Abstract
Although earlier studies have documented the influence of weather on human health in major Argentine cities, these studies lack national coverage. Moreover, the use of different health metrics and weather parameters makes it impossible to assess any geographic heterogeneity of impacts. We aimed to analyze the effect of hot and cold temperatures on human mortality rates in Argentina and their differential impacts by age and sex. The study rests on nonparametric techniques applied to data with a panel structure to estimate the causal effect of temperature extremes on mortality risks. Our findings confirm that extreme temperatures increase mortality rates relative to mean monthly temperatures, but the impact of colder than average temperatures is larger in magnitude. On average, a day with a countrywide mean temperature of 5 \(^{\circ }\)C increases overall monthly mortality rate by 3.5% points with respect to the observed mortality for a day with countrywide average temperature. As expected, there exists substantial heterogeneity between age groups, with older people facing larger risks. To a lesser extent, there are also heterogeneous impacts by gender and geographic regions. These findings provide relevant information for policy makers about potential impacts of changing temperatures over Argentina in the upcoming decades.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Climate change represents a major threat for humans and other forms of life in our planet. The potential impact of climate and climate variability on the social and environmental determinants of health outcomes is at the forefront of scientific and policy concerns. Recently, the World Health Organization (WHO) reported that climate change is expected to cause approximately 250,000 additional deaths per year worldwide between 2030 and 2050, due to malnutrition, diarrhea, and heat stress (World Meteorological Organization 2018).
Presently, the global mean temperature is approximately 1.2 \(^{\circ }\)C above the pre-industrial era (World Meteorological Organization 2017). There exists a strong agreement among the scientific community regarding the human influence on the observed and predicted changes in temperature and precipitation patterns. For instances, the Intergovernmental Panel on Climate Change (IPCC) states that anthropogenic influences have very likely contributed to the observed rise in terrestrial and ocean temperatures since 1970. Without further attempts to curb these emissions, it is predicted that the global mean temperature will rise between 3.7 and 4.8 \(^{\circ }\)C by the end of the century, increasing extremely hot days while decreasing cold ones (Intergovernmental Panel on Climate Change 2014). Understanding the effects that extreme temperatures pose on human health is key to promote effective adaptation policies to rising temperatures from climatic change.
Potential impacts of weather changes on mortality are usually divided between direct impacts, i.e., those produced by temperature increases or weather-related natural disasters, and indirect impacts arising mainly from changes in vector-borne diseases and food security. This paper concerns with the former: the direct effect that extreme temperatures have on mortality risks.
The relationship between thermal extremes and mortality has been extensively documented in the literature for developed countries (Baccini et al. 2008; Basu and Samet 2002; Basu et al. 2005; Braga et al. 2002; Curriero et al. 2002; Medina-Ramón and Schwartz 2007) and to a lesser extent in developing countries. In Latin America, the evidence is pretty thin (Bel et al. 2008; Romero-Lankao et al. 2013). In general, these studies find excess mortality during both cold and hot periods, although this relationship varies greatly by geographic regions. Also, they report differences in population susceptibility, with women and the elderly at most risk. For a more detailed survey of findings, see Basu and Samet (2002) and Basu (2009).
A few studies have documented the influence of weather on human health in major Argentine cities. The closers to our work are Almeira et al. (2016), which reports a U-shaped relationship between temperature and mortality for the cities of Buenos Aires and Rosario, and De Garín and Bejarán (2003), which examines the effect of thermal stress during summertime, characterized by the relative strain index, on mortality rates in Buenos Aires city. Other study, using data from emergency room visits at a hospital in central Buenos Aires reports the association between weather conditions and several pathologies for wintertime and summertime, during the 1996–97 season (Rusticucci et al. 2002). Yet other studies have turned their focus into specific pathologies, particularly respiratory diseases. For instance, Piccolo et al. (1988) documented the relationship between asthma hospitalizations and meteorological variables in Bahia Blanca. More recently, two studies for the city of Córdoba find that a higher daily mean temperature and a wider daily temperature range are important determinants of infectious diseases in both the upper and lower respiratory tracts, particularly among the elder population, and in low-income households facing housing deprivation (Amarillo and Carreras 2012; Carreras et al. 2015).
Although very informative, these studies lack national coverage. Moreover, the use of different health metrics and weather parameters makes it impossible to assess any geographic heterogeneity of impacts. In a context of climatic change, where resource to promote adaptation to the new climate norms must be allocated, comparable countrywide estimates of health costs are most needed to develop a rational adaptation policy.
This paper makes two contributions to the literature. First, it extends on a very thin literature on climatic determinants of mortality in Argentina. Second, it provides the first countrywide and comparable regional estimates of the incidence of temperature on mortality, breaking it up by gender and age group.
Econometric Modeling
The causal effect of temperature on mortality rates in Argentinean municipalities is analyzed using nonparametric models for panel data, i.e., repeated cross-sectional data. Nonparametric models estimated by ordinary least squares have been widely applied in the epidemiological literature (Barreca and Shimshack 2012; Curriero et al. 2002; Doyon et al. 2008; Kaiser et al. 2007) because the relationship between weather and mortality rates is likely to be nonlinear (Basu 2009). Thus, the estimated benchmark model is described by the following equation:
where \(\mathrm {TM}_{cpmy}\) is the mortality rate per 100,000 inhabitants in municipality c within province p in month m in year y. The final unit of analysis is a “municipality by month.” The exposure functions \(f\left( \mathrm {temp}_{cpmy} \right) \) and \(f\left( \mathrm {prep}_{cpmy} \right) \) are additive functions containing parameters to be estimated related to exposure to monthly average temperature and precipitation, respectively. \(\mu _{m}\) stands for time effects that allow controlling for potentially confounding effects common to all municipalities that vary overtime, for example technological advances or macroeconomic shocks affecting the countrywide economic performance, which might affect health outcomes. Finally, \(\omega _{cm}\) is an interaction term which captures temporal variations between municipalities due to differences in air quality, income levels, educational attainment, and population density. Thus, these fixed effects could be interpreted as a baseline estimate of mortality rates in each municipality (Barreca and Shimshack 2012).
The exposure functions are estimated by means of restricted piecewise cubic splines, using the mkspline package in the statistical software Stata, version 14.0. Restricted cubic spline performs better than a linear spline when working with very curved functions (Rosenberg et al. 2003), thus allowing both mortality and weather to vary more flexibly without needing to choose a priori any functional form. A total of six knots were chosen for both the average monthly temperatures. The number of knots seems appropriate for large datasets, and the specific values were selected using the percentile distribution (Curriero et al. 2002; Rosenberg et al. 2003) of the weather variables (Harrell 2001).
The estimated exposure parameters cannot be directly interpreted; therefore, they should be compared to a reference value, which in this case was selected at 18.9 degree Celsius (\(^{\circ }\)C), the national mean daily temperature. It can be calculated as (Stata 2017):
where \(k_{i}\) is the value for the ith knot \((i=1,\ldots ,n)\), \(V_{i}\) is the exposure parameter to be estimated \((i=1,\ldots ,n-1)\), and \(V_{1}\) is the reference temperature (18.9 \(^{\circ }\)C). Finally, \((u_{+})=u\) if u is strictly positive, and \((u_{+})=0\) if u is zero or negative.
Data
The estimation strategy outlined above relies on two major sets of data between the years 2004 and 2010: death counts by administrative subdivision and weather records from meteorological stations.
The mortality data corresponds to the universe of 1,812,745 million deaths occurred across the country, compiled by Dirección de Estadísticas e Información Pública, which is the agency in charge of the national system of health statistics. The dataset reports each death along with the date of death, the gender and age, and the municipality of residence of the deceased. Thus, death counts had to be aggregated at the municipal level, the smallest administrative subdivision in the dataset.
Death counts were complemented with annual population estimates in order to construct all-cause monthly municipal mortality rates per 100,000 inhabitants, by gender and age groups. Annual municipal population had to be interpolated from the 2001 and 2010 national population censuses. Specifically, following Deschênes and Greenstone (2011) and Barreca et al. (2016), population was stratified in four age groups (0–4, 5–44, 45–64, and >64 years old), according to the population summaries in the 2001 census. Unfortunately, population summaries did not allow constructing separate mortality rates for infants, i.e., younger than one year old, which are far more susceptible to thermal stress than other young children (Keim et al. 2002).
Weather records were obtained from Servicio Meteorológico Nacional, the official weather and climatological agency. Daily maximum and minimum temperatures in degree Celsius, and total precipitation in millimeters (mm) are reported for 71 weather stations that comprise the national weather station network. Ten weather stations, all located in Patagonia, southern Argentina, had to be discarded due to incomplete weather records. The monitoring network might seem to be sparse given the surface area and the degree of development for a country such as Argentina. However, according to the 2010 national census, Argentinian population is mostly urban, with 91% living in towns bigger than 2000 inhabitants, and half of the total population living in just 8 cities. Therefore, these 61 weather stations included in the analysis provide coverage to approximately 82% of the country’s population.
Daily station data had to be spatially interpolated at the municipal level to construct monthly weather exposure variables. Following a common approach in the literature, square inverse distance weights were calculated from each municipality geographical centroid to each station within a 100 km radius (Hanigan et al. 2006). Thus, the interpolated weather variables are simply the weighted average of the station records within that radius. Limiting the cutoff distance 100 km was necessary to balance the number of municipalities included in the study and minimizing the potential measurement error introduced by using distant stations. Similar cutoff levels have been used in empirical estimates for the USA (Barreca 2012; Barreca and Shimshack 2012; Barreca et al. 2016; Deschênes and Greenstone 2011; Ranson 2014).
Impact of Extreme Temperatures on Mortality
Panel A of Table 1 presents summary statistics of interpolated daily mean, maximum, and minimum temperatures for the 322 municipalities included in the study, stratified by census region, over the 2004–2010 period. It can be observed that the lower temperature records correspond to municipalities in Cuyo and Pampean regions—recall Patagonia has been excluded due to lack of complete weather station records. Minimum temperatures over these regions are on average 5.9 and 5.2 \(^{\circ }\)C lower than in the warmer northeast region. As expected, municipalities in northern regions experience higher maximum temperatures, with records between 3.9 and 4.9 \(^{\circ }\)C higher than the region with the lowest maximum temperatures.
Summary statistics for monthly mortality rates between age groups are reported in Panel B and by region in Panel C of the same table. Average mortality rates are 10.8 per 100,000 inhabitants for children under 5 year of age, 6.7 for people between 5 and 44 years of age, 47 for adults between 44 and 65, and 325 for older adults. Consequently, one should expect to observe larger impacts of extreme temperatures among these two last groups, given that they appear to the most vulnerable people. Looking at different regions, higher mortality seems to be correlated with higher daily mean temperatures, although one should be cautious to infer causation since confounding factors, for instance income levels, could be also correlated with climate. Notwithstanding, the identification strategy described in the previous section allows controlling for these confounding factors by including a series of fixed effects.
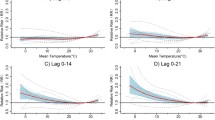
Figure 1 presents the estimated exposure impacts, and their respective 95% confidence intervals, computed by nonparametric regressions between mortality rates and temperature at the municipal level, controlling for precipitation levels, and fixed effects by month and municipality by month. The results must be interpreted as the relative impact of temperature (daily mean, maximum, or minimum) over annual mortality in percentage points (pp) due to an additional day in a given month with temperature above or below the observed average temperature during the 2004–2010 period.
Effect of temperature on overall mortality rate. The solid lines are the impacts of temperature on the mortality rate compared to a month with the average countrywide temperature. Blue lines are colder than average and red lines hotter than average temperature. Dashed line is the 95% confidence intervals. A Daily mean temperature (reference value is 18.9 \(^{\circ }\)C). B Maximum daily temperature (reference value is 24.4 \(^{\circ }\)C). C Minimum daily temperature (reference value is 12.2 \(^{\circ }\)C)
For example, Panel A of Fig. 1 shows that on average, an additional day with a countrywide mean temperature of 5 \(^{\circ }\)C increases overall annual mortality rate by 3.5 pp (95% CI: 3.06–3.96) with respect to the observed mortality for a day with countrywide average temperature (i.e., 18.9 \(^{\circ }\)C). In general, Figure 1 shows a nonlinear relationship between temperature (daily mean, maximum, and minimum, respectively) and the overall mortality rate, i.e., all age groups, genders, and regions. A striking regularity depicted in Fig. 1 is that the estimated impacts of colder than average temperatures are higher than the computed estimates for hotter than average temperatures. Again, using Panel A to illustrate, any day with a mean daily temperature below the average, 18.8 \(^{\circ }\)C, positively and significantly affects mortality rates, and the estimated impacts increase as the temperature decreases. However, only those days with temperatures above 25.5 \(^{\circ }\)C generate statistically significant impacts on mortality risks. Another interesting result is that while colder temperatures are always significant, only the highest maximum (Panel B) and highest minimum (Panel C) temperatures produce slightly statistical significant impacts on mortality.
Effect of daily mean temperature by census regions. The solid lines are the relative risks of mortality compared to a day with the average countrywide daily mean temperature (18.9 \(^{\circ }\)C). Blue lines are colder than average and red lines hotter than average temperature. Dashed line is the 95% confidence intervals. a Buenos Aires metropolitan area. b Pampean. c Northwest. d Northeast. e Cuyo
Physiological factors and adaptation to the environment may affect the relationship between mortality risks and temperature. In order to examine potential heterogeneity in the temperature–mortality relationship, regressions were stratified by census regions (Fig. 2), and age group and gender (Fig. 3). Figure 2 shows that for all regions, colder than (the national) average temperatures have at same point of the curve a positive and statistically significant impact on mortality rates. For instance, one additional day in a month with a mean daily temperature of 9.4 \(^{\circ }\)C increases annual mortality by 4.6 pp (95% CI: 3.38–5.79) in Buenos Aires metropolitan area (Panel A). In the same fashion, an additional day of 5.6 \(^{\circ }\)C rises annual mortality risks by 5.2 (95% CI: 2.37–8.08) in the Pampean region (Panel B). In the northeast (Panel C), a day of 8.33 \(^{\circ }\)C increases mortality by 8.3 pp (95% CI: 0.54–16.05), while in the northwest region (Panel D) a day with mean daily temperature of 10.55 \(^{\circ }\)C raises mortality by 7.83 pp (95% CI: 3.81–11.87). Finally, in the western region of Cuyo (Panel E) an additional day of temperature around 2 \(^{\circ }\)C raises local mortality rates by 10.02 pp (95% CI: 2.47–17.57). Again, the estimated impacts are relative to a one less day in a month with mean daily temperature of 18.9 \(^{\circ }\)C, which is the national average temperature.
Figure 3 provides evidence of heterogeneous impacts by age group (females in Panel A and males in Panel B). Only the elderly are affected by extreme temperatures, but colder than average temperatures seem to be more likely to be statistically significantly different from a day with 18.9 \(^{\circ }\)C. Also, cold temperatures have a greater impact on male mortality risks, with no apparent difference between sexes for hotter than normal temperatures.
Effect of daily mean temperature by age group and gender. The solid lines are the relative risks of mortality compared to a day with the average countrywide daily mean temperature (18.9 \(^{\circ }\)C). Blue lines are colder than average and red lines hotter than average temperature. Dashed line is the 95% confidence intervals. a Females. b Males
Discussion
Environmental factors are important determinants of human health. Recently, due to global warming and the recurrence of heat waves, the attention has been placed on how weather affects health outcomes, among which mortality has captured the most attention.
The existing literature, mainly for developed countries, has pointed to a U-shaped type of relationship between temperature and mortality risks. Using flexible regression models over longitudinal monthly weather and mortality data for 322 municipalities spanning January 2004 and December 2010, this study has confirmed this relationship from a countrywide perspective.
We found a significant impact of both cold and hot days on mortality risks; however, colder than average temperatures have a greater effect on mortality. This finding holds irrespective of using the daily mean, maximum, or minimum temperatures. Using a comparable methodology applied for US counties, Barreca and Shimshack (2012) also reported a similar association between colder temperatures and influenza mortality, although their work concerned mainly with the impact of absolute humidity. Almeira et al. (2016) also report a higher susceptibility to colder extremes than to hotter temperatures in the cities of Buenos Aires and Rosario. An additional interesting result is that hotter than average temperatures have no impact when splitting the data by regions. In particular, we found no significant impact of hotter than average temperatures in Buenos Aires metropolitan area. In contrasts, De Garín and Bejarán (2003) reported that higher temperatures in Buenos Aires city, through its impact on the relative strain index, explain almost 10% of summertime mortality.
Our study has several limitations. First, the available population data did not allow constructing separate mortality rates for infants, i.e., younger than one year old, which are far more susceptible to thermal stress than other young children, as previously mentioned. Therefore, our results of no statistical significant influence of extreme temperatures on children’s mortality rates have to be taken with caution. The second limitation is that mortality is obviously an extreme outcome, and thus underestimates the overall effect of extreme temperatures on human health. Unfortunately, there is no detailed countrywide medical database available to estimate both mortality and morbidity impacts. Another possible source of underestimation comes from the adoption of precautionary measures, particularly air conditioning, which have a protective effect during extreme temperatures (Barreca et al. 2016).
Another limitation concerns the use of weather data from meteorological stations. Given the sparse distribution of the station network, interpolation of weather parameters from distant stations might have introduced measurement error. To limit the chance of this type of error, we follow the convention of excluding weather station further than 100 km away from each municipal geographical center. Satellites might provide better weather information, at least in terms of spatial coverage (Kloog et al. 2014), but we leave this to future research. Also, we did not have access to information about mortality by cause. Therefore, the impacts of temperature on the overall mortality rate should understate the true impacts.
Having pointed out the potential short comes of this research, we believe this study provides valuable information on weather determinants of mortality in Argentina. The estimation approach employed in this papers allows to disentangle the causal effect of temperatures on mortality risk while controlling for possible confounders, reducing the possibility that the observed temperature–mortality link was driven by omitted factors associated with both weather and mortality.
To conclude, two main contributions of the paper are worth mentioning. Firstly, we produce the first countrywide and geographical comparable estimates of the temperature–mortality relationship in a sizable portion of the population. Second, we use repeated cross-sectional data instead of the more traditional time series approach used in previous empirical papers. This approach might help overcome the problem of relatively short time series usually observed in Argentinian data.
References
Almeira G, Rusticucci M, Suaya M (2016) Relationship between mortality and extreme temperatures in Buenos Aires and Rosario. Meteorologica 41(2):65–79
Amarillo AC, Carreras HA (2012) The effect of airborne particles and weather conditions on pediatric respiratory infections in Cordoba, Argentina. Environ Pollut 170:217–221
Baccini M, Biggeri A, Accetta G, Kosatsky T, Katsouyanni K, Analitis A et al (2008) Heat effects on mortality in 15 European cities. Epidemiology 19(5):711–719
Barreca A (2012) Climate change, humidity, and mortality in the United States. J Environ Econ Manage 63(1):19–34
Barreca AI, Shimshack JP (2012) Absolute humidity, temperature, and influenza mortality: 30 years of county-level evidence from the United States. Am J Epidemiol 176(7):114–122
Barreca A, Clay K, Deschênes O, Greenstone M, Shapiro JS (2016) Adapting to climate change: the remarkable decline in the US temperature-mortality relationship over the 20th century. J Polit Econ 124(1):105–159
Basu R (2009) High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. A global access science source. Environ Health 8(1):40
Basu R, Samet JM (2002a) An exposure assessment study of ambient heat exposure in an elderly population in Baltimore, Maryland. Environ Health Perspect 110(12):1219–1224
Basu R, Samet JM (2002b) Relation between elevated ambient temperature and mortality, a review of the epidemiologic evidence. Epidemiol Rev 24(2):190–202
Basu R, Dominici F, Samet JM (2005) Temperature and mortality among the elderly in the United States: a comparison of epidemiologic methods. Epidemiology 16(1):58–66
Bel lML, O’Neill MS, Ranjit N, Borja-Aburto VH, Cifuentes L, Gouveia NC (2008) Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol 37(4):796–804
Braga ALF, Zanobetti A, Schwartz J (2002) The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 110(9):859–863
Carreras H, Zanobetti A, Koutrakis P (2015) Effect of daily temperature range on respiratory health in Argentina and its modification by impaired socio-economic conditions and PM10 exposures. Environ Pollut 206:175–182
Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA (2002) Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 155(1):80–87
De Garín A, Bejarán R (2003) Mortality rate and relative strain index in Buenos Aires city. Int J Biometeorol 48(1):31–36
Deschênes O, Greenstone M (2011) Climate change, mortality, and adaptation: evidence from annual fluctuations in weather in the US. Am Econ J Appl Econ 3(4):152–185
Doyon B, Bélanger D, Gosselin P (2008) The potential impact of climate change on annual and seasonal mortality for three cities in Québec, Canada. Int J Health Geogr 7(23):1–12
Hanigan I, Hall G, Dear KBG (2006) A comparison of methods for calculating population exposure estimates of daily weather for health research. Int J Health Geogr 13(5):1–16
Harrell F (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. In: Springer series in statistics
Intergovernmental Panel on Climate Change (2014) Climate change 2014 synthesis report. Contribution of working groups I, II and III to the fifth assessment report of the intergovernmental panel on climate change. http://www.ipcc.ch/pdf/assessment-report/ar5/syr/AR5_SYR_FINAL_SPM.pdf. Cited 9 Aug 2019
Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, Rubin CH (2007) The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Pub Health 97(Suppl 1):S158:62
Keim SM, Guisto JA, Sullivan JB (2002) Environmental thermal stress. Ann Agric Environ Med 9(1):1–15
Kloog I, Nordio F, Coull BA, Schwartz J (2014) Predicting spatiotemporal mean air temperature using MODIS satellite surface temperature measurements across the Northeastern USA. Rem Sens Environ 150:132–139
Medina-Ramón M, Schwartz J (2007) Temperature, temperature extremes, and mortality: a study of acclimatization and effect modification in 50 United States cities. Occup Environ Med 64(12):827–833
Piccolo MC, Perillo GM, Ramon CG, DiDio V (1988) Outbreaks of asthma attacks and meteorologic parameters in Bahia Blanca, Argentina. Ann Allergy 60(2015):107–110
Ranson M (2014) Crime, weather, and climate change. J Environ Econ Manage 67(3):274–302
Romero-Lankao P, Qin H, Borbor-Cordova M (2013) Exploration of health risks related to air pollution and temperature in three Latin American cities. Soc Sci Med 83:110–118
Rosenberg PS, Katki H, Swanson CA, Brown LM, Wacholder S, Hoover RN (2003) Quantifying epidemiologic risk factors using non-parametric regression: model selection remains the greatest challenge. Stat Med 22(21):3369–3381
Rusticucci M, Bettolli ML, Harris De Los Angeles, M (2002) Association between weather conditions and the number of patients at the emergency room in an Argentine hospital. Int J Biometeorol 46(1):42–51
Stata Corp L (2017) Stata base reference manual release, vol 15. Stata Press
World Health Organization (2018) Climate change and health. http://www.who.int/news-room/fact-sheets/detail/climate-change-and-health. Cited 9 Aug 2019
World Meteorological Organization (2017) WMO statement on the state of the global climate in 2017. http://library.wmo.int/opac/index.php?lvl=notice_display&id=20220#.WsSZlI4zMt8. Cited 9 Aug 2019
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
García-Witulski, C.M., Rabassa, M.J. (2021). The Impact of Temperature on Mortality in Argentinean Municipalities. In: Belfiori, M.E., Rabassa, M.J. (eds) The Economics of Climate Change in Argentina. The Latin American Studies Book Series. Springer, Cham. https://doi.org/10.1007/978-3-030-62252-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-62252-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-62251-0
Online ISBN: 978-3-030-62252-7
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)