Abstract
This chapter describes the long-term benefits of Disease Management Programmes (DMPs) in The Netherlands. We used the Chronic Care Model to thoroughly evaluate their long-term effects. Results clearly show that DMPs based on the chronic care model in the Netherlands resulted in (i) the successful improvement of quality of chronic care as perceived by chronically ill patients and professionals, (ii) more productive interaction between chronically ill patients and their health care professionals (iii) and improvements in chronically ill patients’ health behaviors (they smoke less and are more physically active) and physical quality of life. The findings highlight the need to broaden the scope of DMPs not aimed at functional health and self-management of a chronic disease only but also at broader self-management abilities and overall well-being which calls for person-centred care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Using the Chronic Care Model to Evaluate the Long-Term Effects of Disease Management Programs in The Netherlands
Healthcare systems and providers are currently not equipped to deal with the complexities of aging populations and the high prevalence of chronic diseases that come with it. Clearly, rapid increase of people with chronic diseases is expected to lead to increased healthcare, social care and social security costs. However, evidence also indicates that carefully planning ahead and making evidence-based choices will enable countries and their primary care systems to successfully manage the situation. According to Ed Wagner, care processes must be redesigned and supportive of productive patient–professional interactions, which in turn leads to better outcomes (Wagner et al. 1996a, b, 2001; Coleman et al. 2009) which resulted in the chronic care model (Fig. 72.1). This model provides a multidimensional framework guiding disease management programs (DMPs) aiming to replace their current system which are usually based on acute and reactive care, with planned, population-based care delivery to patients with chronic diseases (Wagner et al. 2001; Coleman et al. 2009; Norris et al. 2003).
The CCM includes six interrelated components of the quality of care for the chronically ill:
-
1.
Self-management support (i.e., empowering patients to self-manage their own care through education, lifestyle programs, skills building, planning, goal setting and problem solving);
-
2.
Delivery system design (i.e., redesign the way that care is delivered to chronically ill patients by redefining healthcare team members’ roles);
-
3.
Decision support (i.e., implement and use of care standards and clinical guidelines, use the latest evidence when decisions are made with patients);
-
4.
Clinical information systems (i.e., implement information systems, providing timely reminders and feedback for patients and health professionals, planning and coordinating care for individual patients, monitoring healthcare team performance and effectiveness of individual care);
-
5.
Healthcare systems (i.e., promoting effective strategies at all levels to comprehensively change the care system, developing agreements to coordinate care and address quality issues, provide (financial) incentives to improve the quality of chronic care delivery); and
-
6.
Community linkages (i.e., developing partnerships with community organizations to support interventions that complement health services, advocating for policy changes that improve patient care) (Cramm and Nieboer 2015a, b, c; Wagner et al. 1996a, b, 2001; Coleman et al. 2009).
Although it is known that DMPs based on the chronic care model prevent disease complications among patients with chronic obstructive pulmonary disease (COPD) (Adams et al. 2007) and are related to better outcomes indicated by measures of care processes and clinical outcomes (Tsai et al. 2005) and their long-term benefits have not been established thoroughly. Furthermore, the Chronic Care Model is not static but incorporates flexibility in the implementation of interventions, resulting in a mixture of DMPs (Cramm et al. 2013). Thus, different DMPs may incorporate the six components of the Chronic Care Model to various extents using diverse constellations of interventions. To understand the design and effects of DMPs based on the Chronic Care Model, it is important to (1) know which interventions were actually implemented within the Dutch DMPs, (2) assess if implementation of interventions led to better quality of chronic care, (3) investigate if (improvements in) quality of chronic care resulted in more productive patient–professional interactions and (4) assess long-term effects on patient outcomes (healthier lifestyles, better self-management abilities, quality of life). These four questions will be answered in this chapter.
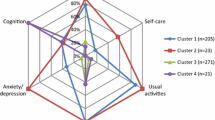
This study included patients and professionals participating in 18/22 disease management programs based on the Chronic Care Model that were implemented in various regions of the Netherlands that were followed for at least two years (Lemmens et al. 2011; Cramm et al. 2014a, b). For this chapter, four DMPs were excluded due to (i) a sample size smaller than 15 patients; (ii) incomplete data availability caused by delayed questionnaire distribution; (iii) DMPs aimed at hospitalized patients instead of those still living on their own and (iv) slightly different questionnaire content to address a specific mental health condition (e.g., eating disorders and depression). The 18 included DMPs were aimed at patients with CVDs (n = 9), COPD (n = 4), heart failure (n = 1), comorbidity (n = 1) and diabetes (n = 3) (Cramm et al. 2014a, b).
2 Question 1: Which Interventions Mapped to the Chronic Care Model Were Actually Implemented Within the Dutch DMPs?
In order to answer this research question, we developed a template based on the Chronic Care Model. All project leaders of the 18 DMPs were asked about the implementation of all interventions within their DMP. After finalizing, the template was sent back to the project leaders for final corrections (Cramm and Nieboer 2015a, b, c).
Each disease management program successfully implemented a constellation of interventions within each of the six dimensions of the Chronic Care Model (see Table 72.1). Care standards/clinical guidelines, training and independence of practice assistants, professional education and training for care providers and hospital or practice information system were implemented within all the DMPs, whereas organizing a health market, use of cognitive behavioral therapy, use of care protocols for immigrants specifically and having an electronic patient records system with a working patient portal were implemented in a single DMP only. DMPs clearly vary in the interventions they implemented within each DMP.
3 Question 2: Did the Quality of Chronic Care Delivery Measured with the CCM Dimensions Improve Over Time?

An important question is the implementation of the interventions listed in Table 72.1 resulted in better quality of chronic care. Looking at the results of professionals’ experiences with quality of chronic care delivery over a two-year time frame, all six dimensions of the CCM as well as the overall score improved significantly (Table 72.2). Two years after implementation of the DMPs, all CCM areas were indicated as advanced support for chronic illness care (Bonomi et al. 2002; Cramm and Nieboer 2014; Cramm et al. 2014a, b).
In addition to investigating quality of care as experienced by professionals, we were also interested in assessing patients’ experiences. These results indicated DMPs implementation which also led to more positive experiences among chronically ill patients (Cramm and Nieboer 2013a, b).
Furthermore, results clearly showed that quality of chronic care delivery at T0 (p < 0.001) and quality changes in the first (p < 0.001) and second (p < 0.01) years predicted program sustainability (Cramm and Nieboer 2014).
4 Question 3: Did Quality of Chronic Care Delivery Result in Productive Interactions Between Patients and Healthcare Professionals?

While theoretically it is expected that improvement in the six components of the Chronic Care Model increases productive patient–professional interaction, empirical evidence is lacking. We, therefore, aimed to assess the influence of (improvement in) the six components of the Chronic Care Model on productive patient–professional interaction. The results presented in Table 72.3 clearly show that after controlling for main characteristics of patients, quality of care delivery at baseline, as well as first- and second-year changes therein predicted productive interactions between patients and professionals (Cramm and Nieboer 2013a, b).
5 Question 4: Did DMP Implementation Lead to Better Patient Outcomes?

Finally, we aimed to determine experiences of DMPs and their long-term effects on the following outcomes (i) health behaviors (smoking and physical exercise), (ii) self-management abilities (self-efficacy, investment behavior, and initiative taking), and (iii) physical and mental quality of life among chronically ill patients. Analyses showed DMP implementation improved patients’ physical quality of life and their health behaviors; they smoked less and are more physically active (Cramm and Nieboer 2015a, b, c). However, they struggled with patients’ mental quality of life and their self-management abilities to maintain well-being (Cramm and Nieboer 2015a, b, c). Self-management abilities to maintain well-being as well as mental quality of life decreased over time, despite improvements in quality of care and more productive patient–professional interactions. These findings suggest that the Chronic Care Model and DMPs based on it focus primarily on clinical and functional outcomes rather than overall quality of life and well-being (Barr et al. 2003; Cramm and Nieboer 2015a, b, c; Cramm and Nieboer 2012).
6 Conclusion
The long-term benefits of DMPs based on the Chronic Care Model in the Netherlands resulted in (i) the successful improvement of quality of chronic care as perceived by chronically ill patients and professionals, (ii) more productive interaction between chronically ill patients and their healthcare professionals (iii) and improvements in chronically ill patients’ health behaviors and physical quality of life. However, these programs did not successfully improve or even maintain broader self-management abilities or mental quality of life, which declined over time. These findings highlight the need to broaden the scope of DMPs not aimed at functional health and self-management of a chronic disease only but also at broader self-management abilities and overall well-being. DMPs have failed to address important difficulties chronically patients are dealing with such as the effects of pain and fatigue on the ability to maintain a job, hobby and social life. Patients’ ability to maintain engagement in stimulating activities related to work and one’s social life may be even more important than aspects of disease self-management such as glycemic control or blood pressure. This calls for a person-centered approach aimed at their physical, social and mental well-being (Cramm and Nieboer 2012).
References
Adams, S. G., Smith, P. K., Allan, P. F., Anzueto, A., Pugh, J. A., & Cornell, J. E. (2007). Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med, 167, 551–561.
Barr, V. J., Robinson, S., Marin-Link, B., et al. (2003). The expanded chronic care model: An integration of concepts and strategies from population health promotion and the chronic care model. Hospital Quarterly, 7, 73–82.
Bonomi, A. E., Wagner, E. H., Glasgow, R. E., et al. (2002). Assessment of chronic illness care (ACIC): A practical tool to measure quality improvement. BMC Health Services Research, 37, 791–820.
Coleman, K., Austin, B. T., Brach, C., & Wagner, E. H. (2009). Evidence on the chronic care model in the new millennium. Health Affairs (Millwood), 28(1), 75–85.
Cramm, J. M., & Nieboer, A. P. (2012). In The Netherlands, rich interaction among professionals conducting disease management led to better chronic care. Health Affairs, 31(11), 2493–2500.
Cramm, J. M., & Nieboer, A. P. (2013a). Short and long term improvements in quality of chronic care delivery predict program sustainability. Social Science and Medicine, 101, 148–154.
Cramm, J. M., & Nieboer, A. P. (2013b). High-quality chronic care delivery improves experiences of chronically ill patients receiving care. International Journal for Quality in Healthcare, 25(6), 689–695.
Cramm, J. M., & Nieboer, A. P. (2014). A longitudinal study to identify the influence of quality of chronic care delivery on productive interactions between patients and (teams of) healthcare professionals within disease management programs. British Medical Journal Open, 4, e005914. https://doi.org/10.1136/bmjopen-2014-005914.
Cramm, J. M., & Nieboer, A. P. (2015a). Disease management: The need for a focus on broader self-management abilities and quality of life. Population Health Management, 18(4), 246–255.
Cramm, J. M., & Nieboer, A. P. (2015b). Chronically ill patients’ self-management abilities to maintain overall well-being: What is needed to take the next step in the primary care setting? BMC Family Practice, 16, 123.
Cramm, J. M., & Nieboer, A. P. (2015c). Productive patient-professional interaction improves the well-being of chronically ill patients. Quality of Life Research, 24(4), 897–903.
Cramm, J. M., Adams, S. A., Walters, B. H., Tsiachristas, A., Bal, R., Huijsman, R., et al. (2014a). The role of disease management programs in the health behavior of chronically ill patients. Patient Education and Counseling, 87(3), 411–415.
Cramm, J. M., Tsiachristas, A., Adams, S. A., Hipple-Walters, B. H., Bal, R., Huijsman, R., et al. (2014b). Evaluating disease management programmes in The Netherlands. Sociaal-Medische Wetenschappen (SMW).
Cramm, J. M., Tsiachristas, A., Hipple-Walters, B., Adams, S., Bal, R., Huijsman, R., et al. (2013). The management of cardiovascular disease in The Netherlands: Analysis of different programmes. International Journal for Integrated Care, 13, e028.
Lemmens, K. M. M., Rutten-Van Mölken, M. P. M. H., Cramm, J. M., Huijsman, R., Bal, R. A., & Nieboer, A. P. (2011). Evaluation of a large scale implementation of disease management programmes in various Dutch regions: A study protocol. BMC Health Services Research, 11, 6.
Norris, S. L., Glasgow, R. E., Engelgau, M. M., O’Connor, P. J., & McCulloch, D. (2003). Chronic disease management: A definition and systematic approach to component interventions. Disease Management and Health Outcomes, 11, 477–488.
Tsai, A. C., Morton, S. C., Mangione, C. M., & Keeler, E. B. (2005). A metaanalysis of interventions to improve care for chronic illnesses. The American Journal of Managed Care, 11, 478–488.
Wagner, E. H., Austin, B. T., & Von Korff, M. (1996a). Improving outcomes in chronic illness. Managed Care Quarterly, 4(2), 12–25.
Wagner, E. H., Austin, B. T., & Von Korff, M. (1996b). Organizing care for patients with chronic illness. Milbank Quarterly, 74, 511–544.
Wagner, E. H., Austin, B. T., Davis, C., Hindmarsh, M., Schaefer, J., & Bonomi, A. (2001). Improving chronic illness care: Translating evidence into action. Health Affairs (Millwood)., 20(6), 64–78.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cramm, J.M., Nieboer, A.P. (2021). Disease Management Programs in The Netherlands; Do They Really Work?. In: Amelung, V., Stein, V., Suter, E., Goodwin, N., Nolte, E., Balicer, R. (eds) Handbook Integrated Care. Springer, Cham. https://doi.org/10.1007/978-3-030-69262-9_72
Download citation
DOI: https://doi.org/10.1007/978-3-030-69262-9_72
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-69261-2
Online ISBN: 978-3-030-69262-9
eBook Packages: Business and ManagementBusiness and Management (R0)