Summary
The conversion of methionine to inorganic sulfate involves the formation of homocysteine encompassing transmethylation followed by transsulfuration. Several inherited enzyme deficiencies within this pathway have been described. Those causing hypermethioninemia may be confused with the many known secondary causes of increased methionine demanding diagnostic expediency. Most of the disorders have been described in small numbers of patients so that the full clinical spectrum of these is not known. Exceptions are methionine adenosyltransferase (MAT) I/III deficiency and cystathionine ß-synthase deficiency which causes classical homocystinuria, characterized primarily by an increased risk of thrombosis and embolism, lens dislocation, and other connective tissue involvement and cognitive impairment. While methionine adenosyltransferase I/III deficiency is only symptomatic in some patients causing different neurological problems and glycine N-methyltransferase deficiency affects liver function, other diseases causing hypermethioninemias may be associated with a multisystem disease of varying severity and progression. MAT II deficiency can be associated with thoracic aortic aneurysms in some heterozygotes for MAT2 mutations. Methanethiol oxidase deficiency causes cabbage-like breath odor (extraoral halitosis). The association of mercaptopyruvate sulfur transferase deficiency with cognitive impairment, as the only disease characteristic, is questionable. Isolated sulfite oxidase deficiency is characterized by refractory convulsions in early infancy, brain atrophy, severe psychomotor retardation, and lens dislocation. Ethylmalonic encephalopathy is a severe disorder manifesting with seizures, developmental delay and cognitive impairment, orthostatic acrocyanosis and petechia due to vasodilation, failure to thrive, and chronic hemorrhagic diarrhea. Measurement of plasma and urine amino acids and total homocysteine can detect many of the disorders described in this chapter, while other tests are necessary for others. Confirmatory tests are enzyme assays and/or mutation analysis. Treatment combines one or more of dietary restriction of precursors, substitution of essential products, pharmacologic doses of cofactors, and binding and removing of harmful metabolites. Early diagnosis and early treatment favor better outcome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Sulfur-containing amino acids include methionine, homocysteine, cystathionine, cysteine, and taurine. This chapter deals with inherited deficiencies of enzymes in the transmethylation and transsulfuration pathways that convert sulfur from methionine via homocysteine and cysteine to sulfate, including sulfide metabolism (Fig. 22.1). Since adenosine kinase deficiency also disrupts the methionine cycle, it is included in this chapter.
Metabolism of sulfur amino acids and of hydrogen sulfide. Methionine is converted to cysteine via a series of reactions involving the following enzymes: MATI/III methionine adenosyltransferase I/III, MATII methionine adenosyltransferase II, GNMT glycine N-methyltransferase, SAHH S-adenosylhomocysteine hydrolase, BHMT betaine homocysteine methyltransferase, CBS cystathionine beta-synthase, CTH cystathionine gamma-lyase, AdoMet S-adenosylmethionine, AdoHcy S-adenosylhomocysteine. Cysteine serves as the major precursor for synthesis of hydrogen sulfide catalyzed by CBS, CTH, aspartate aminotransferase (AST), and mercaptopyruvate sulfurtransferase (MPST); hydrogen sulfide may be also synthesized by methanethiol oxidase (MTO). Another route of cysteine oxidation to taurine is catalyzed by cysteine dioxygenase (CDO) and cysteine sulfinic acid decarboxylase (CSAD). Mitochondrial oxidation of hydrogen sulfide requires the following enzymes: SQOR sulfide:quinone oxidoreductase, ETHE1 persulfide dioxygenase, TST thiosulfate transferase, SUOX sulfite oxidase, GSH glutathione, GSSH glutathione persulfide
Most disorders described in this chapter are inherited as autosomal recessive traits. Exceptions are autosomal dominant forms of methionine adenosyltransferase (MAT) II deficiency and a subgroup of MAT I/III deficiency, caused by mutations with dominant negative effect on the wild-type allele (Chamberlin et al. 1997).
Pathophysiology of disorders of sulfur-containing amino acids is complex and only partly understood (Kožich et al. 2016). In disorders associated with hypermethioninemia, very high concentrations can be harmful themselves, primarily for the brain. In MAT I/III deficiency, low adenosylmethionine (AdoMet) and subsequent deficient methylation could be contributing factors. There are several hypotheses of how MAT2A loss-of-function mutations could lead to aortic disease, and it is possible that they require a second “hit” (Guo et al. 2015). Methionine can be also transaminated yielding methanethiol; deficiency of methanethiol oxidase results in accumulation of malodorous molecules such as methanethiol and dimethylsulfide. In S-adenosylhomocysteine (AdoHcy) hydrolase deficiency, high concentrations of AdoHcy inhibit numerous methyltransferases with very variable clinical consequences. Several putative pathogenetic mechanisms of adenosine kinase deficiency are related to increased adenosine and its various toxic effects. Another mechanism could be inhibition of numerous methyltransferases caused by secondary elevation of S-adenosylhomocysteine. The latter mechanism could also be important in classical homocystinuria, where a major pathogenetic mechanism seems to be elevation of homocysteine with its adverse effect on coagulation, vessels and secondary to vascular changes in many tissues, and possibly the decreased production of cysteine manifesting in connective tissue including lens zonular fibers. Clinical consequences of sulfite oxidase deficiency are likely due to toxic effects of sulfite, S-sulfocysteine, and thiosulfate on the brain and connective tissue. Patients with ethylmalonic encephalopathy accumulate a large amount of hydrogen sulfide, which leads directly to vasodilation and to secondary inhibition of cytochrome c-oxidase with subsequent impairment of short-chain fatty oxidation with typical metabolite changes and of oxidative phosphorylation with lactic acidosis.
Clinical presentation can occur at any age and varies widely in its severity.
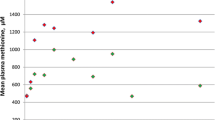
MAT I/III deficiency is asymptomatic in all individuals with the autosomal dominant disease, while about half of the patients with the autosomal recessive form have developed neurological symptoms (Chien et al. 2015). Hypermethioninemia, the biochemical hallmark of this disease, if severe, is itself associated with increased risk of various neurological problems (Braverman et al. 2005). The most characteristic brain imaging changes are demyelination with edema of subcortical and deep white matter, more pronounced in dorsal brain stem and resulting in separation of myelin layers—the so-called vacuolating myelinopathy (Braverman et al. 2005). Neurological abnormalities tend to occur in patients with plasma methionine concentrations generally above 800 μmol/L, whereas they have been rare in subjects with lower levels (Chien et al. 2015).
MAT II deficiency is only a risk factor for developing thoracic aortic aneurysms in some heterozygotes for MAT2A mutations.
Glycine N-methyltransferase (GNMT) deficiency (Mudd et al. 2001) has been so far described in only five children. The only clinical sign was mild hepatomegaly present in two siblings. The patients have remained clinically well during follow-up (Barić et al. 2017). Their aminotransferase activities ranged from borderline to fivefold increase. Plasma methionine can reach potentially damaging values (see MAT I/III deficiency).
S-adenosylhomocysteine hydrolase deficiency (Barić et al. 2004) has been proven and reported so far in ten patients. Two sibs had fetal hydrops, liver synthetic failure, and muscular hypotonia leading to respiratory failure and death in early infancy. They also showed brain abnormalities including cerebellar and pontine hypoplasia, hypoplastic corpus callosum, and hypomyelination. Muscle disease with high creatine kinase was present also in other patients with a milder phenotype. They also had, in various combinations, developmental delay, behavioral abnormalities, myelination delay, strabismus, coagulopathy, and liver disease. One patient had hepatocellular carcinoma, and there is some evidence that this disease carries increased risk for this malignancy.
Adenosine kinase deficiency has been described so far in 19 patients. All had severe developmental delay, hypotonia, and frontal bossing. The majority had hypertelorism, failure to thrive, epilepsy, macrocephaly, neonatal jaundice, and liver disease with elevated aminotransferases. About half of patients had cardiac anomalies (Staufner et al. 2016; Alhusani et al. 2019).
Cystathionine beta-synthase (CBS) deficiency is clinically variable and characterized primarily by an increased risk of thrombosis—predominantly in venous beds—and pulmonary embolism and in more severe forms by osteoporosis, lenticular myopia and lens dislocation, developmental delay, and cognitive impairment (Mudd et al. 1985). About half of patients are pyridoxine responsive with a less severe disease (Morris et al. 2017).
Cystathionase deficiency is considered a benign condition (Kraus et al. 2009) although it was originally described in patients with psychomotor retardation and other neurological findings.
Methanethiol oxidase (MTO) deficiency has been described in only five patients with cabbage-like breath odor (extraoral halitosis) due to accumulation of methanethiol and dimethylsulfide (Pol et al. 2018).
Isolated sulfite oxidase deficiency is characterized by refractory convulsions starting in the neonatal or early infantile period, severe psychomotor retardation, brain imaging findings resembling hypoxic-ischemic encephalopathy with development of cysts, and early death. Lens dislocation occurs usually after the neonatal period. Milder and late-onset cases have been reported (Claerhout et al. 2018; Bindu et al. 2017, see Online resources).
Persulfide dioxygenase (PDO) deficiency or ethylmalonic encephalopathy (ETHE1) is a severe disorder manifesting in seizures, developmental delay and cognitive impairment, orthostatic acrocyanosis and petechia due to vasodilation, failure to thrive, and chronic hemorrhagic diarrhea (Di Meo et al. 2017, see Online resources).
Mercaptopyruvate sulfur transferase (MPST) deficiency and/or excretion of the mercaptolactate has been reported in two patients with mental retardation (Ampola et al. 1969); however, subsequently no association with cognitive impairment was reported.
Nomenclature
No. | Disorder | Alternative name | Abbreviation of the disease/deficiency | Gene symbol | Chromosomal localization | Mode of inheritance | Affected protein | OMIM No. | Subtype |
|---|---|---|---|---|---|---|---|---|---|
Methionine adenosyltransferase I/III deficiency | MAT deficiency | MAT I/III | MAT1A | 10q22 | AR | Methionine adenosyltransferase I/III | 250850 | Potentially symptomatic form | |
Methionine adenosyltransferase I/III deficiency | MAT deficiency | MAT I/III | MAT1A | 10q22 | AD | Methionine adenosyltransferase I/III | 250850 | Benign form | |
Methionine adenosyltransferase II deficiency | S-adenosylmethionine synthase isoform type 2 deficiency; MATII deficiency | MATII | MAT2A | 2p11.2 | AD | Methionine adenosyltransferase II alpha | 601468 | Potentially symptomatic | |
Glycine N-methyltransferase deficiency | GNMT deficiency | GNMT | GNMT | 6p12 | AR | Glycine N-methyltransferase | 606664 | All forms | |
S-adenosylhomocysteine hydrolase deficiency | SAHH deficiency | AHCY | AHCY | 20q11.22 | AR | Adenosylhomocysteinase, S-adenosylhomocysteine hydrolase | 613752 | All forms | |
Adenosine kinase deficiency | Hypermethioninemia due to adenosine kinase deficiency | ADK | ADK | 10q22.2 | AR | Adenosine kinase | 614300 | All forms | |
Cystathionine beta-synthase deficiency | Classical homocystinuria | CBS | CBS | 21q22.3 | AR | Cystathionine beta-synthase | 263200 | All forms | |
Cystathionase deficiency | Cystathionine gamma-lyase deficiency | CTH | CTH | 1p31.1 | AR | Cystathionine gamma-lyase | 219500 | All forms (probably benign) | |
Methanethiol oxidase deficiency | Extraoral halitosis, MTO deficiency | MTO | SELENBP1 | 1q21.3 | AR | Methanethiol oxidase | 604188 | All forms | |
Sulfite oxidase deficiency | Isolated sulfite oxidase deficiency | SUOX | SUOX | 12q13.13 | AR | Sulfite oxidase | 272300 | Isolated | |
Mitochondrial sulfur dioxygenase deficiency | Ethylmalonic encephalopathy | ETHE1 | ETHE1 | 19p13.32 | AR | Mitochondrial persulfide dioxygenase | 602473, 608451 | All forms | |
Mercaptopyruvate sulfur transferase deficiency | β-Mercaptolactate cysteine disulfiduria | MPST | MPST | 22q12.3 | AR | Mercaptopyruvate sulfur transferase | 602496 | All forms (probably benign) |
Metabolic Pathway
Metabolism of sulfur amino acids is summarized in Fig. 22.1. Methionine and homocysteine are linked by the remethylation cycle (see Chap. 28 for details) and the transsulfuration pathway. The essential amino acid methionine is derived from the diet or catabolism of proteins. Methionine is first converted to S-adenosylmethionine by two methionine S-adenosyltransferases, the ubiquitously expressed MATII and liver-expressed MATI/III encoded by MAT2A and MAT1A genes, respectively. S-adenosylmethionine (AdoMet) is the methyl-group donor in a wide range of transmethylation reactions including DNA methylation, creatine, and neurotransmitter synthesis, and surplus amounts are converted to sarcosine by glycine N-methyltransferase. The transfer of methyl groups from AdoMet yields S-adenosylhomocysteine, which is a strong inhibitor of transmethylation reactions and must be cleaved to adenosine and homocysteine by S-adenosylhomocysteine hydrolase. Depending on a number of factors, about half of available homocysteine is recycled into methionine by the folate and cobalamin-dependent remethylation cycle, while the other half is channeled into the transsulfuration pathway. In the latter series of reactions, homocysteine is condensed with serine to form cystathionine via a reaction catalyzed by the pyridoxal phosphate-requiring cystathionine ß-synthase. Cystathionine is cleaved to cysteine, α-ketobutyrate, and ammonia by another pyridoxal phosphate-dependent enzyme, γ-cystathionase. Cysteine is an important precursor for the synthesis of glutathione and taurine and the major source for endogenous production of the signaling molecule hydrogen sulfide. The sulfur atom of cysteine can be fully oxidized to sulfate via two major pathways. Cysteine can be converted to cysteine sulfinic acid by cysteine dioxygenase followed by transamination with α-oxoglutarate yielding pyruvate and sulfite, although cysteine sulfinate can be also decarboxylated and give rise to hypotaurine and finally to taurine. The other pathway utilizes cysteine for the synthesis of the gasotransmitter hydrogen sulfide by catalysis of CBS, CTH, MPST, and cysteinyl-tRNA synthetase; hydrogen sulfide exists in a dynamic equilibrium of dissolved gas, hydrosulfide, and various organic and inorganic polysulfides. Oxidation of hydrogen sulfide occurs in mitochondria and starts with persulfidation of GSH by sulfide:quinone oxidoreductase, followed by release of sulfite under the catalysis of ETHE1. Sulfite is finally oxidized by the molybdenum cofactor-containing sulfite oxidase to the ultimate oxidation product sulfate.
Signs and Symptoms
Reference Valuesa
Analyte | Infant <1 year | Child 1–12 years | Adolescent 12–18 years | Adult >18 years |
|---|---|---|---|---|
Plasma amino acids (μmol/L) | ||||
Methionine | 12–31 | 11–30 | 16–23 | 15–40 |
Homocystine | Below detection limit (approx. 5 μmol/L) | |||
Cystathionine | Below detection limit (approx. 5 μmol/L) | |||
Taurine | 15–200 | 19–139 | 10–162 | 6–126 |
S-sulfocysteine | Below detection limit (approx. 5 μmol/L) | |||
Special assays in plasma or blood (in blood where indicated in brackets) (μmol/L) | ||||
Total homocysteine | 3.5–10 | 4–10 | 4–13 | 5–15 |
Total cysteine | 200–360 (not age stratified) | |||
Sarcosine | 0.6–2.5 (not age stratified) | |||
S-adenosylmethionine | 0.03–0.16 (not age stratified) | |||
S-adenosylhomocysteine | 0.015–0.06 (not age stratified) | |||
Cystathionine (by sensitive GC-MS or LC-MS/MS assays) | 0.08–0.5 (up to 1 in neonates) | |||
Methionine-to-cystathionine ratio | 40–200 (not age stratified) | |||
Thiosulfate | 0.4–0.7 (not age stratified) | |||
Sulfite | 0.2–0.5 (not age stratified) | |||
Free sulfide (hydrogen sulfide) | 0.15–0.3 (not age stratified) | |||
Dimethylsulfide (blood) | <0.007 (not age stratified) | |||
Dimethylsulfoxide (blood) | <1 (not age stratified) | |||
Lactate (blood) | Reference ranges for lactate in blood are shown in Chap. 42 of this book | |||
Dried blood spots (μmol/L blood) | ||||
Methionine | 7–40 (not age stratified) | |||
Methionine/phenylalanine | 0.15–0.6 | |||
Total homocysteine | 2.5–9 | 5.5–9 | 8–13 | |
Methionine-to-total homocysteine ratio | 2–4 (not age stratified) | |||
Reference ranges for acylcarnitines in dried blood spots are shown in Chap. 5 of this book | ||||
Urinary amino acids (mmol/mol creatinine) | ||||
Methionine | 7–29 | 5–20 | 3–17 | 2–16 |
Cystathionine | Usually below detection limit (not age stratified) | |||
Homocystine | 0.2–3.7 (not age stratified) | |||
Reference ranges for organic acids in urine are shown in Chap. 4 of this book | ||||
Urinary special assays (mmol/mol creatinine) | ||||
Total cysteine | 10–50 (not age stratified) | |||
Total homocysteine | 1–4 (not age stratified) | |||
Thiosulfate | 0.8–2.5 (not age stratified) | |||
Sulfite | 0.03–0.15 (not age stratified) | |||
S-sulfocysteine | 0.3–1 (not age stratified) | |||
Simple tests in urine (qualitative test) | ||||
Nitroprusside test | Negative (not age stratified) | |||
Exhaled air (ppb) | ||||
Dimethylsulfide | 1–19 (not age stratified) | |||
Methanethiol | 0.01–0.24 (not age stratified) | |||
Pathological Valuesa,b,c
Metabolites | 22.1b MAT I/III | 22.3 GNMT | 22.4 SAHH | 22.5 ADK | 22.6 CBS | 22.7 CTH | 22.8 MTO | 22.9 SUOX | 22.10 ETHE1 | 22.11 MPST |
|---|---|---|---|---|---|---|---|---|---|---|
Plasma amino acids | ||||||||||
Methionine | ↑↑↑ | ↑↑↑ | n-↑↑ | n-↑↑↑ | n-↑↑↑ | n | n | |||
Homocystine | ↑-↑↑↑ | |||||||||
Cystathionine | ↑ | |||||||||
Taurine | ↑-↑↑ | ↑ | ||||||||
S-sulfocysteine | ↑-↑↑ | |||||||||
Plasma acylcarnitines | ||||||||||
C4 butyrylcarnitine | ↑↑ | |||||||||
C4 isobutyrylcarnitine | ↑ | |||||||||
C5 2-methylbutyrylcarnitine | ↑ | |||||||||
C5 isovalerylcarnitine | ↑ | |||||||||
Glutarylcarnitine | ↑ | |||||||||
Special assays in plasma or blood (in blood where indicated in brackets) | ||||||||||
Total homocysteine | n-↑ | n-↑ | n-↑ | n-↑ | ↑-↑↑↑ | n-↑ | ↓ | n-↓ | ||
Total cysteine | ↓↓ | n | ↓ | |||||||
Sarcosine | n-↑ | n | n-↑ | ↑-↑↑ | ||||||
S-adenosylmethionine | n-↓ | ↑↑↑ | ↑↑↑ | ↑-↑↑ | ↑↑ | |||||
S-adenosylhomocysteine | ↑↑↑ | ↑-↑↑ | ↑-↑↑ | |||||||
Cystathionine (by sensitive GC-MS or LC-MS/MS assays) | n-↓↓ | ↑↑↑ | ||||||||
Methionine-to-cystathionine ratio | ↑↑ | ↑-↑↑↑ | ↓↓ | |||||||
Thiosulfate | ↑↑ | ↑↑ | ||||||||
Sulfite | ↑↑ | ↑↑ | ||||||||
Free sulfide (hydrogen sulfide) | ↑ | ↑↑ | ||||||||
Lactate (blood) | ↑ | |||||||||
Dimethylsulfoxide (blood) | ↑↑ | |||||||||
Dimethylsulfide (blood) | ↑↑ | |||||||||
Dried blood spots | ||||||||||
Methionine | ↑↑-↑↑↑ | n-↑↑ | ||||||||
Methionine/phenylalanine | ↑↑-↑↑↑ | n-↑↑ | ||||||||
Total homocysteine | n | ↑-↑↑↑ | ||||||||
Methionine-to-total homocysteine | ↑↑ | ↓ | ||||||||
Adenosine | n-↑ | |||||||||
C4 butyrylcarnitine | ↑↑ | |||||||||
C4 isobutyrylcarnitine | ↑ | |||||||||
C5 2-methylbutyrylcarnitine | ↑ | |||||||||
C5 isovalerylcarnitine | ↑ | |||||||||
Glutarylcarnitine | ↑ | |||||||||
Urinary amino acids | ||||||||||
Methionine | ↑↑↑ | ↑↑↑ | n-↑↑ | ↑↑ | n-↑↑ | |||||
Cystathionine | n-↓ | ↑↑ | ||||||||
Homocystine | ↑-↑↑↑ | |||||||||
Organic acids in urine | ||||||||||
Ethylmalonic acid | ↑↑-↑↑↑ | |||||||||
2-Methylbutyrylglycine | ↑↑ | |||||||||
Methylsuccinic acid | ↑↑ | |||||||||
Isovalerylglycine | ↑ | |||||||||
Urinary special assays | ||||||||||
Total homocysteine | ↑-↑↑↑ | n-↑ | ||||||||
Thiosulfate | ↑↑↑ | ↑↑ | ||||||||
Sulfite | ↑↑↑ | ↑↑ | ||||||||
S-sulfocysteine | ↑-↑↑ | n-↑ | ||||||||
Adenosine | n-↑ | |||||||||
Alpha-aminosemialdehyde | ↑ | |||||||||
Mercaptolactate, mercaptopyruvate | ↑↑ | |||||||||
Mercaptocysteine disulfide | ↑↑ | |||||||||
Simple tests in urine | ||||||||||
Nitroprusside testd | Positive | Positive | ||||||||
Exhaled air | ||||||||||
Dimethylsulfide | ↑↑ | |||||||||
Methanethiol | ↑↑ | |||||||||
Special assays in cerebrospinal fluid | ||||||||||
Pipecolic acid | ↑ | |||||||||
Pyridoxal 5′-phosphate | ↓ | |||||||||
Diagnostic Flowcharts
Since most of the mentioned diseases are at least partly treatable if diagnosed early and may have rapid course, the diagnostic work-up in suspected cases should also be rapid. Suspicion should be raised in all patients having unexplained neurological symptoms, muscle disease, liver disease, lens dislocation and other marfanoid features, orthostatic acrocyanosis, or any other symptom attributable to diseases from this group or unexplained hypermethioninemia and/or hyperhomocysteinemia or hypohomocysteinemia (see Sect. 22.4). Measurement of plasma total homocysteine and amino acids (methionine, taurine, and S-sulfocysteine) and special tests for sarcosine, cystathionine, S-adenosylmethionine, and S-adenosylhomocysteine should be sufficient as the first step to detect all diseases from this group; sulfite and thiosulfate analysis is necessary for diagnosing disorders in the distal part of transsulfuration pathway (for differential diagnosis of hypermethioninemia and hypo- and hyperhomocysteinemia, see Diagnostic flowcharts, Figs. 22.2 and 22.3).
Diagnostic flowchart for hypo- (a) and hyperhomocysteinemia (b). * tHcy range of 5–15 μmol/L is used here as reference range for all ages; actually, in children the upper limit of reference range is lower (see Reference Values). ** In non-treated CBS deficiency, tHcy is usually significantly >50 μmol/L but may be lower in mild cases, in particular when on vitamin supplementation (even non-pharmacological doses of pyridoxine). *** In non-CBS hypermethioninemias, tHcy is usually normal or only mildly elevated, and values of about 50 μmol/L are exceptionally seen. **** In ADK and SAHH deficiency, plasma methionine concentrations can occasionally be normal, for instance, in SAHH deficiency in early infancy during lower methionine intake and higher needs for growth. ***** Cystathionine for differential diagnosis of hyperhomocysteinemia cannot be detected by amino acid analyzers and must be determined by sensitive GC-MS or LC-MS/MS assay. ****** This disease has been reported in only few patients (for details, see Chap. 16), and all abnormalities are not necessarily present in all patients. Mild hypohomocysteinemia (below 3.5–5 μmol/L) is sometimes seen without association with a particular disease. ADK adenosine kinase, AdoHcy S-adenosylhomocysteine, AdoMet S-adenosylmethionine, CBS cystathionine beta synthase, GNMT glycine N-methyltransferase, G6PD glucose-6-phosphate dehydrogenase, MAT I/III methionine adenosyltransferase I/III, Met methionine, MoCo molybdenum cofactor, MTHFR methylenetetrahydrofolate reductase, NFE2L2 nuclear factor, erythroid 2 like 2, NRF2 nuclear factor-erythroid 2-related factor 2, SAHH S-adenosylhomocysteine hydrolase, SUOX sulfite oxidase, tHcy plasma total homocysteine
Diagnostic flowchart in patients with hypermethioninemia. *In untreated CBS deficiency, tHcy is usually >50 μmol/L but may be lower in mild cases, in particular when on vitamin supplementation (non-pharmacological doses). **In non-CBS deficiency hypermethioninemias, tHcy is usually normal or only mildly elevated, and values of about 50 μmol/L are rarely seen. ***Tyrosine can be elevated. ADK adenosine kinase, AdoHcy S-adenosylhomocysteine, AdoMet S-adenosylmethionine, CBS cystathionine beta synthase, GNMT glycine N-methyltransferase, MAT I/III methionine adenosyltransferase I/III, mtDNA mitochondrial DNA, SAHH S-adenosylhomocysteine hydrolase, tHcy plasma total homocysteine
It is useful to keep in mind that in MAT I/III deficiency homocysteine can be sufficiently elevated to mimic CBS deficiency, probably due to less than normal stimulation of CBS by low AdoMet and inhibition of betaine-homocysteine methyltransferase, N5-methyltetrahydrofolate-homocysteine methyltransferase and cystathionine gamma-lyase by methionine, in particular in patients with very high methionine values (Stabler et al. 2002). Mild elevations of tHcy, which can be diagnostically misleading, have also been described in other methylation defects and in CTH deficiency.
Pyridoxine responsiveness test in CBS deficiency. This test is performed in patients with CBS deficiency to assess pyridoxine responsiveness. Recent guidelines recommended standard tests in patients detected symptomatically using 10 mg/kg/day pyridoxine (maximum of 500 mg/day) for 6 weeks; the plasma tHcy concentration should be measured at least twice before treatment and twice on treatment (by the end of weeks 2 and 6). The test should be done on normal protein intake, folate supplements should be given, and vitamin B12 deficiency should be corrected prior to testing. Classification of pyridoxine responsiveness is as follows: full responsiveness, plasma tHcy levels below 50 μmol/L; extreme responsiveness, tHcy below 50 μmol/L on pyridoxine doses <1 mg/kg/day; partial responsiveness, tHcy falls >20% of pre-test average but above 50 μmol/L; and non-responsiveness, tHcy falls by <20% (Morris et al. 2017).
Loading Test
Increase of plasma dimethylsulfone and dimethylsulfoxide in methionine loading test in patients suspected to suffer from extraoral halitosis due to methanethiol oxidase deficiency can point to the cause of the disease. The methionine loading test became obsolete in diagnosis of sulfur-containing amino acids disorders.
Specimen Collection
Overview on required samples for metabolite, enzyme, and mutation analysis
Disorder | Metabolite: sample |
|---|---|
Amino acids (including taurine): plasma or seruma and urine | |
Organic acids: urine | |
Acylcarnitines: dried blood spots and plasma/serum | |
Special assays | |
CBS, CTH, SUOX | Total homocysteine and total cysteine: plasmab and urine |
MATI/III, GNMT, ADK, CBS | S-adenosylmethionine: plasmac, whole blood |
MATI/III, GNMT, ADK, CBS | S-adenosylhomocysteine: plasmac, whole blood |
SUOX, ETHE | Thiosulfate: plasma and urined,e |
SUOX, ETHE | Sulfite: plasma and urined,e |
SUOX, ETHE | Free sulfide (hydrogen sulfide): plasmad |
MTO | Methanethiol and dimethylsulfide in exhaled air |
CBS | Methionine, Met/Phe and tHcy in dried blood spots |
Other assays: plasma, blood or urine (may require special sampling conditions, consult the laboratory) | |
Enzyme assaysf: specimen | |
MAT I/III | Liverg |
GNMT | Liverg |
SAHH | Cultured fibroblasts, erythrocytes, liver |
ADK | Not available |
CBS | Cultured fibroblasts and plasmaa |
CTH | Liverg |
SUOX | Cultured fibroblasts |
ETHE1 | Not available |
MPST | Erythrocytes |
MTO | Erythrocytes |
Mutation analysis | |
All disorders | DNA |
Prenatal Diagnosis
Prenatal diagnosis is only relevant for SAHH, ADK, CBS, ETHE1, and SUOX deficiencies. Generally the first choice of method for each of these is mutation analysis in chorionic villous material provided that disease-causing mutations and their parental origin have been confirmed. Alternatively, enzyme assay in cultured amniocytes can be performed in some diseases.
DNA Testing
All genes in this chapter are known, and mutation analysis of genomic DNA isolated from peripheral blood, chorionic villi, amniocytes, or other cells is feasible. Sanger sequencing of individual genes or next-generation sequencing of gene panels are used. For mutations suspected to affect splicing, mRNA analysis in appropriate tissues may be necessary.
Treatment Summary
The general treatment goal for disorders of sulfur amino acid and hydrogen sulfide metabolism is correcting biochemical abnormalities in order to suppress their adverse effects. This causal treatment primarily consists in various combinations of high doses of cofactors, low-protein or low-methionine or low-cysteine diet, and supplementation of metabolites behind the enzymatic block. Betaine is an additional means to decrease homocysteine concentration.
In MAT I/III deficiency, methionine restriction is indicated in symptomatic patients and those with brain imaging changes. It is justified also in asymptomatic patients with severe deficiency and plasma methionine >500–800 μmol/L. AdoMet supplementation may be necessary. It seems that GNMT deficiency, cystathionase deficiency, and autosomal dominant MATI/III deficiency do not require treatment. In AdoHcy hydrolase deficiency, low-methionine diet can decrease plasma AdoMet and AdoHcy, with a positive effect on methylation and clinical and biochemical abnormalities (Barić et al. 2005). Phosphatidylcholine, creatine, and cysteine supplementation may be useful. Liver transplantation seemed beneficial in one patient with short follow-up. CBS-deficient patients are treated with varying doses of pyridoxine if responsive in the pyridoxine test. Folate and cobalamin should be added to avoid vitamin depletion and stimulate homocysteine remethylation. Betaine and/or a low-methionine diet (sometimes with methionine-free/cystine-enriched amino acid mixture) may also be needed in partial responders but necessary in pyridoxine nonresponsive patients. In isolated sulfite oxidase deficiency, partial success with low-protein diet combined with methionine- and cysteine-free amino acid mixture has been reported only in late-onset patients (Touati et al. 2000). Low methionine diet may ameliorate the liver phenotype in adenosine kinase deficiency. For MATII deficiency and mercaptopyruvate sulfurtransferase deficiency, no successful causal treatment has been reported. In ethylmalonic encephalopathy, metronidazole and N-acetylcysteine may reduce some symptoms. Early liver transplantation may be an option to reverse otherwise unfavorable outcome. In MTO deficiency, metronidazole can reduce methanethiol production by gut bacteria.
Emergency Treatment
Methionine Adenosyltransferase I/III Deficiency (AR and ADa forms)
If unexplained neurological signs are present with very high methionine level, discontinuance of methionine intake for 1–3 days followed by low-methionine diet until symptoms disappear, in combination with AdoMet supplementation (for instance, at a dose of 400 mg twice daily, Surtees et al. 1991), seems to be indicated. See also the comment b below the standard treatment table.
S-Adenosylhomocysteine Hydrolase Deficiency
Severe cases, such as those presenting with fetal hydrops, insufficiency of liver synthetic function, and severe muscular hypotonia leading to respiratory insufficiency, may potentially benefit from strict methionine restriction and choline and cysteine supplementation in combination with vigorous symptomatic treatment.
Ethylmalonic Encephalopathy
Continuous renal replacement therapy may help to reestablish metabolic control during acute metabolic decompensations in patients on chronic treatment with N-acetylcysteine and metronidazole (Kitzler et al. 2019).
For other disorders from this group, emergency situations amenable to specific disease-related emergency treatment are not likely. A diet low in protein and an amino acid mixture without cystine and methionine may be helpful in mild sulfite oxidase deficiency.
Standard Treatment
Disease | Comment | Medication/diet | Dosagea | Goals |
|---|---|---|---|---|
22.1 MAT I/III deficiency | For the autosomal dominant form of the disease, treatment does not seem to be indicated For the autosomal recessive form, if plasma methionine concentrations are above risky level (clear risk above 800 μmol/L, existing risk above 500–600 μmol/L), a methionine-restricted diet is recommended If the mean plasma methionine is below 500–600 μmol/L, treatment does not seem to be indicated | Low-methionine diet | In infancy ~15–20 mg of methionine/kg/day; later less as expressed in mg/kg/day and according to clinical and biochemical parameters | Disappearance/prevention of clinical symptoms Normalization of brain imaging findings The aim of the diet is to maintain methionine levels around 500–600 μmol/L, even in asymptomatic individuals It should be borne in mind that lowering plasma methionine below 500 μmol/L in patients with some residual MAT I/III activity may further limit the flux through MAT I/III and further decrease the availability of AdoMet (Mudd et al. 2001) |
AdoMet supplementation, especially if methionine intake is limited, may be necessary | S-adenosylmethionine | 2–3 × 400 mg daily per osb | Clinical improvement, normalization of plasma and/or CSF AdoMet; normalization of hyperhomocysteinemia | |
22.2 Methionine adenosyltransferase II deficiency | No causal treatment; surgery and other measures according to risk assessment of thoracic aorta aneurysm development | |||
22.3 GNMT deficiency | There is no evidence that therapy is necessary; low-methionine diet can correct biochemical abnormalities. It may be indicated when plasma methionine reaches values above 500–600 μmol/L, which may be risky regardless of cause | Low-methionine diet | In infancy ~15–20 mg of methionine/kg/day; later less as expressed in mg/kg/day and according to clinical and biochemical parameters | Correction of biochemical abnormalities and potential neurological problems due to high hypermethioninemia |
22.4 AHCY deficiency | Due to small number of patients, these recommendations are based only on pathogenetic hypotheses and limited clinical experience Liver transplantation seemed beneficial in one patient with a short follow-up | Low-methionine diet | In infancy natural protein intake containing ~10–20 mg/kg/day of methionine, depending on the severity of the disease and biochemical findings, in combination with methionine-free amino acid mixture to meet needs for proteins | Clinical improvement and decrease of AdoMet and AdoHcy as close to normal values as possible, while avoiding protein malnutrition |
Phosphatidylcholine | 3 × 600–1200 mg/day | Avoidance of possible phosphatidylcholine and choline deficiency | ||
N-acetylcysteine | 3 × 100–200 mg/day | Avoidance of possible glutathione deficiency | ||
Creatine (may be useful theoretically) | 3–5 g/day | Avoidance of possible creatine deficiency | ||
22.5 ADK deficiency | Low methionine diet should be considered as a therapeutic option, since it ameliorates the liver phenotype clinically and biochemically. Positive effect on the neurological outcome has only been reported in a single case. Diazoxide is recommended for recurrent hypoglycemia when it is due to hyperinsulinism (Barić et al. 2017) | Low methionine diet | Daily intake of 15–20 mg of methionine per kg of body weight in infants and small children; later less as expressed in mg/kg/day and according to clinical and biochemical parameters | Improvement of clinical and biochemical indices of liver disease |
22.6 CBS deficiencyc | Test of pyridoxine responsiveness should be done on normal protein intake at the beginning of the treatment (for details, see above) Before test possible folate and cobalamin deficiency should be corrected to assure proper assessment of the test results | A. Pyridoxine responders and partial responders | Clinical targets: For early diagnosed patients, prevention of all the complications of CBS deficiency while maintaining normal growth and nutrition For late-diagnosed patients, prevention of further complications, especially thromboembolic disease Biochemical targets: Maintenance of tHcy concentration as close to normal as possible. In fully responsive patients, standard doses can lead to tHcy levels below 50 μmol/L (and sometimes within the normal range in extreme responsive patients). Some patients who are partially responsive to pyridoxine may be able to achieve a tHcy level below 50 μmol/L if they are also on a low-Met diet; for others it is not a realistic goal. Excessive methionine restriction, with plasma methionine concentrations that are sometimes below the normal range, may impair growth and neurodevelopmental progress in children. In pyridoxine unresponsive patients, it is recommended to keep tHcy levels at least below 100 μmol/L, but this may need revision when very long-term data become available (Morris et al. 2017). Plasma methionine levels in patients treated with betaine should be kept below 800 μmol/L (it is probably safer below 500–600 μmol/L) | |
Pyridoxine | The pyridoxine dose should be the lowest that achieves the biochemical targets. Recommended doses are up to 10 mg/kg/day divided into 1–3 doses; doses above 500 mg/day should be avoided | |||
Folated | Optimal dose is not known; up to 1 mg/day is probably sufficient if folate deficiency is not present | |||
Hydroxocobalamin | Vitamin B12 should be monitored and supplemented if deficient | |||
Low-methionine diet (for partially responsive patients only) | The degree of methionine or natural protein restriction required varies and is determined for each patient according to their plasma tHcy, methionine, and other parameters | |||
Betaine (for partially responsive patients only) | Patients’ responses to betaine are variable and optimal doses have to be individualized. For children, the initial betaine dose is 50 mg/kg twice daily. For adults, the starting dose is 3 g twice a day. The dose and frequency are adjusted according to response. There is unlikely to be any benefit in exceeding a dose of 150–200 mg/kg/day | |||
Guidelines for protein intake in methionine-restricted diet are very approximate. Diet must be adjusted, in combination with other measures, to achieve therapeutic goal, if possible, but should not jeopardize the patient; therefore strict monitoring of growth and nutritional indices (including aromatic and branched chain amino acids) is necessary | B. Pyridoxine nonresponders | |||
There is no evidence that long-term pyridoxine is beneficial if there is no biochemical response in a properly conducted test (Morris et al. 2017) | ||||
Folated | Optimal dose is not known; less than 1 mg/day is probably sufficient if folate deficiency is not present | |||
In nearly all CBS-deficient patients, high remethylation activity may lead to folate and/or cobalamin depletion; therefore, folate and cobalamin should be added to the therapy | Cobalamin | Vitamin B12 should be monitored and supplemented if deficient | ||
Low-methionine diet | Patients may require only isolated mild protein/methionine restriction or more severe restriction combined with amino acid mixture administration. The combined intake of low natural protein and methionine-free/cystine-enriched amino acid mixture (total protein equivalent) should follow the WHO/FAO recommendations (Joint FAO/WHO/UNU Expert Consultation on Protein and Amino Acid Requirements in Human Nutrition 2007). Methionine intake in natural protein depends on age and should be adjusted to maintain plasma tHcy levels <100 μmol/L while avoiding protein over-restriction. This can be typically achieved by prescribing 0.4–1.0 g natural protein/kg/day; however, higher or lower intake may be needed. If diet is based on calculation of methionine intake, appropriate amount may be between 4 and 10 mg/kg/day, with higher needs in infancy, particularly early infancy | |||
Betaine | See pyridoxine responders | |||
22.7 CTH deficiency | The disorder seems benign and therapy unnecessary | |||
22.8 Methanethiol oxidase deficiency | There is no standard treatment for this recently described disease, and options provided are based on pathogenesis (low methionine diet, metronidazole) and short trial in a single patient (metronidazole), respectively (Pol et al. 2018). Although an effect is expected from metronidazole, it is not recommended as prophylactic treatment | Metronidazole | Metronidazole: children 20–30 mg/kg/day three times daily; adults 400 mg three times daily (doses provided here are those usually used for anaerobic infections and for this indication may depend on the effect, occasion, and duration of the therapy/prophylaxis) Low-protein/low methionine diet can be considered but should not be over-restrictive so that methionine intake carefully adjusted to avoid harmful effects | To minimize the malodor while avoiding side effects |
Low-protein/low methionine diet | ||||
22.9 Isolated SUOX deficiency | The treatment has been useful only in milder forms of the disease. The diet must be carefully monitored to avoid protein malnutrition. Thiamine and pyridoxine can be added to avoid thiamine and pyridoxal-5-phosphate deficiency due to sulfite accumulation | Low-methionine and low-cysteine diet | Dependent on age and biochemical markers of the disease and protein status | Clinical improvement, decrease of toxic metabolites (S-sulfocysteine, thiosulfate), to limit excitotoxicity (dextromethorphan) |
Dextromethorphan (NMDA receptor antagonist) | Dextromethorphan: 12.5 mg/kg daily (dosage reported in patient with molybdenum cofactor deficiency; largely variable dosage has been reported in nonketotic hyperglycinemia) | |||
22.10 Ethylmalonic encephalopathy | Metronidazole and N-acetylcysteine may improve metabolic abnormalities (decrease H2S accumulation and the sulfur atom from H2S, respectively), reduce some symptoms, and slow disease progression | Metronidazole N-acetylcysteine | Metronidazole 25–50 mg/kg/day three times daily N-acetylcysteine 50–100 mg/kg/day in 2–3 doses | Decrease of H2S accumulation and assimilation of the sulfur atom from H2S, respectively, reducing some symptoms and slowing disease progression |
22.11 Mercaptopyruvate sulfurtransferase deficiency | This condition could be benign | Not reported | – | – |
Warning Boxes/Pitfalls
-
1.
In patients treated with low-methionine diet, careful clinical and biochemical monitoring is necessary to avoid consequences of protein malnutrition.
-
2.
Long-term folate therapy in high doses may be associated with increased cancer risk.
-
3.
There is a high risk of peripheral neuropathy following long-term treatment with pyridoxine doses above 900 mg/day, but it has not been found in patients treated with less than 500 mg/day. In children, the safe dose is likely to depend on body weight; there are few data but last guidelines suggest using doses up to 10 mg/kg/day, with a maximum of 500 mg/day (Morris et al. 2017).
-
4.
A major potential problem of betaine therapy in CBS deficiency and other disorders with both elevated tHcy and methionine is potential increase of methionine to the concentrations that may be toxic for the brain, leading to cerebral edema and other consequences of excessive hypermethioninemia described above.
-
5.
Accidental inhalation of betaine in powder form can cause pulmonary problems.
Experimental Treatment
For CBS deficiency, molecular chaperones have been investigated in proof of principle studies, while enzyme replacement therapy is in phase I/II of a clinical trial.
For ethylmalonic encephalopathy, early liver transplantation may be an option to reverse otherwise poor outcome (Dionisi-Vici et al. 2016). Diet restricted in sulfur-containing amino acids may contribute to better outcome in patients detected by newborn screening, particularly if liver transplantation would be proven as an option. In some patients, improvement in some symptoms has been observed with ubiquinone and/or riboflavin.
Follow-Up and Monitoring
Recommendations given in the table are only approximate guidelines and should be adjusted individually according to age, severity of the disease, compliance, and other factors.
Disease | Clinical follow-up and monitoring | Biochemical follow-up and monitoring |
|---|---|---|
22.1 MAT I/III deficiency | Both for untreated patients and those on therapy: any neurological sign or symptom should be considered as a possible sign of the disease and reason for further clinical (including brain imaging) and metabolic evaluation. Therefore, neurological and cognitive evaluation should be performed regularly in all patients with the risk of grossly elevated plasma methionine (clear risk above 800 μmol/L and existing risk above 500–600 μmol/L). In these patients neurological testing should take place about once every 2–3 months in infants and every 6–12 months later in life. If indicated, brain MRI should be performed (Chien et al. 2015). For patients on low-methionine diet, additionally, signs of protein malnutrition should be regularly looked for | In untreated patients without symptoms, checking of methionine, AdoMet, and total homocysteine (tHcy) is justified. The frequency depends on the severity of enzyme deficiency and mode of inheritance. The autosomal dominant form of MAT I/III deficiency is considered benign and does not require regular biochemical monitoring. In patients with the autosomal recessive form of the disease with severe enzyme deficiency and previous plasma methionine close to 500 μmol/L or more, or abnormal tHcy values, checking should be more frequent (i.e., in infancy every 3 months, later every 3–12 months and after significant changes in dietary methionine intake). In patients with the autosomal recessive form and mild enzyme deficiency, if highest plasma methionine values, which should be checked after normal and high protein intake, are not close to 500 μmol/L, only sporadic checking of plasma methionine is indicated, i.e., when symptoms attributable to MAT I/III deficiency appear. In patients on low-methionine diet, regular monitoring of protein status and plasma amino acids is indicated (in infancy at least every 3 months, later every 6–12 months and after significant changes in dietary methionine intake). In hyperhomocysteinemic patients in similar intervals, tHcy should be measured and thrombophilia screen should be performed at least once |
22.2 MAT II deficiency | In individuals with MAT2 mutations, regular cardiac evaluation by ultrasound and if needed other methods to check for possible development of thoracic aorta dilatation are indicated | Not possible due to the lack of biochemical markers |
22.3 GNMT deficiency | In GNMT-deficient patients tending to have very high plasma methionine levels which have been related to central nervous system complications (see MAT I/III deficiency above), regular neurological and cognitive testing is justified. aYearly liver ultrasound seems justified | Due to possible hypermethioninemia-related problems, plasma methionine checking in regular intervals is recommended (in infancy every 3 months, if indicated even more frequently, later every 6–12 months or depending on previous values). Liver function tests, alpha-fetoproteina |
22.4 AHCY deficiency | Careful evaluation of all body systems, particularly of the nervous system and development, muscles, liver, and coagulation. In infancy every 1–3 months, if indicated even more frequently, later every 3–6 months. This includes imaging studies, particularly regular liver imaging | Careful biochemical monitoring is mandatory to control both disease development and treatment to avoid their complications. The following tests are indicated: protein status, amino acids, AdoMet, AdoHcy, liver function tests, creatine kinase, alpha-fetoprotein, coagulation tests, liver imaging, while others depend on the clinical situation. Follow-up intervals depend on age and clinical course. In infancy this could be every 1–3 months, if indicated even more frequently, later every 3–6 months |
22.5 ADK deficiency | Careful clinical evaluation with regular follow-up visits depending on age and severity is recommended (intervals ranging from 1 month to 1 year), including regular monitoring of psychomotor development and neurological examination and regular liver imaging Since epilepsy is often present in ADK deficiency, regular electroencephalography is recommended. In one patient retinal dystrophy was diagnosed; thus ophthalmological examination on a regular basis should be considered. Because of an increased incidence of cardiac defects, echocardiography should be performed in all patients and followed up accordingly. Several patients presented with cholelithiasis; thus abdominal ultrasound should be performed in cases of unexplained pain (colic) | Assays of protein status, plasma amino acids, tHcy, AdoMet, AdoHcy, adenosine in urine and/or dried blood spot, serum aminotransferases, total and direct bilirubin, ammonia, blood glucose, uric acid, coagulation tests, and alpha-fetoprotein are relevant. Regular blood glucose profiles should be performed, depending on the presence and treatment of recurrent hypoglycemia. A full blood count should be included in the regular monitoring to check for megaloblastic anemia |
22.6 CBS deficiency | The adequate frequency of monitoring depends on the severity of the disorder, treatment, compliance, age, status of the patient, and previous complications (e.g., thrombosis). Approximate schedule could be the following: Neurological and, depending on age, developmental or mental evaluation in infancy every 3 months, later every 6–12 months. Ophthalmology examination yearly. Bone mineral density once in 1–3 years. Vascular status every 6–12 months, depending on the severity of the disease and clinical course | Plasma amino acids and total homocysteine in infancy every 1–3 months, if indicated even more frequently, later every 3–6 months. If tHcy is monitored in dried blood spots, this test may be done more frequently. In patients on low-methionine diet protein status in the same intervals. Unless on supplementation, serum cobalamin and folate every 3–6 months. Thrombophilia screening should be considered once. Lipids first time at age 2–3 years, afterward, if normal, every 2–3 years, if not every 3 months alongside therapy |
22.7 CTH deficiency | Not necessary | |
22.8 MTO deficiency | Malodor can be monitored clinically. Possible related psychological burden may need psychologist’s evaluation | If metronidazole is used, caution should be taken because of possible side effects. If low-protein/low methionine diet is used, protein status should be checked to avoid methionine deficiency and/or protein malnutrition |
22.9 Isolated SUOX deficiency | General and, particularly, neurological (including EEG and imaging) and developmental evaluation in infancy every 1–3 months, later every 3–6 months, if indicated more frequently. Ophthalmology every 6 months, if indicated, more frequently | If on diet, protein status, amino acids, S-sulfocysteine, thiosulfate, sulfite in infancy every 1–3 months, if indicated more frequently, later every 3–6 months |
22.10 Ethylmalonic encephalopathy | General and, particularly, neurological (including EEG and imaging) and developmental evaluation in infancy every 1–3 months, later every 3–6 months, if indicated more frequently. Nutritional evaluation | Blood count according to blood losses in stool. Specific markers of the disease activity include lactate, plasma and urinary thiosulfate and sulfite, urinary ethylmalonate, and plasma C4- and C5-acylcarnitines. The frequency of monitoring depends on clinical condition and is more frequent in crises and/or following active treatment attempts, like liver transplantation. Otherwise it can be carried out in parallel with clinical evaluation, every 1–3 months in infancy, later every 3–6 months, if indicated more frequently |
22.11 Mercaptopyruvate sulfurtransferase deficiency | If the disease is associated with intellectual disability, regular cognitive assessment seems justified | There is no evidence that intervention in this very rare disorder is needed or effective. Specific markers would be beta-mercaptolactate cysteine disulfide (urine), mercaptopyruvate, and mercaptolactate. It is questionable if this would have practical meaning |
Online Resources
-
1.
Bindu PS, Nagappa M, Bharath RD, Taly AB (2017) Isolated sulfite oxidase deficiency.
GeneReviews® https://www.ncbi.nlm.nih.gov/books/NBK453433/ Sep21, 2017
-
2.
Di Meo I, Lamperti C, Tiranti V (2017) Ethylmalonic encephalopathy. GeneReviews® https://www.ncbi.nlm.nih.gov/books/NBK453432/ Sep21, 2017.
-
3.
Enzyme Commission numbers—http://www.chem.qmul.ac.uk/iubmb/enzyme/
-
4.
Inborn Errors of Metabolism Knowledgebase (IEMbase)—http://www.iembase.org/
-
5.
OMIM catalogue—http://www.ncbi.nlm.nih.gov/omim/
-
6.
The Online Metabolic and Molecular Bases of Inherited Disease—https://ommbid.mhmedical.com/
-
7.
Human Metabolome Database—http://www.hmdb.ca/
References
Alhusani A, Obaid A, Blom HJ, Wedell A, Alfadhel M. Adenosine kinase deficiency: report and review. Neuropediatrics. 2019;50:46–50.
Ampola MG, Efron ML, Bixby EM, Meshorer E. Mental deficiency and a new aminoaciduria. Am J Dis Child. 1969;117:66–70.
Barić I, Fumić K, Glenn B, et al. S-adenosylhomocysteine hydrolase deficiency in a human: a genetic disorder of methionine metabolism. Proc Natl Acad Sci U S A. 2004;101:4234–9.
Barić I, Ćuk M, Fumić K, et al. S-Adenosylhomocysteine hydrolase deficiency: a second patient, the younger brother of the index patient, and outcomes during therapy. J Inherit Metab Dis. 2005;28:885–902.
Barić I, Staufner C, Augoustides-Savvopoulou P, et al. Consensus recommendations for the diagnosis, treatment and follow-up of inherited methylation disorders. J Inherit Metab Dis. 2017;40:5–20.
Braverman NE, Mudd SH, Barker PB, Pomper MG. Characteristic MR imaging changes in severe hypermethioninemic states. Am J Neuroradiol. 2005;26:2705–6.
Chamberlin ME, Ubagai T, Mudd SH, Levy H, Chou JY. Dominant inheritance of isolated hypermethioninemia is associated with a mutation in the human methionine adenosyltransferase 1A gene. Am J Hum Genet. 1997;60:540–6.
Chien YH, Abdenur JE, Baronio F, et al. Mudd’s disease (MAT I/III deficiency): a survey of data for MAT1A homozygotes and compound heterozygotes. Orphanet J Rare Dis. 2015;10:99.
Claerhout H, Witters P, Régal L, Jansen K, Van Hoestenberghe MR, Breckpot J, Vermeersch P. Isolated sulfite oxidase deficiency. J Inherit Metab Dis. 2018;41:101–8.
Dionisi-Vici C, Diodato D, Torre G, Picca S, Pariante R, Giuseppe Picardo S, Di Meo I, Rizzo C, Tiranti V, Zeviani M, de Ville de Goyet J. Liver transplant in ethylmalonic encephalopathy: a new treatment for an otherwise fatal disease. Brain. 2016;139:1045–51.
Duran M, Blau N, Gibson MK, editors. Laboratory guide to the methods in biochemical genetics. Berlin: Springer; 2008. p. 859.
Guo DC, Gong L, Regalado ES, Santos-Cortez RL, Zhao R, Cai B, et al. MAT2A mutations predispose individuals to thoracic aortic aneurysms. Am J Hum Genet. 2015;96:170–7.
Joint FAO/WHO/UNU Expert Consultation on Protein and Amino Acid Requirements in Human Nutrition (2002: Geneva, Switzerland). Protein and amino acid requirements in human nutrition. Report of a Joint WHO/FAO/UNU Expert Consultation. WHO Technical Report Series 935. Geneva: WHO; 2007.
Kitzler TM, Gupta IR, Osterman B, Poulin C, Trakadis Y, Waters PJ, Buhas DC. Acute and chronic management in an atypical case of ethylmalonic encephalopathy. JIMD Rep. 2019;45:57–63.
Kožich V, Morris AAM, Blom HJ. Disorders of sulfur amino acid metabolism. In: Saudubray JM, Baumgartner MR, Walter J, editors. Inborn metabolic diseases: diagnosis and treatment. 6th ed. Berlin: Springer; 2016. p. 309–20.
Kraus JP, Hasek J, Kozich V, et al. Cystathionine gamma-lyase: clinical, metabolic, genetic, and structural studies. Mol Genet Metab. 2009;97:250–9.
Morris AA, Kožich V, Santra S, et al. Guidelines for the diagnosis and management of cystathionine beta-synthase deficiency. J Inherit Metab Dis. 2017;40:49–74.
Mudd SH, Skovby F, Levy HL, et al. The natural history of homocystinuria due to cystathionine β-synthase deficiency. Am J Hum Genet. 1985;37:1–31.
Mudd SH, Cerone R, Schiaffino MC, et al. Glycine N-methyltransferase deficiency: a novel inborn error causing persistent isolated hypermethioninemia. J Inherit Metab Dis. 2001;24:448–64.
Pol A, Renkema GH, Tangerman A, et al. Mutations in SELENBP1, encoding a novel human methanethiol oxidase, cause extraoral halitosis. Nat Genet. 2018;50:120–9.
Stabler SP, Steegborn C, Wahl MC, et al. Elevated plasma total homocysteine in severe methionine adenosyltransferase I/III deficiency. Metabolism. 2002;51:981–8.
Staufner C, Lindner M, Dionisi-Vici C, et al. Adenosine kinase deficiency: expanding the clinical spectrum and evaluating therapeutic options. J Inherit Metab Dis. 2016;39(02):273–83.
Surtees R, Leonard J, Austin S. Association of demyelination with deficiency of cerebrospinal-fluid S-adenosylmethionine in inborn errors of methyl-transfer pathway. Lancet. 1991;338:1550–4.
Touati G, Rusthoven E, Depondt E, et al. Dietary therapy in two patients with a mild form of sulfite oxidase deficiency. Evidence for clinical and biological improvement. J Inherit Metab Dis. 2000;23:45–53.
Acknowledgements
The authors would like to acknowledge the help of Ms. Jitka Sokolová, MSc. with the manuscript preparation. Institutional and grant support to V.K. was provided by RVO-VFN 64165 and Progres Q26, and AZV 16-30384A, respectively.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Barić, I., Kožich, V., Fowler, B. (2022). Disorders of Sulfur Amino Acid and Hydrogen Sulfide Metabolism. In: Blau, N., Dionisi Vici, C., Ferreira, C.R., Vianey-Saban, C., van Karnebeek, C.D.M. (eds) Physician's Guide to the Diagnosis, Treatment, and Follow-Up of Inherited Metabolic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-67727-5_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-67727-5_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67726-8
Online ISBN: 978-3-030-67727-5
eBook Packages: MedicineMedicine (R0)