Abstract
Anaplastic thyroid cancer (ATC) has an overall poor prognosis. In 2018, the US Food and Drug Administration approved a BRAF/MEK inhibitor combination, dabrafenib/trametinib, for BRAFV600E-mutated ATC, which has shown high response rates (69%) and improved survival and is now the standard of care in the USA. Rapid determination of the BRAFV600E status is part of the initial workup for all ATC patients, in addition to the assessment of the airway and staging. In patients where a complete resection cannot be achieved (the majority), chemoradiation can be offered. Those with BRAF mutations, however, may benefit from neoadjuvant dabrafenib/trametinib followed by surgery and chemoradiation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Anaplastic thyroid cancer (ATC) is a deadly disease, and, until recently, little progress had been made to change the outcomes of these patients. In 2018, the US Food and Drug Administration (FDA) approved a BRAF/MEK inhibitor combination, dabrafenib/trametinib, for BRAFV600E -mutated ATC. These drugs are highly efficacious in this ATC subtype, and therefore, BRAFV600E status is now part of the initial evaluation for all ATC patients. Dabrafenib/trametinib is now the standard of care for BRAFV600E-mutated ATC patients in the USA.
Case Presentation
A 72-year-old woman presented to the local emergency room with dyspnea and palpitations. She was found to have a right-sided neck mass, a pulmonary embolism, and a large pleural effusion. Thoracentesis was performed, revealing metastatic adenocarcinoma, positive for PAX8 (diffuse) and TTF-1 (weak) and negative for thyroglobulin and estrogen receptor, compatible with a thyroid primary. Ultrasound of the neck revealed a 5.5 cm partially cystic mass in the right supraclavicular region and multiple thyroid nodules. CT scan of the neck and chest revealed similar findings as well as mediastinal adenopathy. Taken together, the clinical picture was consistent with stage IVC ATC. The patient subsequently underwent biopsy of the supraclavicular mass, which showed poorly differentiated carcinoma. The patient was referred to an academic cancer center.
On initial staging FDG-PET/CT, shown in Fig. 43.1, (panel a), a large right necrotic mass adjacent to right thyroid hypermetabolic nodule was identified. Additional sites of disease included bilateral cervical lymph nodes, bilateral pulmonary nodules, a left sternal bone metastasis, and paracaval lymph nodes. An MRI of the brain showed no evidence of metastatic disease.
Pre- and post-treatment FDG-PET/CT imaging. (a) Baseline FDG-PET/CT imaging showing a right supraclavicular mass with an SUV of 32, a small right-sided thyroid nodule in the neck (left panel), and multiple mediastinal adenopathy and left pleural effusion (right panel). (b) FDG-PET/CT was performed after treatment with dabrafenib/trametinib for 2 months, showing near resolution of metastatic lymphadenopathy in the neck and lungs. The right thyroid nodule shows significantly less metabolic activity
Fine-needle aspiration with cell block preparation of the supraclavicular lesion was performed in order to obtain immunohistochemistry staining for BRAFV600E. The biopsy showed high-grade, poorly differentiated carcinoma with squamoid features, positive for PAX-8, TTF-1, and BRAFV600E . She was started on dabrafenib 150mg twice a day and trametinib 2mg once daily by mouth. The patient noticed a rapid reduction in her neck mass. Restaging FDG-PET scan performed 2 months after starting dabrafenib/trametinib (Fig. 43.1, panel b) showed significant reductions in size and FDG avidity within the right supraclavicular mass, right thyroid nodule, sternal metastasis, bilateral lung, pleural, and nodal disease in the chest and abdomen. The patient’s disease has remained stable on dabrafenib/trametinib.
Assessment and Literature Review
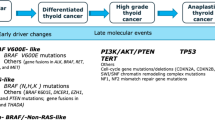
ATC is a rare form of thyroid cancer and the most aggressive. The clinical picture is of a rapidly growing neck mass causing dyspnea, stridor, hoarseness, and/or dysphagia. Because ATC is often derived from well-differentiated thyroid cancer (“anaplastic transformation”), patients may report a history of prior thyroid cancer. The diagnosis of ATC can be made via fine-needle (FNA), core, or incisional biopsy. Core biopsy or FNA with a cell block preparation is preferred, to allow for immunohistochemical staining for BRAFV600E and molecular testing. Image guidance is helpful to avoid tumor areas with significant necrosis to increase diagnostic yield.
BRAFV600E is the most common actionable mutation in ATC and influences initial treatment. Thus it must be assessed at diagnosis in all ATC patients. Although next-generation sequencing (NGS) of tumor is the gold standard for molecular testing, results can take several weeks to obtain. Therefore, rapid methods are used as an adjunct to NGS. The most rapid method is immunohistochemistry (IHC) staining for BRAFV600E protein [1]. This test should only be performed on FNA cell blocks or core/surgical specimens to maximize accuracy. The second test is cell-free DNA (cfDNA) on peripheral blood specimens [2, 3]. The pathologic diagnosis is at times difficult to make, as this is a rare tumor and there are many pathologic morphologies, some of which can mimic other cancers. For example, the squamous morphology is often confused with squamous cell carcinoma of the head and neck or lung.
Assessment of the airway, staging, and BRAFV600E status should be performed quickly and in tandem, in order to initiate treatment as soon as possible. The first step is to ensure that the airway is secure. The airway may be threatened by vocal cord paralysis, laryngeal edema, external compression, and/or direct invasion by disease. Laryngoscopy should be performed on all patients with a new diagnosis of ATC. Tracheostomy may be necessary to secure the airway in patients presenting with significant respiratory distress. Patients without respiratory distress or concerning physical exam findings may not require upfront prophylactic tracheostomy. Imaging of the neck and chest with contrast is necessary for staging and determination of resectability. Cross-sectional imaging with CT or MRI of the body and brain is also necessary to determine the extent of disease at other sites, as 50% of patients have distant metastases at diagnosis. FDG-PET/CT is very helpful with identifying areas of metastasis that may be difficult to evaluate with cross-sectional imaging alone.
Once staging is complete and BRAFV600E status has been determined, further treatment planning can start. Surgery can be considered as the primary treatment for stage IVA patients who are fit for surgery and can undergo resection without significant morbidity. Stage IVB patients (nodal metastasis or disease extending outside the thyroid without distant metastasis) with resectable disease may also be considered for upfront surgery on a case-by-case basis with goals of achieving complete resection. Surgery that leaves behind gross disease (R2) is not beneficial to patients and should not be performed. Furthermore, radical surgery such as laryngectomy and/or esophagectomy is not recommended in ATC patients. Stage IVB patients who do not have a BRAFV600E mutation and cannot be treated with surgical resection should receive external beam radiation to the neck with concomitant chemotherapy. Those who do have BRAFV600E-mutated stage IVB ATC may also undergo upfront chemoradiation. However, a newer approach to these patients is to start neoadjuvant dabrafenib plus trametinib and later undergo surgical resection followed by chemoradiation [4]. Ongoing clinical trials are evaluating whether this approach leads to improved survival.
Until recently, there were no effective systemic therapies for patients with stage IVC disease (distant metastasis). Targeted therapy against BRAFV600E with dabrafenib plus trametinib has shown high response rates (69%) and improved survival [5]. The median progression-free and overall survival were 14 and 20 months in clinical trial, respectively [6]. The BRAF/MEK inhibitor combination, dabrafenib/trametinib, is now approved in the USA and considered the standard of care for patients with tumors harboring a BRAFV600E mutation. It should be recognized, however, that the clinical trial that led to the approval enrolled only patients able to swallow whole pills. This likely biased the patient population. Others have reported shorter median overall survival [7, 8] and treatment resistance [9]. Thus, newer approaches to deter resistance, such as the addition of immunotherapy to the BRAF/MEK inhibitor combination [10], are being studied at this time.
In addition to BRAFV600E , gene fusions, particularly NTRK and RET fusions, are also potentially actionable in patients with ATC. There are currently selective NTRK and RET inhibitors approved for solid tumors harboring these fusions [11,12,13,14]. However, these alterations are rare in ATC, and response rates have not been established in a larger population of ATC patients.
Patients without an actionable mutation or fusion still lack effective therapies. Thus, patients with stage IVC without a BRAFV600E mutation should be referred for clinical trials. Emerging research suggests that the anti-PD1 checkpoint inhibitor, spartalizumab, may have efficacy in ATC patients with high PD-L1 expression and in those without a BRAFV600E mutation [15]. Combinations of checkpoint inhibitors [16] or checkpoint inhibitors plus targeted therapy [10] have also been studied in ATC and appear promising.
Clinical Pearls/Pitfalls
-
BRAFV600E mutation status is now part of the initial evaluation of ATC patients.
-
Rapid BRAF testing should be performed by immunohistochemistry on tumor biopsy specimens and/or assessment of cell-free DNA in peripheral blood.
-
Dabrafenib (BRAF inhibitor) and trametinib (MEK inhibitor) are effective for ATC patients with BRAFV600E mutation and now the standard of care.
-
Stage IVC ATC patients without a BRAFV600E mutation should be treated within the context of a clinical trial, as there are still no effective therapies for these patients.
References
Smith AL, Williams MD, Stewart J, Wang WL, Krishnamurthy S, Cabanillas ME, Roy-Chowdhuri S. Utility of the BRAF p.V600E immunoperoxidase stain in FNA direct smears and cell block preparations from patients with thyroid carcinoma. Cancer Cytopathol. 2018;126:406–13.
Iyer PC, Cote GJ, Hai T, Gule-Monroe M, Bui-Griffith J, Williams MD, Hess K, Hofmann M-C, Dadu R, Zafereo M, Busaidy NL, Ferrarotto R, Subbiah V, Gross N, Gunn BG, Skinner HD, Garden AS, Cabanillas ME. Circulating BRAF V600E cell-free DNA as a biomarker in the management of anaplastic thyroid carcinoma. JCO Precis Oncol. 2018;2:1–11.
Sandulache VC, Williams MD, Lai SY, Lu C, William WN, Busaidy NL, Cote GJ, Singh RR, Luthra R, Cabanillas ME. Real-time genomic characterization utilizing circulating cell-free DNA in patients with anaplastic thyroid carcinoma. Thyroid. 2017;27:81–7.
Wang JR, Zafereo ME, Dadu R, Ferrarotto R, Busaidy NL, Lu C, Ahmed S, Gule-Monroe MK, Williams MD, Sturgis EM, Goepfert RP, Gross ND, Lai SY, Gunn GB, Phan J, Rosenthal DI, Fuller CD, Morrison WH, Iyer P, Cabanillas ME. Complete surgical resection following neoadjuvant dabrafenib plus trametinib in BRAF(V600E)-mutated anaplastic thyroid carcinoma. Thyroid. 2019;29:1036–43.
Subbiah V, Kreitman RJ, Wainberg ZA, Cho JY, Schellens JHM, Soria JC, Wen PY, Zielinski C, Cabanillas ME, Urbanowitz G, Mookerjee B, Wang D, Rangwala F, Keam B. Dabrafenib and trametinib treatment in patients with locally advanced or metastatic BRAF V600-mutant anaplastic thyroid cancer. J Clin Oncol. 2017:JCO2017736785.
Keam B, Kreitman RJ, Wainberg ZA, Cabanillas ME, Cho DC, Italiano A, Stein A, Cho JY, Schellens JHM, Wen PY, Zielinski CC, Boran AD, Mookerjee B, Burgess P, Rangwala F, Subbiah V. Updated efficacy and safety data of dabrafenib (D) and trametinib (T) in patients (pts) with BRAF V600E–mutated anaplastic thyroid cancer (ATC). Ann Oncol. 2018;29(suppl_8):viii645–6.
Iyer P, Dadu R, Ferrarotto R, Busaidy N, Habra MA, Zafereo M, Gross ND, Hess K, Gule-Monroe M, Williams MD, Cabanillas M. Real world experience with targeted therapy for the treatment of anaplastic thyroid carcinoma. Thyroid. 2017;28:79–87.
Iyer PC, Dadu R, Gule-Monroe M, Busaidy NL, Ferrarotto R, Habra MA, Zafereo M, Williams MD, Gunn GB, Grosu H, Skinner HD, Sturgis EM, Gross N, Cabanillas ME. Salvage pembrolizumab added to kinase inhibitor therapy for the treatment of anaplastic thyroid carcinoma. J Immunother Cancer. 2018;6:68. https://doi.org/10.1186/s40425-018-0378-y.
Cabanillas ME, Dadu R, Iyer P, Wanland KB, Busaidy NL, Ying A, Gule-Monroe M, Wang JR, Zafereo M, Hofmann MC. Acquired secondary RAS mutation in BRAF(V600E)-mutated thyroid cancer patients treated with BRAF inhibitors. Thyroid. 2020;30(9):1288–96. https://doi.org/10.1089/thy.2019.0514.
Cabanillas ME, Dadu R, Ferrarotto R, Liu S, Fellman BM, Gross ND, Gule-Monroe M, Lu C, Grosu H, Williams MD, Duose D, Mallampati S, Dervin S, McKenna EF, Wang JR, Zafereo M, Busaidy N. Atezolizumab combinations with targeted therapy for anaplastic thyroid carcinoma (ATC). J Clin Oncol. 2020;38(Suppl):abstr 6514.
Bayer HeathCare Pharmaceuticals. Vitrakvi (larotrectinib) [package insert]. U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/211710s000lbl.pdf. Accessed 2 Jun 2020.
Roche Pharmaceutical. Rozlytrek (entrectinib) [package insert]. U.S. Food and Drug Adminstration website. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212725s000lbl.pdf. Accessed 2 Jun 2020.
Eli Lilly and Company. Retevmo (selpercatinib) [package insert]. U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213246s000lbl.pdf. Accessed 2 Jun 2020.
Wirth LJ, Sherman E, Robinson B, Solomon B, Kang H, Lorch J, Worden F, Brose M, Patel J, Leboulleux S, Godbert Y, Barlesi F, Morris JC, Owonikoko TK, Tan DSW, Gautschi O, Weiss J, de la Fouchardiere C, Burkard ME, Laskin J, Taylor MH, Kroiss M, Medioni J, Goldman JW, Bauer TM, Levy B, Zhu VW, Lakhani N, Moreno V, Ebata K, Nguyen M, Heirich D, Zhu EY, Huang X, Yang L, Kherani J, Rothenberg SM, Drilon A, Subbiah V, Shah MH, Cabanillas ME. Efficacy of Selpercatinib in RET-Altered Thyroid Cancers. N Engl J Med. 2020;383:825–35.
Capdevila J, Wirth LJ, Ernst T, Ponce Aix S, Lin CC, Ramlau R, Butler MO, Delord JP, Gelderblom H, Ascierto PA, Fasolo A, Fuhrer D, Hutter-Kronke ML, Forde PM, Wrona A, Santoro A, Sadow PM, Szpakowski S, Wu H, Bostel G, Faris J, Cameron S, Varga A, Taylor M. PD-1 Blockade in Anaplastic Thyroid Carcinoma. J Clin Oncol. 2020:JCO1902727.
Lorch JH, Barletta JA, Nehs M, Uppaluri R, Alexander EK, Haddad R, Hanna GJ, Margalit DN, Tishler RB, Schoenfeld JD, Goguen LA, Jabiev A, Sorensen MJ, Ahmadi S, Marqusee E, Kim MI, Stanizzi D, Harris E, Kacew A. Barbie DA. A phase II study of nivolumab (N) plus ipilimumab (I) in radioidine refractory differentiated thyroid cancer (RAIR DTC) with exploratory cohorts in anaplastic (ATC) and medullary thyroid cancer (MTC). J Clin Oncol. 2020;38(Suppl):abstr 6513.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cabanillas, M.E., Wang, J.R. (2021). A Patient with BRAFV600E-Mutated Anaplastic Thyroid Cancer with Metastatic Disease. In: Grani, G., Cooper, D.S., Durante, C. (eds) Thyroid Cancer. Springer, Cham. https://doi.org/10.1007/978-3-030-61919-0_43
Download citation
DOI: https://doi.org/10.1007/978-3-030-61919-0_43
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-61918-3
Online ISBN: 978-3-030-61919-0
eBook Packages: MedicineMedicine (R0)