Abstract
Esophageal motor disorders are common in patients with morbid obesity. The most detailed objective evaluation of esophageal function involves esophageal manometry testing. Bariatric surgery impacts esophageal motility including peristalsis and lower esophageal sphincter (LES) pressure. Preoperative manometry is useful in surgical planning if there exists concern for underlying esophageal dysmotility. As gastric banding appears to impair LES relaxation, this procedure should be performed judiciously in patients with underlying abnormal peristalsis. Sleeve gastrectomy in patients with a hypotensive LES should be performed with caution, although existing data is limited on how this impacts outcomes. Roux-en-Y gastric bypass has been found to lead to the least functional impairment of the LES and esophageal peristalsis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Esophageal dysmotility is common in morbidly obese patients. Multiple studies have suggested that individuals with morbid obesity have a significantly increased prevalence of esophageal motor disorders compared to their non-obese peers, including abnormal lower esophageal sphincter (LES) function and altered peristalsis. In addition, current literature suggests that bariatric surgery affects esophageal motility and health, thus increasing the importance of including an evaluation of swallowing disorders in the preoperative stage.
Per current clinical practice guidelines, esophageal manometry is not routinely performed as part of the preoperative work-up of all patients undergoing bariatric surgery [1]. However, there is mounting evidence of the usefulness of manometry prior to bariatric surgery and many institutions are incorporating the performance of manometry into their preoperative protocols. Different bariatric surgical techniques can influence both LES pressures as well as peristalsis, thus the choice of therapy should be carefully and individually considered for each surgical candidate. Understanding physiologic changes that occur as a result of bariatric surgery can help guide what preoperative evaluation should be performed and when to use caution in choosing surgical options. This chapter will address whether esophageal manometry testing should be included as a part of preoperative testing in bariatric surgery and discuss the changes in esophageal mechanics related to bariatric surgery.
2 Search Strategy
A literature search of English language publications in the medical database (PubMed) from 1999 to 2019 was used to identify published data on the use of manometry in bariatric surgery. Terms used in the search were “manometry”, “motility disorder”, “esophageal function”, “esophageal motor disorder”, “dysmotility”, and “preoperative”, “weight loss surgery”, “bariatric surgery”. Due to low numbers of high evidence papers, the majority of the studies were prospective or retrospective cohort studies, with no randomized controlled trials available. The data was classified using the GRADE system.
3 Results
3.1 Prevalence of Esophageal Disorders in Morbidly Obese Patients
When completing the bariatric preoperative evaluation, it is important to understand that individuals with morbid obesity have a significantly increased prevalence of esophageal motor disorders compared to individuals without obesity. Morbid obesity has been found to be associated with increased dysmotility of both the LES and the esophageal body. The mechanism responsible for alterations in motility in this population remains to be clearly defined. One proposed mechanism suggests that intake of food high in fat content leads to lower LES pressure through the secretion of hormones such as secretin and cholecystokinin [2]. The reported prevalence of both any abnormal manometric findings and of specific diagnosed esophageal disorders significantly varies between studies. (Table 15.1) This may be in part due to the dynamic landscape of manometry interpretation and continuously evolving understanding of esophageal mechanics.
Reported general abnormal esophageal motility in morbid obesity ranged from 17% on the conservative side to up to 61% [3, 8]. In comparison to healthy controls, Iovino et al. demonstrated significantly lower LES pressure in the morbidly obese [10]. Other authors have also found a hypotensive LES as the most common pathology on manometry in this population [7, 9]. The prevalence of a hypotensive LES was reported to range from 6.8% to 25% [3, 5]. Jaffin and colleagues studied 111 morbidly obese patients seeking bariatric surgery, finding that 61% had abnormal manometric findings [3]. This included 25% of patients with a hypotensive LES and 21% with a hypertensive disorder of the esophageal body. Interestingly, 59% of patients with abnormal manometry were asymptomatic, raising concern for abnormal visceral sensation in the morbidly obese population. A more recent evaluation of 221 patients who underwent preoperative manometric testing revealed disturbed manometry in 33.4%, of which 64% had a hypotensive LES [7]. This subset of patients was more likely to have erosive esophagitis and pathologic pH reflux monitoring; however, reflux symptoms did not appear to significantly differ between subjects with normotensive and hypotensive LES, suggesting that reflux symptoms alone may not be a reliable measure of underlying pathology.
Kristo et al. published a prospective analysis of 147 individuals with morbid obesity who underwent esophageal function testing, aimed to investigate the prevalence and to characterize the pathology in this population [5]. They found that 34% of patients had a motility disorder per the Chicago Classification, 14.3% had a hypertensive LES and 6.8% a hypotensive LES. Interestingly, the hypercontractility disorder Jackhammer esophagus was discovered in 7.5% of subjects. Older studies have also described an increased prevalence of elevated contraction amplitudes on manometry in the morbidly obese, although many noted hypertensive peristalsis called Nutcracker esophagus, which has since been omitted from the most recent Chicago Classification due to its unclear clinical significance [3, 4]. Comparison of these studies is difficult given that manometry interpretation guidelines have significantly changed over the course of time, but it raises the suspicion of undiagnosed hypertensive esophageal body disorders in this population. As newer longitudinal studies suggest that a quarter of Jackhammer esophagus patients progress to achalasia, this even further highlights the importance of a careful preoperative evaluation of esophageal health prior to bariatric surgery [11].
3.2 Preoperative Evaluation
Multiple components of the preoperative evaluation may raise suspicion of an underlying esophageal motor disorder and help guide the decision to pursue esophageal manometric testing, including an assessment of symptomatology, results of other preoperative testing and the choice of surgical technique. A detailed history can elucidate symptoms concerning for esophageal dysmotility such as dysphagia or regurgitation. Presence of these symptoms can accentuate concern for an underlying disorder, but may also shed light into potential postoperative outcomes. Symptoms to consider include reflux, as was studied by Kavanaugh and colleagues who developed a protocol at their center requiring foregut testing for all bariatric surgical candidates with symptoms of reflux who were being evaluated for SG [12].
Notably, patients with morbid obesity and underlying esophageal disorders may not present with typical gastrointestinal symptoms. In fact, studies have raised concern that dysphagia symptoms are unreliable to identify underlying abnormal esophageal dysmotility in patients with morbidly obesity. Instead, for example, patients may experience respiratory symptoms as a manifestation of their underlying pathology, leading to a possible missed diagnosis preoperatively [13]. Additionally, the perception of esophageal symptoms may itself be altered in the setting of underlying obesity. The autonomic nervous system may be susceptible to obesity-induced perturbations, causing dysregulation of sensory pathways [14].
In rare cases, other preoperative testing such as upper endoscopy and barium esophagram may pick up esophageal motor changes that need to be confirmed on manometry, such as achalasia [8]. A meta-analysis of preoperative esophagogastroduodenoscopy before bariatric surgery did not recommend manometry to be performed routinely in asymptomatic average-risk patients, and did not find that a significant portion of patients had pathologic findings requiring referral for further manometric testing [15]. However, in patients for whom this testing is indicated, findings on upper endoscopy that could trigger the need for manometry include the presence of liquid stasis in the esophagus and a puckered tight LES. Similarly, although not routinely recommended, barium swallow can be included in preoperative work up. On barium swallow, discovery of a bird’s beak appearance, esophageal dilation, or severe peristaltic abnormality can reinforce the importance of diagnostic manometry prior to surgery.
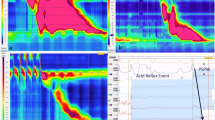
3.3 Bariatric Surgery and Esophageal Mechanics
In both patients with and without underlying esophageal dysmotility, bariatric surgery has been found to be associated with changes in esophageal mechanics. A number of prospective and retrospective cohort studies exist evaluating key preoperative esophageal characteristics that influence bariatric surgery outcomes as well as how bariatric surgery can influence esophageal motility. (Table 15.2) Unfortunately, there is a lack of large randomized controlled trials to better define the risks and benefits of each surgery in how it impacts esophageal function and how specific procedure techniques could be improved to lead to better outcomes. In this chapter we will focus on three most studied bariatric surgical procedures, laparoscopic adjustable gastric band (LAGB), sleeve gastrectomy (SG) and roux-en-Y gastric bypass (RYGB) and their associated changes in motility.
3.3.1 Laparoscopic Adjustable Gastric Band
The important question of how preoperative manometry influences outcomes in bariatric surgery has been studied mostly in LAGB patients. Lew and colleagues reviewed preoperative manometry data on 77 LAGB patients, finding that 18% of them had an abnormal manometry [29]. While abnormal baseline manometry did not appear to impact weight loss and reflux symptoms, severe postoperative emesis did occur in this patient group, with majority of these patients categorized as having either decreased or ineffective peristalsis. The clinical significance of altered LES pressure was studied by Suter et al., who looked at whether preoperative testing including manometry correlated with outcomes in 134 patients after LAGB surgery [30]. Their group found that patients with higher preoperative LES pressure were more likely to develop long reflux episodes and poor late food tolerance. In a retrospective analysis of 68 patients undergoing LABG, 44.3% were found to have an incompetent LES preoperatively [31]. LES incompetence was associated with a statistically significant increase in reoperation, leading the authors to recommend consideration of preoperative manometry before LAGB and standardization of this into their practice.
Klaus et al. conducted a prospective study of 164 patients with preoperative GERD symptoms undergoing LAGB, finding that patients who remained symptomatic after surgery (31.7%) were more likely to have poorer preoperative esophageal body motility and deterioration of LES relaxation after surgery [32]. Importantly, one third of postoperatively symptomatic patients developed esophageal dilatation following LAGB. Other groups have also demonstrated evidence of concerning esophageal dilatation after LAGB [11, 21]. A retrospective review of 121 patients one year post surgery revealed that 14% had esophageal dilatation on barium swallow [21]. This anatomic change was associated with increased emesis and reflux symptoms.
In the postoperative period, impairment of LES relaxation as well as weakened esophageal peristalsis have been found on multiple studies after LAGB [10, 17, 19, 20]. Tolone et al. performed high resolution manometry and pH testing pre- and post-operatively in 112 patients undergoing one of seven bariatric surgeries [16]. There was no difference in LES pressures before and after therapy for all bariatric procedures except for LAGB who experienced an increase in pressure. Furthermore, several LAGB patients developed pseudoachalasia syndrome postoperatively. A systematic review by de Jong and colleagues demonstrated that all but one patient experienced increase in LES pressure after surgery and most patients had decreased LES relaxation [17]. Furthermore, evidence of disturbed peristalsis was found in four out of six studies that had adequate data on manometry. In a prospective study of 43 LAGB patients esophageal body contractions weakened and there was a trend towards postoperative motility disorders, however the LES appeared unaffected by surgery [19]. This led the authors to recommend that manometry be performed routinely prior to LAGB. On the contrary, a small prospective study of LAGB and RYGB patients showed no effect of gastric reduction surgery on postoperative esophageal function, with 20 LAGB patients undergoing pre- and post-operative manometry [18]. This study was noted to have a smaller sample size compared to others, and notably of the LAGB patients only one had preoperative dysmotility and 18% had weak LES pressure, which likely influenced the result. Overall, the majority of studies suggest that preoperative dysmotility in LAGB patients is associated with increased adverse outcomes such as vomiting, reflux, and potential need for reoperation. Furthermore, LAGB placement in general appears to increase LES pressure, impair LES relaxation, and potentially disturbs peristalsis which can lead to esophageal stasis in patients with poor underlying motility and rarely to pseudoachalasia.
3.3.2 Sleeve Gastrectomy
Research to date is limited on the effects of sleeve gastrectomy on esophageal function. Studies demonstrate a trend towards delayed esophageal emptying and are inconsistent on changes to the lower esophageal sphincter [22, 23, 25, 33]. It is thought that the large variance may be due to the number of different surgical techniques available during sleeve creation.
A study of 73 patients undergoing SG described a significant decrease in LES pressures postoperatively, with the number of patients with LES hypotonia progressing from 8% to 32% after surgery [24]. The authors also found a significant decrease in the number of patients with normal peristalsis after surgery. Tolone et al. demonstrated that the frequency of ineffective peristalsis significantly increased in patients after sleeve gastrectomy, while not being significantly altered following other bariatric operations [16]. Patients after SG also had greater intragastric pressure and gastroesophageal pressure gradients compared to prior, leading to a large increase in esophageal acid exposure.
Braghetto and colleagues sought to describe changes in the LES after SG, studying 20 patients prospectively until 6 months after surgery [25]. They discovered that resting LES pressures reduced significantly postoperatively, with 85% of patients having an incompetent LES. A longer prospective study 13 months postoperatively showed no change in LES function, however there was a significant increase in ineffective peristalsis and incomplete bolus transit [23]. On the other hand, a small prospective study of 37 patients demonstrated a significant increase in LES pressure postoperatively, which the authors credited to their utilized surgical strategy [22]. Chiu and colleagues attempted to consolidate the available data on the effect of SG on GERD into consensus unsuccessfully, and while a similar effort has not been performed to date for esophageal function, it is clear that great variability in results exists between studies [34]. In summary, SG appears to alter esophageal function with a greater number of studies suggesting decreasing LES pressure and weakened peristalsis postoperatively; however, more objective data is needed to improve our understanding.
3.3.3 Roux-en-Y Gastric Bypass
Compared to other bariatric surgeries, RYGB has been found to lead to the least functional impairment of the LES and esophageal body. In a prospective study of multiple bariatric surgeries, the frequency of ineffective peristalsis and LES pressure was found to be unchanged before and after RYGB [16]. Three other small prospective studies demonstrated no LES dysfunction or change in motility pre- and post-operatively after RYGB [6, 18, 26]. Comparatively, a study of RYGB patients without GERD symptoms showed postoperatively no significant difference in all manometric variables except for peristalsis [27]. A different group looked at 20 patients after RYGB, describing that the percentage of patients with altered esophageal function diminished from 35% to 25% [28]. In this cohort, there was no observed change in basal LES pressure, but the amplitude of esophageal contractions decreased after RYGB. Overall, RYGB is found to have the least impact on LES function compared to LAGB and SG, and the majority of studies did not find a significant change in motility postoperatively.
4 Conclusions
Bariatric surgery has been found to impact esophageal function and may lead to esophageal motor impairment. The increased prevalence of esophageal motility disorders in patients with morbid obesity augments the importance of a thorough pre-operative evaluation. There is currently inadequate evidence for routine preoperative manometry testing in all patients undergoing bariatric surgery. However, for patients with concerning symptoms of an underlying esophageal motor disorder, manometry is a useful tool in the preoperative setting. In patients undergoing LAGB, the presence of preoperative abnormal peristalsis may increase adverse outcomes postoperatively. There is increasing evidence that preoperative esophageal manometry should be considered in patients undergoing SG given its effect on LES function and peristalsis, although larger and higher quality studies are needed in the future to define its benefit. RYGB appears to have the least amount of effect on esophageal motility and should be considered in patients with known esophageal motor disorders. However, bariatric surgery should always be performed with caution in patients with motility disorders.
5 A Personal View of the Data
Understanding the increased prevalence of esophageal dysmotility in morbid obesity, we perform a detailed review of any symptomatology that could reveal an underlying esophageal motor disorder and trigger the need for esophageal manometry testing in all patients undergoing a preoperative bariatric surgery evaluation. Symptoms are interpreted with caution as patients with morbid obesity may not present with typical symptoms and symptom perception itself may be altered in the setting of obesity. If manometry reveals a significantly hypotensive LES, RYGB may be considered over SG given that it is the least likely to lead to worsening reflux. LAGB is a rarely recommended treatment for morbid obesity, in part due to the significant rate of esophageal dysmotility and esophageal dilatation after LAGB. Future high quality studies are needed to improve our understanding of how underlying esophageal disorders can affect postoperative outcomes and of the effect of bariatric surgery on esophageal function.
6 Recommendations
-
1.
Use of esophageal manometry testing is not part of current clinical practice guidelines and is not routinely recommended as part of the pre-operative work-up for asymptomatic patients undergoing bariatric surgery (Evidence quality moderate; strong recommendation)
-
2.
If there is concern for preexisting esophageal dysmotility based on history, symptoms, upper endoscopy, or barium swallow, preoperative manometry testing should be strongly considered as it may influence the chosen surgical approach (Evidence quality moderate; moderate recommendation)
-
3.
Gastric bypass is favored over other surgical approaches in the setting of underlying esophageal dysmotility, as it appears to have the least amount of effect on esophageal motility (Evidence quality low, weak recommendation)
References
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures – 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2019;25(12):1346–59.
Nebel O, Castell DO. Inhibition of the lower oesophageal sphincter by fat: a mechanism for fatty food intolerance. Gut. 1973;14(4):270–4.
Jaffin B, Knoepflmacher P, Greenstein R. High prevalence of asymptomatic esophageal motility disorders among morbidly obese patients. Obes Surg. 1999;9(4):390–5.
Hong D, Khajanchee Y, Pereira N, Lockhart B, Patterson E, Swanstrom L. Manometric abnormalities and gastroesophageal reflux disease in the morbidly obese. Obes Surg. 2004;14(6):744–9.
Kristo I, Paireder M, Jomrich G, Felsenreich DM, Nikolic M, Langer FB, et al. Modern esophageal function testing and aastroesophageal reflux disease in morbidly obese patients. Obes Surg. 2019;29(11):3536–41.
Merrouche M, Sabate J, Jouet P, Harnois F, Scaringi S, Coffin B, et al. Gastro-esophageal reflux and esophageal motility disorders in morbidly obese patients before and after bariatric surgery. Obes Surg. 2007;17(7):894–900.
Mora F, Cassinello N, Mora M, Bosca M, Minguez M, Ortega J. Esophageal abnormalities in morbidly obese adult patients. Surg Obes Relat Dis. 2016;12(3):622–8.
Schneider R, Lazaridis I, Kraljevic M, Beglinger C, Wolnerhanssen B, Peterli R. The impact of preoperative investigations on the management of bariatric patients; results of a cohort of more than 1200 cases. Surg Obes Relat Dis. 2018;14(5):693–9.
Suter M, Dorta G, Giusti V, Calmes J. Gastroesophageal reflux and esophageal motility disorders in morbidly obese patients. Obes Surg. 2004;14(7):959–66.
Iovino P, Angrisani L, Tremolaterra F, Nirchio E, Ciannella M, Borrelli V, et al. Abnormal esophageal acid exposure is common in morbidly obese patients and improves after a successful lap-band system implantation. Surg Endosc. 2002;16(11):1631–5.
Huang L, Pimentel M, Rezaie A. Do Jackhammer contractions lead to achalasia? A longitudinal study. Neurogastroenterol Motil. 2017;29(3):e12953.
Kavanagh R, Smith J, Bashir U, Jones D, Avgenakis E, Nau P. Optimizing bariatric surgery outcomes: a novel preoperative protocol in a bariatric population with gastroesophageal reflux disease. Surg Endosc. 2019;34(4):1812–8.
Almogy G, Anthone G, Crookes P. Achalasia in the context of morbid obesity: a rare but important association. Obes Surg. 2003;13(6):896–900.
O'Brien PD, Hinder LM, Callaghan BC, Feldman EL. Neurological consequences of obesity. Lancet Neurol. 2017;16(6):465–77.
Bennett S, Gostimir M, Shorr R, Mallick R, Mamazza J, Neville A. The role of routine preoperative upper endoscopy in bariatric surgery: a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12(5):1116–25.
Tolone S, Savarino E, de Bortoli N, Frazzoni M, Frazzoni L, Savarino V, et al. Esophageal high-resolution manometry can unravel the mechanisms by which different bariatric techniques produce different reflux exposures. J Gastrointest Surg. 2019;24(1):1–7.
de Jong JR, Besselink MG, van Ramshorst B, Gooszen HG, Smout AJ. Effects of adjustable gastric banding on gastroesophageal reflux and esophageal motility: a systematic review. Obes Rev. 2010;11(4):297–305.
Korenkov M, Kohler L, Yucel N, Grass G, Sauerland S, Lempa M, et al. Esophageal motility and reflux symptoms before and after bariatric surgery. Obes Surg. 2002;12(1):72–6.
Suter M, Dorta G, Giusti V, Calmes J. Gastric banding interferes with esophageal motility and gastroesophageal reflux. Arch Surg. 2005;140(7):639–43.
Weiss H, Nehoda H, Labeck B, Peer-Kuehberger R, Oberwalder M, Aigner F, et al. Adjustable gastric and esophagogastric banding: a randomized clinical trial. Obes Surg. 2002;12(4):573–8.
Milone L, Daud A, Durak E, Olivero-Rivera L, Schrope B, Inabnet WB, et al. Esophageal dilation after laparoscopic adjustable gastric banding. Surg Endosc. 2008;22(6):1482–6.
Petersen WV, Meile T, Kuper MA, Zdichavsky M, Konigsrainer A, Schneider JH. Functional importance of laparoscopic sleeve gastrectomy for the lower esophageal sphincter in patients with morbid obesity. Obes Surg. 2012;22(3):360–6.
Del Genio G, Tolone S, Limongelli P, Brusciano L, D'Alessandro A, Docimo G, et al. Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg. 2014;24(1):71–7.
Valezi AC, Herbella FA, Mali-Junior J, Menezes MA, Liberatti M, Sato RO. Preoperative manometry for the selection of obese people candidate to sleeve gastrectomy. Arq Bras Cir Dig. 2017;30(3):222–4.
Braghetto I, Lanzarini E, Korn O, Valladares H, Molina JC, Henriquez A. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg. 2010;20(3):357–62.
Ortega J, Escudero MD, Mora F, Sala C, Flor B, Martinez-Valls J, et al. Outcome of esophageal function and 24-hour esophageal pH monitoring after vertical banded gastroplasty and roux-en-Y gastric bypass. Obes Surg. 2004;14(8):1086–94.
Valezi AC, Herbella FA, Junior JM, de Almeida Menezes M. Esophageal motility after laparoscopic roux-en-Y gastric bypass: the manometry should be preoperative examination Routine? Obes Surg. 2012;22(7):1050–4.
Mejia-Rivas MA, Herrera-Lopez A, Hernandez-Calleros J, Herrera MF, Valdovinos MA. Gastroesophageal reflux disease in morbid obesity: the effect of Roux-en-Y gastric bypass. Obes Surg. 2008;18(10):1217–24.
Lew JI, Daud A, DiGorgi MF, Olivero-Rivera L, Davis DG, Bessler M. Preoperative esophageal manometry and outcome of laparoscopic adjustable silicone gastric banding. Surg Endosc. 2006;20(8):1242–7.
Suter M, Giusti V, Calmes J, Paroz A. Preoperative upper gastrointestinal testing can help predicting long-term outcome after gastric banding for morbid obesity. Obes Surg. 2008;18(5):578–82.
Bueter M, Thalheimer A, le Roux CW, Wierlemann A, Seyfried F, Fein M. Upper gastrointestinal investigations before gastric banding. Surg Endosc. 2010;24(5):1025–30.
Klaus A, Gruber I, Wetscher G, Nehoda H, Aigner F, Peer R, et al. Prevalent esophageal body motility disorders underlie aggravation of GERD symptoms in morbidly obese patients following adjustable gastric banding. Arch Surg. 2006;141(3):247–51.
Tolone S, Savarino E, Yates RB. The impact of bariatric surgery on esophageal function. Ann N Y Acad Sci. 2016;1381(1):98–103.
Chiu S, Birch DW, Shi X, Sharma AM, Karmali S. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011;7(4):510–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lipowska, A.M. (2021). Manometry is Useful Prior to Bariatric Surgery. In: Alverdy, J., Vigneswaran, Y. (eds) Difficult Decisions in Bariatric Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-030-55329-6_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-55329-6_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-55328-9
Online ISBN: 978-3-030-55329-6
eBook Packages: MedicineMedicine (R0)