Summary
Introduction: Advanced multimodal monitoring (MMM) of the brain is recommended as a tool to manage severe acute brain injury in intensive care units (ICUs) and prevent secondary lesions. The aim of this study was to determine if MMM has implications for patient outcome and mortality.
Methods: We analyzed data on 389 patients admitted with a subarachnoid hemorrhage (SAH) or traumatic brain injury (TBI) to two general ICUs and one neurocritical care ICU (NCCU) between March 2014 and October 2016, and their subsequent outcomes.
Results: The study population consisted of 259 males and 130 females. Group 1, which comprised 69 patients with MMM admitted to the NCCU, was compared with group 2, which comprised patients managed without MMM. With the exceptions of the Simplified Acute Physiology Score (SAPS II) and Glasgow Coma Scale (GCS) scores, there were no differences between the two groups. Group 1 had significantly better outcomes at ICU discharge, at 28 days, and at 3 months, and also had a lower mortality rate (P < 0.05). When outcomes were adjusted for SAPS II scores, patients who had MMM had better outcomes (odds ratios 0.215 at ICU discharge, 0.234 at 28 days, 0.338 at 3 months, and 0.474 at 6 months) but no difference in mortality.
Conclusion: Use of MMM in patients with SAH or TBI is associated with better outcomes and should be considered in the management of these patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The primary focus of neurocritical care is early detection and prevention of secondary brain injury because the impact of the primary lesion is often irreversible [1]. Thus, advanced multimodal monitoring (MMM) of the brain has been recommended as an important tool to manage severe acute brain injury in intensive care units (ICUs). MMM allows simultaneous and continuous assessment of cerebral hemodynamics, oxygenation, and metabolism, providing an individualized approach at the bedside [2]. MMM should be done in a continuous way so as not to overlook clinically significant events. Data should be collected simultaneously, time synchronized, and displayed in an integrated fashion [2] to provide targeted individualized care. MMM of the brain includes monitoring provided by different devices, including intracranial pressure (ICP), cerebral perfusion pressure (CPP), cerebral oximetry with near-infrared spectroscopy (NIRS), brain tissue oxygen partial pressure (pbtO2), and cerebral blood flow (CBF) evaluated by transcranial Doppler ultrasonography and/or by thermal diffusion flowmetry.
Use of the pressure reactivity index (PRx) for continuous assessment of autoregulation and optimal CPP [3] is the fulcrum of MMM and is feasible at the bedside [4]. Impaired autoregulation leads to secondary injury and is an independent predictor of a fatal outcome following acute brain injury (ABI) [4]. Although there are retrospective published data on the association between cerebral autoregulation and acute brain injury outcomes [5,6,7,8], suggesting that preserved autoregulation leads to a better prognosis, there is a lack of robust evidence that use of MMM (including PRx) and treatment by a dedicated team contributes to better outcomes. Outcomes at ICU discharge, 28 days, 3 months, and 6 months can be assessed with use of the Glasgow Outcome Scale (GOS). A GOS score of 1 means death, a score of 2 means a persistent vegetative state, a score of 3 means severe disability, a score of 4 means moderate disability, and a score of 5 means good recovery [9].
The aim of this study was to determine if MMM has implications for mortality and outcomes in patients with severe acute brain injury—namely, severe aneurysmal subarachnoid hemorrhage (SAH) or severe traumatic brain injury (TBI).
Materials and Methods
Patient Selection
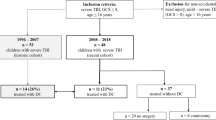
This study included all patients admitted with a diagnosis of severe aneurysmal SAH or severe TBI to two general ICUs and one neurocritical care ICU (level III) in the same intensive care department at Centro Hospitalar Universitário São João between March 2014 and December 2016. Severity was defined by clinical evaluation and the decision to manage the patient with level III care. A total of 389 patients were included in the study.
Patients less than 18 years old, pregnant females, and patients with expected survival of <3 days were excluded. The research ethics committee at Centro Hospitalar Universitário São João approved the study protocol and data collection.
Data Collection
Patient files were reviewed retrospectively, and data on several demographic and clinical variables were recorded—namely, the patient’s age, sex, Glasgow Coma Scale score at ictus and at hospital admission, pupillary response at admission, blood glucose level, blood pressure (absence or presence of hypotension, defined as systolic arterial blood pressure <90 mmHg), oxygenation (absence or presence of hypoxemia with peripheral oxygen saturation (SpO2) of <90%), and the presence or absence of seizures. Disease severity and mortality prediction on admission were calculated by use of the Simplified Acute Physiology Score (SAPS II). For SAH, other scales of severity were also used: the Hunt and Hess Scale, the Fisher Scale [10], and the World Federation of Neurological Surgeons (WFNS) Grading Scale [11, 12].
With regard to systemic monitoring, all patients were managed with a Philips Intellivue multiparameter monitor, which allowed continuous bedside acquisition of electrocardiographic, heart rate, respiratory rate, invasive arterial blood pressure, pulse oximetry, and end-tidal CO2 data. With regard to MMM of the brain [4], ICP wave, CPP, NIRS, pbtO2, and CBF data were recorded. For evaluation of autoregulation, PRx was continuously calculated at the bedside, using ICM+ software. PRx was calculated as the Pearson coefficient between 30 consecutive 10-s averaged values of arterial blood pressure (ABP) and corresponding ICP signals. A positive correlation between ABP and ICP at a low frequency indicates passive cerebral vessels and impaired autoregulation. A zero or negative correlation indicates intact autoregulation [5]. The optimal CPP is the CPP value with the lowest associated PRx value. Outcomes at ICU discharge, 28 days, 3 months, and 6 months were assessed with use of the GOS.
Statistical Analysis
Continuous variable data were expressed as mean values with standard deviations or medians and 25th–75th percentile ranges. Categorical variable data were presented as numbers (n) and percentages (%). The GOS score was dichotomized into a poor outcome (GOS score ≤ 3) and a good outcome (GOS score > 3), and comparative analysis was performed for all patients and also separately for the two subgroups of patients with TBI and SAH. When a hypothesis about continuous variables was being tested, nonparametric Mann–Whitney or Kruskall–Wallis tests were used, as appropriate, taking into account normality assumptions and the number of groups compared. When a hypothesis about categorical variables was being tested, a χ 2 test and a Fisher’s exact test were used, as appropriate. To gain more thorough understanding of the factors associated with a poor outcome and mortality (dependent variables), univariate and multivariate logistic regression modeling was used with sex, age, glycemia, hypotension, and the Glasgow Coma Scale at first aid and the kind of ICU (general versus NeuroCritical) as independent variables.
The significance level used was 0.05. Statistical analyses was performed using SPSS version 24.0 software.
Results
The total studied population consisted of 389 patients: 95 with SAH and 294 with TBI. The overall median age was 61 (17–97) years; the median ages were 64 years in patients with SAH and 60 years in those with TBI. The ICU lengths of stay (LOSs) for SAH and TBI were 12 (6–28) and 15 (8–23) days, respectively, and the hospital LOSs were 29 (18–52) and 30 (17–49) days, respectively, with no statistical differences between the two groups. The SAPS II score was 44 in patients with SAH and 32 in those with TBI (P < 0.0001). There were no differences between SAH and TBI in terms of the pupillary response at hospital admission. With regard to hypoxia, 29 patients with TBI versus only 3 with SAH presented SpO2 values <90% (P = 0.039). Hypotension was also more frequent in TBI patients than in SAH patients (12.6% versus 4.2%, P = 0.021). In terms of metabolic control, 39.8% of TBI patients versus 23.2% of SAH were hyperglycemic and 57.1% of TBI patients versus 68.4% of SAH patients were normoglycemic (P = 0.003).
With regard to outcomes at ICU discharge, 47.4% of patients with SAH had a poor outcome, compared with 77.1% of those with TBI (P < 0.001). Good outcomes were recorded in 55.3% of patients with SAH versus 31.6% of those with TBI at 28 days (P < 0.001), 74.7% versus 50.2% at 3 months (P < 0.001), and 81% versus 56.5% at 6 months (P < 0.001) (Table 1).
Of the 259 males, 221 had TBI and 38 had SAH; of the 130 females, 73 had TBI and 57 had SAH.
A second analysis was done in which two different groups were compared: group 1, comprising 69 patients managed with MMM and use of PRx; and group 2, comprising 320 patients managed without MMM in either a general ICU or the NCCU.
In this comparison of the above groups, there were no differences in age, sex, ICU LOS, or hospital LOS. The median Glasgow Coma Scale (GCS) scores at hospital admission were 4 (3–12) in group 1 versus 8 (3–13) in group 2 (P = 0.050). The median SAPS II scores were 40 (29–49) in group 1 versus 43 (33–55) in group 2 (P = 0.047) (Table 2).
With regard to outcomes, good outcomes were seen in 59% of group 1 versus 24% of group 2 at ICU discharge, 65% versus 30% at 28 days, and 77% versus 51% at 3 months (P < 0.001 at all three times of evaluation). At 6 months, good outcomes were seen in 78% of group 1 versus 59% of group 2 (P = 0.005).
The mortality rates were 7% in group 1 versus 19% in group 2 at ICU discharge (P = 0.020), 7% versus 20% at 28 days (P = 0.013), 9% versus 25% at 3 months (P = 0.008), and 13% versus 25% at 6 months (P = 0.039).
When outcomes were adjusted for injury severity (evaluated by SAPS II) with poor outcome as a dependent variable, the odds ratios were 0.215 at ICU discharge (P < 0.001), 0.234 at 28 days (P < 0.001), 0.338 at 3 months (P < 0.001), and 0.474 at 6 months (P = 0.044). Thus, the differences between groups 1 and 2 persisted despite adjustment for injury severity.
However, when mortality was adjusted for the SAPS II score, there were no significant differences between groups 1 and 2.
Discussion
Our comparison between TBI and SAH confirmed our clinical and subjective perceptions that at baseline, TBI patients are more severely injured; in fact, they had higher SAPS II scores and higher rates of hypoxemia and hypotension. Although there were no differences in mortality between these two groups until 6 months (at which stage, mortality was higher in TBI patients), their outcomes were clearly different, and patients with SAH had better outcomes than those with TBI. We hypothesized that this might depend on the initial insult and inability to promptly revert causes of secondary lesions, such as hypoperfusion and hypoxemia, since the initial diagnosis (either TBI or SAH) did not limit or direct the type of monitoring used in each patient. Another hypothesis was that if MMM was used in patients with acute brain injury, their prognoses would be better. For that reason, we analyzed two different groups on the basis of use or nonuse of MMM. Despite statistical differences between the two groups at baseline, when the results were adjusted for severity scores, outcomes were better in patients who received MMM (including use of PRx). Whether this benefit arose from use of all of the monitoring devices together or from use of one device in particular warrants further investigation.
Conclusion
Despite the limitations of a small population (n = 389), our study showed that use of MMM was beneficial. Outcomes at all points of evaluation were better in patients managed with MMM. Regarding mortality the group with MMM had lower mortality rates. Use of a dedicated team to manage patients with acute brain lesions may contribute to improve outcomes and reduce mortality. However, this work warrants further validation, preferably in a multicenter, randomized, controlled study.
References
Roh D, Soojin P (2016) Brain multimodality monitoring: updated perspectives. Curr Neurol Neurosci Rep 16(6):56. https://doi.org/10.1007/s11910-016-0659-0
Citerio G, Oddo M, Taccone F (2015) Recommendations for the use of multimodal monitoring in the neurointensive care unit. Curr Opin Crit Care 21:113–119
Smith M (2018) Multimodality neuromonitoring in adult traumatic brain injury. Anesthesiology 128:401–415. https://doi.org/10.1097/ALN.0000000000001885
Dias C, Silva MJ, Pereira E, Monteiro E, Maia I, Barbosa S, Silva S, Honrado T, Cerejo A, Aries M, Smielewski P, Paiva JA, Czosnyka M (2015) Optimal cerebral perfusion pressure management at bedside: a single-center pilot study. Neurocrit Care 23(1):92–102. https://doi.org/10.1007/s12028-014-0103-8
Aries M, Czosnyka M, Budohoski P, Steiner L, Lavinio A, Kolias A, Hutchinson P, Brady K, Menon D, Pickard J, Smielewski P (2012) Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med 40(8):2456–2463. https://doi.org/10.1097/CCM.0b013e3182514eb6
Rasulo FA, Girardini A, Lavinio A et al (2012) Are optimal cerebral perfusion pressure and cerebrovascular autoregulation related to long-term outcome in patients with aneurysmal subarachnoid hemorrhage? J Neurosurg Anesthesiol 24(1):3–8
Stein SC, Georgoff P, Meghan S, Mirza KL, El Falaky OM (2010) Relationship of aggressive monitoring and treatment to improved outcomes in severe traumatic brain injury. J Neurosurg 112(5):1105–1112
Czosnyka M, Balestreri M, Steiner L et al (2005) Age, intracranial pressure, autoregulation, and outcome after brain trauma. J Neurosurg 102(3):450–454
Jennett B (1975) Assessment of outcome after severe brain damage: a practical scale. Lancet 305:480–484
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6(1):1–9
Drake C (1988) Report of the World Federation of Neurological Surgeons Committee on a universal subarachnoid hemorrhage grading scale. J Neurosurg 68(6):985–986
Lagares A, Gómez PA, Lobato RD, Alén JF, Alday R, Campollo J (2001) Prognostic factors on hospital admission after spontaneous subarachnoid haemorrhage. Acta Neurochir 143:665–672
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Ethics declarations
The authors have no conflicts of interest.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Monteiro, E. et al. (2021). Brain Multimodal Monitoring in Severe Acute Brain Injury: Is It Relevant to Patient Outcome and Mortality?. In: Depreitere, B., Meyfroidt, G., Güiza, F. (eds) Intracranial Pressure and Neuromonitoring XVII. Acta Neurochirurgica Supplement, vol 131. Springer, Cham. https://doi.org/10.1007/978-3-030-59436-7_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-59436-7_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-59435-0
Online ISBN: 978-3-030-59436-7
eBook Packages: MedicineMedicine (R0)