Abstract
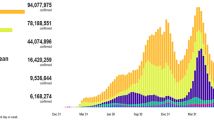
Coronavirus pandemic is proven as wreaking havoc with the rising number of cases since its first identification in Wuhan, China. This invisible threat has taken approximately 1.06 M lives with more than 36.5 M cases worldwide as on October 9th, 2020. World Health Organization (WHO) estimated the mortality rate for COVID-19 to be around 3–4% with higher risk to the people that have underlying medical conditions such as respiratory disease, diabetes, cancer, heart disease, asthma, and kidney disease. Numerous public health experts have defined a clear link between coronavirus death rates and long-term exposure to air pollution, especially PM2.5 and NO2 levels. Medical health experts are working hard to find a reliable treatment for COVID-19. The need for real-time monitoring systems to promote indoor air quality is another critical concern that demands the attention of the research community. The main contribution of this study is to present the connection between COVID-19 pandemic, public health and indoor air quality while addressing the importance of real-time monitoring systems for public health and wellness. This chapter presents the necessity of developing indoor air quality monitoring systems for hospitals, schools, offices and homes for enhanced health and well-being.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
World Health Organization: Coronavirus. In: World Health Organization (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 17 May 2020
World Health Organization: COVID-19 situation reports. In: World Health Organization (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 17 May 2020
Cucinotta, D., Vanelli, M.: WHO declares COVID-19 a pandemic. Acta Biomed. 91, 157–160 (2020). https://doi.org/10.23750/abm.v91i1.9397
Vellingiri, B., Jayaramayya, K., Iyer, M., et al.: COVID-19: a promising cure for the global panic. Sci. Total Environ. 725, 138277 (2020). https://doi.org/10.1016/j.scitotenv.2020.138277
World Health Organization: Modes of transmission of virus causing COVID-19—mplications for IPC precaution recommendations (2020). https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed 17 May 2020
Nicola, M., Alsafi, Z., Sohrabi, C., et al.: The socio-economic implications of the Coronavirus and COVID-19 pandemic: a review. Int. J. Surg. (2020). https://doi.org/10.1016/j.ijsu.2020.04.018
Ozili, P., Arun, T.: Spillover of COVID-19: impact on the Global Economy. SSRN Electron. J. (2020). https://doi.org/10.2139/ssrn.3562570
Balakrishnan, K., Dey, S., Gupta, T., et al.: The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the Global Burden of Disease Study 2017. Lancet Planet. Health 3, e26–e39 (2019). https://doi.org/10.1016/S2542-5196(18)30261-4
Jiang, F., Deng, L., Zhang, L., et al.: Review of the clinical characteristics of coronavirus disease 2019 (COVID-19). J. Gen. Intern. Med. 35, 1545–1549 (2020). https://doi.org/10.1007/s11606-020-05762-w
Mitter, S.S., Vedanthan, R., Islami, F., et al.: Household fuel use and cardiovascular disease mortality: golestan cohort study. Circulation 133, 2360–2369 (2016). https://doi.org/10.1161/CIRCULATIONAHA.115.020288
Sun, Q., Yue, P., Ying, Z., et al.: Air pollution exposure potentiates hypertension through reactive oxygen species-mediated activation of Rho/ROCK. Arterioscler. Thromb. Vasc. Biol. 28, 1760–1766 (2008). https://doi.org/10.1161/ATVBAHA.108.166967
Weisel, C.P.: Assessing exposure to air toxics relative to asthma. Environ. Health Perspect. 110, 527–537 (2002)
Wu, X., Nethery, R.C., Sabath, B.M., et al.: Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. Epidemiology (2020)
Goldizen, F.C., Sly, P.D., Knibbs, L.D.: Respiratory effects of air pollution on children. Pediatr. Pulmonol. 51, 94–108 (2016). https://doi.org/10.1002/ppul.23262
Graudenz, G.S., Oliveira, C.H., Tribess, A., et al.: Association of air-conditioning with respiratory symptoms in office workers in tropical climate. Indoor Air 15, 62–66 (2005). https://doi.org/10.1111/j.1600-0668.2004.00324.x
Patel, V., Kantipudi, N., Jones, G., et al.: Air pollution and cardiovascular disease: a review. Crit. Rev. Biomed. Eng. 44, 327–346 (2016). https://doi.org/10.1615/CritRevBiomedEng.2017019768
Samet, J.M., Bahrami, H., Berhane, K.: Indoor air pollution and cardiovascular disease: new evidence from Iran. Circulation 133, 2342–2344 (2016). https://doi.org/10.1161/CIRCULATIONAHA.116.023477
Chen, K., Wang, M., Huang, C., et al.: Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health (2020). https://doi.org/10.1016/S2542-5196(20)30107-8
Guan, L., Zhou, L., Zhang, J., et al.: More awareness is needed for severe acute respiratory syndrome coronavirus 2019 transmission through exhaled air during non-invasive respiratory support: experience from China. Eur. Resp. J. 55, 2000352 (2020). https://doi.org/10.1183/13993003.00352-2020
Ogen, Y.: Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 726, 138605 (2020). https://doi.org/10.1016/j.scitotenv.2020.138605
Altmann, D.M., Douek, D.C., Boyton, R.J.: What policy makers need to know about COVID-19 protective immunity. The Lancet 395, 1527–1529 (2020). https://doi.org/10.1016/S0140-6736(20)30985-5
US EPA O: Indoor Air Quality. In: US EPA (2017). https://www.epa.gov/report-environment/indoor-air-quality. Accessed 17 May 2020
Saini, J., Dutta, M., Marques, G.: A comprehensive review on indoor air quality monitoring systems for enhanced public health. Sustain. Environ. Res. 30, 6 (2020). https://doi.org/10.1186/s42834-020-0047-y
Ezzati, M., Kammen, D.M.: The health impacts of exposure to indoor air pollution from solid fuels in developing countries: knowledge, gaps, and data needs. Environ. Health Perspect. 110, 1057–1068 (2002). https://doi.org/10.1289/ehp.021101057
Kurmi, O.P., Lam, K.B.H., Ayres, J.G.: Indoor air pollution and the lung in low- and medium-income countries. Eur. Respir. J. 40, 239–254 (2012). https://doi.org/10.1183/09031936.00190211
Apte, K., Salvi, S.: Household air pollution and its effects on health. F1000Research 5, 2593 (2016). https://doi.org/10.12688/f1000research.7552.1
Zhu, Y., Xie, J., Huang, F., Cao, L.: Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 727, 138704 (2020). https://doi.org/10.1016/j.scitotenv.2020.138704
NYC Health: COVID-19: Data—NYC Health (2020). https://www1.nyc.gov/site/doh/covid/covid-19-data.page. Accessed 18 May 2020
Office for National Statistics: Measuring pre-existing health conditions in death certification—deaths involving COVID-19: March 2020—Office for National Statistics (2020). https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/methodologies/measuringpreexistinghealthconditionsindeathcertificationdeathsinvolvingcovid19march2020. Accessed 18 May 2020
Barcelo, D.: An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J Environ Chem Eng. (2020). https://doi.org/10.1016/j.jece.2020.104006
Marques, G., Pitarma, R.: Indoor air quality monitoring for enhanced healthy buildings. In: Abdul Mujeebu, M. (ed.) Indoor Environmental Quality. IntechOpen (2019)
Satheesan, M.K., Mui, K.W., Wong, L.T.: A numerical study of ventilation strategies for infection risk mitigation in general inpatient wards. Build. Simul. (2020). https://doi.org/10.1007/s12273-020-0623-4
Gan, W.H., Lim, J.W., Koh, D.: Preventing intra-hospital infection and transmission of coronavirus disease 2019 in health-care workers. Safety Health Work 11(2), S209379112030161X (2020). https://doi.org/10.1016/j.shaw.2020.03.001
Maki, D.G., Crnich, C.J., Safdar, N.: Chapter 51—Nosocomial infection in the intensive care unit. In: Parrillo, J.E., Dellinger, R.P. (eds.) Critical Care Medicine, 3rd edn, pp. 1003–1069. Mosby, Philadelphia (2008)
Slack, R.C.B.: 69 - Hospital infection. In: Greenwood, D., Barer, M., Slack, R., Irving, W. (eds.) Medical Microbiology, Eighteenth edn, pp. 718–726. Churchill Livingstone, Edinburgh (2012)
Wong, S.C.Y., Kwong, R.T.-S., Wu, T.C., et al.: Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J. Hosp. Infect. 105, 119–127 (2020). https://doi.org/10.1016/j.jhin.2020.03.036
Chamseddine, A., El-Fadel, M.: Exposure to air pollutants in hospitals: indoor–outdoor correlations. In: Brebbia, C.A. (ed.) WIT Transactions on the Built Environment, 1st ed.,, pp. 707–716. WIT Press (2015)
El-Sharkawy, M.F., Noweir, M.E.H.: Indoor air quality levels in a University Hospital in the Eastern Province of Saudi Arabia. J. Family Commun. Med. 21, 39–47 (2014). https://doi.org/10.4103/2230-8229.128778
Gola, M., Settimo, G., Capolongo, S.: Chemical pollution in healing spaces: the decalogue of the best practices for adequate indoor air quality in inpatient rooms. Int. J. Environ. Res. Public Health 16 (2019). https://doi.org/10.3390/ijerph16224388
Li, Y., Leung, G.M., Tang, J.W., et al.: Role of ventilation in airborne transmission of infectious agents in the built environment? a multidisciplinary systematic review. Indoor Air 17, 2–18 (2007). https://doi.org/10.1111/j.1600-0668.2006.00445.x
Amegah, A.K., Jaakkola, J.J.: Household air pollution and the sustainable development goals. Bull. World Health Organ. 94, 215–221 (2016). https://doi.org/10.2471/BLT.15.155812
Chafe, Z.A., Brauer, M., Klimont, Z., et al.: Household cooking with solid fuels contributes to ambient PM2.5 air pollution and the burden of disease. Environ. Health Perspect. 122, 1314–1320 (2014). https://doi.org/10.1289/ehp.1206340
Josyula, S., Lin, J., Xue, X., et al.: Household air pollution and cancers other than lung: a meta-analysis. Environ. Health 14, 24 (2015). https://doi.org/10.1186/s12940-015-0001-3
McCracken, J.P., Wellenius, G.A., Bloomfield, G.S., et al.: Household air pollution from solid fuel use: evidence for links to CVD. Glob. Heart 7, 223–234 (2012). https://doi.org/10.1016/j.gheart.2012.06.010
Pope, D.P., Mishra, V., Thompson, L., et al.: Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol. Rev. 32, 70–81 (2010). https://doi.org/10.1093/epirev/mxq005
Banerjee, A., Pasea, L., Harris, S., et al.: Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet (2020). https://doi.org/10.1016/S0140-6736(20)30854-0
Endocrinology TLD & (2020) COVID-19: underlying metabolic health in the spotlight. Lancet Diabetes Endocrinol. (2020). https://doi.org/10.1016/S2213-8587(20)30164-9
Ghergu, C., Sushama, P., Vermeulen, J., et al.: Dealing with indoor air pollution: an ethnographic tale from urban slums in Bangalore. Int. J. Health Sci. 6, 348–361 (2016)
Steinemann, A.: Volatile emissions from common consumer products. Air Qual. Atmos. Health 8, 273–281 (2015). https://doi.org/10.1007/s11869-015-0327-6
Kwon, J.-W., Park, H.-W., Kim, W.J., et al.: Exposure to volatile organic compounds and airway inflammation. Environ Health 17(1) (2018). https://doi.org/10.1186/s12940-018-0410-1
Win-Shwe, T.-T., Fujimaki, H., Arashidani, K., Kunugita, N.: Indoor volatile organic compounds and chemical sensitivity reactions. Clin. Dev. Immunol. 2013. https://doi.org/10.1155/2013/623812
Giamarellos-Bourboulis, E.J., Netea, M.G., Rovina, N., et al.: Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe S1931312820302365 (2020). https://doi.org/10.1016/j.chom.2020.04.009
Tay, M.Z., Poh, C.M., Rénia, L., et al.: The trinity of COVID-19: immunity, inflammation and intervention. Nat. Rev. Immunol. 1–12 (2020). https://doi.org/10.1038/s41577-020-0311-8
Liu, P., Wang, X., Fan, J., et al.: Effects of air pollution on hospital emergency room visits for respiratory diseases: urban-suburban differences in Eastern China. Int. J. Environ. Res. Public Health 13(3), 41 (2016). https://doi.org/10.3390/ijerph13030341
Zhang, H., Niu, Y., Yao, Y., et al.: The impact of ambient air pollution on daily hospital visits for various respiratory diseases and the relevant medical expenditures in Shanghai, China. Int. J. Environ. Res. Public Health 15(3), 425 (2018). https://doi.org/10.3390/ijerph15030425
Zakaria Abouleish, M.Y.: Indoor air quality and coronavirus disease (COVID-19). Public Health (2020). https://doi.org/10.1016/j.puhe.2020.04.047
Hapsari, A.A., Hajamydeen, A.I., Abdullah, M.I.I.: A review on indoor air quality monitoring using IoT at campus environment. Int. J. Eng. Technol. 7, 55–60 (2018). https://doi.org/10.14419/ijet.v7i4.22.22191
Sun, S., Zheng, X., Villalba-Díez, J., Ordieres-Meré, J.: Indoor air-quality data-monitoring system: long-term monitoring benefits. Sensors 19, 4157 (2019). https://doi.org/10.3390/s19194157
Lozano, J., Suárez, J.I., Arroyo, P., et al.: Wireless sensor network for indoor air quality monitoring. Chem. Eng. Trans. 30, 319–324 (2012). https://doi.org/10.3303/CET1230054
Yi, W., Lo, K., Mak, T., et al.: A survey of wireless sensor network based air pollution monitoring systems. Sensors 15, 31392–31427 (2015). https://doi.org/10.3390/s151229859
Elbayoumi, M., Ramli, N.A., Fitri Md Yusof, N.F.: Development and comparison of regression models and feedforward backpropagation neural network models to predict seasonal indoor PM2.5–10 and PM2.5 concentrations in naturally ventilated schools. Atmos. Pollut. Res. 6, 1013–1023 (2015). https://doi.org/10.1016/j.apr.2015.09.001
Kolokotsa, D.: Artificial intelligence in buildings: a review of the application of fuzzy logic. Adv. Build. Energy Res. 1, 29–54 (2007). https://doi.org/10.1080/17512549.2007.9687268
Masih, A.: Machine learning algorithms in air quality modeling. Glob. J. Environ. Sci. Manag. 5, 515–534 (2019). https://doi.org/10.22034/GJESM.2019.04.10
Kumar, P., Skouloudis, A.N., Bell, M., et al.: Real-time sensors for indoor air monitoring and challenges ahead in deploying them to urban buildings. Sci. Total Environ. 560–561, 150–159 (2016). https://doi.org/10.1016/j.scitotenv.2016.04.032
Revel, G., Arnesano, M., Pietroni, F., et al.: Cost-effective technologies to control indoor air quality and comfort in energy efficient building retrofitting. Environ. Eng. Manag. J. 14, 1487–1494 (2015). https://doi.org/10.30638/eemj.2015.160
Bruce, N., Perez-Padilla, R., Albalak, R.: Indoor air pollution in developing countries: a major environmental and public health challenge. Bull. World Health Organ. 78, 1078–1092 (2000)
Roberton, T., Carter, E.D., Chou, V.B., et al.: Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob. Health (2020). https://doi.org/10.1016/S2214-109X(20)30229-1
Marques, G., Pitarma, R.: A cost-effective air quality supervision solution for enhanced living environments through the internet of things. Electronics 8, 170 (2019). https://doi.org/10.3390/electronics8020170
Idrees, Z., Zou, Z., Zheng, L.: Edge computing based IoT architecture for low cost air pollution monitoring systems: a comprehensive system analysis. Design Considerations Dev. Sens. 18, 3021 (2018). https://doi.org/10.3390/s18093021
Tiele, A., Esfahani, S., Covington, J.: Design and development of a low-cost, portable monitoring device for indoor environment quality. J. Sens. 2018, 1–14 (2018). https://doi.org/10.1155/2018/5353816
Yu, T.-C., Lin, C.-C.: An intelligent wireless sensing and control system to improve indoor air quality: monitoring, prediction, and preaction. Int. J. Distrib. Sens. Netw. 11, 140978 (2015). https://doi.org/10.1155/2015/140978
Okokpujie, K., Noma-Osaghae, E., Odusami, M., et al.: a smart air pollution monitoring system. Int. J. Civil Eng. Technol. 9, 799–809 (2018)
Bulot, F.M.J., Russell, H.S., Rezaei, M., et al.: Laboratory comparison of low-cost particulate matter sensors to measure transient events of pollution. Sensors 20, 2219 (2020). https://doi.org/10.3390/s20082219
Li, J., Mattewal, S.K., Patel, S., Biswas, P.: Evaluation of nine low-cost-sensor-based particulate matter monitors. Aerosol Air Qual. Res. 20, 254–270 (2019). https://doi.org/10.4209/aaqr.2018.12.0485
Liu, M., Lin, J., Boersma, K.F., et al.: Improved aerosol correction for OMI tropospheric NO2 retrieval over East Asia: constraint from CALIOP aerosol vertical profile. Atmos. Meas. Tech. 12, 1–21 (2019). https://doi.org/10.5194/amt-12-1-2019
Morawska, L., Tang, J.W., Bahnfleth, W., et al.: How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 142, 105832 (2020). https://doi.org/10.1016/j.envint.2020.105832
Sun, C., Zhai, Z.: The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 62, 102390 (2020). https://doi.org/10.1016/j.scs.2020.102390
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Saini, J., Dutta, M., Marques, G. (2021). Indoor Air Quality Monitoring Systems and COVID-19. In: Arpaci, I., Al-Emran, M., A. Al-Sharafi, M., Marques, G. (eds) Emerging Technologies During the Era of COVID-19 Pandemic. Studies in Systems, Decision and Control, vol 348. Springer, Cham. https://doi.org/10.1007/978-3-030-67716-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-67716-9_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67715-2
Online ISBN: 978-3-030-67716-9
eBook Packages: Intelligent Technologies and RoboticsIntelligent Technologies and Robotics (R0)