Abstract
Large granular lymphocyte (LGL) disorders account for several conditions characterized by the proliferation of clonal LGLs with cytotoxic activity. According to the LGL immunophenotype, most cases represent expansions of TCRα/β+ LGL, displaying a CD8+ CD4− or less frequently a CD4+ CD8−/+dim phenotype with variable expression of cytotoxic NK cell antigens, including CD57, CD16, and CD56. Clonal expansions of TCRγ/δ+ LGL are also described. Proliferations of CD3− CD16+ NK cells with a restricted pattern of NK receptors usually comprise 15% of the total. Morphologic, immunophenotypic and molecular analyses are mandatory for a correct diagnosis of disease. The JAK/STAT pathway is typically involved in sustaining LGL proliferation and recently the presence of STAT3 and STAT5B somatic mutations has been reported as a hallmark of the disease and included in the recent 2017 WHO classification. Understanding how the leukemic LGL clone survives is central to reconcile the molecular mechanisms to the clinical behavior of disease, in order to find new clues to overcome the still unacceptable limit of the conventional immunosuppressive treatments.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction


The 2017 WHO classification reports large granular lymphocyte (LGL) leukemia in the category of cytotoxic T and NK cell lymphoma and leukemia. LGL leukemia is a lymphoproliferative disorder, defined by the presence of a high percentage of circulating LGLs in peripheral blood. The lymphocytosis is chronic and is sustained by clonal mature T or NK cells, thus configuring T-LGL leukemia (T-LGLL) or chronic lymphoproliferative disease of NK cells (CLPD-NK), respectively. T-LGLL is the most frequent form, accounting for about 85% of cases, whereas NK form is less represented with 10% of cases. In this scenario, also rare cases (incidence 5%) of aggressive LGL disorders of T or NK lineage are included, with very poor prognosis. Among these latter, the T-related type is described in the literature, but it is not yet included in the WHO classification that actually recognizes only the NK form, referred to as aggressive NK cell lymphoma (ANKL), more frequently found in oriental populations and usually associated with Epstein-Barr virus (EBV) infection. The etiopathogenesis of LGL leukemia has not been established, but it is hypothesized that a viral or autologous antigen triggers the initial lymphocytosis whose survival over the time is then maintained by the activation of many cell pathways. Among these, JAK/STAT3 axis is claimed as the principal signal involved in cell imbalance toward cell survival, the signal transducer and activator of transcription 3 (STAT3) activation being the hallmark of LGL disease. Moreover, in about 40% of patients, mutations on STAT3 have been recognized that further sustain the activation of this pathway.
T and NK cell disorders share several biological and clinical features. Both entities are characterized by STAT3 activation, and both types of patients show clinical manifestations due to cytopenia. Furthermore, the treatment of T-LGLL and CLPD-NK patients is very similar, entailing an immunosuppressive regimen or careful observation of chronic lymphocytosis.
2 LGL Leukemia: Clinical Aspects
2.1 Leukemic LGL Cytology and Immunophenotype
On blood films, the LGL nucleus is typically round with condensed, mature chromatin; the cytoplasm is pale and abundant with randomly distributed azurophilic granules containing perforins and granzyme conferring its cell lytic ability [1] (Fig. 15.1). Leukemic LGLs do not show morphologic difference with LGLs in healthy individuals.
The immunophenotype is central to identify LGLs among lymphocytes. The presence/absence of CD3 expression on cell surface distinguishes LGL belonging to T or NK lineage, respectively.
CD3+ LGL leukemia cells usually express the TCR αβ+, CD4−, CD8+ phenotype, and the disease may be also referred to as CD8+ T-LGLL. Less frequently, in 10–15% of cases, the disorder is sustained by TCR αβ+, CD4+, CD8+/− LGLs, often expressing TCR Vβ13.1 [2], defining the CD4+ T-LGLL. T-LGLs are also typically equipped with CD16, CD56, and CD57. CD57 is almost always present, and it is considered a specific marker of LGL, whereas CD16 and CD56 may be present or absent in different combinations. The rare cases with T-LGLs CD57 negative are usually characterized by the expression of CD16. In T-LGLL, CD5 and CD7 are weakly expressed, and LGLs usually display a cytotoxic phenotype corresponding to that of a fully differentiated mature cytotoxic T lymphocyte (CD45RA+, CD27−, CD28−, CD62L−, CCR7−). Leukemic LGLs are constitutively equipped with IL-2Rβ (CD122), but not IL-2Rα (CD25), and can variably express NK receptors as CD94/NKG2 (A or C) and killer immunoglobulin-like receptors (KIRs) [3].
Beyond the expansions of T cells bearing the TCR αβ+, there is a minority of cases derived from TCRγδ+ cells, presenting a Vγ9+/Vδ2+ or, less frequently, a Vγ9−/Vδ1+ phenotypic profile with TCRγ monoclonal restriction [4].
Some cases of a rare aggressive form of T-LGLL were reported, and these cases are usually equipped with a phenotype CD3+, CD8+, and CD56+ but devoid of CD16 and CD57 expression [5].
CLPD-NK are characterized by the lack of TCR and the CD16+, CD56+, CD45RA+, CD122+, CD25− phenotype. CD57 antigen is usually weakly detectable. CD56 antigen is normally expressed by LGL, although some negative cases are reported. CD94 antigen is found at high density on patients’ NK cells; this antigen is usually associated with the inhibitory subunit NKG2A, although in some cases the association CD94/NKG2C has been reported [6]. Patients’ NK cells characteristically express functional β and γ chains of IL-2/IL-15 receptor, which are strictly related to the role of these cytokines in the pathogenesis of disease [7]. Expression of NK receptors, mostly represented by KIR, is altered in patients with CLPD-NK. A restricted pattern of KIR expression is currently used in these patients to define the clonal nature of NK cell proliferation [6, 8, 9].
The aggressive and rare ANKL is not provided by an immunophenotype specifically distinguishable from CLPD-NK, and clinical evaluation is necessary to make the diagnosis. The presence of large nucleoli in NK cells strongly supports the diagnosis of ANKL, associated with age <40 years, systemic symptoms, lymph node swelling, and hepatosplenomegaly [10, 11].
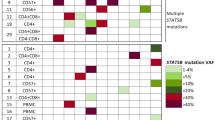
Some representative cytometer panels of the most frequent immunophenotype for each LGLL subtype are reported in Fig. 15.2.
2.2 Diagnosis
Historically, the evidence of a lymphocytosis greater than 2 x 109 LGL/L, lasting for more than 6 months and clonal, was requested for the diagnosis of disease [1], considering that normally circulating LGL count is 0.25 × 109/L. However, the demonstration of clonal restriction of LGL proliferation can often be provided even in the presence of less than 2 x 109 LGL/L, particularly in symptomatic disease. For this reason, the threshold actually accepted for diagnosis is 0.5 x 109 LGL/L [12]. Additionally, the lymphocytosis must be characterized by immunophenotyping and molecular analyses.
As detailed in the previous paragraph, a proper definition of LGL immunophenotype is mandatory to recognize LGL lymphoproliferation and to define LGL leukemia subtypes: Tαβ LGLL including CD8+ T-LGLL, CD4+ T-LGLL, and aggressive T-LGLL; Tγδ LGLL; and CLPD-NK.
The molecular analysis is critical to distinguish reactive LGL proliferation from true LGL leukemic clonal expansion. Polyclonal expansions of LGLs are usually transient and due to a viral infection, such as EBV or cytomegalovirus (CMV), neoplasms, or autoimmune diseases [13,14,15,16]. Sometimes, this condition may develop after splenectomy. In contrast, clonal LGL proliferations are stably maintained for time, whether or not the patients are symptomatic.
The T-LGL leukemia can be tested for clonality by TCR rearrangement study. TCR gamma polymerase chain reaction analysis is a routine and easy technique to assess T-LGL clonality in both Tαβ and Tγδ LGLL. Showing the preferential use of one or two TCR-Vβ segments, flow cytometry analysis with monoclonal antibodies against the various Vβ regions of the TCR allows to suggest, and then used as a surrogate marker, the clonality of the LGLs [17]. The current Vβ monoclonal antibody panel covers 75% of the Vβ spectrum, with a high correlation between Vβ flow cytometry and TCRγ-polymerase chain reaction results. No prevalence of any of Vβ was reported in T-LGLL but Vβ13.1 in CD4+ T-LGLL [2]. These techniques should be applied to all suspected cases and are useful in those patients in whom the absolute LGL count is not significantly increased. To these routinely used investigations, deep sequencing (NGS) of TCR has recently emerged to be a useful tool to demonstrate restricted diversity of TCR repertoire [18], not only supplying information about the clonal nature of LGL expansion but also providing the number and the entity of clones included in LGL increase and the identification of the CDR3 sequence. NGS analysis has been proven to be also useful to monitor therapy response and minimal residual disease.
The clonality of CLPD-NK is more difficult to assess, NK-LGLs being not equipped with the TCR. In this case, chromosomal abnormalities or the restriction fragment polymorphism of X-linked gene analysis can provide the proof of clonality. A KIR-restricted expression pattern, demonstrated by flow cytometry analysis, has been accepted as a surrogate marker of monoclonal expansion [8].
At the diagnosis, when the criteria are difficult to be satisfied, histologic bone marrow (BM) immunochemistry analysis is requested. LGLs in BM appear as individual cells or small clusters localized in sinusoids. Since the amount of infiltrating cells is usually low, BM involvement by leukemic LGLs is often difficult to identify, even when LGL expansion is apparent in peripheral blood [19, 20].
2.3 Clinical Features
LGL leukemia is an extremely rare disease representing 2–5% of chronic lymphoproliferative disorders in North America and Europe and 5–6% in Asia. Two registries, one Dutch and one American, report the incidence of LGL leukemia as 0.72 and 0.2 cases per one million of individuals per year, respectively [21, 22]. T-LGL leukemia patients have reduced survival compared with general population, with a median overall survival of 9 years [12].
The disease usually affects old people (mean 60 years), men or women with the same proportion. The disease runs asymptomatic in nearly 40% of cases, with lymphocytosis representing the only observed hematological abnormality [23, 24]. The definition of T-cell clonopathy of unknown significance (TCUS) has also been suggested to designate these asymptomatic patients [25]. Disease may run asymptomatic for many years; however, during the course of disease in 60% of cases, therapy is needed, mostly for cytopenia-related manifestations. Symptomatic patients show clinical complications more frequently due to neutropenia, as fever caused by infections or mouth lesions. Recurrent infections are reported in 15–39% of cases [26]. Neutropenia is defined as an absolute neutrophil count (ANC) less than 1.5 × 109/L and severe neutropenia with ANC <0.5 × 109/L. However, some patients with severe and persistent neutropenia can be also devoid of infections for a long period of time; in these cases, therapy can be delayed. Weakness due to anemia represents another relevant finding, with 10–30% of cases being transfusion-dependent. B-related symptoms (fever, night sweats, weight loss) are observed in nearly 25% of cases. Thrombocytopenia is generally moderate and is found in less than 25% of cases, whereas pure red cell aplasia (PRCA) occurs in 8–19% of the cases [27].
Frequently, patients may have other associated conditions; among these, rheumatoid arthritis (RA) is the most commonly reported comorbidity condition [12, 28], but several other connective tissue diseases, including systemic lupus erythematosus, vasculitis, and polymyositis, have been reported [29,30,31,32]. Hematological disorders are another well-represented group including monoclonal gammopathies, multiple myeloma, myelodysplastic syndromes, myelofibrosis, and Hodgkin’s and non-Hodgkin’s lymphomas [12, 28]. An association has been established between LGL disorders and pulmonary hypertension, with documented infiltration of the lung by LGLs, and inclusion body myositis has occasionally been reported [32]. From 20% up to a half of the patients have splenomegaly, around 20% of cases present skin lesions, and only a minority have hepatomegaly; lymphadenopathy is rare [33]. Diseases associated with LGL leukemia are listed in Table 15.1.
2.4 The Predicting Value of the Immunophenotype
Intriguingly, a correlation between immunophenotype and clinical and genetic features has been reported [34, 35], even if the nature of this relationship needs to be elucidated. In CD8+ T-LGLL, it has been demonstrated that CD16+/CD56− phenotype, with or without CD57, is strongly linked to patients characterized by neutropenia and the presence of STAT3 mutation [35]. The association between STAT3 mutation and symptomatic disease has been further reported in several papers [36,37,38]. The rare aggressive form of T-LGLL is characterized by proliferations of CD8+/CD56+/CD16−/CD57− LGLs, and patients are frequently mutated in STAT5b [39]. Interestingly, CD4+ T-LGLL patients are always CD8±/CD56+ and include patients carrying STAT5b mutations, but they never show to carry STAT3 mutations, and they are almost always characterized by an indolent clinical course [35, 40].
In 2017 WHO classification, STAT3 and STAT5b mutations are introduced to be considered for the identification of a subset of patients, STAT5b mutations being associated with a more aggressive disease. Anyway, this consideration will need to be updated with the discovery of STAT5b genetic lesions also in indolent CD4+ T-LGLL [40].
Similar to T-LGLL, discrete subtypes of CLPD-NK can be identified by flow analysis depending on the intensity of CD56 and CD16 expression and on CD57 presence or absence. Interestingly, patients characterized by CD56−/dim/CD16high/CD57− cytotoxic NK cell expansion include a unique phenotypic subgroup characterized by a more symptomatic disease and the presence of STAT3 mutation [41].
The dominant LGL immunophenotypes indicative for clinical presentation are schematically reported in Fig. 15.3.
2.5 Therapy
The percentage of patients requiring therapy during the natural history of the disease ranges from 30% to 70%, according to different series [12, 28]. Indications for treatment include severe and symptomatic neutropenia (associated with recurrent infections), transfusion-dependent anemia, or thrombocytopenia as far as progressive disease (i.e., appearance of organomegaly, B symptoms, and rapidly LGL raising counts). Correction of cytopenias with therapy may be achieved without eradication of the clone, which often persists even after treatment. Given that LGLs are activated cytotoxic lymphocytes, therapy is based on immunomodulatory drugs. Methotrexate (MTX, 10 mg/m2/weekly), low-dose cyclophosphamide (CTX, 50–100 mg/day), or cyclosporine A (CyA, 3–5 mg/kg/day) are commonly used [42, 43]. Corticosteroids may be useful as part of the initial treatment to accelerate response, and growth factors are often used as supportive care. Splenectomy may be considered as an adjuvant in patients with relevant splenomegaly and refractory cytopenias [44].
The first-line therapy relies on the use of single immunosuppressive oral agent, and up to now MTX or CTX have been considered as the best first-line choice. Moreover, MTX is reported to be more efficient for neutropenic and STAT3 Y640F mutated patients [42, 45].
Once patients with LGL leukemia start treatment, the regimen should be continued for a period of at least 4 months, and they should be closely observed through complete blood counts [43]. After this time point, a hematological complete response is considered achieved when blood counts reveal platelets >150 × 109/L, ANC >1.5 × 109/L, lymphocytes <4 × 109/L, and hemoglobin >12 g/dL. Complete molecular remission is reached when the T-cell clone is no longer detectable through PCR analysis [43]. Partial response is considered when overall blood counts improve, but the ANC has not achieved levels > 0.5 x 109 cells/L, still leaving the patient at potential risk for secondary infections. If an improvement is not achieved after 4 months of continued treatment, one of the alternative therapies described above must be taken into account. However, evidence is accumulating for continuing treatment once established for a longer period of time (usually 1 year), before changing therapy.
The overall response rate (ORR) ranges from 21% to 85%, with similar responses to each of the three drugs. The complete response (CR) rate is 21% for MTX, 33% for CTX, and 5% for CyA [43]. Unfortunately, when the clinical response occurs, patients frequently relapse, and new therapeutic strategies are needed.
Chemotherapeutic agents, such as gemcitabine, liposomal doxorubicin, and bendamustine, and the purine analogs, such as fludarabine, cladribine, and nelarabine, represent possible new agents to be considered for symptomatic LGL disorders [26, 28]. These molecules have been reported to be promising but only in few patients. The use of these agents should be considered for young patients as they allow the achievement of good remissions, including the reduction of bone marrow infiltration.
In some patients with refractory disease, stem cell therapy may be considered. In a series of 15 patients receiving auto- or allogeneic stem cell therapy for LGL leukemia, six patients remained disease-free after transplantation [46].
Monoclonal antibodies anti-CD52 (Campath-1H) and anti-CD122 have been incorporated in the therapeutic scenario for refractory patients. However, the use of anti-CD52 is restricted for its limited availability and infection risks, and the administration of anti-CD122 to patients did not show any response [26, 47]. Similarly, also a phase 2 study with the use of RAS farnesyltransferase inhibitor tipifarnib, according to the finding of a constitutively active signaling of Ras/MAPK/ERK pathway, has unfortunately led to unsatisfactory clinical response [48]. Rather, JAK3-specific inhibitor (tofacitinib citrate), tested in refractory patients, and the multicytokine inhibitor BNZ-1, tested in phase 1 trial, showed promising responses [49]. In addition, the proteasome inhibitor bortezomib has been reported to display anticancer activity against aggressive NK leukemia and extranodal NK/T cell lymphoma in vitro and in vivo, opening new therapeutic perspectives for LGL patients [50, 51]. Recent data support this approach [52].
Treatment of the rare forms of aggressive LGL leukemia includes polychemotherapy based on CHOP-like (CTX, doxorubicin, vincristine, and prednisone) or cytosine arabinoside-containing regimens [26], usually with unsatisfactory results.
3 LGL Leukemia: Molecular Aspects
3.1 Pathogenesis
The etiology of LGL leukemia remains still unknown, but some crucial cornerstones for disease development have been identified. It is supposed that no single, specific agent can finally trigger the LGL proliferation. In fact, the proliferation and accumulation of a transformed T or NK cell might represent the expression of a dysregulation of cytotoxic LGL homeostasis because of persistent antigenic drive in combination with immunogenetic factors favoring persistent cell expansions [53]. Moreover, the recognized role in LGL survival, played by some inflammatory cytokines and monocytes, dendritic cells, and mesenchymal stromal cells (MSC), supports the involvement of an inflammatory environment in the pathogenesis of the disease (Fig. 15.4).
3.2 The Inciting Event
Many reports strongly support the role of a chronic/persistent antigenic stimulation by auto-antigens or foreign infective antigens as the initial step. This would lead to the expansion of a fully differentiated effector cytotoxic LGL which is not cleared as a consequence of an impairment of apoptotic pathways [53, 54].
Supporting the involvement of auto-antigens, dysregulated autoimmune responses are frequently demonstrated in LGLL patients [15, 55], such as the presence of rheumatoid factors and antinuclear antibodies, rheumatic diseases being commonly associated with LGL leukemia (Table 15.1).
Several reports support a possible role of viral antigens. The pathogenic role of EBV or human T-cell leukemia viruses (HTVL) in some cases of LGL disorder has been reported [14, 16, 56]. Although no prototypic HTLV infection was demonstrated, the evidence that sera from a series of cases from Europe and USA react with the recombinant HTLV env protein p21E, specifically in BA21 epitope, indicates that exposure to a protein containing homology to BA21 may be important in the pathogenesis of this lymphoproliferative disorder [57]. Similarly, evidence has been provided that chronic stimulation of T cells by CMV leads to a persistent clonal expansion of CD4+/CD8−/+dim LGLs, with a predominance of TCR Vb13.1 usage in individuals with an HLADRB1*0701 haplotype [58]. The hypothesis has been formulated that a persistent CMV stimulation can trigger and maintain the LGL clone in patients with a genetic predisposition.
All these data show that not an exclusive and unique factor may be responsible for the initial event causing LGL expansion but rather that multiple factors, referred to auto/viral antigens, may be alternatively involved.
3.3 Bone Marrow Involvement
As stated before, LGLL patients usually present leukemic infiltration in bone marrow, where clonal LGLs cluster in small lymphoid aggregates or in microvascular structures [19]. LGLL patients’ bone marrow was also demonstrated to be fibrotic for the induction of high collagen (types I, III, and V) deposition by MSC, finally leading to an impaired hematopoietic stem cell proliferation. Together with LGL infiltration, fibrosis has been reported to correlate with the presence of cytopenia [59].
It has been proposed that bone marrow represents the setting in which the putative antigen presentation takes place. Furthermore, dendritic cells (DCs) have been suggested to represent the target of infection in these patients [60]. In fact, a co-localization of DCs and leukemic LGLs has been identified both in T-LGLL and in CLPD-NK. Moreover, bone marrow-derived DCs induced a strong proliferation of autologous purified LGLs from T-LGLL patients pointing that DCs pulsed with a specific antigen might be the putative-inciting agent responsible for T-LGL proliferation [60]. On the contrary, the clonal expansion of NK cells might be due to an impairment in NK/DC equilibrium in the bone marrow, because leukemic NK cells failed to induce DC maturation due to a NKp30 down-modulation [61].
3.4 Peripheral Blood Inflammatory Cytokines
Several proinflammatory cytokines have been identified to be higher in LGLL patients’ plasma in comparison to healthy controls, such as IL-1β, IL-1Rα, IFNγ, CCL5, CCL4, IL-18, IL-8, CXCL10, CXCL9, and IL-6. Most of them can be related to immune cytotoxic response after viral infection or to RA, which is often associated with LGLL [62,63,64,65,66]. The role of IL-6 was demonstrated: IL-6 and its specific receptor, IL-6Rα, were found to be higher in patients’ plasma, and they were released by the non-leukemic fraction of the mononuclear cells; IL-6 contributed to the survival by stimulating STAT3, a key protein in LGLL development [66].
IL-15 is another cytokine that was proven to be important in LGLL pathogenesis both in vitro and in vivo. IL-15 was shown to induce LGL cytotoxicity and proliferation through proteasomal degradation of the pro-apoptotic protein Bid [7, 67]. The pathogenetic role was demonstrated by the generation of IL-15 transgenic mice (IL-15tg) as they developed a fatal clonal NK and memory CD8+ expansion [68]. IL-15 induced chromosomal instability and DNA hypermethylation via repression of mir-29b and the induction of a Myc/NF-kB/DNMT3a axis [51]. Nevertheless, the lethal expansion was induced only when there was a cis activation by IL15Rα. In fact, the specific receptor IL-15Rα was expressed by LGLs, and it was detectable in high amounts in patients’ plasma [7, 69]. Further supporting the role of IL-15 in the pathogenesis, a systematic biology approach identified IL-15 and PDGF as master survival signaling switches that may have a profound effect on all known deregulations in T-LGL leukemia [70].
3.5 Clonal Drift
The phenomenon of clonal drift supports the theory that the emergence of LGL clone might be caused by the recognition of different epitopes of the same chronic antigen. This phenomenon is characterized by the change of the dominant LGL clone over the time. It has been reported that 37% of T-LGLL patients displayed a change in the dominant clone, developing a different Vβ clone instead of the original one owned at diagnosis as demonstrated by Vβ typing [71]. In another series of 42 patients with KIR-restricted CLPD-NK, the presence of monoclonal T cell populations in 48% of cases was also demonstrated. These T monoclonal populations can be detected at the time of diagnosis or occur during the natural history of disease, indicating that the association of T and NK proliferations is more frequent than initially thought. The T cell clone can eventually become so relevant to be dominant, leading to the shift from CLPD-NK to T-LGLL [72]. Similarly, also a T-LGLL patient who developed CLPD-NK over time has been described [73] (Fig. 15.5). All these observations indicate that cells are under antigenic pressure, suggesting that the putative antigen is likely to persist for many years and possibly for the lifelong of patients.
3.6 AICD Failure
Physiologically, during infection exposure or antigen stimulation, LGLs undergo proliferation and, after antigen clearance, are eliminated by a process called activation-induced cell death (AICD). This process leads to cell death through the induction of a death-inducing signaling complex (DISC). In LGLL patients, LGLs do not undergo apoptosis for a dysfunctional AICD mechanism, leading to the increase of leukemic cells in the peripheral blood. In detail, LGLs are not sensitive to Fas-induced apoptosis [74], a process essential for AICD [75], and possess high levels of c-FLIP, a DISC inhibitory protein [53].
3.7 JAK/STAT Pathway
In addition to the deregulation of apoptosis mechanism, in leukemic LGLs, multiple cell survival pathways have been found to be constitutively activated. Among these, JAK/STAT3 is the main involved axis. In fact, the activated (phosphorylated) form of STAT3 characterizes all leukemic LGLs, and it is currently considered the disease hallmark. The finding that the JAK-selective tyrosine kinase inhibitor AG-490 or the STAT3-specific inhibitor, Stattic, in vitro induces LGL apoptosis highlights the role of STAT3 in LGL clonal expansion [66, 76]. In 2012, recurrent somatic mutations in the Src homology 2 (SH2) domain of the STAT3 gene have been discovered. These gain-of-function mutations increase the stability of STAT3 dimers resulting in an enhanced transcriptional activity of the mutated proteins. Their frequency is 27–40% in T-LGLL patients [34, 77] and 9-30% in CLPD-NK [77, 90]. In the T-LGLL, STAT3 mutations characterize the CD8+ T-LGLL and have never been observed in the CD4+ T-LGLL [35, 40, 89]. Patients with STAT3 mutations present with neutropenia more frequently than patients without these mutations [35]. The association between PRCA and neutropenia with STAT3 gene mutations was also reported in Asia [78, 79]. The most frequent STAT3 mutations are Y640F and D661Y, representing 60% of the recognized mutations. Although almost all STAT3 lesions are located in SH2 domain, very rare activating mutations were described also in DNA-binding and coiled-coil domains [80]. Another member of STAT protein family has been reported carrying activating mutations in the SH2 domain, STAT5B. STAT5b mutations were identified in 2% of the CD8+ T-LGLL, specifically affecting the rare aggressive form of LGL leukemia [39], and were also found in 15–55% of CD4+ T-LGLL, whereas indolent CD8+ T-LGLL and CLPD-NK seemed to be devoid of these genetic lesions [35, 40].
Since in vitro inhibition of STAT3 was observed to restore the apoptosis of LGL independently from STAT3 mutational status and that STAT3 is activated also in STAT3 wild-type LGLL patients, STAT3 mutation cannot represent the only factor or be itself mandatory to trigger LGL clonal expansion. In unmutated LGLL patients, a high amount of the proinflammatory cytokine IL-6 is able to activate the STAT3 axis [66], and the inhibition of this cytokine restores LGL apoptosis. Moreover, in LGLL the physiological negative feedback loop carried out by the suppressor of cytokine signaling (SOCS3) protein on the activated STAT3 is downregulated [66].
3.8 Other Cell Survival Dysregulated Pathways
Although STAT3 activation plays the most significant role in LGL disorders, other multiple cell survival pathways have been described. Increased activity of the PI3K-AKT signaling axis in T-LGLs appears to operate in conjunction with or parallel to increased STAT3 activation to inhibit the apoptotic program [81]. Sustaining this axis, RANTES, MIP-1beta, and IL-18 are high in serum LGLL patients [64]. Acting downstream of the PI3K-AKT pathway to prevent apoptosis through Mcl-1 independently of STAT3, a crucial role is played by NF-kB. Leukemic LGLs express high levels of c-Rel, a member of the NF-kB family, and exhibit higher NF-kB activity than normal PBMCs [70]. A pathogenetic role for NF-kB signaling is also proved by the finding of a recurrent (8%) mutation of TNFAIP3, a NFkB inhibitor [82]. In CLPD-NK, the activation of Ras/MEK/ERK pathway contributes to the accumulation of NK cells caused by a constitutive stimulation of both ERK and Ras. Consistently, Ras and ERK inhibition causes the reduction of the survival of patient NK cells [83]. In addition, ERK1/2 signaling can be activated also by a dysregulation of sphingolipid rheostat [84, 85].
3.9 Neutropenia Molecular Mechanism
The pathogenesis of neutropenia in these patients is probably multifactorial, including humoral and cytotoxic mechanisms. However, the most important mechanism accounting for neutropenia is myeloid progenitor and neutrophil destruction via Fas-mediated apoptosis [86, 87]. T-LGLs express Fas ligand (FasL), and mature neutrophils express Fas. There is high surface expression of Fas/FasL in LGL, and large amounts of soluble FasL have been detected in sera of neutropenic T-LGL patients [35, 86]. FasL and other inhibitory cytokines produced by LGL may lead to hematopoietic suppression through apoptosis of neutrophil precursors in the bone marrow or result in direct killing of neutrophils that express a high concentration of Fas on their surface. The correction of cytopenias in T-LGL leukemia has been associated with a disappearance or reduction of serum FasL levels [86]. Intriguingly, it has been reported that FasL expression can be driven by STAT3 activation (higher in STAT3-mutated patients) [35]. In addition, it was recently shown that a microRNA(miR)-146b is downregulated specifically in neutropenic patients so allowing the translation of human antigen R (HuR), an essential FasL mRNA stabilizer. HuR protein mediates FasL mRNA stabilization, leading to increased FasL production and, consequently, to neutropenia development [88].
4 Concluding Remarks
Further knowledge of developmental pathways of normal LGLs is crucial to get insights into the characteristics of LGL disorders. This would allow to face the urgent unmet need to develop better therapeutics for LGL leukemia, because this disease still remains incurable. The knowledge of the precise mechanism through which mutated STAT5b can mediate an aggressive disease in CD8+ T-LGLL whereas the same mutation when present in CD4+ T-LGLL does not induce detrimental effects is central to design targeted therapies for these patients. Due to the rarity of disease, well-designed prospective comparative clinical trials are up to now lacking. Only the results from a randomized clinical trial from the USA recruiting 55 patients are available showing a still unsatisfactory overall response rate [42]. In addition, the results of an important prospected randomized clinical trial from France are coming (#NCT01976182). In the lack of this relevant information, the decision on which immunotherapy should be first started is still related to arbitrary medical decision. Finally, the possibility to know the biological mechanisms switching on and off in responding patients as compared to non-responding ones would certainly contribute to design more precisely targeted therapies.
References
Semenzato G, Zambello R, Starkebaum G, Oshimi K, Loughran TP Jr. The lymphoproliferative disease of granular lymphocytes: updated criteria for diagnosis. Blood. 1997;89:256–60.
Zambello R, Trentin L, Facco M, Cerutti A, Sancetta R, Milani A, et al. Analysis of the T cell receptor in the lymphoproliferative disease of granular lymphocytes: superantigen activation of clonal CD3+ granular lymphocytes. Cancer Res. 1995;55:6140–5.
Baesso I, Pavan L, Boscaro E, Miorin M, Facco M, Trentin L, et al. T-cell type lymphoproliferative disease of granular lymphocytes (LDGL) is equipped with a phenotypic pattern typical of effector cytotoxic cells. Leuk Res. 2007;31:371–7.
Bourgault-Rouxel AS, Loughran TP Jr, Zambello R, Epling-Burnette PK, Semenzato G, Donadieu J, et al. Clinical spectrum of gammadelta+ T cell LGL leukemia: analysis of 20 cases. Leuk Res. 2008;32:45–8.
Gentile TC, Uner AH, Hutchison RE, Wright J, Ben-Ezra J, Russell EC, et al. CD3+, CD56+ aggressive variant of large granular lymphocyte leukemia. Blood. 1994;84:2315–21.
Zambello R, Falco M, Della Chiesa M, Trentin L, Carollo D, Castriconi R, et al. Expression and function of KIR and natural cytotoxicity receptors in NK-type lymphoproliferative diseases of granular lymphocytes. Blood. 2003;102:1797–805.
Zambello R, Facco M, Trentin L, Sancetta R, Tassinari C, Perin A, et al. Interleukin-15 triggers the proliferation and cytotoxicity of granular lymphocytes in patients with lymphoproliferative disease of granular lymphocytes. Blood. 1997;89:201–11.
Barcena P, Jara-Acevedo M, Tabernero MD, Lopez A, Sanchez ML, Garcia-Montero AC, et al. Phenotypic profile of expanded NK cells in chronic lymphoproliferative disorders: a surrogate marker for NK-cell clonality. Oncotarget. 2015;6:42938–51.
Epling-Burnette PK, Painter JS, Chaurasia P, Bai F, Wei S, Djeu JY, et al. Dysregulated NK receptor expression in patients with lymphoproliferative disease of granular lymphocytes. Blood. 2004;103:3431–9.
Oshimi K. Progress in understanding and managing natural killer-cell malignancies. Br J Haematol. 2007;139:532–44.
Ishida F. Aggressive NK-cell leukemia. Front Pediatr. 2018;6:292.
Moignet A, Lamy T. Latest advances in the diagnosis and treatment of large granular lymphocytic leukemia. Am Soc Clin Oncol Educ Book. 2018;38:616–25.
Djaoud Z, David G, Bressollette C, Willem C, Rettman P, Gagne K, et al. Amplified NKG2C+ NK cells in cytomegalovirus (CMV) infection preferentially express killer cell Ig-like receptor 2DL: functional impact in controlling CMV-infected dendritic cells. J Immunol. 2013;191:2708–16.
Kawa-Ha K, Ishihara S, Ninomiya T, Yumura-Yagi K, Hara J, Murayama F, et al. CD3-negative lymphoproliferative disease of granular lymphocytes containing Epstein-Barr viral DNA. J Clin Invest. 1989;84:51–5.
Zambello R, Loughran TP Jr, Trentin L, Pontisso P, Battistella L, Raimondi R, et al. Serologic and molecular evidence for a possible pathogenetic role of viral infection in CD3-negative natural killer-type lymphoproliferative disease of granular lymphocytes. Leukemia. 1995;9:1207–11.
Hart DN, Baker BW, Inglis MJ, Nimmo JC, Starling GC, Deacon E, et al. Epstein-Barr viral DNA in acute large granular lymphocyte (natural killer) leukemic cells. Blood. 1992;79:2116–23.
Langerak AW, van Den Beemd R, Wolvers-Tettero IL, Boor PP, van Lochem EG, Hooijkaas H, et al. Molecular and flow cytometric analysis of the Vbeta repertoire for clonality assessment in mature TCRalphabeta T-cell proliferations. Blood. 2001;98:165–73.
Clemente MJ, Przychodzen B, Jerez A, Dienes BE, Afable MG, Husseinzadeh H, et al. Deep sequencing of the T-cell receptor repertoire in CD8+ T-large granular lymphocyte leukemia identifies signature landscapes. Blood. 2013;122:4077–85.
Morice WG, Kurtin PJ, Tefferi A, Hanson CA. Distinct bone marrow findings in T-cell granular lymphocytic leukemia revealed by paraffin section immunoperoxidase stains for CD8, TIA-1, and granzyme B. Blood. 2002;99:268–74.
Osuji N, Beiske K, Randen U, Matutes E, Tjonnfjord G, Catovsky D, et al. Characteristic appearances of the bone marrow in T-cell large granular lymphocyte leukaemia. Histopathology. 2007;50:547–54.
Dinmohamed AG, Brink M, Visser O, Jongen-Lavrencic M. Population-based analyses among 184 patients diagnosed with large granular lymphocyte leukemia in the Netherlands between 2001 and 2013. Leukemia. 2016;30:1449–51.
Shah MV, Hook CC, Call TG, Go RS. A population-based study of large granular lymphocyte leukemia. Blood Cancer J. 2016;6:e455.
Semenzato G, Pandolfi F, Chisesi T, De Rossi G, Pizzolo G, Zambello R, et al. The lymphoproliferative disease of granular lymphocytes. A heterogeneous disorder ranging from indolent to aggressive conditions. Cancer. 1987;60:2971–8.
Loughran TP Jr. Clonal diseases of large granular lymphocytes. Blood. 1993;82:1–14.
Dhodapkar MV, Li CY, Lust JA, Tefferi A, Phyliky RL. Clinical spectrum of clonal proliferations of T-large granular lymphocytes: a T-cell clonopathy of undetermined significance? Blood. 1994;84:1620–7.
Lamy T, Moignet A, Loughran TP Jr. LGL leukemia: from pathogenesis to treatment. Blood. 2017;129:1082–94.
Go RS, Li CY, Tefferi A, Phyliky RL. Acquired pure red cell aplasia associated with lymphoproliferative disease of granular T lymphocytes. Blood. 2001;98:483–5.
Zambello R, Semenzato G. Large granular lymphocyte disorders: new etiopathogenetic clues as a rationale for innovative therapeutic approaches. Haematologica. 2009;94:1341–5.
Zhang R, Shah MV, Loughran TP Jr. The root of many evils: indolent large granular lymphocyte leukaemia and associated disorders. Hematol Oncol. 2010;28:105–17.
Audemard A, Lamy T, Bareau B, Sicre F, Suarez F, Truquet F, et al. Vasculitis associated with large granular lymphocyte (LGL) leukemia: presentation and treatment outcomes of 11 cases. Semin Arthritis Rheum. 2013;43:362–6.
Murphy PW, Brett LK, Verla-Tebit E, Macik BG, Loughran TP Jr. Acquired inhibitors to factor VIII and fibrinogen in the setting of T-cell large granular lymphocyte leukemia: a case report and review of the literature. Blood Coagul Fibrinolysis. 2015;26:211–3.
Greenberg SA, Pinkus JL, Amato AA, Kristensen T, Dorfman DM. Association of inclusion body myositis with T cell large granular lymphocytic leukaemia. Brain. 2016;139:1348–60.
Lamy T, Loughran TP Jr. Clinical features of large granular lymphocyte leukemia. Semin Hematol. 2003;40:185–95.
Koskela HL, Eldfors S, Ellonen P, van Adrichem AJ, Kuusanmaki H, Andersson EI, et al. Somatic STAT3 mutations in large granular lymphocytic leukemia. N Engl J Med. 2012;366:1905–13.
Teramo A, Barila G, Calabretto G, Ercolin C, Lamy T, Moignet A, et al. STAT3 mutation impacts biological and clinical features of T-LGL leukemia. Oncotarget. 2017;8:61876–89.
Rajala HL, Olson T, Clemente MJ, Lagstrom S, Ellonen P, Lundan T, et al. The analysis of clonal diversity and therapy responses using STAT3 mutations as a molecular marker in large granular lymphocytic leukemia. Haematologica. 2015;100:91–9.
Rajala HL, Porkka K, Maciejewski JP, Loughran TP Jr, Mustjoki S. Uncovering the pathogenesis of large granular lymphocytic leukemia-novel STAT3 and STAT5b mutations. Ann Med. 2014;46:114–22.
Haapaniemi EM, Kaustio M, Rajala HL, van Adrichem AJ, Kainulainen L, Glumoff V, et al. Autoimmunity, hypogammaglobulinemia, lymphoproliferation, and mycobacterial disease in patients with activating mutations in STAT3. Blood. 2015;125:639–48.
Rajala HL, Eldfors S, Kuusanmaki H, van Adrichem AJ, Olson T, Lagstrom S, et al. Discovery of somatic STAT5b mutations in large granular lymphocytic leukemia. Blood. 2013;121:4541–50.
Andersson EI, Tanahashi T, Sekiguchi N, Gasparini VR, Bortoluzzi S, Kawakami T, et al. High incidence of activating STAT5B mutations in CD4-positive T-cell large granular lymphocyte leukemia. Blood. 2016;128:2465–8.
Barila G, Teramo A, Calabretto G, Ercolin C, Boscaro E, Trimarco V, et al. Dominant cytotoxic NK cell subset within CLPD-NK patients identifies a more aggressive NK cell proliferation. Blood Cancer J. 2018;8:51.
Loughran TP Jr, Zickl L, Olson TL, Wang V, Zhang D, Rajala HL, et al. Immunosuppressive therapy of LGL leukemia: prospective multicenter phase II study by the eastern cooperative oncology group (E5998). Leukemia. 2015;29:886–94.
Lamy T, Loughran TP Jr. How I treat LGL leukemia. Blood. 2011;117:2764–74.
Subbiah V, Viny AD, Rosenblatt S, Pohlman B, Lichtin A, Maciejewski JP. Outcomes of splenectomy in T-cell large granular lymphocyte leukemia with splenomegaly and cytopenia. Exp Hematol. 2008;36:1078–83.
Loughran TP Jr, Kidd PG, Starkebaum G. Treatment of large granular lymphocyte leukemia with oral low-dose methotrexate. Blood. 1994;84:2164–70.
Marchand T, Lamy T, Finel H, Arcese W, Choquet S, Finke J, et al. Hematopoietic stem cell transplantation for T-cell large granular lymphocyte leukemia: a retrospective study of the European Society for Blood and Marrow Transplantation. Leukemia. 2016;30:1201–4.
Waldmann TA, Conlon KC, Stewart DM, Worthy TA, Janik JE, Fleisher TA, et al. Phase 1 trial of IL-15 trans presentation blockade using humanized Mikbeta1 mAb in patients with T-cell large granular lymphocytic leukemia. Blood. 2013;121:476–84.
Epling-Burnette PK, Sokol L, Chen X, Bai F, Zhou J, Blaskovich MA, et al. Clinical improvement by farnesyltransferase inhibition in NK large granular lymphocyte leukemia associated with imbalanced NK receptor signaling. Blood. 2008;112:4694–8.
Wang TT, Yang J, Zhang Y, Zhang M, Dubois S, Conlon KC, et al. IL-2 and IL-15 blockade by BNZ-1, an inhibitor of selective gamma-chain cytokines, decreases leukemic T-cell viability. Leukemia. 2019;33:1243–55.
Shen L, Au WY, Guo T, Wong KY, Wong ML, Tsuchiyama J, et al. Proteasome inhibitor bortezomib-induced apoptosis in natural killer (NK)-cell leukemia and lymphoma: an in vitro and in vivo preclinical evaluation. Blood. 2007;110:469–70.
Mishra A, Liu S, Sams GH, Curphey DP, Santhanam R, Rush LJ, et al. Aberrant overexpression of IL-15 initiates large granular lymphocyte leukemia through chromosomal instability and DNA hypermethylation. Cancer Cell. 2012;22:645–55.
Yang J, LeBlanc FR, Dighe SA, Hamele CE, Olson TL, Feith DJ, et al. TRAIL mediates and sustains constitutive NF-kappaB activation in LGL leukemia. Blood. 2018;131:2803–15.
Yang J, Epling-Burnette PK, Painter JS, Zou J, Bai F, Wei S, et al. Antigen activation and impaired Fas-induced death-inducing signaling complex formation in T-large-granular lymphocyte leukemia. Blood. 2008;111:1610–6.
Zambello R, Teramo A, Barila G, Gattazzo C, Semenzato G. Activating KIRs in chronic lymphoproliferative disorder of NK cells: protection from viruses and disease induction? Front Immunol. 2014;5:72.
Pandolfi F, Loughran TP Jr, Starkebaum G, Chisesi T, Barbui T, Chan WC, et al. Clinical course and prognosis of the lymphoproliferative disease of granular lymphocytes. A multicenter study. Cancer. 1990;65:341–8.
Loughran TP Jr, Zambello R, Ashley R, Guderian J, Pellenz M, Semenzato G, et al. Failure to detect Epstein-Barr virus DNA in peripheral blood mononuclear cells of most patients with large granular lymphocyte leukemia. Blood. 1993;81:2723–7.
Loughran TP Jr, Hadlock KG, Yang Q, Perzova R, Zambello R, Semenzato G, et al. Seroreactivity to an envelope protein of human T-cell leukemia/lymphoma virus in patients with CD3- (natural killer) lymphoproliferative disease of granular lymphocytes. Blood. 1997;90:1977–81.
Rodriguez-Caballero A, Garcia-Montero AC, Barcena P, Almeida J, Ruiz-Cabello F, Tabernero MD, et al. Expanded cells in monoclonal TCR-alphabeta+/CD4+/NKa+/CD8−/+dim T-LGL lymphocytosis recognize hCMV antigens. Blood. 2008;112:4609–16.
Mailloux AW, Zhang L, Moscinski L, Bennett JM, Yang L, Yoder SJ, et al. Fibrosis and subsequent cytopenias are associated with basic fibroblast growth factor-deficient pluripotent mesenchymal stromal cells in large granular lymphocyte leukemia. J Immunol. 2013;191:3578–93.
Zambello R, Berno T, Cannas G, Baesso I, Binotto G, Bonoldi E, et al. Phenotypic and functional analyses of dendritic cells in patients with lymphoproliferative disease of granular lymphocytes (LDGL). Blood. 2005;106:3926–31.
Balsamo M, Zambello R, Teramo A, Pedrazzi M, Sparatore B, Scordamaglia F, et al. Analysis of NK cell/DC interaction in NK-type lymphoproliferative disease of granular lymphocytes (LDGL): role of DNAM-1 and NKp30. Exp Hematol. 2009;37:1167–75.
Makishima H, Ishida F, Ito T, Kitano K, Ueno S, Ohmine K, et al. DNA microarray analysis of T cell-type lymphoproliferative disease of granular lymphocytes. Br J Haematol. 2002;118:462–9.
Choi YL, Makishima H, Ohashi J, Yamashita Y, Ohki R, Koinuma K, et al. DNA microarray analysis of natural killer cell-type lymphoproliferative disease of granular lymphocytes with purified CD3-CD56+ fractions. Leukemia. 2004;18:556–65.
Kothapalli R, Nyland SB, Kusmartseva I, Bailey RD, McKeown TM, Loughran TP Jr. Constitutive production of proinflammatory cytokines RANTES, MIP-1beta and IL-18 characterizes LGL leukemia. Int J Oncol. 2005;26:529–35.
Momose K, Makishima H, Ito T, Nakazawa H, Shimodaira S, Kiyosawa K, et al. Close resemblance between chemokine receptor expression profiles of lymphoproliferative disease of granular lymphocytes and their normal counterparts in association with elevated serum concentrations of IP-10 and MIG. Int J Hematol. 2007;86:174–9.
Teramo A, Gattazzo C, Passeri F, Lico A, Tasca G, Cabrelle A, et al. Intrinsic and extrinsic mechanisms contribute to maintain the JAK/STAT pathway aberrantly activated in T-type large granular lymphocyte leukemia. Blood. 2013;121:3843–54. S1
Hodge DL, Yang J, Buschman MD, Schaughency PM, Dang H, Bere W, et al. Interleukin-15 enhances proteasomal degradation of bid in normal lymphocytes: implications for large granular lymphocyte leukemias. Cancer Res. 2009;69:3986–94.
Fehniger TA, Suzuki K, VanDeusen JB, Cooper MA, Freud AG, Caligiuri MA. Fatal leukemia in interleukin-15 transgenic mice. Blood Cells Mol Dis. 2001;27:223–30.
Chen J, Petrus M, Bamford R, Shih JH, Morris JC, Janik JE, et al. Increased serum soluble IL-15Ralpha levels in T-cell large granular lymphocyte leukemia. Blood. 2012;119:137–43.
Zhang R, Shah MV, Yang J, Nyland SB, Liu X, Yun JK, et al. Network model of survival signaling in large granular lymphocyte leukemia. Proc Natl Acad Sci U S A. 2008;105:16308–13.
Clemente MJ, Wlodarski MW, Makishima H, Viny AD, Bretschneider I, Shaik M, et al. Clonal drift demonstrates unexpected dynamics of the T-cell repertoire in T-large granular lymphocyte leukemia. Blood. 2011;118:4384–93.
Gattazzo C, Teramo A, Passeri F, De March E, Carraro S, Trimarco V, et al. Detection of monoclonal T populations in patients with KIR-restricted chronic lymphoproliferative disorder of NK cells. Haematologica. 2014;99:1826–33.
Yan Y, Olson TL, Nyland SB, Feith DJ, Loughran TP Jr. Emergence of a STAT3 mutated NK clone in LGL leukemia. Leuk Res Rep. 2015;4:4–7.
Lamy T, Liu JH, Landowski TH, Dalton WS, Loughran TP Jr. Dysregulation of CD95/CD95 ligand-apoptotic pathway in CD3(+) large granular lymphocyte leukemia. Blood. 1998;92:4771–7.
Krueger A, Fas SC, Baumann S, Krammer PH. The role of CD95 in the regulation of peripheral T-cell apoptosis. Immunol Rev. 2003;193:58–69.
Epling-Burnette PK, Liu JH, Catlett-Falcone R, Turkson J, Oshiro M, Kothapalli R, et al. Inhibition of STAT3 signaling leads to apoptosis of leukemic large granular lymphocytes and decreased Mcl-1 expression. J Clin Invest. 2001;107:351–62.
Jerez A, Clemente MJ, Makishima H, Koskela H, Leblanc F, Peng Ng K, et al. STAT3 mutations unify the pathogenesis of chronic lymphoproliferative disorders of NK cells and T-cell large granular lymphocyte leukemia. Blood. 2012;120:3048–57.
Qiu ZY, Fan L, Wang L, Qiao C, Wu YJ, Zhou JF, et al. STAT3 mutations are frequent in T-cell large granular lymphocytic leukemia with pure red cell aplasia. J Hematol Oncol. 2013;6:82.
Ishida F, Matsuda K, Sekiguchi N, Makishima H, Taira C, Momose K, et al. STAT3 gene mutations and their association with pure red cell aplasia in large granular lymphocyte leukemia. Cancer Sci. 2014;105:342–6.
Andersson E, Kuusanmaki H, Bortoluzzi S, Lagstrom S, Parsons A, Rajala H, et al. Activating somatic mutations outside the SH2-domain of STAT3 in LGL leukemia. Leukemia. 2016;30:1204–8.
Schade AE, Wlodarski MW, Maciejewski JP. Pathophysiology defined by altered signal transduction pathways: the role of JAK-STAT and PI3K signaling in leukemic large granular lymphocytes. Cell Cycle. 2006;5:2571–4.
Johansson P, Bergmann A, Rahmann S, Wohlers I, Scholtysik R, Przekopowitz M, et al. Recurrent alterations of TNFAIP3 (A20) in T-cell large granular lymphocytic leukemia. Int J Cancer. 2016;138:121–4.
Epling-Burnette PK, Bai F, Wei S, Chaurasia P, Painter JS, Olashaw N, et al. ERK couples chronic survival of NK cells to constitutively activated Ras in lymphoproliferative disease of granular lymphocytes (LDGL). Oncogene. 2004;23:9220–9.
LeBlanc FR, Liu X, Hengst J, Fox T, Calvert V, Petricoin EF 3rd, et al. Sphingosine kinase inhibitors decrease viability and induce cell death in natural killer-large granular lymphocyte leukemia. Cancer Biol Ther. 2015;16:1830–40.
Kothapalli R, Kusmartseva I, Loughran TP. Characterization of a human sphingosine-1-phosphate receptor gene (S1P5) and its differential expression in LGL leukemia. Biochim Biophys Acta. 2002;1579:117–23.
Liu JH, Wei S, Lamy T, Epling-Burnette PK, Starkebaum G, Djeu JY, et al. Chronic neutropenia mediated by fas ligand. Blood. 2000;95:3219–22.
Lamy T, Bauer FA, Liu JH, Li YX, Pillemer E, Shahidi H, et al. Clinicopathological features of aggressive large granular lymphocyte leukaemia resemble Fas ligand transgenic mice. Br J Haematol. 2000;108:717–23.
Mariotti B, Calabretto G, Rossato M, Teramo A, Castellucci M, Barilà G, et al. Identification of a miR-146b-Fas ligand axis in the development of neutropenia in T large granular lymphocyte leukemia. Haematologica. 2020;105:1351–1360.
Teramo A, Barilà G, Calabretto G, Vicenzetto C, Gasparini VR, Semenzato G, et al. Insights Into Genetic Landscape of Large Granular Lymphocyte Leukemia. Front Oncol. 2020;10:152.
Gasparini VR, Binatti A, Coppe A, Teramo A, Vicenzetto C, Calabretto G, et al. A high definition picture of somatic mutations in chronic lymphoproliferative disorder of natural killer cells. Blood Cancer Journal. 2020;10:42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Teramo, A. et al. (2021). Large Granular Lymphocyte Leukemia. In: Dreyling, M., Ladetto, M. (eds) Indolent Lymphomas . Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-55989-2_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-55989-2_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-55988-5
Online ISBN: 978-3-030-55989-2
eBook Packages: MedicineMedicine (R0)