Abstract
Different surgical techniques for the treatment of achalasia exist, including laparoscopic Heller myotomy. Laproscopic Heller myotomy is the most common approach; it has better short-term outcomes and similar long-term outcomes when compared to open myotomies. Typical clinical symptoms for achalasia include dysphagia combined with weight loss, regurgitation, recurrent bronchopulmonary infection, chest pain, hiccups, and coughing. We perform a laparoscopic Heller myotomy with fundoplication entering through the umbilicus, upper-left quadrant, and upper midline position. We first open the gastro-hepatic ligament and gastrophrenic membrane while preserving the nervus vagus. To complete the myotomy, we dissect a 10 cm longitudinal section of the muscular layer along the proximal and distal plane centralized at the esophagogastric junction. It is crucial at this point to avoid mucosal injury. After ligating the left and right margins of the esophageal muscle layer to the crus, we apply a Thal—fundoplication. We complete the operation using an endoscope for an air test control. Postoperatively we transfer the patient to a peripheral ward with a nasogastric tube which drains by gravity. The patient is allowed clear liquids after 24 h and a soft diet after 2 days if an esophagogram is clear (the emptying of the esophagus and no leakage). We then discharge the patient (2–4 days) and permit a full diet and normal activity after 4 weeks.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Evidence on Outcome for Laparoscopic Heller Myotomy
Different surgical approaches for achalasia are available: open myotomy, thoracoscopic myotomy, laparoscopic myotomy plus fundoplication, endoscopic peroral myotomy [1] and more recently, robotic myotomy. Heller myotomy is most commonly performed using a laparoscopic approach, as it has better short-term outcomes and similar long-term outcomes compared to the open procedure [2, 3]. In a comparative study to the thoracoscopic approach, Pattie et al. found that the laparoscopic technique resulted in a shorter hospital stay, a better result in terms of resolution of dysphagia and reflux, as well as better postoperative results in terms of reflux control [4]. In contrast, the thoracoscopic and endoscopic peroral myotomies do not allow an antireflux prophylaxis [5]. Robotic myotomy seems promising, with potentially less esophagal perforation and less conversion to open surgery. However, long term results are not yet available and in smaller children, instrument size may be a limiting factor [6]. Therefore, once achalasia is diagnosed in a child, we suggest to try pneumatic dilation in three consecutive settings. If dilation is not successful it is advisable to apply a laparoscopic heller myotomy, particularly in patients of young age and low surgical risk factors.
2 Preoperative Workup and Considerations
The main clinical symptoms of achalasia are dysphagia combined with weight loss, regurgitation, recurrent bronchopulmonary infection, chest pain, hiccups and cough [7]. In Patients who show clinical symptoms of achalasia, a diagnostic algorithm of endoscopy, upper gastrointestinal contrast study, and high resolution manometry is warranted to confirm the diagnosis. Three stages of achalasia are described in literature. A Hypermotile achalasia = Vigorous Achalasie (Type 1), B—Hypomotile achalasia (Type 2), C—Amotile achalasia (Type 3). It is important to take into consideration that the extent of the esophagographic findings do not necessarily correlate with symptoms.
3 Anesthetic Considerations
Heller myotomy and additional hemifundoplication is typically preformed under general endotracheal anaesthesia. A naso- or orogastric-tube is placed to decompress the stomach, or alternatively, simultaneous intraoperative esophagogastroscopy can be performed. Periooperativly, a single antibiotic dose is given for prophylaxis. Although intraopertive bleeding is rare, having blood and two peripheral intravenous lines available is advisable.
4 Operative Technique Equipment
-
3–5 mm 30° Laparoscope
-
3–5 mm trocars (the authors prefer to place a single-port trocar in the umbilicus)
-
3 mm trocars as needed
-
3–5 mm instruments and trocars
-
3–5 mm Maryland dissector
-
3–5 mm atraumatic grasper
-
3–5 mm needle holder
-
3–5 mm Metzenbaum scissors
-
3–5 mm hook monopolar cautery (grounding pad)
-
3–5 mm Laparoscopic liver retractor
-
3–5 mm monopolar hook cautery
-
6–10 mm endoscope
-
2–0 silk sutures on a skin needle
5 Positioning
The patient is positioned supine with arms tucked to the sides and abducted lower extremities. The surgeon stands at the foot end of the bed, the monitor is placed at the head of the patient in-line with the surgeon and patient. The assistant is on the right side and the scrub nurse on the left of the patient (Fig. 4.1). The abdomen is prepped and draped from the nipples to the symphysis.
6 Trocar Placement
The umbilical trocar (in our case a single-port trocar) is placed in the umbilicus via a longitudinal incision. A 3 mm 30° optic is introduced through the umbilical port. After insufflating the capnoperitoneum and under vision, one 3 mm trocar is placed in the epigastric area and one 3 mm trocar is placed in the left upper abdominal quadrant (Fig. 4.2).
7 Operative Milestones
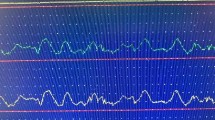
After placing the trocars, the liver is suspended upwards towards the abdominal wall using a laparoscopic liver retractor (Video 4.1). We position a concomitant endoscope oropharyngeally at the esophagogastric junction as a visual reference, since in our opinion, the transillumination helps with identification of the muscle fibers during the dissection (Milestone 4.1).

Laparoscopic liver retractor and concomitant endoscope (Video 4.1 Laparoscopic Heller Myotomy). (▸ https://doi.org/10.1007/000-2tx)
After grasping the stomach and retracting it to the superior left side of the patient the gastro-hepatic ligament and gastrophrenic membrane are opened using a monopolar hook cautery to gain access to the esophagus (Milestone 4.2). The vagal nerve as well as the vessels are identified and carefully mobilized from the esophagus using a Maryland dissector and preserved throughout the operation (Milestone 4.3). A blunt division of the longitudinal muscular fibre is carried out from distal (stomach) to proximal (esophagus) using a monopolar hook cautery. We generally carry out the dissection approximately 5 cm distal and 5 cm proximal to the esophagogastric junction through the seromuscular muscular layers, creating a generous, adequate myotomy and thereby minimizing the chance of recurrence (Milestone 4.4).
The muscular margins are then sutured to the right and left crus using simple 2-0 silk sutures, retracting the myotomy open. Subsequently, a (180° anterior) Thal—fundoplication is created by folding the fundus over the myotomy and attaching it with 2-0 silk interrupted sutures to the right crus, the anterior hiatus and the left crus. Finally, the completed Heller myotomy and fundoplication is checked using the endoscope and gas insufflation (Milestone 4.5).
8 Postoperative Care
The patient is transferred to a peripheral ward and a nasogastric tube is left and drained to gravity. The patient is allowed clear liquids after 24 h. Two days after surgery, an esophagogram is preformed to evaluate the emptying of the esophagus and to rule out any leakage. If the scan does not show complications, the patient is given a soft diet and discharged from hospital on full enteral nutrition. We tend to prescribe a no-chunk diet initially and allow normal eating and normal activitiy after 4 weeks. Clinical follow up is performed at yearly intervals to make sure the patient does not suffer recurrence.
9 Pearls/Tips & Tricks
-
1.
Using a single-port trocar allows the surgeon to place both the optic and the liver retractor through the navel and limit additional trocar sites.
-
2.
We create a long myotomy, at least 5 cm proximal and 5 cm distal of the esophagogastral junction, using the horizontal muscle fibers of the antrum as the reference point that the gastroenteric tract is reached, making sure not to leave any remnant muscle fibers and thereby to avoid a recurrence.
-
3.
Intraoperative endoscopy helps to delineate the muscle fibers by transillumination. At the same time, perforation can be ruled out from endoluminally and by insufflating gas.
10 Pitfalls & Ways to Avoid
-
1.
Mucosal injury and leakage is one of the most serious complications during myotomy especially if monopolar energy is used for the dissection of the muscular layer. The monopolar energy current should be dosed carefully to prevent thermal injury to the mucosa. Therefore, identification and dissection of the muscluar tissue is important. If a leak occurs it can be repaired with e.g. Monocryl 5.0.
-
2.
The vagus nerve runs along the operative field. It is important to identify and preserve it during the procedure.
References
Caldaro T, Familiari P, et al. Treatment of esophageal achalasia in children: today and tomorrow. J Pediatr Surg. 2015;50:726–30.
Allaix ME, Patti MG. Heller myotomy for achalasia. From the open to the laparoscopic approach. World J Surg. 2015;39:1603–7.
Askegard-Giesmann JR, Fau GJ, et al. Minimally invasive Heller’s myotomy in children: safe and effective. J Pediatr Surg. 2009;44:909–11.
Hunter JG, Fau TT, Branum GD, et al. Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg. 1997;225:655–65.
Rothenberg SS, Da Fau P, et al. Evaluation of minimally invasive approaches to achalasia in children. J Pediatr Surg. 2001;36:808–10.
Ballouhey Q, Dib N, Binet A, et al. How robotic-assisted surgery can decrease the risk of mucosal tear during Heller myotomy procedure? J Robotic Surg. 2017;11:255–8.
Kotilea K, Mahler T, Bontems P, et al. Management of esophageal motility disorders in children: a review. Acta Gastroent Belg. 2018;81:295–304.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Waldron, L.S., Muensterer, O.J. (2021). Laparoscopic Heller Myotomy. In: Lacher, M., Muensterer, O.J. (eds) Video Atlas of Pediatric Endosurgery (VAPE). Springer, Cham. https://doi.org/10.1007/978-3-030-58043-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-58043-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-58042-1
Online ISBN: 978-3-030-58043-8
eBook Packages: MedicineMedicine (R0)