Abstract
In August 2019, a 47-year-old male patient was admitted to the hospital due to recurrent right-sided hemiparesis that occurred during 12 h. Symptoms started evening before the hospitalization with right side weakness that withdrawn spontaneously after 10 min. Right-sided hemiparesis reappeared during the night and lasted for about 40 min.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Large cerebral vessel vasculitis
- HIV-related vasculitis
- neurosyphilis
- meningovascular syphilis
- Heubner arteritis
- Nissl arteritis
In August 2019 , a 47-year-old male patient was admitted to the hospital due to recurrent right-sided hemiparesis that occurred during 12 h. Symptoms started evening before the hospitalization with right side weakness that withdrawn spontaneously after 10 min. Right-sided hemiparesis reappeared during the night and lasted for about 40 min.
According to available anamnestic data, the patient had performed brain MRI about 10 years ago due to an episode of headache—MRI was reported normal. He claimed he had an episode of right-sided weakness in duration of 10 min before 7 or 8 years, after which no diagnostic procedures or medical treatment have been conducted. Patient was a smoker: smoked 10–12 cigarettes per day.
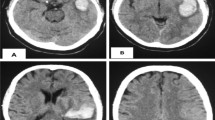
In neurologist assessment on admission, mild right-sided hemiparesis was reported. Head CT and CTA of cerebral arteries were performed in the EHD (Fig. 25.1). All laboratory findings, blood count, prothrombin time, C-reactive protein, urea, creatinine, electrolytes and liver function tests were normal on admission.
Computed tomography of the brain, axial (a–c) and coronal (d–f) scans, and computed tomography angiography of cerebral arteries, axial (g) and coronal (h, i) images, performed in the EHD, were evaluated by interventional radiologist who was on call: head CT was reported normal while middle and distal part of M1 segment of the left middle cerebral artery (MCA) were reported stenotic on cerebral CTA
Because two successive brain CTs were reported normal (Figs. 25.1 and 25.2), brain MRI was performed and evaluated by neuroradiologist.
During the course of MRI and MRA procedures, I have re-evaluated both brain CTs because it was strange to me why changes of the M1-MCA wall were reported on cerebral CTA without evidence of parenchymal lesion. On CT performed on the admission (Fig. 25.1), I have found irregular hypodensity in the posterior limb of the left internal capsule consistent with acute ischaemia (Fig. 25.1b, c, f), old lacunar infarct in the medial part of the left globus pallidus (Fig. 25.1a, d, e) and small gliosis in the genus of the left internal capsule (Fig. 25.1a, b). On brain CT performed the next day (Fig. 25.2), I realized hypodensity of the posterior limb of the left internal capsule was the same in size, but slightly more hypodense and clearly demarcated.
I have analyzed brain MRI and cerebral MRA images (Fig. 25.3) and reported large cerebral vessel vasculitis with acute ischaemia. Afterwards, I have asked myself why would previously healthy middle-aged patient had such changes. I contacted the attending neurologist to discuss possible aetiologies including drugs and HIV status. The neurologist had informed me that the patient was not a drug addict, but was a homosexual, tested for HIV 5 years ago when he was negative. After our conversation patient was retested for HIV and the test was positive. He was also tested for HBV and HCV. hepatitis B surface antigen (HbsAg) was negative, antibody to hepatitis B core antigen (anti-HBc) and antibody to hepatitis B surface antigen (anti-HBs, 4.34 IU/L) were positive, indicating past infection. Anti-HCV was negative. Consulted immunologist did not think that systemic disease was the aetiology of the patient’s vasculitis: recommended specific tests were negative.
Magnetic resonance imaging of the brain, axial T2WI (a–c), FLAIR FS (d–f), DWI (g–i), ADC (j–l), revealed multiple acute infarcts in the left cerebral hemisphere: three punctate acute ischaemia in the left amygdala (a, d, g, j), acute ischaemia involving posterior part of the left putamen and globus pallidus and posterior limb of the internal capsule (b, e, h, k), four punctate acute ischaemia in the subcortical white matter of the left occipital lobe (b, e, h, k), and small acute ischemia in the periventricular white matter of the left frontal lobe (c, f, i, l). Old lacunar infarct in the medial part of the left globus pallidus and small gliosis in the genu of the left internal capsule were revealed as well (b, e). Cerebral magnetic resonance angiography (3D TOF), axial (m–o) images, showed mural irregularities with alternating stenosis and dilatation resulting in beaded appearance of the M1 segment of the left MCA which indicated vasculitis
Afterwards, patient was in infectologist treatment: additional CSF analysis was positive for syphilis, final diagnose of meningovascular form of syphilis was made, and the patient was successfully treated for neurosyphilis . Medicamentous treatment of HIV infection was initiated as well.
1 Large Cerebral Vessel Vasculitis in Undiagnosed HIV-Positive Patient: Meningovascular Syphilis
Vasculitis of the CNS is a rare entity that may result from numerous causes responsible for the presence of inflammatory lesions at the vascular wall with or without necrosis that lead to obstruction of the lumen. Cerebral vessels of all sizes can be affected, and the clinical manifestations are highly variable, ranging from focal neurological signs to diffuse manifestations with an acute to chronic evolution. Vasculitis disorders of the CNS consist of primary angiitis of the CNS, CNS vasculitis associated with connective tissue disorders, vasculitis associated with Behcet’s disease, and sarcoidosis, as well as infectious and neoplastic diseases [1].
Cerebrovascular disease is common in patients with HIV, occurring in up to 1.9% of HIV-infected patients [2]. In particular, patients with AIDS have been reported to be at increased risk of both ischaemic and haemorrhagic strokes, of which ischaemic stroke is more frequent. The pathogenesis of ischemic stroke in HIV is not well understood, with multiple postulated mechanisms including cardioembolism, coagulopathy, opportunistic infections, HIV-related vasculitis and HAART-related accelerated atherosclerosis, as well [3].
Vasculitis in HIV is generally secondary to lymphoproliferative diseases or opportunistic infections, including varicella-zoster virus, syphilis, cryptococcus and tuberculosis. In patients in whom the above have been excluded, HIV-related vasculitis is one consideration. This has been reported to occur in up to 20% of patients with HIV [3]. While the pathophysiology behind HIV-related vasculitis is not well defined, this condition is more commonly described in patients with low CD4 counts [3, 4].
As sexually transmitted diseases, syphilis and HIV frequently coexist. Among patients with HIV, those with lower CD4 counts are more likely to have concomitant neurosyphilis [5]. CNS involvement is an uncommon manifestation of syphilis, occurring in less than 10% of patients with syphilis [6]. A study of HIV-infected patients by Ghanem et al. identified CD4 count of less than 350 cells/ml and lack of HAART treatment as predictors of neurosyphilis [7]. Lower CD4 counts have also been found to be associated with an increased risk of ischemic stroke.
Illicit drug users (e.g. cocaine and methamphetamine) and men who have sex with men are at the main risk to contract syphilis. After the initial stage, syphilis is a self-limited disease and may go undetected. Untreated syphilitic infection progresses through four stages; primary, secondary, latent and tertiary [8]. Neurosyphilis is a form of tertiary syphilis commonly seen in HIV-infected individuals, occurring in less than 10% of untreated individuals with syphilis [9]. Spirochetes (Treponema pallidum) usually invade CNS within 3–18 months of inoculation with the organism [4]. The major forms of neurosyphilis are syphilitic meningitis, meningovascular syphilis, parenchymatous syphilis, and gummatous syphilis. With the advent of penicillin therapy, neurosyphilis more frequently manifests as meningeal and vascular syndromes, not as abnormalities of the CNS parenchyma.
The average latency of meningovascular syphilis is reported to be 7 years; however, meningovascular syphilis can occur within a few months of infection in HIV patients which indicates the difficulty in diagnosing neurosyphilis in patients with HIV.
Meningovascular neurosyphilis is an inflammatory process resulting from the development of typical endarteritis obliterans in blood vessels of the meninges, brain and spinal cord that leads to multiple small areas of infarction. Heubner arteritis is the most common form that affects large- and medium-sized arteries and is characterized by fibroblastic proliferation of the intima, thinning of the media and fibrous and inflammatory changes in the adventitia causing luminal narrowing and ectasia. Nissl arteritis affects small vessels and is characterized by the proliferation of endothelial and adventitial cells. Both the types of arteritis may result in vessel occlusion, with secondary ischaemia and infarction [10]. The middle cerebral artery followed by an involvement of the basilar artery and its branches is the most commonly involved.
Neurological symptoms with little or no evidence of primary or secondary syphilis may well be the first manifestation. Clinical manifestations may vary greatly from asymptomatic to symptoms such as headache, vertigo, seizures, transient hemiplegia, insomnia or behavioural changes ranging from personality changes and emotional lability to dementia. These symptoms may appear from months to even a decade after the primary infection, with an average latency of 7 years.
Typical imaging findings are ischaemic infarcts in the perforator vessel territory of the basal ganglia or brainstem or in the large vessel territory of the middle cerebral artery. Syphilitic cerebral gummas are uncommon. They appear as isolated, peripherally located nodules on CT that appear isodense to cortex and enhance intensely following iodinated contrast material administration. On MRI, they are isointense to grey matter on T1W sequences, usually enhance homogeneously, and are hyperintense on T2W sequences. Cranial nerve involvement, particularly of the optic and vestibulocochlear nerves, has also been reported [11,12,13].
Angiographically, meningovascular syphilis tends to display focal segmental narrowing and dilatation, resulting in the appearance of “beading”. However, these findings are nonspecific and can resemble findings in other medium and large vessel vasculitides, and an underlying HIV-associated vasculopathy cannot be excluded [3, 14].
In the smaller arteries, particularly Sylvian branches of the middle cerebral artery, focal stenosis and aneurysmal dilatation may be demonstrated.
The gold standard for the diagnosis of CNS vasculitis is histopathological evidence of vessel wall inflammation [15]. Brain biopsy is an invasive technique. Therefore, diagnosis of neurosyphilis could be established if there is a syndrome consistent with neurosyphilis , investigations of CSF cell count and protein concentration, and test of non-treponemal antibody as well as serologic treponemal antibody testing are made. Serologic screening for syphilis should be performed in patients with cryptogenic stroke, particularly in those with risk factors for syphilis. The presence of a positive treponemal test should prompt further evaluation for neurosyphilis with lumbar puncture. CSF features suggestive of neurosyphilis include lymphocytic pleocytosis, low glucose and raised protein, which may occur in HIV alone as well.
Neurosyphilis is a treatable disease with a favourable outcome. Treatment of neurosyphilis is the same in HIV-positive and -negative patients and involves a 10- to 14-day course of high-dose intravenous benzylpenicillin. Neurological deficits frequently but not always resolve following treatment.
Many authors state that syphilis appears to be the “great imitator” of other diseases. Therefore, the diagnosis of neurosyphilis remains a challenge, as it requires a high index of suspicion. Recent studies recommend that, due to the re-emergence of syphilis, search for Treponema pallidum infection should be systematic in young stroke victims [16]. The question remains as to whether the search should include all-age patients even in the absence of a suggestive history.
Middle-aged male homosexual patient with the acute ischaemia in the MCA vascular territory and evidence of vasculitis of M1 segment, who did not use illicit drugs and did not have connective tissue disorder, are highly suspicious for being HIV positive and should be tested for neurosyphilis [13].
Regarding the patient’s anamnestic data available in the hospital information system, in the section of “functions and habits”, there was no information about illicit drug usage or sexual orientation. However, those information were well known to attending neurologist. As neuroradiologist, I have suspected possible aetiology of multiple small infarctions in the MCA vascular territory and M1 segment vasculitis. The problem was that the neurologist had information about the patient’s sexual orientation and illicit drug non-use, but did not think those information could be of interest or helpful to neuroradiologist in reporting MRI and MRA findings. Since the attending neurologist knew that the patient is a homosexual, and I reported M1-MCA vasculitis with small acute infarctions, the patient was tested for HIV and, after the positive testing result, referred to infectologist for further treatment.
The patient also gave information that he had an episode of right-sided weakness in duration of 10 min 7 or 8 years ago, after which no diagnostic procedures or medical treatment have been conducted. CT (Fig. 25.1a, b) and MRI (Fig. 25.3b, e) revealed two old vascular lesions in the left medial globus palidus and genus of internal capsule indicating that the patient definitely had small acute ischemia before. It is possible that those two lesions were small acute ischaemia at the time 7 or 8 years ago when patient suffered from a transient episode of right-sided weakness. I cannot be sure because he might also have been asymptomatic at the time those two lesions originated. It will remain unclear when this two lesions appeared regarding the time of their origin, but they definitely confirm that the patient had CNS vasculitis for some time before the advent of the episode because of which he was hospitalized.
Unfortunately, neurologists do not offer proper or full information about patients to neuroradiologists from time to time, which could be a problem. For me it means two facts, sometimes I have to call the patient again to perform additional sequences or advanced techniques. The second is that I have to search for information myself: I have to go through the patient’s medical documentation if it is available, and I have to interview a patient if possible. If I am not successful in a search, then I talk to an attending neurologist. Sometimes I realize, like in this case, they had information, but did not give it to me in advance for a reason only known to them. Sometimes, they did not have needed information because they did not ask the patient or did not suspect disorder I reported while evaluating CT or MRI. Fortunately, those situations are not customary or frequent and my collaboration with neurologists is usually successful.
References
Mumtaz S, et al. Central nervous system vasculitis. In: Current clinical neurology: inflammatory disorders of the nervous system: pathogenesis, immunology and clinical management. Totowa, NJ: Humana Press Inc. p. 257–68.
Evers S, et al. Ischaemic cerebrovascular events in HIV infection. Cerebrovas Dis. 2003;15:199–205.
Jan K, et al. Ischemic stroke in an HIV positive patient: an initial presentation of neurosyphilis. Case Rep Neurological Med. 2018;2018:2410154. https://doi.org/10.1155/2018/2410154.
Vaitkus A, et al. Meningovascular neurosyphilis: a report of stroke in a young adult. Medicina (Kaunas). 2010;46(4):282–5.
Marra CM, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004;189(3):369–76.
Abkur TM, et al. Neurosyphilis presenting with a stroke-like syndrome. BMJ Case Rep. 2015;2015:bcr2014206988.
Ghanem KG, et al. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS. 2008;22(10):1145–51.
Krishnan D, et al. Neurosyphilis presenting as an acute ischemic stroke. Clin Med. 2020;20(1):95–7.
Hook EW, Chansolme DH. Neurosyphilis. In: Roos KL, editor. Principles of neurologic infectious diseases. New York: McGraw-Hill; 2005. p. 215–32.
Pezzini A, et al. Meningovascular syphilis: a vascular syndrome with typical features? Cerebrovasc Dis. 2001;11:352–3.
Senocak E, et al. Imaging features of CNS involvement in AIDS. Diagn Interv Radiol. 2010;16:193–200.
Abdel Razek AAK, et al. Imaging spectrum of CNS vasculitis. Radiographics. 2014;34:873–94.
Ruisanchez A, et al. Role of MRI in early detection of stroke secondary to neurosyphilis in an elderly patient. Neurol Clin Pract. 2017;7(2):12–5.
Holland BA, et al. Meningovascular syphilis: CT and MR findings. Radiology. 1986;158:439–42.
Cheron J, et al. Response of human immunodeficiency virus-associated cerebral angiitis to the combined antiretroviral therapy. Front Neurol. 2017;8:95.
Lachaud S, et al. Stroke, HIV and meningovascular syphilis: study of three cases [in French]. Rev Neurol. 2010;166:76–82.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Špero, M. (2021). Large Cerebral Vessel Vasculitis in Undiagnosed HIV-Positive Patient: Meningovascular Syphilis. In: Neuroradiology - Images vs Symptoms. Springer, Cham. https://doi.org/10.1007/978-3-030-69213-1_25
Download citation
DOI: https://doi.org/10.1007/978-3-030-69213-1_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-69212-4
Online ISBN: 978-3-030-69213-1
eBook Packages: MedicineMedicine (R0)