Abstract
The branchial arches are the embryological precursors of the face, neck, and pharynx. Anomalies of the branchial arches are the second most common congenital lesions of the head and neck in children, with second branchial arch anomalies by far the most common. Clinically, these congenital anomalies may present as cysts, sinus tracts, fistulae, or cartilaginous remnants with typical clinical and radiological findings. We review the normal embryological development of the branchial arches and the anatomical structures of the head and neck that derive from each arch. The typical clinical and radiological appearances of both common and uncommon branchial arch abnormalities are discussed with an emphasis on branchial cleft anomalies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Anomalies of the branchial arches usually present as cysts, sinuses, or fistulae.
-
Second branchial arch anomalies account for approximately 95% of cases.
-
There are no pathognomonic imaging features, so diagnosis depends on a high index of suspicion and knowledge of typical locations.
-
Persistent cysts, fistulae, or recurrent localized infection may be due to branchial arch anomalies.
-
Surgical excision of the cyst or tract is the most common curative option.
-
•The most common is a second branchial system anomaly with persistence of both cleft and pouch.
1 Introduction
The branchial arches represent the embryological precursors of the face, neck, and pharynx. Anomalies of the branchial arches are the second most common congenital lesions of the head and neck in children. They may present as cysts, sinus tracts, fistulae, or cartilaginous remnants and present with typical clinical and radiological patterns dependent on which arch is involved. The embryological development of the branchial arches is reviewed and the radiological appearance of branchial arch abnormalities is presented, primarily focusing on branchial cleft anomalies.
2 Presentation
-
The male:female ratio is 3:2.
-
The peak age is the third decade.
-
2/3 are left-sided.
-
2/3 lie anterior to upper sternocleidomastoid.
-
80% present as persistent swelling, 20% are fluctuant.
-
FNA—straw-colored fluid containing cholesterol.
-
30% present with pain.
-
15% present with infection.
-
70% are clinically cystic; 30% feel solid.
3 Investigations
-
FNA.
-
U/S, MRI, or CT—can delineate extent of mass but cannot easily differentiate from a metastatic squamous cell carcinoma lymph node that has undergone cystic degeneration.
4 Differential Diagnosis
-
Benign lymph node.
-
Metastatic lymph node.
-
Branchiogenic carcinoma.
5 Classification
-
A cyst is an epithelium-lined structure without an external opening.
-
A sinus is a blind tract with an opening either externally through the skin (representing persistence of a branchial cleft) or internally into the foregut (representing persistence of a branchial pouch).
-
A fistula is a tract that communicates between the skin externally and the foregut internally and therefore represents persistence of a connection between a branchial cleft and its corresponding pouch.
6 Developmental Anatomy
-
The most typical feature of the head and neck in an early embryo is the series of branchial arches that begin to develop during the fourth week of gestation and give the embryo its characteristic external appearance.
-
Four well-defined pairs of arches appear, while the fifth and sixth are believed to be rudimentary.
-
The arches are separated from each other on the external surface of the embryo by ectodermal clefts, and internally within the pharynx by endodermal pouches.
-
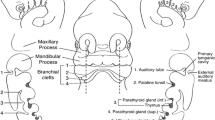
Each arch contains a cartilaginous rod (which forms the skeleton of the arch), a muscular component, a nerve, and an artery (Fig. 57.1).
-
During the fifth week of gestation, the ventral aspect of the second arch grows caudally to overlap the third and fourth arches resulting in the formation of the cervical sinus. This sinus then usually disappears by the 7th week, giving the neck a smooth contour.
-
The first pouch and cleft become closely related and ultimately form much of the middle ear, mastoid, and eustachian tube.
-
The second pouch remains in part as the tonsillar fossa.
-
The third pouch contributes to the thyroid gland and inferior parathyroid, and the fourth to the superior parathyroid gland.
-
The external ear begins to develop at week 6 of gestation in the form of three otic folds or hillocks on the first arch and three on the second arch. These ultimately fuse to form the developing auricle.
-
The thyroid gland appears as an epithelial proliferation in the floor of the pharynx at a point later indicated by the foramen caecum. The thyroid gland then descends down in front of the pharyngeal gut as a bi-lobed diverticulum. During this migration, the gland remains connected to the tongue by a narrow canal called the thyroglossal duct. By the end of the 7th week, the thyroid has reached its final destination anterior to the trachea; the duct involutes and disappears with time. The thyroid gland begins to function at approximately the end of the 3rd month.
7 The Branchial Arches and Their Derivatives
There are six pharyngeal arches, the fifth does not contribute any useful structures and often fuses with the sixth arch.
8 Derivatives of the Pouches
-
Each pouch has a ventral and a dorsal wing. The fourth pouch has an additional accessory wing. The endodermal lining of the pouches proliferates into glandular organs (Table 57.1).
-
First pouch: Dorsal and ventral: Middle ear cavity.
-
Second pouch: Dorsal: Middle ear cavity. Ventral: Tonsillar fossa and palatine tonsil.
-
Third pouch: Dorsal: Parathyroid. Ventral: Thymus.
-
Fourth pouch: Dorsal: Parathyroid. Ventral: Accessory: Ultimobranchial body.
9 Classification
-
Branchial cleft cysts fall into three categories: first, second, and third branchial cleft anomalies (Fig. 57.2).
9.1 First Branchial Cleft Anomalies
-
First branchial cleft anomalies make up less than 1% of all branchiogenic anomalies and usually appear on the face or near the auricle. There are two types of first branchial anomalies, Type I and Type II.
-
Type I—Type I first branchial cleft cysts are duplication anomalies of the external canal and are composed of ectodermally derived tissue. They may pass into the parotid gland and close to the facial nerve.
-
Type II—Type II anomalies may comprise ectodermally and mesodermally derived tissues. These lesions typically present below the angle of the mandible, pass through the parotid gland in close proximity to the facial nerve, and end either inferior to the external auditory canal or into the canal at the bony cartilaginous junction (Figs. 57.3 and 57.4).
-
9.2 Second Branchial Cleft Anomalies
-
Second branchial cleft anomalies are the most common of the three types.
-
They present as discrete, rounded masses below the angle of the mandible and at the anterior border of the sternocleidomastoid muscle.
-
The potential tract of an associated sinus passes deep to the second arch structures (e.g., the external carotid artery and the stylohyoid and digastric muscles) and superficial to the third arch derivatives (e.g., the internal carotid artery), opening into the tonsillar fossa (Figs. 57.5 and 57.6).
-
Operative Notes Take an ellipse of skin around the tract and start dissecting in a cephalad direction. Then perform further stepladder incisions to follow the tract, taking care that it may course over the hypoglossal and glossopharyngeal nerves, and between the internal and external carotid vessels. Tonsillectomy may be required for internal tract closure.
9.3 Third Branchial Cleft Anomalies
-
Third branchial cleft cysts present anterior to the sternocleidomastoid muscle and lower in the neck than either first or second branchial cleft anomalies.
-
Third branchial cleft cysts are deep to the third arch derivatives (e.g., the glossopharyngeal nerve and the internal carotid artery) and superficial to fourth arch derivatives (e.g., the vagus nerve).
-
These anomalies end in the pharynx at the thyrohyoid membrane or pyriform sinus.
10 Thymic Cysts/Ectopic Thymic Tissue
-
These represent third branchial pouch anomalies.
-
They tend to present in first decade of life as a mass in the left paramedian position.
-
Treatment is surgical excision in similar fashion as third/fourth branchial system anomalies.
10.1 Treatment
-
The management of branchial cleft anomalies is initial control of the infection followed by surgical excision of the cyst and tract.
-
As a general rule, incision and drainage procedures should be avoided; however, they may be necessary for acute abscess treatment before definitive excision. Placement of the drainage incision should be determined with the need to excise the scar with definitive surgery.
-
Needle aspiration and decompression can be beneficial in preventing incision and drainage, which increases the difficulty of definitive excision.
11 Thyroglossal Duct Cyst
-
Thyroglossal duct cysts account for around 70% of congenital abnormalities in the head and neck region.
-
Persistent ducts and cysts occur because of a failure of the thyroglossal duct to involute between the 8th and 10th week of gestation and a cyst can therefore occur anywhere along the duct’s natural course from the foramen caecum to the thyroid gland.
-
The duct assumes an intimate anatomical association with the hyoid bone, and in approximately 30% of cases, a tract has been found posterior to this structure.
11.1 Presentation
-
They most commonly present in the first two decades of life.
-
Cysts usually appear as a midline cervical mass and lie in close proximity to the hyoid bone.
-
Patients can present with a smooth, cystic swelling in the midline of the neck, which moves on swallowing and tongue protrusion.
-
Thyroglossal duct cysts can become infected, resulting in a red, painful midline swelling, which can discharge (Figs. 57.7 and 57.8).
11.2 Investigations
-
An ultrasound examination should be performed to establish the presence of a cystic structure in the neck and to confirm that there is a separate and normal-looking thyroid gland.
-
This will prevent the rare possibility of inadvertent removal of an ectopic thyroid gland resulting in post-operative hypothyroidism.
11.3 Treatment
-
A Sistrunk’s procedure is the treatment of choice.
-
This is performed through a horizontal skin crease incision at the approximate level of the hyoid bone, taking a skin ellipse around any discharging sinus.
-
The cyst and its associated tract are then dissected out in continuity with the middle portion of the hyoid bone and a wedge of muscle superior to the hyoid bone extending up to the foramen caecum.
11.4 Complications
-
Hypoglossal nerve injury is unlikely, but conceivable.
-
This can be prevented by transecting the hyoid at the level of the lesser cornu and maintaining all subsequent dissection medial to the anterior belly of digastric.
-
Insertion of a drain will also prevent accumulation of a hematoma.
-
Recurrence rates are low when a Sistrunk’s procedure is performed (0–3%), but can be as high as 50% if an inadequate surgical procedure is performed initially.
Key point: If there is a midline cyst in the neck and an ultrasound examination confirms a normal thyroid gland, then a Sistrunk’s procedure should be performed to avoid recurrence (5% will subsequently turn out to be dermoid cysts).
12 Lingual Thyroid
-
If the primitive thyroid gland fails to descend during development, it can enlarge and function within the tongue base.
12.1 Presentation
-
The thyroid mass usually increases in size as the child develops and may manifest as a mass lesion in the tongue base causing dysphagia, dysphonia, and airway compromise.
12.2 Investigations
-
A radioisotope scan is required to confirm the diagnosis and to determine the amount of functioning thyroid tissue present.
-
Thyroid function tests also.
12.3 Management
-
In an euthyroid and asymptomatic child, no treatment is required.
-
If the child has functional symptoms, then thyroid replacement therapy should be commenced to see if regression of the mass occurs.
-
If this results in an acceptable improvement in symptoms, then medical therapy can continue.
-
An inadequate response requires surgical excision of the mass followed by thyroid replacement.
-
Surgery carries no risk to the parathyroid glands, which are derived from the third and fourth arches.
Take Home Messages
-
Beware of “simple” skin pits/dimples around the face and neck—they may relate to an underlying branchial anomaly.
-
Thyroglossal duct cysts. If there is a midline cyst in the neck and an ultrasound scan confirms a normal thyroid gland, then a Sistrunk’s procedure should be performed to avoid recurrence (5% will subsequently turn out to be dermoid cysts).
Further Readings
Ang AH, Pang KP, Tan LK. Complete branchial fistula: case report and review of the literature. Ann Otol Rhinol Laryngol. 2001;110(11):1077. [PMID: 11713922] (Discusses the diagnosis and management of branchial cleft cysts).
Paczona R, Jori J, Czigner J. Pharyngeal localizations of branchial cysts. Eur Arch Otorhinolaryngol. 1998;255(7):379. [PMID: 9783138] (Reviews the location and development of branchial cysts).
Mandell DL. Head and neck anomalies related to the branchial apparatus. Otolaryngol Clin North Am. 2000;33:1309–32.
Al-Khateeb TH, Al Zoubi F. Congenital neck masses: a descriptive retrospective study of 252 cases. J Oral Maxillofac Surg. 2007;65(11):2242–7.
Al-Dajani N, Wootton SH. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007;21(2):523–41.
Shrime M, et al. Fourth branchial complex anomalies: a case series. Int J Pediatr Otorhinolaryngol. 2003;67(11):1227–33.
Verret DJ, et al. Endoscopic cauterization of fourth branchial cleft sinus tracts. Arch Otolaryngol Head Neck Surg. 2004;130(4):465–8.
Papadogeorgakis N, et al. Branchial cleft cysts in adults. Diagnostic procedures and treatment in a series of 18 cases. Oral Maxillofac Surg. 2009;13(2):79–85.
White WM, et al. Recurrent laryngeal nerve monitoring during thyroidectomy and related cervical procedures in the pediatric population. Arch Otolaryngol Head Neck Surg. 2009;135(1):88–94.
Prasad SC, et al. Branchial anomalies: diagnosis and management. Int J Otolaryngol. 2014;2014:237015.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Abdulkader, F., Lannigan, F.J., Taha, M. (2021). Branchial Arch: Anatomy and Anomalies. In: Al-Qahtani, A., Haidar, H., Larem, A. (eds) Textbook of Clinical Otolaryngology. Springer, Cham. https://doi.org/10.1007/978-3-030-54088-3_57
Download citation
DOI: https://doi.org/10.1007/978-3-030-54088-3_57
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-54087-6
Online ISBN: 978-3-030-54088-3
eBook Packages: MedicineMedicine (R0)