharmacol. 2009;12:501–12.
Condray R, Dougherty GG Jr, Keshavan MS, et al. 3-Hydroxykynurenine and clinical symptoms in first-episode neuroleptic-naive patients with schizophrenia. Int J Neuropsychopharmacol. 2011;14:756–67.
Myint AM, Schwarz MJ, Verkerk R, et al. Reversal of imbalance between kynurenic acid and 3-hydroxykynurenine by antipsychotics in medication-naive and medication-free schizophrenic patients. Brain Behav Immun. 2011;25:1576–81.
Ceresoli-Borroni G, Rassoulpour A, Wu HQ, et al. Chronic neuroleptic treatment reduces endogenous kynurenic acid levels in rat brain. J Neural Transm (Vienna). 2006;113:1355–65.
Buka SL, Tsuang MT, Torrey EF, et al. Maternal infections and subsequent psychosis among offspring. Arch Gen Psychiatry. 2001;58:1032–7.
Westergaard T, Mortensen PB, Pedersen CB, et al. Exposure to prenatal and childhood infections and the risk of schizophrenia: suggestions from a study of sibship characteristics and influenza prevalence. Arch Gen Psychiatry. 1999;56:993–8.
Meyer U, Feldon J. Prenatal exposure to infection: a primary mechanism for abnormal dopaminergic development in schizophrenia. Psychopharmacology. 2009;206:587–602.
Meyer U, Schwarz MJ, Muller N. Inflammatory processes in schizophrenia: a promising neuroimmunological target for the treatment of negative/cognitive symptoms and beyond. Pharmacol Ther. 2011;132:96–110.
Pearce BD. Schizophrenia and viral infection during neurodevelopment: a focus on mechanisms. Mol Psychiatry. 2001;6:634–46.
Buka SL, Cannon TD, Torrey EF, et al. Maternal exposure to herpes simplex virus and risk of psychosis among adult offspring. Biol Psychiatry. 2008;63:809–15.
Brown AS, Begg MD, Gravenstein S, et al. Serologic evidence of prenatal influenza in the etiology of schizophrenia. Arch Gen Psychiatry. 2004;61:774–80.
Brown AS, Cohen P, Greenwald S, et al. Nonaffective psychosis after prenatal exposure to rubella. Am J Psychiatry. 2000;157:438–43.
Sorensen HJ, Mortensen EL, Reinisch JM, et al. Association between prenatal exposure to bacterial infection and risk of schizophrenia. Schizophr Bull. 2009;35:631–7.
Babulas V, Factor-Litvak P, Goetz R, et al. Prenatal exposure to maternal genital and reproductive infections and adult schizophrenia. Am J Psychiatry. 2006;163:927–9.
Brown AS, Schaefer CA, Quesenberry CP Jr, et al. Maternal exposure to toxoplasmosis and risk of schizophrenia in adult offspring. Am J Psychiatry. 2005;162:767–73.
Boksa P. Maternal infection during pregnancy and schizophrenia. J Psychiatry Neurosci. 2008;33:183–5.
Gattaz WF, Abrahao AL, Foccacia R. Childhood meningitis, brain maturation and the risk of psychosis. Eur Arch Psychiatry Clin Neurosci. 2004;254:23–6.
Brown AS. The risk for schizophrenia from childhood and adult infections. Am J Psychiatry. 2008;165:7–10.
Dalman C, Allebeck P, Gunnell D, et al. Infections in the CNS during childhood and the risk of subsequent psychotic illness: a cohort study of more than one million Swedish subjects. Am J Psychiatry. 2008;165:59–65.
Yolken RH, Torrey EF. Viruses, schizophrenia, and bipolar disorder. Clin Microbiol Rev. 1995;8:131–45.
Leweke FM, Gerth CW, Koethe D, et al. Antibodies to infectious agents in individuals with recent onset schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2004;254:4–8.
Krause D, Matz J, Weidinger E, et al. The association of infectious agents and schizophrenia. World J Biol Psychiatry. 2010;11:739–43.
Brown AS, Hooton J, Schaefer CA, et al. Elevated maternal interleukin-8 levels and risk of schizophrenia in adult offspring. Am J Psychiatry. 2004;161:889–95.
Meehan C, Harms L, Frost JD, et al. Effects of immune activation during early or late gestation on schizophrenia-related behaviour in adult rat offspring. Brain Behav Immun. 2017;63:8–20.
Brown AS, Schaefer CA, Wyatt RJ, et al. Maternal exposure to respiratory infections and adult schizophrenia spectrum disorders: a prospective birth cohort study. Schizophr Bull. 2000;26:287–95.
Metcalf SA, Jones PB, Nordstrom T, et al. Serum C-reactive protein in adolescence and risk of schizophrenia in adulthood: a prospective birth cohort study. Brain Behav Immun. 2017;59:253–9.
Benros ME, Nielsen PR, Nordentoft M, et al. Autoimmune diseases and severe infections as risk factors for schizophrenia: a 30-year population-based register study. Am J Psychiatry. 2011;168:1303–10.
Benros ME, Mortensen PB, Eaton WW. Autoimmune diseases and infections as risk factors for schizophrenia. Ann N Y Acad Sci. 2012;1262:56–66.
Gogtay N, Lu A, Leow AD, et al. Three-dimensional brain growth abnormalities in childhood-onset schizophrenia visualized by using tensor-based morphometry. Proc Natl Acad Sci U S A. 2008;105:15979–84.
Steen RG, Mull C, McClure R, et al. Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies. Br J Psychiatry. 2006;188:510–8.
Job DE, Whalley HC, McIntosh AM, et al. Grey matter changes can improve the prediction of schizophrenia in subjects at high risk. BMC Med. 2006;4:29.
Chakos MH, Schobel SA, Gu H, et al. Duration of illness and treatment effects on hippocampal volume in male patients with schizophrenia. Br J Psychiatry. 2005;186:26–31.
Ellman LM, Deicken RF, Vinogradov S, et al. Structural brain alterations in schizophrenia following fetal exposure to the inflammatory cytokine interleukin-8. Schizophr Res. 2010;121:46–54.
Meisenzahl EM, Rujescu D, Kirner A, et al. Association of an interleukin-1beta genetic polymorphism with altered brain structure in patients with schizophrenia. Am J Psychiatry. 2001;158:1316–9.
Filiou MD, Banati RB, Graeber MB. The 18-kDa translocator protein as a CNS drug target: finding our way through the neuroinflammation fog. CNS Neurol Disord Drug Targets. 2017;16:990–9.
Versijpt JJ, Dumont F, Van Laere KJ, et al. Assessment of neuroinflammation and microglial activation in Alzheimer’s disease with radiolabelled PK11195 and single photon emission computed tomography. A pilot study. Eur Neurol. 2003;50:39–47.
van Berckel BN, Bossong MG, Boellaard R, et al. Microglia activation in recent-onset schizophrenia: a quantitative (R)-[11C]PK11195 positron emission tomography study. Biol Psychiatry. 2008;64:820–2.
Doorduin J, de Vries EF, Willemsen AT, et al. Neuroinflammation in schizophrenia-related psychosis: a PET study. J Nucl Med. 2009;50:1801–7.
Takano A, Arakawa R, Ito H, et al. Peripheral benzodiazepine receptors in patients with chronic schizophrenia: a PET study with [11C]DAA1106. Int J Neuropsychopharmacol. 2010;13:943–50.
Sommer IE, de Witte L, Begemann M, et al. Nonsteroidal anti-inflammatory drugs in schizophrenia: ready for practice or a good start? A meta-analysis. J Clin Psychiatry. 2012;73:414–9.
Laan W, Grobbee DE, Selten JP, et al. Adjuvant aspirin therapy reduces symptoms of schizophrenia spectrum disorders: results from a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2010;71:520–7.
Muller N, Riedel M, Scheppach C, et al. Beneficial antipsychotic effects of celecoxib add-on therapy compared to risperidone alone in schizophrenia. Am J Psychiatry. 2002;159:1029–34.
Muller N, Riedel M, Schwarz MJ, et al. Clinical effects of COX-2 inhibitors on cognition in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2005;255:149–51.
Müller N, Riedel M, Dehning S, et al. Is the therapeutic effect of celecoxib in schizophrenia depending from duration of disease? Neuropsychopharmacology. 2004;29:S176.
Muller N. Inflammation in schizophrenia: Pathogenetic aspects and therapeutic considerations. Schizophr Bull. 2018;44:973–82.
Müller N. Neuroprogression in schizophrenia and psychotic disorder: the possible role of inflammation. In: Halaris A, Leonard BE, editors. Neuroprogression in psychiatric disorders, Modern Trends Pharmacopsychiatry. Basel: Karger; 2017.
Muller N. COX-2 inhibitors as antidepressants and antipsychotics: clinical evidence. Curr Opin Investig Drugs. 2010;11:31–42.
Rapaport MH, Delrahim KK, Bresee CJ, et al. Celecoxib augmentation of continuously ill patients with schizophrenia. Biol Psychiatry. 2005;57:1594–6.
Nitta M, Kishimoto T, Muller N, et al. Adjunctive use of nonsteroidal anti-inflammatory drugs for schizophrenia: a meta-analytic investigation of randomized controlled trials. Schizophr Bull. 2013;39:1230–41.
Akhondzadeh S, Tabatabaee M, Amini H, et al. Celecoxib as adjunctive therapy in schizophrenia: a double-blind, randomized and placebo-controlled trial. Schizophr Res. 2007;90:179–85.
Lin A, Kenis G, Bignotti S, et al. The inflammatory response system in treatment-resistant schizophrenia: increased serum interleukin-6. Schizophr Res. 1998;32:9–15.
McAllister CG, van Kammen DP, Rehn TJ, et al. Increases in CSF levels of interleukin-2 in schizophrenia: effects of recurrence of psychosis and medication status. Am J Psychiatry. 1995;152:1291–7.
Mondelli V, Ciufolini S, Belvederi Murri M, et al. Cortisol and inflammatory biomarkers predict poor treatment response in first episode psychosis. Schizophr Bull. 2015;41:1162–70.
Zhang XY, Zhou DF, Cao LY, et al. Cortisol and cytokines in chronic and treatment-resistant patients with schizophrenia: association with psychopathology and response to antipsychotics. Neuropsychopharmacology. 2005;30:1532–8.
Abbasi SH, Hosseini F, Modabbernia A, et al. Effect of celecoxib add-on treatment on symptoms and serum IL-6 concentrations in patients with major depressive disorder: randomized double-blind placebo-controlled study. J Affect Disord. 2012;141:308–14.
Mizoguchi H, Takuma K, Fukakusa A, et al. Improvement by minocycline of methamphetamine-induced impairment of recognition memory in mice. Psychopharmacology (Berl). 2008;196:233–41.
Levkovitz Y, Mendlovich S, Riwkes S, et al. A double-blind, randomized study of minocycline for the treatment of negative and cognitive symptoms in early-phase schizophrenia. J Clin Psychiatry. 2010;71:138–49.
Chaudhry IB, Hallak J, Husain N, et al. Minocycline benefits negative symptoms in early schizophrenia: a randomised double-blind placebo-controlled clinical trial in patients on standard treatment. J Psychopharmacol. 2012;26:1185–93.
Ahuja N, Carroll BT. Possible anti-catatonic effects of minocycline in patients with schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiatry. 2007;31:968–9.
Sommer IE, van Westrhenen R, Begemann MJ, et al. Efficacy of anti-inflammatory agents to improve symptoms in patients with schizophrenia: an update. Schizophr Bull. 2014;40:181–91.
Gruber L, Bunse T, Weidinger E, et al. Adjunctive recombinant human interferon gamma-1b for treatment-resistant schizophrenia in 2 patients. J Clin Psychiatry. 2014;75:1266–7.
Zaidi MR, Merlino G. The two faces of interferon-gamma in cancer. Clin Cancer Res. 2011;17:6118–24.
Miller BJ, Buckley PF. The case for adjunctive monoclonal antibody immunotherapy in schizophrenia. Psychiatr Clin North Am. 2016;39:187–98.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
The work was supported by the foundation “Immunität und Seele.”
Conflict of Interest
None to declare.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Müller, N. (2021). Inflammation and Immunity in Schizophrenia. In: Berk, M., Leboyer, M., Sommer, I.E. (eds) Immuno-Psychiatry. Springer, Cham. https://doi.org/10.1007/978-3-030-71229-7_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-71229-7_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71228-0
Online ISBN: 978-3-030-71229-7
eBook Packages: MedicineMedicine (R0)