Abstract
Tendon injuries in jumping sports are highly common. The biomechanical requirements of each discipline, the duration of training, and the frequency of explosive forces determine the type of injury. Acute and overuse injuries are seen most likely to occur at the lower extremities. The thigh, especially the hamstrings, is at high risk of acute injuries, including strains and ruptures. Overuse injuries more often occur at the patellar and Achilles tendon. Age, gender, and performance level of the athlete are influencing the incidence of those injuries. Adolescent athletes more often show apophyseal pathologies and insertional tendinopathy, whereas older athletes mainly suffer from midportion tendon injuries especially in Achilles tendons (Cassel M, et al. Front Physiol, 2019;10:544). Elite athletes seem to have a lower injury rate than high school athletes. Male athletes are at greater risk of acute or overuse injuries. The male-to-female ratio for complete Achilles tendon ruptures for instance varies between 7:1 and 4:1 in different studies (Vosseller JT, et al. Foot Ankle Int, 2013;34(1):49–53). Repetitive exposures and high total duration of exposure have been identified as significant risk factors for tendinopathies, whereas highly explosive events show a higher risk of acute tendon injuries in jumping sports (Lundberg Zachrisson A, et al. Inj Epidemiol, 2020;7(1):16). The biomechanical diagnosis of tendon injuries should be one of the standard examination methods today, as should imaging methods. It includes stabilometry, isokinetic force measurements (maximum force and rate of force development), running analysis, gait analysis, jump measuring plate, and isokinetic video analysis for the lower extremity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Biomechanics
Athletes competing in track and fields sustain huge impact forces, which need to be transported through the body. The basic function of the tendons is to transmit the force created in the muscle to the bone, thus making joint and limb movement possible [4]. To do this effectively, tendons must be capable of resisting high tensile forces with limited elongation [8]. Tendons tolerate extreme tensile forces during sprinting and jumping. Already during normal walking forces of about 2 times, body weight is acting on the Achilles tendon. With increased speed, these forces increase up to 12.5 times the body weight [5].
The top values reach 1.4 tons (calculated for the high jump world record of 2.45 m). Reference values of in vivo loads on the Achilles tendon during various sports activities are shown in Table 3.1.
Comparably, forces acting on the patellar tendon sometimes reach extremely high values (Fig. 3.1). For example, maximum forces of up to 17.5 times body weight were calculated during weightlifting [7]. In jumping, forces on the patellar tendon are about 2000 Nm in take-off and 3000 Nm in landing, which corresponds to a force equivalent of approx. 200 kg and 300 kg, respectively. In general, these huge stresses can be well compensated by the special microarchitecture of the tendons and by their enormous adaptability with a gradual increase in stress. However, in the presence of specific risk factors (Fig. 3.2) or pre-damage of the tendon, the risk of structural damage increases even without the maximum force values having to be achieved. The primary tear force of the tendon is described for the Achilles tendon with 1.8 tons or 25 times the body weight. Basically, all tendons are subject to a so-called stress–strain mechanism, whereby their elongation capacity up to structural injury is about 8%. Crucially, their stiffness/softness is determined by tendon quality, training condition, and various other influencing factors.
Sprint starts with visualization of the enormous soleus activity (40% push-off capacity) during knee flexion positions going over to gastrocnemius action (33% push-off capacity [5]) while stretching the knee
2 Anatomy
Tendons are composed of collagen fibers and tenocytes, which lie in parallel rows in the extracellular matrix that contains proteoglycans. It forms a dense connective tissue whose purpose usually is to connect muscle and bone and consecutively stabilizes joints and allows for movement through storage and release of energy.
Collagen fibers provide resistance to tensional stress, whereas proteoglycans add viscoelasticity to the tendon. From smallest to largest, the units forming the tendon are tropocollagen < collagen < fibril < fiber < fascicle. Multiple fascicles are surrounded by endotenon, which connects them to form the tendon. It allows for gliding of the fascicles to each other. Epitenon encircles the entire tendon and prevents adhesion to surrounding tissue.
The paratenon finally is the outermost layer further reducing friction between tendon and surrounding tissue [9, 10]. Endotenon and epitenon allow blood vessels and nerves to reach the deeper structures within the unit and prevent separation of the fascicles under stress. At the junction of tendon to bone, the enthesis represents a complex structure with different tissue properties including chondrocytes [11], vulnerable to asymmetrical load and potential of building heterotopic/intratendinous ossification (Fig. 3.3).
Unique anatomical structure of the Achilles tendon with a twist of 90°, from a frontal and a lateral point of view. Soleus fibers aim to the medial calcaneus, which is important to recognize for the biomechanical understanding of the Achilles tendon function (with kind permission by Robert Smigielski, Poland) from Ref. [12]
3 Mechanobiology
Adaptation of tendons to repetitive loading has been increasingly understood in recent years, especially the fact that load is important for remodeling and/or healing of tendons. While tendons in the past were primarily considered poorly vascularized, bradytrophic tissue, their high adaptability to physical stress and their outstanding mechanical properties have recently been increasingly recognized. The latter make them at the same time highly resistant and elastic [13]. The interaction between the mechanical stresses and the responses at the cellular level takes place via a complex homeostatic, mechanobiological feedback [14]. It has long been assumed that the adaptability of tendons in terms of blood circulation and implementation of the extracellular matrix under load are very low. Today, however, it is known that the metabolism of the collagen and the remaining connective tissue adapts to the load and the metabolic activity changes according to the physical activity. Various clinical–experimental works have shown that the oxygen and glucose uptake of the tendon increases under mechanical stress [13]. A recently published meta-analysis impressively summarized how enormously adaptable the tendon is in terms of its mechanical, morphological, and structural properties [15]. Sustainable adaptation can be achieved in particular through high-load training and high intensities over a longer period of time (>12 weeks). On the other hand, the training or contraction form of the muscles (isometric/concentric/eccentric) seems to play a subordinate role.
Current data demonstrate that chronic exposure of the AT to elevated jumping loads results in adaptation of its mechanical and material properties. The Achilles tendon in the jump leg of male collegiate-level jumping athletes had 17.8% greater stiffness and a 24.4% greater Young’s modulus (compared to the contralateral lead (non-jump) leg, respectively). The side-to-side differences in jumpers were greater than observed in a cohort of athletic controls, suggesting that they are not simply due to limb dominance [16].
Jumpers also had 35.3% and 76.7% greater tendon stiffness and Young’s modulus in their jump leg compared to that in the jump leg of athletic (non-jumping) controls [17].
The greater AT Young’s modulus and stiffness in the jump leg of jumpers represent a favorable adaptation. During jumping, a structurally and materially stiffer tendon enables an improved ability to transmit muscle-generated forces, which improved explosive activity performance (jump force and height).
From a pathological standpoint, a stiffer tendon is exposed to greater stress, which may be considered potentially dangerous. However, tendon ultimate stress (i.e., the stress at which a tendon fails) is directly correlated with the tendon Young’s modulus [18]. Thus, the increase in Young’s modulus observed in jump leg of jumpers would be associated with the tendon being able to tolerate more stress before failure.
4 Pathophysiology
Pathophysiological processes have to be divided into different subgroups: “Tendinosis” a group of chronic-degenerative conditions usually of the midsubstance tendon caused by repetitive microtrauma. No inflammatory process can be made accountable for this condition. “Tendinitis” on the other hand is a painful inflammatory process mediated by cytokines and matrix metalloproteinases (MMPs). “Tenosynovitis” is a term describing inflammation of the paratenon with or without additional tendinosis. Lastly, a “rupture” or “tendon tear” is the loss of continuum of the tendon resulting in significant loss of function [19]. As already mentioned with the term “tendinosis,” classic inflammatory changes can rarely be histologically detected. Terms such as “epicondylitis humeri lateralis” or “patellar tendonitis” should therefore be abandoned and named “-tendinosis” or “-tendinopathy” instead [20].
Significant changes can, however, be found histologically, indicating a dysfunctional healing response after microtrauma: thinning, disrupted collagen fibers, neoangiogenesis resulting in increased vascularity and cellularity, granulation tissue, and increased proteoglycan content [21]. Adams et al. already demonstrated in 1974 that age-related changes like tenocyte degeneration, accumulation of lipid amorphous extracellular matrix, and hydroxyapatite deposits could be found in early age affecting different tendons throughout the human body [22]. In comparison with normal tendon with well-aligned parallel and compact collagen fibers with adjacent tenocytes, the most prominent changes occur in the disorganization of the tendon matrix represented by discontinuous, crimped, and thinned collagen fibers with loss of their typical organized structure. Pathological tendons reveal loss of matrix integrity by reduction in total collagen content and increased production of extracellular matrix components that result in tendon stiffening [23].
Sonographic evaluation can reveal intra- and peritendinous changes including collagen disorganization and hypoechogenicity. Neovascularization can be found in combination with these degenerative changes, which are accompanied by nerve sprouting and hypersensitivity [24]. Jumpers are at high risk to be affected by tendinopathy of the patellar tendon as shown above. That is why it is also termed “jumper’s knee.” It can be classified depending on the location: The inferior pole of the patella is predisposed to injury due to maximum tensional stress during loading [25]. Less often but still relevant are the midportion and insertion at the tibial tuberosity [26]. It is important to detect coexisting changes in the Hoffa fat pad to initiate the correct therapy [27].
High levels of tendon strain are associated with a micromorphological deterioration of the collagenous network in the proximal patellar tendon of adolescent jumping athletes. Further, athletes suffering from or developing tendinopathy demonstrated both greater levels of tendon strain and lower levels of fascicle packing and alignment, which lends support to the idea that mechanical strain is the primary mechanical factor for tendon damage accumulation and the progression of overuse [28]. Finally, tendon rupture is associated with degenerative changes and also linked to the impairment of native repair mechanisms to defend the tendon from degeneration and ultimately rupture [29].
5 Pathomechanics
When classifying tendon injury mechanisms, acute injuries have to be distinguished from overload-associated damage and chronic-degenerative injuries (tendinopathy).
5.1 Acute Injury Patterns
Acute injuries mainly occur when large eccentric force acts on the tendon. A tendon is a remarkably strong tissue. Its in vitro tensile strength is about 50–100 N/mm2. The cross-sectional area and the length of the tendon affect their mechanical behavior. The greater the tendon cross-sectional area, the larger loads can be applied prior to failure (increased tendon strength and stiffness). A tendon with a cross-sectional area of 1 cm2 is capable of supporting a weight of 500–1000 kg. Athletes who subject their Achilles tendon to repetitive loads as habitual runners have shown larger Achilles tendon cross-sectional area than control subjects [12, 13]. An increased tendon cross-sectional area would reduce the average stress of the tendon, thereby decreasing the risk of acute tensile tendon rupture.
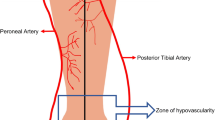
The breaking force of the Achilles tendon in vivo is as high at 18`000 Newton (equivalent to about 1.8 tons) or 25 times body weight. However, this only applies to axial load on the tendon. Brüggemann and Segesser were able to demonstrate a different tensile behavior with nonaxial strains act on the tendon and postulate it as a risk factor for Achilles tendon ruptures [7] and possible risk factor for overuse (Fig. 3.4).
This can be illustrated by the example of the tensile load of a sheet of paper. As long as the paper is pulled straight, it is very resistant. If the tension is applied asymmetrically, sideways, the paper tears with significantly less effort. Thus, it is also easy to understand that pre-damaged tendons are particularly at risk for acute (partial) ruptures in the case of asymmetric tensile loads. The decrease in the tear force of symptomatic Achilles tendons with detectable pathological structural changes was illustrated in a prospective study by Nehrer et al. 28% of patients with sonographically detectable degenerations showed spontaneous ruptures within the following 4 years. Achilles tendon tears, however, are not limited to the structure of the tendon, but also extend to adjacent structures. Thus, more than 80% of the acute Achilles tendon ruptures also have lesions of the M. soleus usually found at the level of the soleus insertion. This could be caused by an asymmetric tensile load between gastrocnemius and soleus muscles.
Thus, the injury of the medial musculotendinous junction of the gastrocnemius head is easily comprehensible when there is an unnatural position of the calcaneus. If an increased varus position of the calcaneus is added with activated gastrocnemius muscles, the medial gastrocnemius fibers are maximally stressed. Because the corresponding tendon fibers of the medial gastrocnemius portion insert distally and laterally at the calcaneus, they have the largest lever arm of the triceps surae muscles and the longest fibers. The eccentric braking movement in this strain position and the maximum, partly asymmetric pull lead to an increased risk of injury. Very high forces associated with a high risk of complete tendon tearing act on the patellar tendon in knee dislocations, whereby chronic-degenerative overload damage at the patellar tendon is still much more common than ruptures. Typical tendon ruptures still occur as an injury to the most eccentrically loaded tendons and as bony apophysis tears in adolescence. Other acute forms of injury are tendon dislocations, mainly on the peroneal tendons (in ankle sprain) and biceps femoris (in knee dislocation) and tibialis posterior (in pronation trauma).
5.2 Chronic Injury Patterns
Chronic tendinopathies belong to the category of overload damage, which is very common in sports, but is often perceived only poorly or even belatedly [30]. The tendons are often subject to a disproportion of high loads with too low regeneration times. Depending on the type and quantity of the load acting on the tissue, dye distinguished a zone of homeostasis, a zone of supraphysiological overload, and a zone of overload, which can cause structural tissue damage. Repetitive loads are associated with immense force values. For example, in a marathon run in world record time, the Achilles tendon is charged at an average speed of more than 20 km/h at each step with approx. 9000 Nm (900 kg) [31], which in total at approx. 800 steps per km, to 42 km (approx. 33,000 steps), corresponds to an equivalent weight force of about 33,000 times the weight of a small car (900 kg) acting on the Achilles tendons. Another example is the total load of approx. 150 tons per patellar tendon during volleyball training with approx. 300 jumps.
It should be noted that an optimally dosed and axis appropriate training can lead to a structural adaptation of the tendon (mechanobiology) and to an enlarged tendon cross section, as Couppe et al. (2009) have shown for the patellar tendon [32]. Here, 30% larger tendon cross sections in the jumping leg of female athletes compared to the nondominant leg and 20% larger tendon cross sections in male athletes in jumping and running sports compared to nonstressing sports (kayak) [33]. In order to prevent tendon injuries, therefore, in sports medicine and sports science, monitoring of stress or symptoms is increasingly being used [34,35,36]. The risk constellation for tendon injuries in old age is controversially discussed. Although the tendons of older persons have histopathologically 30% lower collagen concentrations, they nevertheless show the same mechanical strength due to compensatory increase in the collagen cross-connections (“crosslinks”) [37]. It should also be noted that tendon adaptation can work through ideal training even in old age. Accordingly, one cannot assume an aging process alone, but rather an inactivity process. This is naturally due to comorbidities, such as movement-limiting cardiovascular diseases, arthrosis of the joints, gout, diabetes mellitus or other metabolic pathologies, and increased drug requirements (Fig. 3.2). A very plausible explanation of pathomechanisms was recently postulated by Kjaer et al. [38]. They showed the expression of growth factors and inflammatory mediators that affect collagen synthesis and proteoglycan activity in the peritendineum. The tendons most commonly affected by overload damage (tendinopathies) are the Achilles tendon (usually called midportion tendinopathies in the middle of the tendon, rarer than insertion tendinopathies at the calcaneus approach), the patellar tendon (“jumper’s knee”), the quadriceps tendon, the plantar fascia, and the proximal tendons of the ischiocrural muscles. On average, 36% of volleyball players complain of knee pain over the course of a season, most often due to tendinopathy of the patellar tendon [35]. For a sustainable treatment of affected athletes, a good biomechanical understanding of the load and the knowledge of the intrinsic and extrinsic risk factors are of enormous importance. For the tendinopathy of the patellar tendon, nine specific factors could be identified. These include male sex [39], high weight [40], high training volume [41, 42], high muscle strength of the quadriceps [43, 44], high bounce [36] and training on asphalt [42], sports specialization [45], and reduced flexibility of quadriceps [46] and hamstrings [46, 47]. Frequently attempts have been made to prove a link between axis abnormalities and disturbances of the kinematic chain and the occurrence of patellar tendon tendinopathies (PTs), as it is obvious that these can lead to asymmetric tensile forces and thus increased loads of the patellar tendon and cause damage similar to the finding of Segesser and Brüggemann in the Achilles tendon. While no clear link has been established for the often accused pathological Q-angle (e.g., [42]), there is evidence that both leg length differences, a flattened arch [48, 49], a patella alta [50], and a disturbed patella tracking [51] can be accompanied by patellar tendon tendinopathies. Van der Worp et al. (2014) [49] also showed that the horizontal landing phase of jumps forward is crucial for the development of patellar tendinopathy. Patients with patellar tendon tendinopathies often end up with more bent knee and hip joints, so that further hip and knee flexion and thus a cushioning of the eccentric forces are less possible. The landing is therefore “harder” and is coined with higher peak forces in the patellar tendon. In summary, it can be said that both a thorough orthopedic examination and a biomechanical analysis of the movement patterns in chronic patellar tendon tendinopathies are of great importance (Table 3.2).
6 Biomechanical Diagnostics and Therapy
According to these explanations, which are similarly transferable to other tendinopathies, both the stress pattern and the therapy should be biomechanically analyzed or verified and causal malfunctions should be eliminated. The latter can be done, for example, by adaptation of the movement patterns, e.g., by shoe insert supply or specific muscular stabilization forms. The biomechanical diagnosis of tendon injuries should be one of the standard examination methods today, as should imaging methods. It includes stabilometry, isokinetic force measurements (maximum force and rate of force development), running analysis, gait analysis, jump measuring plate, and isokinetic video analysis for the lower extremity. For the upper limb, these are isokinetic force measurements, video analysis, physiotherapeutic verification of scapula coordination, and muscle length measurement. Due to the explained biomechanical and mechanobiological aspects, the individualized therapy of the causal disorder should also be adapted and include various treatment approaches such as training adaptation, technology optimization, material equipment (shoe equipment, inserts), axis training, elimination of disruptive influencing factors (where possible), and “heavy slow resistance” training, “heavy load eccentric training,” and “tendon neuroplastic training” (TNT) [52,53,54,55,56]. Summary tendons are subject to extremely large force effects, which are well-tolerated under normal conditions and even lead to tendon adaptation with improvement of the mechanical properties of the tendon during ideal training. Various influencing factors of an intrinsic and extrinsic nature can make the tendon susceptible for overload damage (tendinopathies). An asymmetrically eccentric load is particularly dangerous for the tendons. These pathomechanical aspects in the development of tendon pathologies must be diagnosed and eliminated in order to ensure a sustainable freedom of complaint for the patients concerned.
Change history
18 February 2022
This book was inadvertently published with a typo in the book title: the term “injures” has been corrected to “Injuries”
References
Cassel M, Muller J, Moser O, et al. Orthopedic injury profiles in adolescent elite athletes: a retrospective analysis from a sports medicine department. Front Physiol. 2019;10:544.
Vosseller JT, Ellis SJ, Levine DS, et al. Achilles tendon rupture in women. Foot Ankle Int. 2013;34(1):49–53.
Lundberg Zachrisson A, Ivarsson A, Desai P, et al. Athlete availability and incidence of overuse injuries over an athletics season in a cohort of elite Swedish athletics athletes - a prospective study. Inj Epidemiol. 2020;7(1):16.
Maquirriain J. Achilles tendon rupture: avoiding tendon lengthening during surgical repair and rehabilitation. Yale J Biol Med. 2011;84(3):289–300.
Komi PV, Fukashiro S, Jarvinen M. Biomechanical loading of Achilles tendon during normal locomotion. Clin Sports Med. 1992;11(3):521–31.
Weisskopf L, Drews B, Hirschmüller A, et al. In: Engelhardt M, Mauch F, editors. Pathomechanik und Verletzungsmuster – Teil 2: Sehnen, in Muskel- und Sehnenverletzungen. Verlag VOPELIUS, Jena; 2017. p. 49–58.
Zernicke RF, Garhammer J, Jobe FW. Human patellar-tendon rupture. J Bone Joint Surg Am. 1977;59(2):179–83.
Meeuwisse WH. Predictability of sports injuries. What is the epidemiological evidence? Sports Med. 1991;12(1):8–15.
Docheva D, Muller SA, Majewski M, et al. Biologics for tendon repair. Adv Drug Deliv Rev. 2015;84:222–39.
Schneider M, Docheva D. Mysteries behind the cellular content of tendon tissues. J Am Acad Orthop Surg. 2017;25(12):e289–90.
Yan Z, Yin H, Nerlich M, et al. Boosting tendon repair: interplay of cells, growth factors and scaffold-free and gel-based carriers. J Exp Orthop. 2018;5(1):1.
Freedman BR, Gordon JA, Soslowsky LJ. The Achilles tendon: fundamental properties and mechanisms governing healing. Muscles Ligaments Tendons J. 2014;4(2):245–55.
Kjaer M, Langberg H, Heinemeier K, et al. From mechanical loading to collagen synthesis, structural changes and function in human tendon. Scand J Med Sci Sports. 2009;19(4):500–10.
Thompson MS. Tendon mechanobiology: experimental models require mathematical underpinning. Bull Math Biol. 2013;75(8):1238–54.
Bohm S, Mersmann F, Arampatzis A. Human tendon adaptation in response to mechanical loading: a systematic review and meta-analysis of exercise intervention studies on healthy adults. Sports Med Open. 2015;1(1):7.
Bayliss AJ, Weatherholt AM, Crandall TT, et al. Achilles tendon material properties are greater in the jump leg of jumping athletes. J Musculoskelet Neuronal Interact. 2016;16(2):105–12.
Bojsen-Moller J, Magnusson SP, Rasmussen LR, et al. Muscle performance during maximal isometric and dynamic contractions is influenced by the stiffness of the tendinous structures. J Appl Physiol. 1985;99(3):986–94.
LaCroix AS, Duenwald-Kuehl SE, Lakes RS, et al. Relationship between tendon stiffness and failure: a metaanalysis. J Appl Physiol. 1985;115(1):43–51.
Dakin SG, Dudhia J, Smith RK. Resolving an inflammatory concept: the importance of inflammation and resolution in tendinopathy. Vet Immunol Immunopathol. 2014;158(3-4):121–7.
Khan KM, Cook JL, Kannus P, et al. Time to abandon the “tendinitis” myth. BMJ. 2002;324(7338):626–7.
Khan KM, Cook JL, Bonar F, et al. Histopathology of common tendinopathies. Update and implications for clinical management. Sports Med. 1999;27(6):393–408.
Adams CW, Bayliss OB, Baker RW, et al. Lipid deposits in ageing human arteries, tendons and fascia. Atherosclerosis. 1974;19(3):429–40.
Jarvinen M, Jozsa L, Kannus P, et al. Histopathological findings in chronic tendon disorders. Scand J Med Sci Sports. 1997;7(2):86–95.
Comin J, Cook JL, Malliaras P, et al. The prevalence and clinical significance of sonographic tendon abnormalities in asymptomatic ballet dancers: a 24-month longitudinal study. Br J Sports Med. 2013;47(2):89–92.
Malliaras P, Cook J, Purdam C, et al. Patellar tendinopathy: clinical diagnosis, load management, and advice for challenging case presentations. J Orthop Sports Phys Ther. 2015;45(11):887–98.
Sarimo J, Sarin J, Orava S, et al. Distal patellar tendinosis: an unusual form of jumper's knee. Knee Surg Sports Traumatol Arthrosc. 2007;15(1):54–7.
Ward ER, Andersson G, Backman LJ, et al. Fat pads adjacent to tendinopathy: more than a coincidence? Br J Sports Med. 2016;50(24):1491–2.
Schechtman H, Bader DL. In vitro fatigue of human tendons. J Biomech. 1997;30(8):829–35.
Carmont MR, Silbernagel KG, Nilsson-Helander K, et al. Cross cultural adaptation of the Achilles tendon Total rupture score with reliability, validity and responsiveness evaluation. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1356–60.
Bahr R. No injuries, but plenty of pain? On the methodology for recording overuse symptoms in sports. Br J Sports Med. 2009;43(13):966–72.
Arndt AN, Komi PV, Bruggemann GP, et al. Individual muscle contributions to the in vivo achilles tendon force. Clin Biomech (Bristol, Avon). 1998;13(7):532–41.
Couppe C, Hansen P, Kongsgaard M, et al. Mechanical properties and collagen cross-linking of the patellar tendon in old and young men. J Appl Physiol (1985). 2009;107(3):880–6.
Kongsgaard M, Aagaard P, Kjaer M, et al. Structural Achilles tendon properties in athletes subjected to different exercise modes and in Achilles tendon rupture patients. J Appl Physiol (1985). 2005;99(5):1965–71.
Clarsen B, Bahr R, Heymans MW, et al. The prevalence and impact of overuse injuries in five Norwegian sports: application of a new surveillance method. Scand J Med Sci Sports. 2015;25(3):323–30.
Clarsen B, Ronsen O, Myklebust G, et al. The Oslo sports trauma research center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med. 2014;48(9):754–60.
Visnes H, Aandahl HA, Bahr R. Jumper’s knee paradox--jumping ability is a risk factor for developing jumper’s knee: a 5-year prospective study. Br J Sports Med. 2013;47(8):503–7.
Couppe C, Kongsgaard M, Aagaard P, et al. Differences in tendon properties in elite badminton players with or without patellar tendinopathy. Scand J Med Sci Sports. 2013;23(2):e89–95.
Kjaer M, Bayer ML, Eliasson P, et al. What is the impact of inflammation on the critical interplay between mechanical signaling and biochemical changes in tendon matrix? J Appl Physiol (1985). 2013;115(6):879–83.
Lian O, Dahl J, Ackermann PW, et al. Pronociceptive and antinociceptive neuromediators in patellar tendinopathy. Am J Sports Med. 2006;34(11):1801–8.
Lian O, Refsnes PE, Engebretsen L, et al. Performance characteristics of volleyball players with patellar tendinopathy. Am J Sports Med. 2003;31(3):408–13.
Visnes H, Bahr R. Training volume and body composition as risk factors for developing jumper's knee among young elite volleyball players. Scand J Med Sci Sports. 2013;23(5):607–13.
Ferretti A. Epidemiology of jumper's knee. Sports Med. 1986;3(4):289–95.
Janssen I, Steele JR, Munro BJ, et al. Sex differences in neuromuscular recruitment are not related to patellar tendon load. Med Sci Sports Exerc. 2014;46(7):1410–6.
Janssen I, Steele JR, Munro BJ, et al. Predicting the patellar tendon force generated when landing from a jump. Med Sci Sports Exerc. 2013;45(5):927–34.
Cerullo G, Puddu G, Conteduca F, et al. Evaluation of the results of extensor mechanism reconstruction. Am J Sports Med. 1988;16(2):93–6.
Witvrouw E, Bellemans J, Lysens R, et al. Intrinsic risk factors for the development of patellar tendinitis in an athletic population. A two-year prospective study. Am J Sports Med. 2001;29(2):190–5.
Witvrouw E, Lysens R, Bellemans J, et al. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28(4):480–9.
Van der Worp H, de Poel HJ, Diercks RL, et al. Jumper’s knee or lander’s knee? A systematic review of the relation between jump biomechanics and patellar tendinopathy. Int J Sports Med. 2014;35(8):714–22.
van der Worp H, van Ark M, Roerink S, et al. Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med. 2011;45(5):446–52.
Kujala UM, Friberg O, Aalto T, et al. Lower limb asymmetry and patellofemoral joint incongruence in the etiology of knee exertion injuries in athletes. Int J Sports Med. 1987;8(3):214–20.
Allen GM, Tauro PG, Ostlere SJ. Proximal patellar tendinosis and abnormalities of patellar tracking. Skelet Radiol. 1999;28(4):220–3.
Alfredson H, Pietila T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26(3):360–6.
Beyer R, Kongsgaard M, Hougs Kjaer B, et al. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: a randomized controlled trial. Am J Sports Med. 2015;43(7):1704–11.
Kongsgaard M, Aagaard P, Roikjaer S, et al. Decline eccentric squats increases patellar tendon loading compared to standard eccentric squats. Clin Biomech (Bristol, Avon). 2006;21(7):748–54.
Kongsgaard M, Kovanen V, Aagaard P, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sports. 2009;19(6):790–802.
Rio E, Kidgell D, Moseley GL, et al. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br J Sports Med. 2016;50(4):209–15.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 ISAKOS
About this chapter
Cite this chapter
Weisskopf, L., Hesse, T., Sokolowski, M., Hirschmüller, A. (2022). Tendons and Jumping: Anatomy and Pathomechanics of Tendon Injuries. In: Canata, G.L., D'Hooghe, P., Hunt, K.J., M. M. J. Kerkhoffs, G., Longo, U.G. (eds) Management of Track and Field Injuries. Springer, Cham. https://doi.org/10.1007/978-3-030-60216-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-60216-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-60215-4
Online ISBN: 978-3-030-60216-1
eBook Packages: MedicineMedicine (R0)