Abstract
Primary immunodeficiencies (PIDs) constitute a rapidly expanding field. As of 2019 there are 430 distinct human inborn errors of immunity listed in the current IUIS classification (International Union of Immunological Societies) (Tangye et al., J Clin Immunol 40:24–64, 2020).
Within the last 20 years, hundreds of genetic defects underlying PID have been identified. Historically, these were classified into humoral immunodeficiencies, on the one hand, and cellular immunodeficiencies, on the other hand. However, as our understanding has been evolving, these categories have become increasingly complex: genetic defects, for example, can affect multiple cell populations simultaneously, may affect communication between different cell types, may constitute failure of the bone marrow or other compartments to support and regulate certain cell populations, or may be associated with syndromic features. Within this chapter, we aim to provide an overview over the basic concepts of genetics as well as genetics of cellular immunodeficiencies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
Primary immunodeficiencies (PIDs) constitute a rapidly expanding field. As of 2019 there are 430 distinct human inborn errors of immunity listed in the current IUIS classification (International Union of Immunological Societies) [1].
Within the last 20 years, hundreds of genetic defects underlying PID have been identified. Historically, these were classified into humoral immunodeficiencies, on the one hand, and cellular immunodeficiencies, on the other hand. However, as our understanding has been evolving, these categories have become increasingly complex: genetic defects, for example, can affect multiple cell populations simultaneously, may affect communication between different cell types, may constitute failure of the bone marrow or other compartments to support and regulate certain cell populations, or may be associated with syndromic features. Within the IUIS classification, this is illustrated by the notion to classify PIDs into ten general categories, each with numerous distinct subcategories [1].
2.2 Importance of Establishing a Genetic Diagnosis
Establishing a genetic diagnosis is essential for confirming a suspected diagnosis and counseling PID patients and their family members regarding treatment options, prognosis, as well as family planning. The in-depth molecular characterization of underlying genetic defects and involved pathways has greatly advanced our knowledge of immunology, in general, and furthered our understanding of specific molecular principles of infection control but also of the termination of immune responses once the infection is controlled. For invasive therapies, such as hematopoietic stem cell transplantation or gene therapy approaches, the prior identification of a molecular defect is an essential prerequisite. A better understanding of defective or involved pathways may furthermore help to identify novel therapeutic targets, both for aiding patients with primary immunodeficiencies and for the development of novel immunosuppressive or antiproliferative drugs used in autoimmune diseases and malignancies, as experienced with JAK inhibitors or the BTK antagonist ibrutinib [2].
2.3 A Brief History of Genetics
The origins of genetics can be found within Augustinian monk Gregor Mendel’s experiments on plant hybridization published in 1866, in which he described his observations on the heritability of different traits in peas [3]. However, it took until the early 1900s for the chromosomal theory of heredity to develop, combining Mendel’s laws with the idea of chromosomes as the carriers of hereditary information [4]. Nucleic acid was first discovered in 1869 by the Swiss doctor Friedrich Miescher, though its significance was unclear at the time. It took until 1944 for Avery, McLeod, and McCarthy to show that, in fact, DNA constitutes the genetic material of a cell [5]. In 1953 Watson and Crick famously discovered the structure of DNA and are since often hailed as the founders of modern genetics [6]. Meanwhile the notion of gene mutations as local alterations of a chromosome was derived in the 1920s from Hermann J. Muller’s mutagenesis experiments on drosophila. The first description of a human mutation is generally attributed to V.M. Ingram, who described an amino acid exchange as a cause for sickle cell anemia in 1956 [7]. The first molecular defect underlying a primary immunodeficiency was identified by E.R. Giblett with ADA-SCID in 1972 [8], when she described two young girls with recurrent infections without measurable adenosine deaminase enzyme activity in their erythrocytes while their parents had approximately half-normal levels, from which an autosomal recessive inheritance pattern was correctly assumed.
Initial sequencing approaches constituted protein sequencing methods, allowing for the identification of the amino acid sequence of proteins from the 1950s on. At this time the exact mechanisms of transcription and translation had not yet been identified. Subsequently early RNA sequencing methods were developed, while the classical Sanger DNA sequencing method of dideoxy-chain termination was finally published in 1977 by Fred Sanger [9]. The era of PID genetics finally started in the early 1990s with the discovery of BTK mutations as the genetic cause of X-linked agammaglobulinemia more than 40 years after Bruton’s first report of the disease in 1952 [10, 11]. Since then, advances in technology including automated sequencing and next-generation sequencing have enabled a rapid growth of the field with numerous exciting discoveries.
2.4 Patterns of Inheritance
Human inborn errors of immunity constitute by definition germline monogenic defects and thus follow Mendelian rules of inheritance. Specifically, monogenic defects can follow an autosomal dominant, autosomal recessive, or X-linked pattern of inheritance.
In the case of an autosomal dominant mode of inheritance, only one affected allele is sufficient to cause disease (i.e., a heterozygous mutation). Males and females will be affected at equal frequency, and the disease will not skip any generations. Autosomal dominant mutations can affect the expression and function of the gene product in different ways, namely, may cause haploinsufficiency, may result in gain of function, or may have a dominant negative effect. Haploinsufficiency arises when a single wild-type allele will not lead to sufficient expression of the gene product, usually a protein, and thus leads to a phenotypic effect. Gain-of-function mutations lead to an increased level of activity, novel function, or prolonged life span of the gene product, thus leading to a gain of function. Gain-of-function mutations are generally less common than loss-of-function mutations. Dominant negative mutations lead to a gene product, which will act antagonistically to the wild-type gene product within the same cell, also referred to as antimorphic mutations. Dominant negative mutations will thus reduce effective expression or function by greater than 50%. A dominant negative effect commonly arises in proteins, which form polymeric structures.
In autosomal recessive inheritance, two copies of an affected allele are required for an individual to express the disease phenotype (i.e., a homozygous or compound heterozygous mutation). Males and females will be similarly affected. Typically, both parents are heterozygous carriers, and statistically one-fourth of their children will be affected. In consanguineous unions, conditions with autosomal recessive inheritance will appear with an increased frequency due to common ancestry alleles. Autosomal recessive mutations generally result in loss of function.
In the case of X-linked inheritance usually only males are affected as they only possess one gene copy. Transmission occurs through female carriers, who are mostly phenotypically unaffected (no father-to-son transmission). The disease often occurs in multiple generations.
Whereas human inborn errors of immunity are generally defined through an underlying germline monogenic defect, some primary immunodeficiencies seem to have a complex pattern of inheritance, also referred to as polygenic inheritance. In particular, IgA deficiency and some forms of common variable immunodeficiency, both, however, not constituting cellular immunodeficiencies, seem to follow a complex inheritance pattern with an increased incidence in some families. The genetics of antibody deficiency was described in detail in the first book of this series, Humoral Primary Immunodeficiencies [12]. A list with explanations of genetic terms can be found in (Table 2.1).
2.5 Germline Versus Somatic Mutations
A germline mutation is defined as a heritable mutation, which occurred originally in a germ cell or the zygote at single-cell stage, and thus will be present in all cells in the offspring, including the germ cells. Thus, a germline mutation can be passed on from generation to generation.
In contrast to germline mutations, somatic mutations occur when a mutation arises postzygotically, which will lead to mosaicism. The phenotype of mosaicism depends upon the developmental stage at which the mutation arises. A mutation in early embryonic development will likely affect many different tissues. If only somatic cells are affected, this will be called somatic mosaicism. Somatic mosaicism will not be transmitted to the next generation. If both somatic cells and germ cells are affected, this is defined as gonosomal mosaicism, which will cause symptoms depending on the affected somatic tissues and may be transmitted on to the next generation. In contrast, gonadal mosaicism affects only the germ cells and, thus, typically has no phenotype in the carrier but will be transmitted to the offspring as a germline mutation. Somatic mutations are generally considered phenocopies of PID within the IUIS classification, although we want to point out that mosaicism may in theory cause a phenotype indistinguishable from germline mutations and, if including the germ cells, can lead to full germline mutations in the offspring. Mosaicism should be suspected in case of marked intergenerational phenotypical differences, unexpected intrafamilial reoccurrence in children of seemingly healthy parents without mutation in Sanger sequencing, or unequal height/intensity of sequencing peaks in Sanger chromatograms [13].
2.6 Types of Mutations
Mutations can be classified either by their impact on DNA or by their impact on the respective protein.
Regarding the impact of a mutation on the DNA, a mutation can further be classified as a substitution, i.e., one or multiple bases are substituted by an equal number of other bases; an insertion, where additional bases are gained; or a deletion, i.e., a loss of bases. Inversions and translocations may also be listed in this category and constitute structural rearrangements of DNA. An inversion is defined as an end-to-end reversion of a piece of DNA, whereas a translocation describes the integration of a piece of DNA or a piece of a chromosome at another position. Translocations can be balanced, i.e., an even exchange of DNA, or unbalanced, thus leading to loss or gain of genetic material in daughter cells.
Regarding the impact on the resulting protein, mutations can be classified as silent mutations, missense mutations, or frameshift mutations. A silent mutation is a mutation which does not lead to a change in the amino acid sequence of the protein. A missense mutation is defined as an exchange of a single amino acid within the protein sequence. A nonsense mutation constitutes a change of one amino acid within the protein into a premature stop codon. In contrast, a readthrough mutation constitutes the change of a stop codon into an amino acid. A frameshift mutation arises from a deletion or insertion of bases in the DNA sequence of a number not divisible by three, thus changing the reading frame as the genetic code is organized in base triplets, i.e., codons, each coding for a specific amino acid. Also mutations outside of the coding DNA sequence may have an impact on the protein. Splice site mutations have long been recognized as disease causing; however, deep intronic mutations may have an impact on the protein sequence or expression through inclusion of pseudo-exons due to creation of alternative splice sites or may affect expression when located within regulatory regions, such as promoter or enhancer sequences [14].
2.7 Pleiotropy of PIDs
Many different genetic defects have overlapping phenotypes. Genetic heterogeneity can generally be classified into allelic heterogeneity and locus heterogeneity. Allelic heterogeneity is defined as different mutations (alleles) within the same gene producing a similar phenotype. In contrast, locus heterogeneity implies that a similar phenotype may be caused by mutations in different genes. Similarly, the term genocopy refers to a genotype or mutation resulting in a similar phenotype to another genotype or mutation at a different locus. In contrast, a phenocopy is defined as environmental factors producing the same phenotype as a specific genetic mutation, thus mimicking the phenotype [15]. A phenocopy by definition is not a genetic trait and thus is not hereditary in a strict Mendelian sense, though epigenetic changes may count as phenocopies and can be passed on to daughter cells.
Differences in phenotype despite the same genotype may be caused by a variable expressivity of a trait or phenotype. Expressivity thus constitutes a measure for the extent of phenotypic expression. In contrast, penetrance refers to the proportion of individuals with a certain genotype, who exhibit the associated phenotype. With complete penetrance all individuals with a certain genotype, i.e., a certain mutation, show the associated symptoms/trait, whereas reduced penetrance means that some individuals who carry a genetic defect may in fact be phenotypically healthy.
2.8 Sequencing Technologies
In the past Sanger sequencing constituted the gold standard for genetic diagnostics. Depending on the clinical phenotype, the most likely candidate genes needed to be identified and sequenced sequentially exon by exon. However, this constituted a laborious time- and resource-consuming process and often did not lead to success due to atypical presentations and obvious limitations due to being a hypothesis-driven approach (i.e., the candidate gene needed to be known). In recent years, great advances have been made with the help of next-generation sequencing techniques, which have substituted Sanger sequencing in the diagnostic workup process of PIDs in many places.
Next-generation sequencing technologies allow for the simultaneous massive parallel sequencing of thousands of genes at dramatically reduced costs. With many novel sequencing techniques, several patients can be multiplexed and thus sequenced in the same sequencing run. The introduction of next-generation sequencing methods thus has greatly facilitated the identification of novel genetic defects, which is reflected in the rising number of novel defects described every year. In general, next-generation sequencing methods consist of the following three steps: The first step is the preparation of a library, in which the DNA is fragmented (usually through either restriction enzymes or sonication) and fragments are ligated with custom linkers or sequencing adapters. In panel and exome sequencing, there is an amplification step relying on clonal amplification/PCR, whereas whole genome sequencing, in general, does not necessitate amplification. Lastly, the fragments are sequenced. Depending on the sequencer, different technologies are employed for this step.
Next-generation sequencing approaches can be divided into panel sequencing approaches, whole exome sequencing, and whole genome sequencing, each with their distinct advantages and disadvantages.
Gene panel sequencing provides a high coverage of sequenced regions, which is one of its distinct advantages over whole exome and especially whole genome sequencing and is crucial to reduce errors, particularly in a diagnostic setting. Since less regions are sequenced, panel sequencing results in less variants of unknown significance. Limitations include that panel sequencing is a biased approach (variants can only be detected in sequenced regions, i.e., in identified target genes), preassembled panels are rigid and may not contain all genes of interest, and continuous redesigning and revalidation of the panel may be necessary.
Whole exome sequencing constitutes an unbiased approach, allowing the identification of novel defects. However, in practice, complete coverage of all coding exons is impracticable, and a significant proportion of regions will have a low read depth, necessitating resequencing for use in a clinical context.
Whole genome sequencing is the only method which also allows for the identification of deep intronic variants. However, data interpretation is still difficult and hampered by detection of vast numbers of variants of unknown significance.
All next-generation sequencing approaches necessitate bioinformatic analysis in order to align the sequenced fragments correctly to the reference genome and identify variants. Detected variants subsequently need to be compared with reference databases and evaluated for harmfulness through either prediction tools or experimental validation.
2.9 Interpretation of Sequencing Results
A drawback of the novel sequencing technologies is the detection of numerous variants of unclear significance. Sometimes it may be difficult to establish whether a variant is in fact disease causing or not, which may pose clinical as well as at times ethical and legal challenges.
Sequence variants are common, often benign, and the source of genetic variation. In fact, each genome is thought to have approximately 4 million sequence variants, which mostly constitute single-nucleotide polymorphisms (SNP, by definition frequency above 1%) but may also encompass, e.g., structural variants [16]. The relative occurrence of sequence variants varies between regions and genes, with important functional domains of genes often showing evolutionary conservation through many different species.
To establish whether a variant may be benign or disease causing, several methods can be employed. Firstly, to establish whether a variant has been reported before or is listed as a SNP, bioinformatic analysis including queries of population databases can be employed; useful resources include, e.g., dbSNP, Human Gene Mutation Database (HGMD), ClinVar, and gnomAD (formerly ExAc) [17,18,19,20]. If the variant has not been reported as disease associated before, in silico prediction tools, such as CADD, PolyPhen2, or SIFT, may provide helpful insights [21,22,23]. Additionally, genetic analysis of affected and unaffected family members as well as functional testing including cloning of the mutation may be performed but constitute laborious processes.
To facilitate the classification and interpretation of sequencing results, the American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology have published recommendations [24]. In particular, they recommend to classify variants into the following categories: (i) pathogenic, (ii) likely pathogenic, (iii) uncertain significance, (iv) likely benign, or (v) benign. Furthermore, they advise to use a standardized nomenclature of variants, as published and regularly updated by the Human Genome Variation Society (HGVS) [25].
As a general rule, variants should always be described at the most basic level possible, which will normally be the DNA level (e.g., c.1650C>T, where “>” is used to label a base substitution and “del,” “ins,” and “dup” label deletions, insertions, and duplications, respectively). However, in the case of, e.g., frameshifts, the protein sequence may be used, such as p.R908Kfs*15, indicating that the variant leads to an amino acid exchange from R to K in position 908 with a subsequent frameshift (fs) and termination after 15 amino acids. Importantly, a reference sequence or transcript should always be provided. The online tool Mutalyzer (https://mutalyzer.nl) provides both a name generator producing a valid HGVS variant description and a syntax checker to assess existing variant descriptions regarding compatibility with HGVS nomenclature [26].
Furthermore, variants described in only a single patient should be taken with caution. Casanova et al. published criteria aiding the decision whether data establish a causal relationship between phenotype and genotype for this case [27]. In brief, the variant in question should not occur in healthy individuals, there need to be experimental data indicating that the gene product is altered in function or expression by the variant, and a causal relationship between genotype and phenotype must be confirmed in an animal model or a relevant cellular phenotype.
2.10 Genetics of Combined Immunodeficiencies
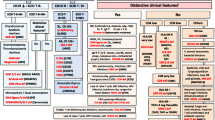
Combined immunodeficiencies can be classified into severe combined immunodeficiencies (SCID) and combined immunodeficiencies less severe than SCID (CID). In total, the current IUIS classification lists a total number of 50 disorders caused by 58 distinct genetic defects.
Clinically, SCID defects can be classified by presence or absence of T, B, and NK cells. Genetically, SCID defects can be grouped by pathogenic mechanism into VDJ recombination and T cell receptor defects, cytokine signaling defects, defects with toxic metabolite accumulation, and defects with defective survival of hematopoietic precursors. SCID usually follows an autosomal recessive or X-linked pattern of inheritance.
VDJ recombination defects constitute mainly enzymatic defects, which are inherited in an autosomal recessive pattern and include RAG1/RAG2 deficiency, DNA cross-link repair enzyme 1c (DCLRE1C)/Artemis deficiency, nonhomologous end-joining enzyme (NHEJ1)/Cernunnos deficiency, DNA ligase IV (LIG4) deficiency, and DNA PKcs deficiency (PRKDC). Recombination-activating proteins (RAG) 1 and 2 initiate recombination of immunoglobulin and T cell receptor genes in B and T cells to diversify the repertoire through rearrangement of variable (V), diversity (D), and joining (J) segments. Failure to induce VDJ recombination will lead to apoptosis. It is essential that the induced double-strand breaks subsequently are repaired correctly to produce a recombined continuous DNA strand. Defects in nonhomologous end-joining DNA repair mechanisms, such as mutations in DCLRE1C, DNA PKcs, NHEJ1, and LIG4, will thus lead to SCID with increased radiosensitivity as DNA damage cannot be sufficiently repaired. Other DNA repair defects leading to radiosensitivity and immunodeficiency regularly include syndromic features and thus belong to syndromic combined immunodeficiencies.
T cell receptor defects affecting CD3D, CD3E, and CD3Z lead to T-B+NK+ SCID, whereas CD3G deficiency leads to combined immunodeficiency, generally less profound than SCID. Also, CD45 deficiency may be counted toward the T cell receptor defects in that CD45 encodes a receptor-associated tyrosine phosphatase essential for the activation of T cells through the T cell receptor, its deficiency also leads to T-B + NK+ SCID. T cell receptor defects generally follow an autosomal recessive inheritance pattern.
Cytokine signaling defects causing SCID include common gamma chain deficiency (IL2RG), JAK3 deficiency, and IL7Rα deficiency (IL7RA). The common gamma chain is a receptor chain shared by the receptors of interleukins IL2, IL4, IL7, IL9, IL15, and IL21. As IL7 and IL15 are essential in the development of T and NK cells, common gamma chain deficiency leads to T-B + NK- SCID. Since the IL2RG gene is located on the X chromosome, common gamma chain deficiency follows an X-linked inheritance pattern and thus is also referred to as X-SCID. The Janus kinase 3 mediates the signal transduction downstream of common gamma chain cytokines; therefore, deficiency also leads to T-B+NK− SCID, however, following an autosomal recessive inheritance pattern. IL7 signaling is essential in the early development of lymphocytes but also proliferation and survival of T cells peripherally; thus, deficiency of the IL7 receptor alpha chain also causes T-B+NK+ SCID. Multiple other cytokine and signaling defects lead to less severe primary immunodeficiencies.
Defects with toxic metabolite accumulation include ADA and PNP deficiency. The adenosine deaminase (ADA) is an essential enzyme of the purine salvage pathway, mediating the deamination of adenosine and 2-deoxyadenosine into inosine and deoxyinosine. Deficiency of ADA leads to toxic accumulation of these metabolites, which results in lymphocyte apoptosis (T-B−NK− SCID). The purine nucleoside phosphorylase (PNP) constitutes another key enzyme within the purine salvage pathway downstream of ADA, deribosylating inosine to hypoxanthine and guanosine to guanine. PNP deficiency leads to toxic accumulation of deoxyguanosine and deoxyguanosine triphosphate, leading to apoptosis, mainly affecting the T cells (T-B+NK− SCID). As PNP deficiency leads to neurological symptoms and autoimmunity, the IUIS classification lists it as a combined immunodeficiency with associated features.
Hypomorphic mutations in any of these SCID genes may lead to less severe phenotypes of leaky SCID/combined immunodeficiency. Detailed descriptions of severe combined immunodeficiencies and combined immunodeficiencies may be found in Chaps. 6 and 7 of this book, whereas Table 2.2 gives an overview of genetic defects associated with cellular immunodeficiencies (Table 2.2).
2.11 Genetics of Combined Immunodeficiencies with Associated or Syndromic Features
In most primary immunodeficiencies, the immunodeficiency is the most prominent clinical finding. In contrast, syndromic immunodeficiencies are characterized by associated syndromes or clinical findings taking a front role. Associated features may commonly affect the skeletal, nervous, or ectodermal development or function but may include almost any organ system. In contrast to most other classes of immunodeficiencies, not all syndromic immunodeficiencies are typically caused by a genetic defect in a single gene but may result from underlying cytogenetic abnormalities, i.e., abnormalities of chromosomal number or structure. DiGeorge syndrome caused by 22q11 deletions is the most well-known example. Cytogenetic abnormalities may be detected by karyotyping or fluorescence in situ hybridization (FISH).
As of 2019, there are a total number of 58 combined immunodeficiencies with associated or syndromic features comprising 62 distinct genetic defects [1]. These include immunodeficiencies with congenital thrombocytopenia (WAS, WIPF1, ARPC1B), other DNA repair defects (ATM, NBS1, BLM, DNMT3B, CDCA7, HELLS, PMS2, RNF168, MCM4, POLE1, POLE2, LIG1, NSMCE3, ERCC6L2, GINS1), thymic defects with congenital abnormalities (22q11.2DS, TBX1, CHD7, SEMA3E, FOXN1, 10p13-p14DS, 11q23del), immuno-osseous dysplasias (RMRP, SMARCAL1, MYSM1, RNU4ATAC, EXTL3), hyper-IgE syndromes (STAT3, IL6R, IL6ST, ZNF341, ERBB2IP, TGFBR1, TGFBR2, SPINK5, PGM3, CARD11), defects in vitamin B12 and folate metabolism (TCN2, SLC46A1, MTHFD1), anhidrotic ectodermal dysplasia with immunodeficiency (IKBKG, NFKBIA, IKBKB), calcium channel defects (ORAI1, STIM1), and other defects (PNP, TTC7A, TTC37, SKIV2L, SP110, BCL11B, EPG5, RBCK1, RNF31, CCBE1, FAT4, NFE2L2, STAT5B, KMT2D, KDM6A, KMT2A). A detailed description of combined immunodeficiencies with associated or syndromic features may be found in Chap. 8 of this book.
2.12 Genetics of Defects in Intrinsic and Innate Immunity
Defects of innate immunity comprise multiple heterogeneous groups of defects, out of which some can be counted toward cellular immunodeficiency, others constitute defects of soluble factors such as complement factors, and yet other defects derive from a defective barrier function, which are defects of nonimmune cells, however, predisposing to infection. Furthermore, defects of innate immunity may have an impact on the adaptive immune system through impaired (co-)stimulation or antigen presentation.
In recent years many novel inborn errors of innate immunity have been described, often leading to an increased susceptibility to a narrow range of pathogens. These include Mendelian susceptibility to mycobacterial disease, predisposition to chronic mucocutaneous candidiasis or invasive fungal infections, predisposition to herpes simplex encephalitis, and other severe viral infections. A detailed description of defects of intrinsic and innate immunity may be found in Chap. 10 of this book.
A major subgroup within the defects of innate immunity are the congenital defects of phagocytes; thus, they are often listed separately, and also this book dedicated a separate chapter to them (for congenital defects of phagocytes, see Chap. 9). Congenital defects of phagocytes comprise congenital neutropenias (i.e., defects with reduced neutrophil numbers); defects of neutrophil function including motility, chemotaxis, and adhesion; defects of respiratory burst (chronic granulomatous disease); and other nonlymphoid defects. As of 2019, the IUIS recognizes 41 distinct phagocyte defects [1].
2.13 Outlook
While so far more than 430 genetic defects causing primary immunodeficiencies have been identified, there may be many more novel defects left to discover. In theory, the number of potential human inborn errors of immunity is only limited by the number of genes related to the immune system. The gene ontology (GO) database lists 2782 genes within the category “immune system process”; thus, there may be many discoveries of novel primary immunodeficiencies in the years to come.
As our understanding of molecular as well as regulatory processes evolves, phenocopies of PID with somatic mutations, polygenic traits, and also epigenetic changes, all not constituting PID in the narrower sense, might gain further importance, which may ultimately lead to changes in our understanding of the concept of what constitutes a primary immunodeficiency or an inborn error of immunity.
References
Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A et al (2020) Human inborn errors of immunity: 2019 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol 40(1):24–64
Herman SE, Gordon AL, Hertlein E, Ramanunni A, Zhang X, Jaglowski S et al (2011) Bruton tyrosine kinase represents a promising therapeutic target for treatment of chronic lymphocytic leukemia and is effectively targeted by PCI-32765. Blood 117(23):6287–6296
Mendel G (1996) Experiments in plant hybridization (1865). Verhandlungen des naturforschenden Vereins Brünn) Available online
Morgan TH, Sturtevant AH, Bridges CB, Muller HJ (1915) The mechanism of Mendelian heredity. H. Holt, New York
Avery OT, Macleod CM, McCarty M (1944) Studies on the chemical nature of the substance inducing transformation of pneumococcal types: induction of transformation by a desoxyribonucleic acid fraction isolated from pneumococcus type III. J Exp Med 79(2):137–158
Watson JD, Crick FH (1953) Molecular structure of nucleic acids; a structure for deoxyribose nucleic acid. Nature 171(4356):737–738
Ingram VM (1956) A specific chemical difference between the globins of normal human and sickle-cell anaemia haemoglobin. Nature 178(4537):792–794
Giblett ER, Anderson JE, Cohen F, Pollara B, Meuwissen HJ (1972) Adenosine-deaminase deficiency in two patients with severely impaired cellular immunity. Lancet 2(7786):1067–1069
Sanger F, Nicklen S, Coulson AR (1977) DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci U S A 74(12):5463–5467
Vetrie D, Vorechovský I, Sideras P, Holland J, Davies A, Flinter F et al (1993) The gene involved in X-linked agammaglobulinaemia is a member of the src family of protein-tyrosine kinases. Nature 361(6409):226–233
Tsukada S, Saffran DC, Rawlings DJ, Parolini O, Allen RC, Klisak I et al (1993) Deficient expression of a B cell cytoplasmic tyrosine kinase in human X-linked agammaglobulinemia. Cell 72(2):279–290
D’Elios MM, Rizzi M (2019) Humoral Primary Immunodeficiencies. Springer, Cham
Mensa-Vilaró A, Bravo García-Morato M, de la Calle-Martin O, Franco-Jarava C, Martínez-Saavedra MT, González-Granado LI et al (2019) Unexpected relevant role of gene mosaicism in patients with primary immunodeficiency diseases. J Allergy Clin Immunol 143(1):359–368
Vaz-Drago R, Custódio N, Carmo-Fonseca M (2017) Deep intronic mutations and human disease. Hum Genet 136(9):1093–1111
Goldschmidt R (1935) Gen und Außeneigenschaft. Z Indukt Abstamm Vererbungsl 69(1):38–69
Marian AJ (2010) DNA sequence variants and the practice of medicine. Curr Opin Cardiol 25(3):182–185
Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM et al (2001) dbSNP: the NCBI database of genetic variation. Nucleic Acids Res 29(1):308–311
Landrum MJ, Lee JM, Benson M, Brown GR, Chao C, Chitipiralla S et al (2018) ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res 46(D1):D1062–D10D7
Karczewski KJ, Weisburd B, Thomas B, Solomonson M, Ruderfer DM, Kavanagh D et al (2017) The ExAC browser: displaying reference data information from over 60 000 exomes. Nucleic Acids Res 45(D1):D840–D8D5
Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q et al (2020) The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581(7809):434–443
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J (2014) A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet 46(3):310–315
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P et al (2010) A method and server for predicting damaging missense mutations. Nat Methods 7(4):248–249
Kumar P, Henikoff S, Ng PC (2009) Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4(7):1073–1081
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424
den Dunnen JT, Dalgleish R, Maglott DR, Hart RK, Greenblatt MS, McGowan-Jordan J et al (2016) HGVS recommendations for the description of sequence variants: 2016 update. Hum Mutat 37(6):564–569
Wildeman M, van Ophuizen E, den Dunnen JT, Taschner PE (2008) Improving sequence variant descriptions in mutation databases and literature using the Mutalyzer sequence variation nomenclature checker. Hum Mutat 29(1):6–13
Casanova JL, Conley ME, Seligman SJ, Abel L, Notarangelo LD (2014) Guidelines for genetic studies in single patients: lessons from primary immunodeficiencies. J Exp Med 211(11):2137–2149
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Frede, N. (2021). Genetics of Cellular Immunodeficiencies. In: D'Elios, M.M., Baldari, C.T., Annunziato, F. (eds) Cellular Primary Immunodeficiencies. Rare Diseases of the Immune System. Springer, Cham. https://doi.org/10.1007/978-3-030-70107-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-70107-9_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70106-2
Online ISBN: 978-3-030-70107-9
eBook Packages: MedicineMedicine (R0)