Abstract
Muscle strains account for about one-third of total sports-related injuries and about 20% of all practice injuries at the collegiate level, with nearly 50% occurring within the thigh. Risk factors typically include muscles that cross two joints and a high percentage of fast-twitch fibers. Acute muscle injury typically presents with acute muscular pain during eccentric loading of a strenuous activity. MRI is the recommended imaging modality when it is necessary to evaluate the severity of injury. Treatment strategies vary from conventional management with rest, ice, compression, nonsteroidal anti-inflammatory drugs, and physical therapy to more recent therapies with platelet-rich plasma and stem-cell therapies. Surgical management is also indicated for specific injuries depending on the location and severity of injury. Appropriate and timely management is essential to ensure prompt and safe return to play, a decision that is heavily based on restoration of strength and range of motion in order to prevent complications such as reinjury.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Epidemiology
American football is an extremely popular sport involving sudden bursts of maximal exertion, high-impact collisions, frequent direction changes, and intense training workloads. American football remains popular with more than 100,000 collegiate athletes and 1 million high school athletes [1]. At the collegiate level, the national estimate of athlete exposures exceeds 5 million [2]. American football remains one of the highest-risk sports for injuries. A surveillance of injuries from 2009–2010 through 2013–2014 estimated an average annual number of injuries of 47,199, accounting for an estimated injury rate per 1000 athlete exposures of 9.2 (9.0–9.4) (cdc mmw article). Injury surveillance shows that muscle strains are the third most common injury in competition, accounting for 12.1% of injuries, the second most common injury in scrimmages accounting for 15.7% of injuries, and the most common injury in regular practices accounting for 26% of injuries [3]. It is interesting to note that compared to all football injuries, which have high rates in competition, muscle strain injuries are more common in practice [3].
Second to strains, muscle contusions are the most frequent muscle injury. Current injury surveillance systems do not delineate muscle from soft tissue contusions, but it is well known that contusions account for a large proportion of injuries. NCAA data shows that contusions account for 16.3% of injuries in competition, 12.5% of injuries in scrimmage, and 10.1% of injuries in regular practice [3]. Epidemiological studies of high school football players demonstrate consistent data with contusions being the second most common injury, accounting for 12.7–15.9% of injuries [4].
Data regarding muscle injury in the NFL is similar to the reported high school and collegiate level. In a single NFL team, 46% of practice injuries were muscle strains [5]. Injuries to hamstring and quadriceps muscle account for 13% of all injuries among NFL players [5]. Surveillance of one NFL team over 10 years revealed a hamstring injury rate of 1.79 per 1000 athlete exposures for practices and 4.07 per 1000 athlete exposures for games [6].
Cumulatively, muscle strain and injuries account for 53–65% of all injuries sustained at high level of football participation [1]. The injury severity of muscle strains and contusions vary based on location. Lower-extremity injuries are the most common, accounting for approximately 28% of all injuries [1]. The burden of injury is varied based on the location. In a study of one NFL team’s training camp injuries, hamstring strains led to the most days lost at 8.3, second only to knee sprains. Additionally, both hip flexor strains (6.6 days) and quadricep strains (5.4 days) accounted for greater than 5 days missed [1]. Additional muscle injuries leading to lost days include lumbar strain (4.9 days), groin strain (4.8 days), Achilles strain (3.8 days), and contusions (3.2 days) [1].
Based on the frequency and burden of muscle injuries, timely and accurate diagnosis is important in order to promptly institute.
Etiology and Risk Factors
The underlying etiology of muscle injuries is multifactorial. As indicated by the incidence, certain muscles are more prone to injuries. Muscles at the highest risk of injury share common underlying characteristics. Muscles in which the origin crosses two joints are at increased risk of muscle injury [7]. The increased susceptibility to injury is due to the muscle’s activity on limiting range of motion of the joint they cross. Additionally, muscles that are used for rapid acceleration and quick movements have a higher percentage of type II fibers and are at increased risk of injury [7]. Since football mainly consists of these types of movements and plays, the incidence of muscle injuries is not surprising.
There are additional modifiable risk factors for muscle injuries that are important to identify. Inadequate preparation due to deconditioning, inadequate warm-up, fatigue, and dehydration are all important modifiable risk factors [8]. Specific lower-extremity muscle strains have been found to share similar risk factors. Previous injuries to hamstrings, quadriceps, and calf muscles, both recent (<8 weeks ago) and remote, are significant risk factors for repeat injury in the same, previously injured muscle [9]. Additionally, past calf injury has been implicated in muscle injuries to both the quadriceps muscles and hamstring muscles [9].
Biomechanics of Injury
Muscle injury typically occurs via two main mechanisms, either direct injury or indirect injury. Direct injury, including direct trauma to the muscle, causes compression against underlying bone which can lead to a spectrum of muscle injuries [MRI]. A three-stage clinical grading system has been defined categorizing contusions as mild, moderate, and severe [10]. Mild contusion consists of loss of range of motion of one-third normal motion, moderate contusion has a loss of range of motion by one-third to two-thirds normal motion, and severe contusion accounts for a greater than two-thirds loss of normal motion [10].
Indirect injury occurs through forcible stretching of muscle fibers. This stretching disrupts the normal architecture of muscle fibers. This most commonly occurs at the musculotendinous junction, which, in skeletally mature patients, is the weakest and most vulnerable site for muscle strain [11]. Muscle strain more commonly occurs during the eccentric phase of contraction when the muscle is lengthening as it contracts. The eccentric contraction generates greater forces than concentric contraction disrupting the normal connective tissue architecture and leading to injury [11].
No universal grading system for muscle strains has been developed. A three-stage grading system was originally described for the classification of quadriceps injury and has been adapted to classify injuries to other muscles. This original grading system describes a grade I injury as a tear of a few muscle fibers with the fascia remaining intact. Grade II injuries describe a tear of a moderate number of fibers without disrupting the fascia. Grade III injuries are a tear of many fibers with partial tearing of the fascia [12]. This initial grading system has been refined, with the most commonly used system incorporating loss of function. This grading system describes a grade I injury as a small tear with <5% loss of function, a grade II injury as a larger tear with 5–50% loss of function, and a grade III injury as >50% loss of function [10].
Clinical Evaluation
Obtaining a relevant clinical history is important in diagnosing acute muscle injuries. A typical history of muscle strain will involve an acute painful episode during an episode of intense exertion [11]. The history for a muscle contusion will typically include a history of a direct blow to the muscle. Not all acute injuries will cause cessation of activity. Ability to continue to participate is typically dependent on severity [11]. History should also focus on the listed risk factors above to help provide a complete clinical picture.
Physical examination of acute muscle injuries should include general inspection, range of motion, and strength. General inspection may reveal superficial ecchymosis and swelling. This is not always present as muscle contusions tend to occur at the muscle-bone interface [MRI]. In the setting of complete muscle tears, a palpable defect may be present. Less severe injuries may have less drastic physical exam findings. Range of motion and strength compared to the unaffected side are important physical exam findings to note. Depending on the severity of injury, range of motion may only be minimally affected. It is important to monitor for pain with active range of motion, especially in the eccentric phase. The affected side will demonstrate weakness compared to the unaffected side, more attributable to decreased central drive due to pain compared to actual muscle damage [11].
Imaging
Plain radiographs and computed tomography have only limited capability in evaluation of acute muscle injuries due to their general poor visualization of soft tissue. Subtle findings such as soft tissue swelling on plain radiographs may be present but has limited diagnostic utility. CT imaging may potentially show acute hemorrhage into injured muscles, but imaging of acute muscle injuries is better pursued through alternative modalities. Ultrasound and magnetic resonance imaging (MRI) are the typically preferred imaging modality due to their ability to detect and localize acute injuries.
Ultrasound
Prior to the development of MRI, ultrasound was the best available tool for evaluation of muscle injury [13]. Due to the clear disadvantage of user dependence, MRI has become more popular in the imaging of musculoskeletal disorders, including sports-related muscle injury [14]. However, due to increased availability and portability of ultrasound, as well as increased education on ultrasound, sonography has become increasingly popular in the evaluation of acute muscle injuries. Advantages of ultrasound compared to MRI include superior spatial resolution, cost, convenience, portability, dynamic evaluation of the injury, and the ability to perform simultaneous intervention [10, 14].
Identification of muscle contusions on ultrasound demonstrates an ill-defined area of hyperechogenicity [10]. Comparison with contralateral muscles of similar location can be useful in identifying the general hyperechoic nature of a contused muscle. In the acute phase of the injury, the area of injury within the muscle may be isoechoic with adjacent unaffected muscle [15]. In the setting of significant direct trauma, muscle hematoma is likely. On ultrasound, this is identified as a hypoechoic fluid collection surrounded by irregular muscle fibers. In the first 24–48 hours, the muscle tissue surrounding the fluid collection may have increased reflectivity, but after 48–72 hours, the hematoma organizes demonstrating a clear echogenic margin [10]. Because of this, the ideal timing of initial ultrasound examination is between 2 and 48 hours [13].
In the evaluation of indirect muscle injuries, ultrasound has been proven to be equivalent to MRI in the sensitivity of detection of acute muscle injury [16]. A three-stage grading system for identification of muscle strain injury has been well established [13]. Grade I injury can be normal on ultrasound or can demonstrate focal or general areas of increased echogenicity involving <5% of the muscle substance [13]. Grade II injury involves a disruption of >5% but <100% of muscle fibers on a cross-sectional view and typically is accompanied by an intramuscular fluid collection [13]. In a grade III injury, or a complete rupture, there is complete discontinuity of the muscle at the musculotendinous junction with the presence of intermuscular and perifascial fluid as well as hyperechogenicity of surrounding muscle [10].
In addition to acute evaluation of suspected muscle injuries, ultrasound can be used to dynamically guide therapeutic interventions. Ultrasound-guided hematoma evacuation allows for increased accuracy and needle placement to minimize procedural pain. Ultrasound-guided needle placement is useful to ensure appropriate site delivery of biologics which have shown a recent increased role in treatment of muscle injuries.
Additionally, recent data has suggested sonography as a tool to guide clinical progression and reduce recurrent rate of thigh muscle strains. A muscle injury return to play protocol has been proposed to use ultrasound, not only in the initial diagnostic setting but also once an athlete has rehabbed to 80% of speed/power to evaluate the presence of residual hematoma, lack of functional contraction, or presence of hyperemia. High-risk ultrasound findings at 80% speed/power including residual hematoma or lack of functional contraction would prevent an athlete from progressing, mitigating risk for reinjury. Presence of persistent hyperemia is only considered an intermediate risk factor allowing an athlete to progress slowly under careful supervision. The development of this protocol was admittedly based on experiential data and the authors acknowledge the need for a prospective study to validate this approach [14].
Magnetic Resonance Imaging
Used in increasing frequency for muscular injuries, MRI provides excellent lesion detection and localization of injury [10]. MRI has been shown to have high-contrast resolution, high sensitivity, and the ability to image in multiple planes. MRI is the imaging modality of choice to confirm and evaluate the extent and severity of injury [16]. MRI imaging protocols vary from institution to institution. Necessary imaging sequences should include a fat-suppressed fluid-sensitive sequence, such as a short tau inversion recovery (STIR), fat-saturated proton density-weighted imaging, or T2-weighted imaging [10, 17]. These images are more sensitive for the identification of muscle edema or hemorrhage [10].
In the identification of muscle contusions and hematomas, there is a characteristic feather-like high signal with the muscle on fat-suppressed fluid-sensitive sequences. There is diffusely high signal present on fluid-sensitive sequences of images obtained after 48 hours after acute injury. Grading of muscle strain injury on MRI follows the general principles outlined above in clinical grading and imaging with ultrasound. Grade I strains, as shown in Fig. 6.1, demonstrate increased signal on fluid-sensitive sequences due to edema in the muscle as well as potential perifascial fluid. The hallmark of grade I strains include the lack of significant disruption of muscle architect, <5% on cross-sectional area. Grade II strains demonstrate a distortion of normal muscle architecture with associated muscular hematoma. Grade III strains demonstrate complete disruption of the musculotendinous junction with accumulation of hematoma between the two [10].
Recent reviews have looked to assess the prognostic ability of MRI in determining reinjury risk as well as identifying predictors for return to play and performance [17, 18]. Based on current evidence, there is no strong evidence for any MRI findings at the time of injury or at the time of return to play as a predictor for hamstring reinjury risk [18]. There is, however, moderate evidence that intratendinous injuries on MRI at the time of injury are associated with higher reinjury risk [18].
In the evaluation of predicting return to play of calf muscle injuries, more extensive involvement of connective tissue is associated with prolonged time to return to play [19]. Current evidence indicates that injuries involving large muscle volume, length, or surface as well as those with central tendon involvement result in a longer return to play [17]. A study specifically on football players who do not have MR evidence of injury but only clinical findings (those with grade 0 to grade I injuries) shows a shorter period of return to play. Unfortunately, there is limited evidence on MRI factors on predicting return to play in grade II–III muscle injuries [17].
Treatment
As noted above, acute muscle injuries can lead to prolonged loss of football participation. Minor injuries can be healed in 1 week but more severe injuries can require 4–8 weeks of healing [11]. Because of this potential for prolonged healing, the identification and utilization of proper treatment modalities are important to try and maximize an athlete’s in-season participation. Additionally, it is important to utilize proper therapy in order to ensure adequate healing to prevent repeat injury. One study showed that recurrent or repeat injuries are more severe than the initial injury and cause the most time lost from sports participation [20].
Acute management with relative immobilization, rest, ice, compression, and elevation have been utilized as the initial treatment modalities based mostly on experiential data without significant clinical studies. Despite logical and physiological basis for their use, there is no significant scientific evidence for these initial treatment modalities.
RICE – Rest, Ice, Compression, and Elevation
The concept of rest after an acute muscle injury promotes pain control. A brief period of relative immobilization should be utilized to allow scar tissue to begin forming connections between the injured muscle fibers. Prolonged immobilization, however, leads to decreased muscle volume, structure, and function with re-organization of sarcomeres [7]. Clinical studies have shown a 20% decrease in muscle strength after only 1 week of immobilization [7]. Additionally, a high incidence of myositis ossificans has been demonstrated with prolonged immobilization [21]. Conversely, mobilization of the injured muscle too early does not allow adequate scar formation to provide the scaffolding for muscle healing and increases the risk of repeat injury [22].
Ideally, relative immobilization and rest for less than 1 week should be employed and gradual return to submaximal activity and motion should be initiated, limited on the basis of pain. Injuries to the lower extremity should be supported with crutches for limited to non-weight-bearing during the time of rest. After this brief period of immobilization, supervised, cautious active mobility should be started. It has been shown that early tensile loading stimulates collagen fiber growth and realignment and early mobilization promotes decreased muscle adhesion formation and more rapid recovery of proprioception [7].
In addition to early immobilization and relative rest, cryotherapy, or the application of ice, plays an important role in the management of muscle injuries. There has been controversy on the true physiologic effect of cryotherapy. Studies have shown that the application of ice to below 15 °C leads to increased permeability causing increased swelling [7]. Additional studies have shown that cryotherapy leads to vasoconstriction with decreased transient perfusion but without long-term changes on muscular microcirculation [23]. In addition, several studies have looked at the role of cryotherapy on inflammation without development of a consensus. Some studies have shown that ice decreases inflammation while other studies have demonstrated an increase in inflammation with ice [7]. Despite this controversy on the effect of cryotherapy on swelling and inflammation, application of ice has been consistently shown to provide an analgesic effect. This analgesic effect can be helpful for early mobilization of the injured extremity to allow for participation in early rehab. Due to its simplicity and relative low risk of treatment, as well as its analgesic benefit, cryotherapy in the initial phase of treatment is still recommended and a mainstay of muscle injury treatment.
Compression and elevation are mainstays of treatment of many, if not all, musculoskeletal injuries. In the setting of acute muscle injuries, it is thought that the application of compression leads to decreased hematoma formation and promotes hematoma reabsorption. This has not been systematically studied but does have logical and physiologic basis for use. Studies have proven decreased muscular blood flow with compression but no sound evidence relating this to accelerated healing [24]. Compression with cryotherapy compared to cryotherapy alone has shown benefit in improved pain control in patients post-ACL reconstruction, but no studies have been performed in the evaluation of muscle injuries. The low risk of harm, the simplicity of the intervention, and the understanding of the benefits of compression make compression an important treatment intervention in the management of acute muscle injury.
Physical Therapy
As previously discussed, a limited period of immobilization with relative early motion is optimal for muscle injury recovery. Early rehabilitation has been shown to be crucial for a faster clinical recovery to sports [25]. One study in recreational athletes with lower-extremity muscle strains demonstrated a decreased return to sport interval by 3 weeks in a group starting rehabilitation at 2 days post injury compared to 9 days post injury [25]. The overall goals of physical therapy are to promote healing, restore full range of motion and strength, and prepare for return to sports specific training. Typically, rehab has focused on four main stages static stretching, isometric loading, dynamic loading with increased resistance, and functional exercises combined with heavy strength training [25].
Therapy protocols can typically be divided into five phases: phase I or the acute phase, phase II or the subacute phase, phase III or the remodeling phase, phase IV or the functional phase, and phase V which is return to competition. The duration in each stage is variable. The acute phase focuses on RICE therapy as discussed above and is utilized for approximately 1–7 days until signs of inflammation begin to resolve. The subacute phase can begin when swelling and pain begin to resolve or improve. This phase focuses on the return of full range of motion and, once without pain, can progress to regular concentric strength exercises. Submaximal isometric contraction is utilized in this phase and begins at 3 days to >3 weeks of injury. The remodeling phase is when hamstring stretching can begin and occurs at 1–6 weeks after injury during severity. During this phase, range of motion needs to be pain-free and the focus is on strengthening and flexibility. Frequent daily stretching at this phase has been shown to regain full range of motion and have a decreased total rehabilitation program. In this third phase of therapy, eccentric exercises can be performed. The functional phase of rehab occurs at 2 weeks to 6 months after injury with the goal to return to sport. Further increases in hamstring flexibility and strength are developed to reach normal values. In this stage, a progression from pain-free jogging to sprinting is utilized. Phase V, return to competition, typically occurs at 3 weeks to 6 months and focuses on maintaining strength and flexibility to prevent reinjury [26].
In addition to these injury location specific exercises, data has shown the importance of programs focused on trunk stabilization and progressive agility training [27]. Programs focused on trunk stabilization and progressive agility training have been shown to be more effective in promoting return to sports and preventing reinjury in hamstring injuries [27]. Thus, rehab that incorporates trunk stabilization and progressive agility training should be an important part of treatment.
Pharmacologic Treatment
Inflammation is an important factor in the setting of acute muscle injuries. It is thought that inflammation produces signals that trigger the healing cascade. However, it is well known that inflammation can be a contributing factor to pain. Management with anti-inflammatories is a reasonable treatment option. There have been few randomized control trials looking at the use of both nonsteroidal anti-inflammatories (NSAIDs) and glucocorticoids in the treatment of muscle injuries [22].
NSAIDs are commonly used in acute muscle injuries. A systematic review of the literature in human studies shows that acute use of NSAIDs can improve the recovery from acute muscle injury by reducing strength loss, soreness, and blood CK level [28]. Additionally, in experimental models, short-term use of NSAIDs has been demonstrated to decrease the inflammatory cell reaction without adverse effects on the healing process, tensile strength, ability of the injured muscle to contract, or myofiber regeneration [22]. Experimental data in animal models suggest that NSAID administration may have adverse effects in the healing of acute muscle injuries; however, there is no evidence to suggest such effects in human studies [28]. Based on this data, it is therefore reasonable to utilize NSAIDs both in the acute management of acute muscle injuries to decrease acute inflammation and throughout the rehabilitation process in an as needed fashion.
Corticosteroid use in acute injury seems to have negative effects in the healing process of acute muscle injuries. A study of systemic corticosteroids has shown initial benefit in muscle injury with decreased initial inflammation and increased force generating capacity but, in later effects, included delayed clearing of necrotic tissue and normal healing response as well as delayed muscle regeneration [21]. Intramuscular corticosteroid injection has also not been well studied. A retrospective study without objective results did demonstrate that in NFL athletes with hamstring strains, corticosteroids did not produce any adverse effects [29]. This study only highlights the potential safety of intra-injury injections but is unable to draw any conclusions regarding efficacy. At this time, the body of evidence supporting corticosteroid use for acute muscle injuries is insufficient.
Platelet-Rich Plasma Therapy
An evolving therapeutic modality, platelet-rich plasma (PRP) therapy, has an exciting potential for treatment of acute muscle injuries to expedite the healing process. Animal model studies have theorized that the abundance of growth factors and cytokines in PRP induces cell proliferation and migration, increases angiogenesis, and enhances muscle tissue regeneration [30,31,32]. A systematic review by Kunze et al. evaluated 21 studies looking at the basic science effects of PRP in vitro and in vivo models [33]. The review of these basic science studies shows that PRP treatment leads to an increased myocyte proliferation, growth factor expression, leukocyte recruitment, and angiogenesis in muscle model which demonstrates that PRP has the potential to serve as an effective treatment modality to expedite healing of the muscular pathology [33].
Clinical studies, however, have shown conflicting results. A systematic review by Grassi et al. evaluated eight randomized control trials using PRP for muscle injuries. Significant study outcomes for PRP treatment included return to sport, reinjuries, pain, strength, and complications. Of the reviewed studies reporting each outcome, there was no significant difference in reinjury, reported complications, and strength. Conflicting results for pain were reported with three studies reporting better pain outcomes with PRP compared to control and two studies demonstrating no difference. Most interestingly, across six reviewed studies, a random-effect meta-analysis revealed a significant mean difference −7.17 days in favor of PRP. This effect was noted to be not statistically significant when comparing the data from the only two double-blinded studies [34].
While promising basic science evidence exists for the use of PRP for muscle injuries, clinical application lacks robust evidence. The difficulty with extrapolating PRP research into clinical practice is multifactorial. First, the term PRP has a wide definition across the literature in regard to formulation including preparation and contents. Oftentimes, studies either fail to report the preparation and composition of their PRP or they are not an easily reproducible formulation making translation to clinical utility difficult. Additionally, current clinical research is underpowered. While RTP was able to demonstrate a significantly improved time to return, the overall quality of this evidence according to the grade guidelines was reported as low due the limited number of studies and their biases [34].
As PRP continues to be studied, there may be an increase in evidence for its clinical utility. Despite observed anecdotal success, the evidence recommending treatment of muscle injuries with PRP is considered low quality.
Surgical Management
While muscle injuries continue to plague the sport of football, early identification and severity of injury remain critical to the safe return of play of the athlete. Early evaluation in terms of mechanism of injury, physical exam, and imaging including possible ultrasound, CAT scans, and/or an MRI may be necessary to qualify an injury and determine timing for a safe return to play. The interpretation of results is key to not only determine a safe return to play but also minimize the risk of reinjury. Given the difficulty in qualifying muscle injuries as well as the inherent pressure from athletes and the coaching staff to return to play, we will continue to see muscle injuries near the top of our injury lists.
While the majority of muscle injuries can be managed adequately with conservative treatments there are occasions where surgical interventions may have to be considered. There is no consensus as to when a surgical approach should be implemented; however, most common seem to be centered around an intra/intermuscular hematoma and/or the development of subsequent compartment syndrome. Reports of primary repair of muscle fibers are rare and technically challenging. Myositis ossificans is a late complication of muscle injury may also result in surgical necessity.
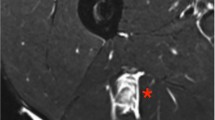
Muscle injuries resulting in hematoma formation can occur with either a direct trauma or contusion or indirectly following a tear of muscle fibers most commonly during an eccentric load to the muscle fibers. The resulting localized bleeding can form a hematoma as demonstrated in Fig. 6.2 below. They also generate increased pressure in the area. Early evaluation at the time of injury is typically characterized by a sensation of a “pop” by the athletes as well as an immediate termination of activity and disability requiring assisted mobilization. Physical exam may result in a palpable defect and then inability to sustain a contraction of the involved muscle group. High grade II (partial tear) or grade III (complete tear) are at risk for bleeding and hematoma formation [35, 36]. Repeat injury to a muscle that was previously considered a lower grade injury is also at great risk. Hematoma formation should be considered in an extremity with increasing girth of the extremity over the first 24 hours as well as increasing pain. Further imaging may be necessary if this level of disability exists.
The prognosis of muscular hematoma is generally good; however, poor prognosis indicators include the increasing size and fluctuating muscle swelling after 24 hours, persistent swelling after 48–72 hours, increasing pain intensity, extension of tenderness from the site of injury, and/or persistent restricted motion of the limb involved [37].
In the event of worsening symptoms, surgical hematoma decompression should be considered. Operative drainage of the hematoma can typically be done with a small incision, therefore minimizing the chance for further or recurrent bleeding (Fig. 6.3). CT or MRI of the extremity can be helpful in determining the best surgical approach. While there is no specific rule to the timing of surgical intervention, allowing the bleeding to stabilize prior to surgical intervention would be optimal. In the event the athlete developed increasing pain, diminished pulses, and/or paresthesia, a development compartment syndrome should be considered. Surgical intervention in this setting should be considered immediate and may also require a compartment release fasciotomy.
Myositis ossificans can be a serious and painful complication after muscle injury. The offending injury can occur from a single blow to the extremity or repeated lower-level injuries to the same area. The periosteal calcifications within the muscle can be diagnosed on serial X-rays usually seen 4–6 weeks after the injury. Athletes typically experience moderate tenderness, swelling, loss of motion, and palpable hardening of the tissues in the area [38]. While typically myositis ossificans is managed conservatively, some athletes develop permanent limitations of motion, persistent pain, and loss of function. These athletes may require surgical intervention to remove the bone. Surgery is not typically attempted prior to 4–6 months after the offending injury to allow for complete maturation of the excess bone in order to minimize recurrence [39].
References
Feeley BT, Kennelly S, Barnes RP, Muller MS, Kelly BT, Rodeo SA, et al. Epidemiology of national football league training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597–603.
Kerr ZY, Marshall SW, Dompier TP, Corlette J, Klossner DA, Gilchrist J. College sports-related injuries - United States, 2009-2010 through 2013-14 academic years. MMWR Morb Mortal Wkly Rep. 2015;64(48):1330–6.
Kerr ZY, Simon JE, Grooms DR, Roos KG, Cohen RP, Dompier TP. Epidemiology of football injuries in the national collegiate athletic association, 2004-2005 to 2008-2009. Orthop J Sports Med. 2016;4(9):232596711666450.
Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204.
Lawrence DW, Hutchison MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the national football league, 2012-2014. Orthop J Sports Med. 2015;3(5):232596711558365.
Elliott MCCW, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843–50.
Noonan TJ, Garrett WE. Muscle strain injury: diagnosis and treatment. J Am Acad Orthop Surg. 1999;7(4):262–9.
Arner JW, McClincy MP, Bradley JP. Hamstring injuries in athletes: evidence-based treatment. J Am Acad Orthop Surg. 2019;27(23):868–77.
Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300–3.
Lee JC, Mitchell AWM, Healy JC. Imaging of muscle injury in the elite athlete. BJR. 2012;85(1016):1173–85.
Garrett WE. Muscle strain injuries: clinical and basic aspects. Med Sci Sports Exerc. 1990;22(3):436–43.
Ryan AJ. Quadriceps strain, rupture, and charlie horse. Med Sci Sports. 1969;1(2):106–11.
Peetrons P. Ultrasound of muscles. Eur Radiol. 2002 Jan;12(1):35–43.
Hall MM. Return to play after thigh muscle injury: utility of serial ultrasound in guiding clinical progression. Curr Sports Med Rep. 2018;17(9):296–301.
Aspelin P, Ekberg O, Thorsson O, Wilhelmsson M, Westlin N. Ultrasound examination of soft tissue injury of the lower limb in athletes. Am J Sports Med. 1992;20(5):601–3.
Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. Am J Roentgenol. 2004;183(4):975–84.
Kumaravel M, Bawa P, Murai N. Magnetic resonance imaging of muscle injury in elite American football players: predictors for return to play and performance. Eur J Radiol. 2018;108:155–64.
van Heumen M, Tol JL, de Vos R-J, Moen MH, Weir A, Orchard J, et al. The prognostic value of MRI in determining reinjury risk following acute hamstring injury: a systematic review. Br J Sports Med. 2017;51(18):1355–63.
Prakash A, Entwisle T, Schneider M, Brukner P, Connell D. Connective tissue injury in calf muscle tears and return to play: MRI correlation. Br J Sports Med. 2018;52(14):929–33.
Brooks JHM, Fuller CW, Kemp SPT, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297–306.
Beiner JM, Jokl P. Muscle contusion injuries: current treatment options. J Am Acad Orthop Surg. 2001;9(4):227–37.
Järvinen TAH, Järvinen TLN, Kääriäinen M, Äärimaa V, Vaittinen S, Kalimo H, et al. Muscle injuries: optimising recovery. Best Pract Res Clin Rheumatol. 2007;21(2):317–31.
Smith TL, Curl WW, George C, Rosencrance E. Effects of contusion and cryotherapy on microvascular perfusion in rat dorsal skeletal muscle. Pathophysiology. 1994;1(4):229–33.
Thorsson O, Lilja B, Nilsson P, Westlin N. Immediate external compression in the management of an acute muscle injury. Scand J Med Sci Sports. 2007;7(3):182–90.
Bayer ML, Magnusson SP, Kjaer M. Early versus delayed rehabilitation after acute muscle injury. N Engl J Med. 2017;377(13):1300–1.
Petersen J. Evidence based prevention of hamstring injuries in sport. Br J Sports Med. 2005;39(6):319–23.
Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):10.
Morelli KM, Brown LB, Warren GL. Effect of NSAIDs on recovery from acute skeletal muscle injury: a systematic review and meta-analysis. Am J Sports Med. 2018;46(1):224–33.
Levine WN, Bergfeld JA, Tessendorf W, Moorman CT. Intramuscular corticosteroid injection for hamstring injuries: a 13-year experience in the national football league. Am J Sports Med. 2000;28(3):297–300.
Hammond JW, Hinton RY, Curl LA, Muriel JM, Lovering RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009;37:1135–42.
Mazzocca AD, McCarthy MB, Chowaniec DM, Dugdale EM, Hansen D, Cote MP, Bradley JP, Romeo AA, Arciero RA, Beitzel K. The positive effects of different platelet-rich plasma methods on human muscle, bone, and tendon cells. Am J Sports Med. 2012;40:1742–9.
Quarteiro ML, Tognini JR, de Oliveira EL, Silveira I. The effect of platelet-rich plasma on the repair of muscle injuries in rats. Rev Bras Ortop. 2015;50:586–95.
Nunze KN, Hannon CP, Fialkoff JD, Frank RM, Cole BJ. Platelet-rich plasma for muscle injuries: a systematic review of the basic science literature. World J Orthop. 2019;10(7):278–91.
Grassi A, Napoli G, Romandini I, Samuelsson K, Zaffagnini S, Candrian C, Filardo G. Is Platelet-Rich Plasma (PRP) effective in the treatment of acute muscle injuries? A systematic review and meta-analysis. Sports Med. 2018;48:971–89.
Almakinders LC. Results of surgical repair versus splinting of experimentally transected muscle. J Orthop Trauma. 1991;5:173–6.
Kujala UM, Orava S, Jarvinen M. Hamstring injuries: current trends in treatment and prevention. Sports Med. 1997;23:397–404.
Klein JH. Muscular hematomas: diagnosis and management. J Manipulativ Physio Ther. 1990;13:96–100.
Larson CM, Almakinders KSG, Garrett WE. Evaluating and managing muscle contusions and myositis ossificans. Phys Sports Med. 2002;30:41–50.
Miller AE, Davis BA, Beckley OA. Bilateral an recurrent myositis ossificans in an athlete: a case report and review of treatment options. Arch Phys Med Rehabil. 2006;87:286–90.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Guy, J., Wagner, A. (2021). Muscle Strains in Football. In: Farmer, K.W. (eds) Football Injuries. Springer, Cham. https://doi.org/10.1007/978-3-030-54875-9_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-54875-9_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-54874-2
Online ISBN: 978-3-030-54875-9
eBook Packages: MedicineMedicine (R0)