Abstract
Almost all general surgery residents consider post-residency training, and up to 80% ultimately pursue fellowship. Important considerations for choosing a surgical specialty include having a thorough understanding of the types of cases you most enjoy doing and patients you most enjoy treating, seeking guidance from trusted mentors, and identifying early “test run” experiences. Ultimately, the decision must be based on personal interests and life considerations which inform the professional choices.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Michelle is a junior surgical resident starting to consider her choice of surgical specialties. Her favorite rotation was on the trauma service, in large part because she was allowed to do multiple procedures independently in the intensive care unit. She is concerned about the work-life balance of a trauma faculty member, but she is worried about raising this concern to her faculty mentors. She wonders what factors she should consider when making her specialty choice.
Approximately three-quarters of graduating general surgery chief residents pursue post-residency surgical fellowship training, leading to general surgery largely becoming a specialty-based practice [1,2,3,4,5]. In the US, more than 20 specialty fellowships of surgery are recognized; this does not include other surgical specialties, such as orthopedics, neurosurgery, urology, ophthalmology, and otolaryngology, all of which have separate residency training programs [6]. General surgery residents believe that pursuing specialty training will lead to better success in the job market, a better income, and potentially a better lifestyle [7]. While decision-making around specialty choice is complex, some key factors provide a framework for how learners can make an informed specialty choice. These include consideration of the types of cases and clinical problems that will be encountered in the specialty; quality of life and on-call responsibilities; competitiveness of the specialty’s fellowship match; the job market and financial compensation; alignment with extra-clinical research or advocacy interests; and the influence of mentors (Table 5.1) [2, 8].
5.1 Framework for Making a Surgical Specialty Choice
Do you want to be a specialist or (relative) generalist? Some specialties, such as hand surgery or transplantation, are relatively narrow in their scope of practice, both in terms of diseases treated and the variety of index cases performed. Others, such as surgical oncology, pediatric surgery, and trauma and acute care surgery, remain broader in disease scope and procedure types performed. Some learners are attracted to the “super-specialist” concept, where a narrow scope of practice allows for deep expertise, such that sooner rather than later it might be possible to comfortably take on the most complex cases within the field or be the pre-eminent content expert. In this scenario, variety is primarily derived from clinical nuance and complexity. In contrast, a more “generalist” practice may involve a wider variety of disease pathologies and anatomic locations.
What types of patients do you want to care for? A high level of intellectual curiosity regarding the disease processes most commonly treated by the specialty is of critical importance in choosing a specialty. For example, a practice in surgical oncology requires a keen interest in tumor biology, multi-disciplinary care and coordination, and acumen in interacting with patients and families potentially facing end of life decisions. A practice in transplantation demands an understanding of rejection and immunosuppression as well as an appreciation for the social determinants that may impact a patient’s success after transplantation. As much as possible, decisions around specialty choice should be made in light of the common diagnoses and pathologies that will be encountered by the specialty (i.e. the ‘horses’) rather than the rare or exceptional cases (i.e. the ‘zebras’).
What are you needed to do? Almost all specialties have a mix of cases that could be considered “want to” and “need to,” and sometimes the “need to” can drive specialty choice. In most cases, a new surgeon’s early case mix will include a healthy number of “need to” cases, so comfort with these cases should be considered when making a specialty choice. For example, a person who enjoys living donor kidney transplantation will likely need to do a variety of dialysis access cases or deceased donor procurements before achieving a more advanced practice mix that includes more of the “want to” cases.
What about quality of life ? Choosing a specialty that brings fulfillment is a necessary first step in achieving optimal work life integration. Basing specialty choice only on quality of life or call responsibility considerations may lead to dissatisfaction if the cases and patients don’t ultimately align with a resident’s interests. But quality of life and call responsibilities cannot be completely ignored, as they are significantly correlated with subsequent job satisfaction and burnout [9]. A systematic review demonstrated some variation in satisfaction and burnout by specialty, with pediatric and endocrine surgeons demonstrating the highest career satisfaction, whereas a significant proportion of plastic surgeons and vascular surgeons were least satisfied [10]. These factors should be considered both in the context of the resident’s present and future life interest and responsibilities. What is appealing when you are young might not continue to be so appealing when you are older or approaching the end of your career.
How does the specialty align with your research, education or advocacy interests? For residents considering a career in academic surgery, the clinical specialty choice ideally is synergistic with extra-clinical research, education, service, or advocacy interests. A resident with significant interest in pursuing a scientific career studying vascular biology would likely achieve optimal synergy in the practice of vascular surgery or transplantation. While exact alignment of academic interests and clinical practice is not always required, a synergistic relationship between scholarly interest and clinical practice is likely to lead to the most success and will certainly entail more efficiency in the long term.
How competitive is the fellowship match? Concern about matching into a fellowship program is rated as a significant factor in specialty choice by nearly a quarter of residents [2]. One study analyzed trends in a normalized competitiveness index over time and rated pediatric surgery as the most competitive specialty, while surgical critical care and vascular surgery were the least competitive [11]. These results are consistent with other studies that have documented a 50% match rate in pediatric surgery [12]. Consideration for the likelihood of a successful match should be made in conjunction with surgical mentors within the field and take into account objective metrics such as American Board of Surgery In Training Examination (ABSITE) scores, rotation evaluations, research and publication record, and references.
How is the job market ? Successfully matching into a surgical specialty fellowship does not guarantee employment in a job that is entirely supported by cases in that clinical discipline, and fear of unemployment or underemployment can be a major factor in specialty choice [13]. Particularly for specialties treating relatively rare diseases, graduating fellows may find few desirable employment opportunities awaiting them at the end of fellowship training. This can mean significant compromise around employer geographic location or institution type. For specialties treating more common diseases and conditions such as breast surgical oncology, trauma and acute care surgery, and/or colorectal surgery, the job market may present options with an immediate specialty-based practice. For specialties and in areas with a more limited referral base, new graduates may consider a more generalized practice early in their careers until a specialty practice can be built—i.e., an endocrine surgeon may consider doing general surgery while building referrals around thyroid, parathyroid and adrenal pathologies. Differential financial compensation also may be considered, but only 20% of residents rate income as an important factor in their choice of clinical specialty [2].
What future trends may impact the specialty? Advances in endovascular surgery have transitioned vascular surgery away from open procedures to catheter-based procedures using imaging guidance. Similar advances in therapeutic endoscopy have changed the scope and complexity of many disorders treated by minimally invasive surgeons. Discoveries in cancer therapeutics could drastically alter the surgical indications for some diseases. These future trends include potential innovations in technologies, such as devices or techniques that will require substantial commitment to ongoing continuing medical education. While not entirely predictable, some consideration should be given to the role future discovery or trends could have on case mix and specialty choice.
Who are your influential surgical mentors? Along with the patients and cases typical of the specialty, fellows rank the influence of a mentor as among the most important factors in their choice of specialty [8]. Surgical mentors can most closely model the experiences of a faculty or attending specialist with regard to the mix of outpatient and inpatient time, call responsibilities and ability to achieve work-life integration. Surgical mentors who are passionate about their specialty and derive fulfillment through their clinical work can be compelling recruiters to their surgical specialty, but learners should be careful not to rely only on anecdotal experiences based on an ‘N of 1’. Instead, residents should pursue broad exposure to clinical mentors and current fellows via different rotations (and electives when possible) during residency and through networking at regional, national or international meetings.
Ben is a senior surgical resident who has decided to pursue a fellowship in minimally invasive surgery after spending 2 years in a vascular biology lab. He discusses this choice with his research mentor who tries to be supportive, but ultimately laments that he is “wasting his talent.”
While many of the above factors should be considered when choosing a surgical specialty, other factors should raise a red flag in specialty decision making. These include choosing a specialty to please a mentor or other influential person and perceptions about specialty hierarchy.
Seeking approval from a mentor, parent or other influential figure. The best mentors do not want to create mentees solely in their own image; rather, mentoring requires generosity and the ability to allow mentees the opportunity to create themselves in their own right [14]. The decision to not follow in clinical footsteps of a beloved mentor can be a difficult choice for a mentee, but one that should be fully supported by the mentor. Similar to seeking approval of a mentor, specialty choice should not be dependent on other external pressures, such as approval from family members, friends or other colleagues. Physician’s children are 24 times more likely than their peers to enter medicine, speaking to the “inherited” nature of the medical profession. While there are not strong data with regard to the influence of family members around subsequent specialty choice, one can assume that a parent’s specialty choice could significantly influence the choice of the child. Learners with physician family members should seek the advice of those family members, but also be certain they are making a specialty choice that aligns with their own interests. Remember: life is short, and it is yours to live!
Perceived specialty hierarchy . Perhaps due to biases related to the surgeons that choose certain specialties or the patients or diseases treated by these specialists, some hold onto the view that some specialties are more highly valued and require substantially more surgical skill, while other specialties do not. Other specialties could be viewed as more appealing for other reasons. This implicit belief could be seen in the clinical specialties of surgeons most likely to be selected for leadership positions, such as Chief of Surgery or Department Chair, where historically the clinical specialties of surgical oncology and transplantation have been heavily represented, and breast surgical oncology or minimally invasive surgery have been underrepresented. This bias can unnecessarily create pressure for trainees to pursue certain specialties or discourage the most talented residents from pursuing other specialties.
5.2 Practical Steps in Making a Decision
Ben is a medical student applying in surgery. He has an interest in pediatric surgery and is uncertain about what steps he should take to decide whether or not this is the correct choice for him.
Students and residents considering a surgical specialty can take numerous practical steps to decide whether that specialty is the right choice. These include making wise initial choices related to residency selection; keeping an open mind; seeking opinions from a broad range of mentors; and taking a “test run” of what it’s like to work in that specialty through experiences on elective rotations, research projects, and at national meetings (Table 5.2).
The influence of the general surgery training program. Rotation experiences have been demonstrated to highly influence resident perception of specialty scope [15]. Some general surgery training programs have a few specialties that are particularly prominent at their institution, in part as a result of the influence of departmental leadership, a research or scholarship focus, geographic location and referral base, local competitors, institutional priorities, or long-standing tradition. This relative prominence can influence specialty choice through early clinical rotations or influential surgical mentors. Similarly, if a particular program has a relative weakness in a clinical discipline (few providers or a small market share or footprint), it might be less likely that residents will have significant enough exposure to the specialty in a meaningful way to cast a fellowship choice in that specialty in a favorable light. Given the strong influence of clinical exposure, it is therefore important that applicants prioritize residency training programs that are strong across many disciplines and that have a track record of placing applicants into many different clinical specialty fellowships. Additionally, exposure should be balanced throughout the clinical years, such that residents can experience specialties before important choices regarding research time or fellowship must be made.
Keep an open mind. While young trainees may be influenced by early rotations, it is important to keep an open mind regarding subsequent fellowship choices. Early experiences (whether good or bad) do not always transition to the typical experiences of senior residents, fellows and faculty in that specialty. Certain experiences that may be very impactful for a practicing surgeon—such as talking a patient through a new cancer diagnosis and then performing his or her cancer resection—may not be easily accessible to a junior surgical resident. By keeping an open mind, trainees can ensure that they have the most information regarding a specialty through their longitudinal experience and graduated responsibility.
Seeking broad opinions. While it is common for trainees to focus on one or two close surgical mentors when selecting a clinical specialty, it is important to consider the opinions of a broad group of faculty and peers when making a specialty choice. Diverse opinions may provide a more balanced view of the pros and cons of various specialties or work to dispel misconceptions about certain clinical disciplines. Soliciting mentorship from a diverse group of faculty also provides some protection from choosing a specialty only because of one dominant mentor, as other mentors can provide advice and support to the resident in case of a split in recommendations or conflict with the primary mentor.
Give it a test run. One of the best ways to confirm that you have made the correct choice about specialty is to give it a test run through dedicated or elective rotations, working on a research project, and/or attending a national meeting in that specialty. This ‘deeper dive’ in the clinical discipline can help to confirm that clinical or research problems are interesting to you, and that the choice seems to be a good fit. Alternatively, a test run may cause re-consideration of specialty choice even relatively late in the process. If this occurs, it is important to remember it is never ‘too late’ to change course if the specialty no longer feels as if it is the best option.
5.3 Diversity, Equity and Inclusion Considerations and Specialty Choice
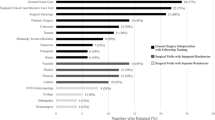
A diverse surgical workforce is necessary to ensure that the field of surgery is optimally positioned to solve complex problems, care for patients, and train the legacy generation [16]. While there have been increases in the number of women choosing to pursue a career in surgery, these gains have not been seen across all specialties, and little progress has occurred around recruiting underrepresented minorities (URMs) into surgical fields. For example, while women and men are equally likely to pursue post-residency fellowship training, there are gender-based differences around specialty choice. Women are more likely to pursue fellowships in surgical oncology, colorectal surgery, and critical care, whereas they are much less likely to pursue fellowship training in thoracic surgery, vascular surgery and transplant surgery (Table 5.3) [4]. These data raise several diversity, equity and inclusion considerations around specialty choice.
Mentorship and representation matters. Given the observation than an influential mentor plays a critical role in a resident’s specialty choice, ensuring access to mentors for all trainees is critical for optimizing diversity, equity and inclusion across surgical specialties. Women and URMs in surgery frequently cite a lack of mentorship as contributing to their general dissatisfaction [17]. Since mentorship is cited as a major influence in choosing a specialty, a paucity of mentors in certain specialties may contribute to gender- or race-based differences in specialty choice. Faculty from all specialties should ensure they are open to mentoring a diverse group of residents. Availability of effective mentorship also requires that specialties work to achieve equity among their ranks at all levels, including leadership positions. Representation and activities at national meetings (particularly around networking and social activities where informal mentorship occurs) should be made to be as inclusive as possible to communicate an openness of the discipline to a diverse workforce.
Work-Life Integration. Some specialties are perceived to be less receptive to the integration of motherhood. In a survey of general surgery residents who were pregnant and delivered a child during surgical training, 15% of respondents altered their fellowship plans owing to perceived challenges of work-life integration . These women commonly did not pursue fellowship or switched to breast surgery or trauma and acute care surgery [18]. In order to achieve diversity, all specialties should actively consider their family leave policies and work to create the most permissive policies possible within the confines of what is required for excellent patient care.
Susan recently completed a fellowship in trauma and surgical critical care at the urging of her mentors. Now in her first year of practice, she finds she misses elective surgery and a longitudinal relationship with patients. She is considering a change of specialty but is uncertain about how to take the next step.
There is more than one way to get to the right specialty choice, including choosing the wrong one initially. There are no definitive data on the number of surgeons who change specialties; given the high rates of dissatisfaction and burnout that exist within surgery, it is likely that many consider a career change, and some pursue it. Deciding to train (again) in a different specialty can be disruptive, requiring a geographic move and resulting in income loss, but for those who pursue it, the end result can be rewarding. The process of changing specialties can be informed by many of the strategies outlined above, including talking with mentors and surgeons in the specialty, seeking broad opinions, and gaining some experiences in the specialty to the extent possible. In addition, those who are considering a specialty change should consult with a trusted mentor or professional coach to assist with self-reflection with regard to the motivation for the change. Once the decision is made, charting a path forward will likely require consultation with members of the specialty to determine the best re-training options.
5.4 Conclusion
Almost all general surgery residents will at least consider post-residency training, and up to 80% ultimately pursue it. Important considerations include having a thorough understanding of the types of cases you most enjoy doing and patients you most enjoy treating, seeking guidance from trusted mentors, and identifying early “test run” experiences. Ultimately, the decision must be based on personal interests and life considerations which inform the professional choices. Specialty societies should promote diversity of membership and inclusivity among the leadership to ensure their specialties remain open to a diverse candidate pool.
References
Klingensmith ME, Cogbill TH, Luchette F, et al. Factors influencing the decision of surgery residency graduates to pursue general surgery practice versus fellowship. Ann Surg. 2015;262(3):449–55; discussion 445–454.
Reed CE, Vaporciyan AA, Erikson C, et al. Factors dominating choice of surgical specialty. J Am Coll Surg. 2010;210(3):319–24.
Fischer JE. The impending disappearance of the general surgeon. JAMA. 2007;298(18):2191–3.
Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. J Am Coll Surg. 2008;206(5):782–8; discussion 788–789.
Lewis FR, Klingensmith ME. Issues in general surgery residency training--2012. Ann Surg. 2012;256(4):553–9.
Grover BT, Kothari SN. Fellowship training: need and contributions. Surg Clin North Am. 2016;96(1):47–57.
Yeo H, Viola K, Berg D, et al. Attitudes, training experiences, and professional expectations of US general surgery residents: a national survey. JAMA. 2009;302(12):1301–8.
McCord JH, McDonald R, Sippel RS, Leverson G, Mahvi DM, Weber SM. Surgical career choices: the vital impact of mentoring. J Surg Res. 2009;155(1):136–41.
Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–71.
Pulcrano M, Evans SR, Sosin M. Quality of life and burnout rates across surgical specialties: a systematic review. JAMA Surg. 2016;151(10):970–8.
Yheulon CG, Cole WC, Ernat JJ, Davis SS. Normalized competitive index: analyzing trends in surgical fellowship training over the past decade (2009-2018). J Surg Educ. 2020;77(1):74–81.
Beres A, Baird R, Puligandla PS. Success in the pediatric surgery match: a survey of the 2010 applicant pool. J Pediatr Surg. 2011;46(5):957–61.
Adams S, Ginther DN, Neuls E, Hayes P. Attitudes and factors contributing to attrition in Canadian surgical specialty residency programs. Can J Surg. 2017;60(4):247–52.
Chopra V, Edelson DP, Saint S. A PIECE OF MY MIND. Mentorship malpractice. JAMA. 2016;315(14):1453–4.
Vick LR, Borman KR, May W. See one, do one, be competent in one? Resident rotations broaden the perceived scope of general surgery. J Surg Educ. 2007;64(6):410–5.
Page SE. Diversity bonus: how great teams pay off in the knowledge economy. Our compel interest. Princeton: Princeton University Press; 2017. p. 1–302.
Thompson-Burdine JA, Telem DA, Waljee JF, et al. Defining barriers and facilitators to advancement for women in academic surgery. JAMA Netw Open. 2019;2(8):e1910228.
Rangel EL, Lyu H, Haider AH, Castillo-Angeles M, Doherty GM, Smink DS. Factors associated with residency and career dissatisfaction in childbearing surgical residents. JAMA Surg. 2018;153(11):1004–11.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Dossett, L.A., Sosa, J.A. (2021). Choosing a Surgical Specialty. In: Telem, D.A., Martin, C.A. (eds) Diversity, Equity and Inclusion. Success in Academic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-55655-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-55655-6_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-55654-9
Online ISBN: 978-3-030-55655-6
eBook Packages: MedicineMedicine (R0)