Abstract
Objective: This study aimed to examine whether changes in intracranial pressure (ICP) waveform morphologies can be used as a biomarker for early detection of ventriculitis.
Methods: Consecutive patients (N = 1653) were prospectively enrolled in a hemorrhage outcomes study from 2006 to 2018. Of these, 435 patients (26%) required external ventricular drains (EVDs) and 76 (17.5% of those with EVDs) had ventriculitis treated with antibiotics. Nineteen patients (25% of those with ventriculitis) showed culture-positive cerebrospinal fluid (CSF) and were included in the present analysis. CSF was routinely cultured three times per week and additionally if infection was suspected. EVDs were left open for drainage, with ICP assessed hourly by clamping. Using wavelet analysis, we extracted uninterrupted segments of ICP waveforms. We extracted dominant pulses from continuous high-resolution data, using morphological clustering analysis of intracranial pressure (MOCAIP). Then we applied k-means clustering, using the dynamic time warping distance to obtain morphologically similar groupings. Finally, metaclusters and further-split clusters (when equipoise existed) were categorized for broad comparison by clinician consensus.
Results: We extracted 275,911 dominant pulses from 459.9 h of EVD data. Of these, 112,898 pulses (40.9%) occurred before culture positivity, 41,300 pulses (15.0%) occurred during culture positivity, and 121,713 pulses (44.1%) occurred after it. K-means identified 20 clusters, which were further grouped into metaclusters: tri−/biphasic, single-peak, and artifactual waveforms. Prior to ventriculitis, 61.8% of dominant pulses were tri−/biphasic; this percentage reduced to 22.6% during ventriculitis and 28.4% after it (p < 0.0001). One day before the first positive cultures were collected, the distribution of metaclusters changed to include more single-peak and artifactual ICP waveforms (p < 0.0001).
Conclusion: The distribution of ICP waveform morphology changes significantly prior to clinical diagnosis of ventriculitis and may be a potential biomarker.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
External ventricular drains (EVDs) are widely used to control hydrocephalus, with roughly 37,000 patients a year receiving EVDs in the USA alone, generating in-hospital charges of $151,672 per patient, or US$5.6 billion a year [1]. EVDs are frequently complicated by ventriculitis, an infection of the ventricular system. Penetration into the central nervous system (CNS) with ventriculostomy can introduce infectious species into the cerebrospinal fluid (CSF), which acts as a reservoir for microbiota. The infection can lead to inflammation of the arachnoid villi, decreasing CSF outflow and instigating hydrocephalus [2]. Up to 22% of patients with EVDs develop ventriculitis [3]. The Centers for Disease Control guidelines define ventriculitis by combinations of clinical features such as fever, headache, or meningeal signs (neck stiffness, photophobia), laboratory test features such as elevations in the CSF white blood cell count and protein level, a decreased CSF glucose level, and a CSF culture that is positive for an organism [4]. A negative CSF Gram stain does not exclude the presence of ventriculitis [5, 6]. Patients with certain conditions such as subarachnoid hemorrhage (SAH) or intraventricular hemorrhage (IVH) are at increased risk of ventriculitis [7].
Delays in implementing proper antimicrobial therapy for infections are associated with increases in mortality [7], so neurocritical care units commonly institute periodic or responsive (to fever) drawing of CSF from EVDs to send away for culturing and other laboratory studies [8]. The longer an EVD remains indwelling, the higher the risk of ventriculitis, with the rate of infection ranging from 6.3 to 10.4 infections per 1000 EVD-days [9]. The frequency of drawing fluid samples from the EVD is, in itself, another risk factor. One study showed a 5% decrease in the rate of ventriculitis in patients sampled every 3 days versus daily [10], and another study found a significant increase in the risk of infection with both daily and alternate-day sampling regimens in comparison with sampling 1–2 times per week [11]. Imaging and laboratory test characteristics can also identify ventriculitis. Magnetic resonance imaging has shown promise in small studies, where intraventricular debris and pus on fluid attenuation inversion recovery (FLAIR) imaging and choroid plexitis on T-1 imaging were sensitive for ventriculitis [12]. Serum procalcitonin, a marker of bacterial pneumonia, has shown utility in distinguishing bacterial meningitis from viral meningitis, and early high serum procalcitonin concentrations were predictive of bacterial ventriculitis in a study of 36 patients with EVDs [13]. However, neither serum nor CSF procalcitonin have proven able to differentiate between fevers of infectious or noninfectious etiology, making procalcitonin a poor noninvasive predictor [14, 15]. One study showed a significant increase in CSF red blood cell counts in culture-positive ventriculitis, though this was shown to be neither sensitive nor specific and is confounded by concurrent hemorrhage [16]. Furthermore, any detection system that relies on assaying CSF still requires periodic draws, thus negating the hypothetical advantages of another method of detection.
We made clinical observations of blunted single-peak waveforms in patients with ventriculitis. Understanding that ICP waveforms should reflect the changing poroelastic property of the parenchyma, we hypothesized that the temporal dynamics of intracranial pressure waveforms could reveal a pathological change in compliance in patients developing ventriculitis.
Materials and Methods
Study Population and Data Collection
We studied consecutive patients with EVDs who were prospectively enrolled in a hemorrhage outcomes study from 2006 to 2018. The study was approved by the Columbia University Medical Center institutional review board. In each case, written informed consent was obtained from the patient or a surrogate.
Physiological data for the duration of the intensive care unit stay were acquired using a high-resolution acquisition system (BedMasterEX, Excel Medical Electronics, Jupiter, FL, USA) from General Electric Solar 8000i monitors (Port Washington, NY, USA; 2006–2013) at 240 Hz (waveforms) or Philips Intellivue MP70/MX800 monitors (Amsterdam, the Netherlands; 2013–present) at 125 Hz (waveforms). We converted the proprietary file format (STP) defined by BedMasterEx into the Hierarchical Data Format, version 5 (HDF5; 1997–2018; http://www.hdfgroup.org/HDF5/), which is specifically designed to store and efficiently organize large quantities of data.
Outcome Definition
Given the uncertainty around the clinical diagnosis of definite ventriculitis, we limited the outcome in our cohort to culture-positive ventriculitis [4, 17].
Data Analysis
Using wavelet analysis [18], we extracted uninterrupted segments of ICP waveforms. We extracted dominant pulses from continuous high-resolution data, using a validated technique, morphological clustering analysis of intracranial pressure (MOCAIP) [19]. Then we applied hierarchical k-means clustering, using the dynamic time warping (DTW) distance to obtain morphologically similar groupings [20]. DTW is an algorithm for measuring similarity between two temporal sequences, which may vary in speed. Metaclusters were categorized for broad comparison by clinician consensus and labeled as compliant (three peaks), noncompliant (one peak), and artifactual groups. Finally, we compared the distribution of these metaclusters before, during, and after the diagnosis of definite ventriculitis.
Statistical Analysis
We used a chi-squared test of independence to compare the distribution of the metaclusters before, during, and after ventriculitis, and we used change point analysis [21] to identify significant changes in the distribution leading to ventriculitis.
Results
Consecutive patients (N = 1653) were prospectively enrolled in a hemorrhage outcomes study from 2006 to 2018. Of these, 435 patients (26%) required EVDs, and 76 (17.5% of those with EVDs) had ventriculitis. Nineteen patients (25% of those with ventriculitis) showed culture-positive CSF and were included in the present analysis. Of these, nine patients had enough physiological data recorded for analysis.
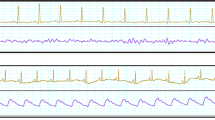
We extracted 275,911 dominant pulses from 459.9 h of EVD data. Of these, 112,898 pulses (40.9%) occurred before culture positivity, 41,300 pulses (15.0%) occurred during culture positivity, and 121,713 pulses (44.1%) occurred after it. K-means identified 20 clusters, which were further grouped into metaclusters: tri−/biphasic, single-peak, and artifactual waveforms. Prior to ventriculitis, 61.8% of dominant pulses were tri−/biphasic; this percentage reduced to 22.6% during ventriculitis and 28.4% after it (p < 0.0001) (Fig. 1a, b).
Changes in the distribution of intracranial pressure tri−/biphasic (green), single-peak (yellow), and artifactual (red) waveforms. (a) Cumulative changes before, during, and after ventriculitis; an asterisk denotes a significant change (p < 0.0001). (b) The top 20 metaclusters; the inset in each graph indicates the dynamic time warping distance to the centroid of each waveform. (c) Change point analysis (in days) indicating that there is a change in the distribution of the waveforms at least 1 day before the diagnosis of ventriculitis. (d) Changes in the distribution of clusters over time (in days) before and after ventriculitis
Change point analysis [21] with 99% confidence showed a significant change in the distribution of the metaclusters 1 day before the cultures that revealed ventriculitis were sent away for analysis (Fig. 1c, d).
Discussion
There is a compelling need for identification of ventriculitis that does not rely on CSF sampling. We analyzed ICP waveforms before, during, and after adjudication of ventriculitis. We found significant differences in the distribution of the morphologies of the ICP waveforms. Using change point analysis, we further identified that there was a significant difference in the distribution of the cluster 1 day before the cultures that revealed ventriculitis were sent away for analysis. The distribution of ICP waveform morphology changes significantly prior to the clinical diagnosis of ventriculitis and may be a potential biomarker.
This study had the following limitations: (1) the study cohort included only ventriculitis patients, and a comparison with matched controls is warranted in order to create any predictive models; and (2) to generalize this finding across different institutions, further validation using external data is required. In our future work, we plan to address these challenges by comparing our ventriculitis cohort with a matched control group, in order to develop predictive models using ICP waveform dynamics as a biomarker for ventriculitis. Additionally, an external validation study is under way.
References
Rosenbaum BP, Vadera S, Kelly ML, Kshettry VR, Weil RJ (2014) Ventriculostomy: frequency, length of stay and in-hospital mortality in the United States of America, 1988–2010. J Clin Neurosci 21(4):623–632. https://doi.org/10.1016/j.jocn.2013.09.001
Salmon JH (1972) Ventriculitis complicating meningitis. Am J Dis Child 124(1):35–40
Lewis A, Wahlster S, Karinja S, Czeisler BM, Kimberly WT, Lord AS (2016) Ventriculostomy-related infections: the performance of different definitions for diagnosing infection. Br J Neurosurg 30(1):49–56
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting [published correction appears in Am J Infect Control 2008;36(9):655]. Am J Infect Control 36(5):309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Kim HI, Kim SW, Park GY et al (2012) The causes and treatment outcomes of 91 patients with adult nosocomial meningitis. Korean J Intern Med 27(2):171–179
Tunkel AR, Hasbun R, Bhimraj A et al (2017) 2017 Infectious Diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis 64(6):e34–e65
Aronin SI, Peduzzi P, Quagliarello VJ (1998) Community-acquired bacterial meningitis: risk stratification for adverse clinical outcome and effect of antibiotic timing. Ann Intern Med 129(11):862–869
Halpern C, Grady M (2015) Neurosurgury. In: Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Matthews JB, Pollock RE (eds) Schwartz’s principles of surgery, 10th edn. McGraw-Hill, New York, pp 1733–1734
Hagel S, Bruns T, Pletz M, Engel C, Kalff R, Ewald C (2014) External ventricular drain infections: risk factors and outcome. Interdiscip Perspect Infect Dis 2014:708531. https://doi.org/10.1155/2014/708531
Williams TA, Leslie GD, Dobb GJ, Roberts B, van Heerden PV (2011) Decrease in proven ventriculitis by reducing the frequency of cerebrospinal fluid sampling from extraventricular drains. J Neurosurg 115(5):1040–1046
Jamjoom AA, Joannides AJ, Poon MT-C et al (2018) Prospective, multicentre study of external ventricular drainage–related infections in the UK and Ireland. J Neurol Neurosurg Psychiatry 89(2):120–126
Fujikawa A, Tsuchiya K, Honya K, Nitatori T (2006) Comparison of MRI sequences to detect ventriculitis. AJR Am J Roentgenol 187(4):1048–1053. https://doi.org/10.2214/AJR.04.1923
Omar AS, ElShawarby A, Singh R (2015) Early monitoring of ventriculostomy-related infections with procalcitonin in patients with ventricular drains. J Clin Monit Comput 29(6):759–765. https://doi.org/10.1007/s10877-015-9663-1
Halvorson K, Shah S, Fehnel C et al (2017) Procalcitonin is a poor predictor of non-infectious fever in the neurocritical care unit. Neurocrit Care 27(2):237–241. https://doi.org/10.1007/s12028-016-0337-8
Martinez R, Gaul C, Buchfelder M, Erbguth F, Tschaikowsky K (2002) Serum procalcitonin monitoring for differential diagnosis of ventriculitis in adult intensive care patients. Intensive Care Med 28(2):208–210. https://doi.org/10.1007/s00134-001-1176-3
Hoogmoed J, van de Beek D, Coert BA, Horn J, Vandertop WP, Verbaan D (2017) Clinical and laboratory characteristics for the diagnosis of bacterial ventriculitis after aneurysmal subarachnoid hemorrhage. Neurocrit Care 26(3):362–370
Walti LN, Conen A, Coward J, Jost GF, Trampuz A (2013) Characteristics of infections associated with external ventricular drains of cerebrospinal fluid. J Inf Secur 66(5):424–431
Strang G, Nguyen T (1996) Wavelets and filter banks, 2nd edn. Wellesley-Cambridge, Cambridge
Hu X, Xu P, Scalzo F, Vespa P, Bergsneider M (2009) Morphological clustering and analysis of continuous intracranial pressure. IEEE Trans Biomed Eng 56(3):696–705
Niennattrakul V, Ratanamahatana CA (2007) On clustering multimedia time series data using k-means and dynamic time warping. Presented at the 2007 International Conference on Multimedia and Ubiquitous Engineering (MUE’07), Seoul, pp 26–28
Killick R, Eckley I, Haynes K (2019) Changepoint: an R package for changepoint analysis. R package version 1.1.5. http://CRAN.R-project.org/package=changepoint.
Acknowledgments
Soojin Park is supported by National Institutes of Health grant number K01 ES026833.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
The authors have no conflicts of interest to declare.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Megjhani, M. et al. (2021). Use of Clustering to Investigate Changes in Intracranial Pressure Waveform Morphology in Patients with Ventriculitis. In: Depreitere, B., Meyfroidt, G., Güiza, F. (eds) Intracranial Pressure and Neuromonitoring XVII. Acta Neurochirurgica Supplement, vol 131. Springer, Cham. https://doi.org/10.1007/978-3-030-59436-7_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-59436-7_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-59435-0
Online ISBN: 978-3-030-59436-7
eBook Packages: MedicineMedicine (R0)