Abstract
Robotic surgery has emerged as innovative technique with specific difficulties, completely different from open and laparoscopic surgery. In order to introduce robotic surgery safely and efficiently without compromising the surgical results and patient safety, structured learning in specific competence-based training curricula is required.
Currently, there is no international consensus on the credentials for robotic surgeons. Validating training curricula in which trainees’ performance is assessed using validated assessment tools is a crucial first step toward robotic surgery credentials. These training programs should be organized in a modular way, consisting of knowledge development (online), training of basic and advanced skills in dry and wet laboratory environments, and console training. It must be considered technical-robotic surgical training and nontechnical skills for completeness.
The validation of training curricula is essential as this demonstrates their educational impact and the potential for differentiation between different levels of competence. This can be obtained from randomized and well-developed studies in which the performance of trained and untrained participants is compared by independent and blind assessors in a center of excellence.
Technological evolution will continue to bring new innovations in the field of minimally invasive surgery, and training should evolve accordingly.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 The Rationale Behind the Need for Validated Robotic Surgery Training Curricula
Under the influence of technological evolution, surgery has undergone a major transformation leading to the development and application of minimally invasive surgical techniques. Starting in the early 1980s, minimally invasive surgery quickly and widely became the “gold standard” for many surgical interventions which previously were performed only in the classical, “open” approach. This innovation has allowed for less surgical trauma, postoperative pain, shorter length of stay, better cosmetic results, and earlier functional recovery relative to open surgery [1].
Over the last decades, robotic surgery has emerged as a novel technology which has revolutionized the field of minimally invasive surgery. This innovative technique has become an integral part of many different surgical specialties such as urology, general, thoracic, cardiac, and head and neck surgeries [2,3,4,5]. Since the introduction of robotic surgery in the mid-1990s, its implementation has increased exponentially, with more than 5,000,000 robot-assisted procedures performed by 2017 with the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, USA) [6]. Moreover, in specific surgical fields, such as urology, robotic surgery has become the preferred surgical approach for several procedures [3, 4, 7,8,9,10].
However, this innovation has also created new challenges in terms of training and teaching. Robotic surgery comes with specific difficulties since the platform is very different from other forms of surgery [11]. Just as the Fundamentals of Laparoscopic Surgery (FLS) , a validated, evidence-based skills program, was born in response to the need for specific training in laparoscopic surgery, the same need for training is developing in robotic surgery. Although seen as an evolution of laparoscopic surgery, the skills needed in robot-assisted surgery are unique and cannot be compared to those needed in laparoscopic or open surgery [2, 4, 5, 12, 13]. In robotic surgery, the required skills are mainly for console control, maneuvers without haptic feedback, and communication with the bedside assistant. Conversely, in laparoscopic surgery, the required skills are mainly for 2D surgery with instruments with a restricted range of motion. The guidelines that exist for training in laparoscopic surgery therefore cannot be considered an equivalent to robotic surgery [2, 4, 12].
While the role of robot-assisted surgery is expanding rapidly and widely, there is lack of structured training in robotic surgery. Specified and centralized competency standards for new robotic surgeons do not exist [9]. In 2013, a group of experts expressed concern that robotic surgery training is random and insufficient to ensure patient safety [4]. An independent review from the Emergency Care Research Institute (ECRI), an institute on health technology hazards, in 2015 identified a lack of robotic surgical training as one of the top 10 risks to patients [14]. Therefore, the development of standardized and validated training programs is urgently needed. In order to introduce robotic surgery to surgeons in a safe and efficient way without compromising surgical outcomes and patient safety, new, specific, and structured educational curricula as well as proficiency-based credentialing processes are needed. Furthermore, in robotic surgery, the importance of team training is essential. Specific trainings for all members of the surgical team, consisting of the console surgeon, the bedside assistant, the scrub nurse, the circulating nurse, and the anesthesiologist, are necessary since they all need to understand the spatial relationships of the instruments outside the vision of the surgical field to ensure patient safety and avoid involuntary tissue injury [3].
Robotic surgery training curricula increase preclinical exposure avoiding patients to be used as a training module, which is unacceptable from an ethical point of view. Validated curricula will help standardization of training in robotic surgery with accreditation and certification of surgeons for robot-assisted surgery [2,3,4, 9, 12, 15].
The aim of this chapter is to highlight the aspect of training in robotic surgery. We will discuss the organization and validation of training curricula with robotic surgeon credentialing as a final goal, including an overview of all currently available robotic surgery training curricula and the status of their validation.
2 What Does a Proper Robotic Training Curriculum Look Like?
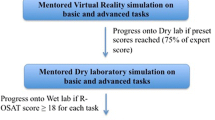
Training should occur in a modular fashion with a well-structured road map (Fig. 5.1) [2].
A training curriculum should start with adequate theoretical knowledge development. A trainee should become familiar with the robotic technology by education on the specific robotic device’s parameters and functions. Knowledge and working of the console are of the utmost importance. Instructions on troubleshooting and the limitations of the operating system are essential. Online modules are available that introduce the basic concepts of the only commercially available system, the Da Vinci Robot (https://www.davincisurgerycommunity.com/Training?tab1=TR). Certification in these online modules is essential before starting any console training [2,3,4, 15].
After a trainee is well educated on the robotic platform, the training of robotic technical skills can start. The first step consists in performing dry lab exercises on inanimate benchtop models or virtual reality-simulated environments. These exercises are an important step in achieving basic and advanced console skills and improving coordination development, bimanuality, dissection, and suturing techniques. Simulators are cheap to run, well tolerated, convenient, and efficient [2, 4, 12, 15]. However, the exercises that we can perform with virtual reality simulators lack bleeding and do not compare with real-life surgery.
The wet lab should be the next step in training after basic surgical skills are acquired in the dry lab. In the wet lab, surgical techniques are trained on cadaveric (i.e., dog model) or live animals (i.e., porcine model) or human cadavers. These anatomical models are more comparable to real-life surgery, allowing the trainees to learn to recognize the robustness and consistency of real tissues and to simulate complete surgical procedures and emergency scenario such as vascular/organ injuries. However, wet labs imply great costs and a large number of animals to be sacrificed [2, 4, 12, 15]. Worldwide, there are 24 recognized, fully equipped educational centers for wet lab training. In Europe, there are three recognized training centers offering a wet lab: the European Robotic and Minimal Invasive Surgery Institute ORSI Academy (Melle, Belgium), the Center of Advanced Simulation and Education (CASE) (Istanbul, Turkey), and Practicum Clinical Skills Centre (Lund, Sweden).
Subsequently, real-life case observation in a training center is essential. This should include patient-side training with learning of basic surgical skills such as patient positioning, establishing pneumoperitoneum, procedure-specific port placement, robot docking, and basic laparoscopic skills [2, 12].
Only after going through all these steps a trainee can start performing supervised surgery in a modular fashion under the supervision of expert surgeons. The presence of a dual console is strongly encouraged, allowing two surgeons to interact and operate at the same time, thus resulting in better control [3, 12, 15]. The learning curriculum ends with independent performance of surgery [3, 4, 12, 15].
Besides training in technical robotic surgical skills, trainees should also be trained in nontechnical skills , including surgical cognitive skills (surgical knowledge, decision-making, planning, and situational awareness) and social skills (abilities of leadership, communication, and teamwork). Cognitive and interpersonal skills and team organization lead to effective transmission of robotic surgical care, but a lack of nontechnical skills may impact patient safety and can lead to adverse events [2, 8, 9]. Nontechnical skills training and team training therefore must be an integral part of robotic training curricula, with the possibility to learn through a simulation training that can replicate common and emergency scenarios in robotic surgery [16].
The curricula must include a final evaluation that allows to verify the learning of the procedure. Only after positive evaluation, the trainee should be certified as a robotic surgeon.
Nowadays, the training in robotic surgery is not organized, and centralized competency standards do not exist. Moreover, the process of robotic surgery certification lacks consistency [3, 4, 9, 17,18,19]. Therefore, consistent and validated surgical curricula are essential in the standardization of training, accreditation, and certification of surgeons for robot-assisted surgery.
An adequate and effective robotic surgery training curriculum should encompass a complete preparation on performing robotic surgery in a safe way with good clinical outcomes. Therefore, the development of these training curricula requires a systematic approach. Once learning needs are identified and integrated in a curriculum, validation is essential before implementation (Fig. 5.2) [4].
3 How to Validate a Robotic Surgery Training Curriculum
To develop a structured and validated curriculum , it is fundamental first of all to identify the right population to be trained and to assess the time needed for each step of the curriculum [20]. A training curriculum to be validated and implemented should undergo different degrees of validation (face, content, construct, concurrent and predicted validity) and should be reproducible (reliability), feasible (feasibility), and acceptable (acceptability) [21]. Educational impact and cost-effectiveness are also mandatory to assess before its implementation (Fig. 5.3) [21,22,23].
The main goal of training curricula in robotic surgery is to objectively demonstrate that performing a proposed training program will result in improved robotic surgical performance in clinical practice, thus proving concurrent validity (Fig. 5.3) [23]. Seen the need of robotic surgeons to have a defined, clear, and coherent training, it is necessary to specify the validation modality of the programs in which these surgeons are trained. The validation of a robotic training curriculum proves its educational impact and its potential to differentiate between different levels of competence and is therefore essential [24].
A recent review performed by Ahmed et al. [24] on observational tools for assessment of procedural skills underlines that the validation process of a study in which technical skills are assessed should be performed in a well-powered, experimental study in a controlled environment. Trainees should be evaluated by different independent and blind assessors (inter-rater reliability). The results of different test items should be compared for internal consistency (inter-item reliability ), and the same assessor should rate the performance of the same subject at two different occasions (e.g., on different times) for test-retest reliability . Construct validity can be determined by dividing different tests for various levels of training, and concurrent validity may be established by correlating the tool to a gold standard method if available [24]. In practice, the validation of a robotic surgery training curriculum should occur in a randomized study, performed in a robotic surgery center of excellence. The performance of trained and untrained participants should be evaluated and compared objectively by use of validated assessment tools. In order to make the curriculum internationally recognized, the leading, recognized world-governing bodies for the specific specialty must be involved [4].
Before implementation at the institutional level, training curricula need to be evaluated for feasibility, acceptability, educational impact, and cost-effectiveness. Using surveys or interviews with trainees, it is possible to recognize the feasibility and acceptability of the training, while the educational impact can be assessed by providing constructive feedback to the participants. Cost analysis of the process depends on many aspects including the evaluation environment and the geographical area in which the program is run (Fig. 5.4) [23].
4 Robotic Surgery Training: Virtual Reality Robotic Surgery Simulators
To familiarize with the robotic system , it is necessary to start the practice with the use of virtual simulators. Indeed, virtual reality robotic surgery simulators are an integral part of all currently available major robotic surgery training curricula. Simulators give a safe environment for trainees to learn how to use the robotic surgery platform and to develop robotic surgical skills. The robotic system is ideal to integrate different forms of simulation next to classical surgical teaching [3, 17]. In this way, trainees may pass their basic learning curve on a simulator and use it as a bridge before starting with real-life surgery. Patient safety and surgical outcome are thereby ensued [3, 17, 18].
Evidence suggests that simulators should be integrated into proficiency-based curricula for training in basic robotic surgical skills and procedural tasks prior to independent practice since training on VR training consoles may improve performance in real life [2, 3, 19, 25]. However, there is lack of strong evidence on the predictive validity of the simulators, i.e., the application of skills gained using simulators to real-life robotic surgery [2, 7, 10].
The first virtual reality robotic surgery simulator was introduced in 2010. So far, six virtual reality simulators are commercially available for robotic surgery training: the da Vinci Skills Simulator (by Intuitive Surgical, Sunnyvale, USA), the Robotic Surgical Simulator (RoSS) (by Simulated Surgical Systems, Buffalo, USA), the SEP robot (by SimSurgery, Norway), the dV-trainer (by Mimic Technologies Inc., Seattle, USA), the ProMIS (Haptica, Ireland), and the RobotiX Mentor (by 3D systems, Israel) [2, 4, 10, 26].
All these simulators underwent evaluation of their validity in different studies. Different degrees of validation are possible [2, 10, 12]:
-
Face validity: The extent to which the simulator resembles a real-life situation. This is generally determined by a group of experts.
-
Content validity: The extent to which the skills tested by the simulator accurately represent the skills required in robotic surgery.
-
Construct validity: The extent to which the assessment exercise measures the intended content domain or the extent to which the simulated task discriminates between operators of different levels of surgical skill.
-
Discriminant validity: The extent to which a simulator is able to differentiate between ability levels within a group with similar experience.
-
Concurrent validity: The extent to which the simulator scores and actual robotic scores are comparable for a similar task.
-
Predictive validity: The extent to which the performance on the simulator predicts future performance on the robotic platform when used clinically.
All simulators (regardless of add-ons) have been evaluated in literature to have at least face, content, and construct validity, except for RoSS which did not show evidence of construct validity [2, 27].
The most frequently used simulator today is the da Vinci Skills Simulator (dVSS) . This simulator is actually a customized computer package that runs on the actual surgical console. It exists for both the Si and the Xi da Vinci systems and offers basic to advanced training modules [12]. The simulator allows instant feedback with an overall score that takes into account both performance efficiency in time, movement economy, and penalty metrics. Modular training add-ons for specific complex procedures, such as radical prostatectomy and hysterectomy, are available. Face, content, construct, concurrent, and predictive validity have been proven in literature [12, 26, 28,29,30].
The Mimic dV-Trainer (MdVT) , RoSS, and RobotiX Mentor are stand-alone virtual reality robotic surgery simulators that mimic the da Vinci Surgical System. All three simulators offer multiple basic to advanced training modules with comprehensive performance metrics, evaluated by an automated, integrated system [3, 12, 17, 26, 31,32,33,34].
MdVT, RoSS, and the RobotiX Mentor offer procedure-specific modules in which trainees interact with a 3D virtual reality anatomical environment. Maestro AR, the procedure-specific add-on of the MdVT , offers training in right partial nephrectomy, hysterectomy, inguinal hernia repair, and radical prostatectomy for both da Vinci Si and Xi [2, 26]. The Tube 3 module of the MdVT is specifically designed to train the vesicourethral anastomosis, thereby increasing the performance of trainees in one of the most complex steps in robot-assisted radical prostatectomy [26, 34]. The Hands-on-Surgical Training (HoST) add-on of RoSS offers training in radical hysterectomy, radical prostatectomy, radical cystectomy, and extended lymph node dissection [2, 26]. The RobotiX Mentor offers training in complete surgical procedures such as radical prostatectomy, hysterectomy, lobectomy, inguinal hernia repair, and right hemicolectomy [17, 26, 35].
Both the RobotiX Mentor and the MdVT offer a laparoscopic assistant component in parallel with the virtual reality console. This allows simultaneous training of both a surgeon and a bedside assistant, improving coordination, communication, and teamwork. For the MdVT, this is a specific add-on called the Xperience Team Trainer [2, 26, 36,37,38].
The SimSurgery Educational Platform (SEP) Robot and the Da Vinci-ProMIS surgical simulator are two robotic surgery simulators that are modifications of previous laparoscopic simulators. In these simulators, the basic laparoscopic instruments have been replaced by the wristed instruments with seven degrees of freedom as found in the da Vinci Robot. The SEP robot is a virtual reality simulator which offers different exercises in which trainees are evaluated based on instrument tip trajectory, time, and error scores [39]. Although being a cost-effective alternative to other simulators, SEP has a lot of shortcomings: it does not offer the possibility to train clutching, needle control, and driving or dissection exercises as in other simulators. Furthermore, a fourth robotic arm, three-dimensional images and performance feedback are not provided by SEP [3, 26].
The da Vinci-ProMIS surgical simulator is a hybrid simulator in which the da Vinci Surgical System is docked to the ProMIS bodyform, a plastic mannequin covered with neoprene. Inside the simulator, three camera-tracking systems detect the instruments inside the simulator, offering evaluation of time, economy of motion, and instrument path length for both virtual and physical training models [26, 40].
Properties of all virtual reality robotic surgery simulators and the status of their validation are summarized in Tables 5.1 and 5.2 [22].
5 Training Curricula in Robotic Surgery
Although multiple, well-developed training programs exist for both open and laparoscopic surgical skills development, the versatility in training curricula in robotic surgery is much smaller.
A large number of available “training curricula” are available worldwide (Table 5.3). However, the term “curriculum” is broad. Some curricula are industry-led short training sessions which lack any formal assessment of competency, whereas others are all-inclusive fellowship-style courses that take months to complete [5, 43, 59]. Of all existing curricula for robotic surgical training, only a few were validated [9, 18, 19, 43, 59].
5.1 The European Association of Urology Robotic Training Curriculum
The European Association of Urology Robotic (ERUS) training curriculum (Fig. 5.5) is a 3-month comprehensive training course which was developed based on an expert panel discussion with the robot-assisted radical prostatectomy as index procedure [19]. After undergoing a specifically developed e-learning module, trainees observe and assist during live surgery for 3 weeks. This is followed by an intensive week of simulation-based training, including virtual reality simulation (using the dVSS), dry lab, and wet lab training platforms. The technical robotic skills included are EndoWrist manipulation, camera movement and clutching, use of energy and dissection, and needle driving.
Structure of the European Association of Urology Robotic Training Curriculum. (Reproduced with permission [19])
Improvement of technical skills is assessed by comparing the scores at baseline and on final assessment using the inbuilt validated assessment metrics on the dVSS [9, 19].
After the simulations, trainees move on to the fellowship stage, which consists of a supervised modular training program in robot-assisted radical prostatectomy with proficiency-based, progressive training of surgical steps with increasing complexity.
The training continues until trainees fulfill a complete robot-assisted radical prostatectomy. During these procedures, the surgical quality of each step is assessed by use of a validated RARP procedure-specific scoring scale. Procedural skills are evaluated by the mentor using the validated Global Evaluative Assessment of Robotic Skills (GEARS) score [9, 19].
A video of the final RARP performed by the trainee is recorded and reviewed by two blinded expert robotic surgeons. They use a generic dedicated scoring criterion for each procedural step to make a final overall score for each trainee, which can then be compared to the score of expert robotic surgeons.
Volpe et al. [19] assessed the validity of the ERUS training curriculum, enrolling ten international fellows in the training program. All trainees completed the e-learning module and passed the final test for the assessment of theoretical knowledge successfully. Afterward, the trainees observed and witnessed a minimum number of procedures (>12 cases) during 3 weeks. The trainees then followed an intensive week of laboratory training, after which their overall score for dVSS tasks significantly increased. In the next 8 weeks, trainees started with supervised modular training, in which they were involved as surgeons in, on average, 18 operations. After completing the curriculum, 80% of trainees was deemed able by their expert supervisors to perform a RARP independently, effectively, and safely. Volpe et al. [19] proved that the structured 12-week ERUS training curriculum is feasible, acceptable, and effective in improving the robotic technical skills and abilities of young surgeons with limited robotic experience to perform the crucial steps of robotic radical prostatectomy [9, 19]. The face, content, and construct validity of the ERUS training curriculum have been demonstrated [9, 19, 59].
In 2016, an update of this training was published that extends the training period of 3 months for a total of 6 months (Fig. 5.6) so that even the most inexperienced participants are confident to continue and finish the training with the awareness of having the time to improve [9].
Structure of the European Association of Urology Robotic Training Curriculum (Update). (Reproduced with permission [9])
A model of this type could represent the ideal training opportunity for naïve surgeons who need both theory-based and practical (domain and technical knowledge) for a specific surgical procedure [9].
5.2 Fundamental Skills of Robotic Surgery (FSRS)
The Fundamental Skills of Robotic Surgery (FSRS) training curriculum is a validated, structured, simulation-based training program that was created by the Roswell Cancer Institute in Buffalo, USA. The curriculum consists of four modules (orientation, motor skills, basic and intermediate surgical skills) with a series of 16 tasks, with each task containing three difficulty levels and an evaluation phase (Fig. 5.7). The curriculum is performed on the validated RoSS simulator, which automatically records and saves performance metrics of trainees. The tasks were specifically created by a group of expert robotic surgeons with integration of previously validated tasks from the Fundamentals of Laparoscopic Surgery curriculum [18, 59].
The Structured Fundamental Skills of Robotic Surgery (FSRS) curriculum. (Derived from Stegemann et al. Reproduced with permission [18])
In the validation study of the FSRS, 53 participants without any previous robotic surgical experience were included whose performance was assessed by three tasks that had to be performed three times each on the da Vinci Surgical System: ball placement, suture pass, and fourth-arm manipulation. The participants were randomized in two groups: an experimental group (EG) and a control group (CG). Participants of both groups received a didactic session to introduce the da Vinci Surgical System, led by an experienced operator. Participants included in the EG completed the FSRS training curriculum once in three to four sessions before completing the three tasks, while participants of the CG had to complete the tasks without completing the FSRS curriculum. Finally, after completing the three tasks, the participants included in the CG were offered to complete the FSRS curriculum and redo the three tasks afterward as a crossover group (CO).
The participants’ performance on the three tasks was evaluated by video assessment by two trained, blinded, and independent reviewers. Assessment parameters included time to complete the tasks, the number of camera and clutch movements, the number of collisions, the number of drops, and the number of movements of instruments outside of the field of view. These assessment parameters were scored for each of the three takes of each task, and mean values were used for comparison of performance of the different study groups. Participants in the EG demonstrated significantly less drops and moved their instruments outside the view of the camera significantly less often than the CG. When comparing the results of the CG and CO participants, there was a significant improvement in time to completion and a significant decrease in number of errors with significantly less drops and movements of instruments outside of the camera’s view. Therefore, Stegemann et al. [18] demonstrated that the FSRS curriculum is a valid and feasible training curriculum that can improve trainees’ basic robotic surgical skills.
In 2014, construct validity of the FSRS curriculum was demonstrated by Raza et al. [60]. Sixty-one surgeons of variable surgical experience (49 novices and 12 experts) were evaluated when performing four tasks (ball placement, coordinated tool control, fourth-arm control and needle handling and exchange), which were selected on expert consensus and represented the core of the three modules of the FSRS curriculum. The performance of participants was assessed by use of the built-in software in the RoSS, which evaluated 10 metrics in each task. Depending on their surgical experience, participants were able to perform one or three preliminary levels of each task, before the final evaluation started. Raza et al. [60] demonstrated that the expert participants performed significantly better than the novices at all aspects of the individual tasks, thereby proving construct validity of the FSRS curriculum.
The Robot-Assisted Surgical Training (RAST) program is a 5-day to 3-week training curriculum that was developed at Roswell Park Cancer Institute and consists of the validated FSRS curriculum combined with other forms of hands-on training, including HoST training and wet lab training. Attalla et al. [41] showed that RAST has an educational impact on trainees [59].
5.3 Proficiency-Based Robotic Curriculum
The proficiency-based robotic curriculum is a validated, comprehensive training program created by the University of Texas Southwestern Medical Center. The curriculum consists of three curricular components: an online tutorial (by Intuitive Surgical) covering fundamental aspects of robotic surgery, a half-day interactive session, and hands-on practice with nine inanimate exercises (Fig. 5.8, Table 5.4) [5]. These exercises were developed by interviewing robotic surgery experts and through observation of live robotic surgery and aim to train 23 unique robotic skills (Fig. 5.9). The exercises are performed on a standard da Vinci system with box trainer and show increasing degrees of complexity to facilitate proficiency-based skill acquisition. It takes 2 months to complete the training program, and trainees have to self-practice the nine exercises.
The proficiency-based robotic curriculum. (Reproduced with permission [5])
Task deconstruction list of 23 unique and necessary surgical skills. (Reproduced with permission [5])
All exercises are assessed using an objective scoring system based on the validated FLS approach time and errors [5].
Content and face validity of the proficiency-based robotic curriculum were demonstrated by Dulan et al. [61] when 12 expert robotic surgeons rated each of the 23 deconstructed skills and performed the 9 exercises. They concluded that all 23 deconstructed skills were highly relevant and that all 9 exercises effectively measure relevant skills [59]. Dulan et al. [42] also demonstrated construct validity of this curriculum in a group of eight expert robotic surgeons and four novice trainees (medical students). After watching a video showing error avoidance strategies and the correct method to perform the nine exercises of the curriculum, the participants completed the nine exercises themselves. Every task of each participant was scored by a single trained proctor for time and accuracy using modified FLS metrics. Expert surgeons were found to achieve significantly better performance than inexperienced students according to each of the nine task scores [59].
5.4 Basic Skills Training Curriculum (BSTC)
The basic skills training curriculum (BSTC) [43] is a validated 4-week training program developed by the University of Toronto. Trainees undergo a series of didactic lectures and self-directed online training modules (including Fundamentals of Robotic Surgery) before being introduced to the da Vinci Robot. The theoretical module, focusing on the cognitive objectives of the BSTC, includes advantages and disadvantages of robotic technology, analysis of the various robotic systems and its equipment, introduction to the patient cart, surgeon console and vision cart, review of the robot installation principles, placement of trocars, docking, exchange of tools, grafting and resolution of common technical problems, and several practical training sessions. After the theoretical module, a 2-hour hands-on robotic training session starts, focusing on the topics dealt with in the theoretical module. Thereafter, trainees start exercising basic skills on the dVSS such as EndoWrist manipulation and camera navigation, instrument clutching, instrument and third-arm functionality, object manipulation, needle guidance, suturing and binding of the nodes, cauterization, and dissection. This standard set of exercises is repeated for three individual 1-hour sessions on the simulator organized at weekly intervals. The robotic surgical skills of the trainees are evaluated by the built-in assessment tool of the simulator. A trainee passes the test when at least 80% of success has been achieved. Wet lab or real-life surgery training is not included in this training curriculum.
Pre- and post-course skills tests have been conducted on two skill exercises standardized with inanimate models: ring transfer and needle passage. Studies have demonstrated improvement of robotic surgical skills among trainees, regardless of specialty, previous robotic experience, or level of training [43, 59].
5.5 Society of European Robotic Gynaecological Surgery (SERGS) Curriculum
The Society of European Robotic Gynaecological Surgery (SERGS) curriculum [44] is a fellowship-styled, validated tri-modular training curriculum that was designed after the ERUS training curriculum (Fig. 5.10) [19]. The SERGS curriculum uses radical hysterectomy and pelvic lymphadenectomy as index procedures.
The curriculum starts with a didactic introduction at the home education center. It consists of 2 days of e-learning and 1 month of assistance in robot-assisted gynecological procedures. E-learning is evaluated by online test modules. In this first module, trainees are encouraged to perform virtual reality exercises.
After completion of the evaluation tests, the second module starts and consists of a 1-week hands-on procedural training at a European education center for robotic surgery. This includes half a day of theoretical system training, followed by 3–4 days of both dry lab training on the dVSS and wet lab training on live anesthetized pigs and cadaver models. Trainees perform hysterectomies, adnexectomies, and pelvic and para-aortic lymphadenectomies under supervision of an expert robotic surgeon. The progress of robotic surgical skills for each individual trainee is evaluated by comparing the overall score on a dVSS virtual training test at the beginning and the end of the week. At the end of the training, the performance is assessed by Non-Technical Skills for Surgeons (NOTSS) for modular training and by Global Evaluative Assessment of Robotic Skills (GEARS) and Objective Structured Assessment of Technical Skills (OSATS) for procedural training.
Finally, trainees move on to the last module , which focuses on in-house training with supervised real-life surgery. In this stage, trainees perform moderate to complex gynecological procedures under direct supervision of an expert robotic surgeon.
Certification as a robotic gynecological surgeon is possible after formal approval of a completed logbook and assessment of video-recorded surgery by an SERGS expert.
Rusch et al. [44] presented data in which four fellows performed a hysterectomy after completion of the SERGS curriculum. Videos of their performance were assessed by the validated GEARS assessment tool. All trainees were able to perform a hysterectomy without supervision of their mentor with good or acceptable surgical quality. After 1 week, all participants performed better on the virtual reality simulator compared to their baseline performance [11, 44].
5.6 “Western Protocol” Cardiac Surgery Virtual Reality Curriculum
In this virtual reality curriculum, participants train different robotic surgical skills exercises on the dVSS that are needed in cardiac surgery, more specifically in the harvesting of the internal thoracic artery (ITA) and in mitral valve annuloplasty (Table 5.5) [45]. The training protocol consists of nine exercises that were selected according to the robotic skills needed for these two surgical procedures, which were defined by two expert robotic cardiac surgeons.
For the validation study of this curriculum, Valdis et al. [45] recruited 20 surgeons with little experience with the Da Vinci console or with robotic simulators. The study included a video of the interventions to highlight the basic operative techniques and the relevant anatomy. The training program includes an initial evaluation of a surgical procedure on a porcine chest wall with the aim of collecting a length of 10 cm of the ITA peduncle. Subsequently, the trainees had to perform a suture on a pig cardiac model of the mitral valve, completing the first three sutures of an annuloplasty valve. Each activity was performed only once by each student and was timed and evaluated using the time criteria of the Laparoscopic Fundamentals program .
Of the 20 participants in the study, half were able to practice on the simulator several times (up to 80 times to reach the level of competence established by experts). The other half did not receive any additional training (control group). After the training period, the trainees were compared again on the robotic procedure on the animal model. Intraoperative surgical skills were assessed by GEARS [45]. Trainees randomized to the VR group were faster than the control group for both surgical procedures and scored significantly higher with the intraoperative scoring tool. Furthermore, trainees included in the VR group achieved a proficiency level similar to the experts for both time-based scores and the intraoperative assessment, whereas the control group was not able to meet this level of proficiency for any of the primary outcomes. Hereby, Valdis et al. [45] proved that the Western Protocol Cardiac VR Curriculum significantly improves the efficiency and quality of learning in robotic cardiac surgery.
6 Assessment Tools to Evaluate Performance of Robotic Surgery Trainees
Although credentialing is essential to guarantee safe clinical practice, there is currently no official credentialing process for robotic surgeons needed to perform robotic surgery. Standardized, proficiency-based and procedure-specific training curricula are an important step toward this credentialing process since the performance of participants is evaluated stepwise before performing live surgery [3,4,5, 8, 12]. Assessment of skills during, at the end of, and beyond training thus is an important factor for credentialing since this forms the basis for validation of training curricula. Increasing complexity of health-care technologies and the decrease in exposure of trainees as a result of working-time regulations have led to an even more distinct need for objective assessment of performance and competence. Different tools exist to assess performance of trainees during their training.
6.1 Global Assessment Tools
The most commonly used validated rating scale in surgery is the Objective Structured Assessment of Technical Skills (OSATS) [3]. This scale evaluates general surgical technical skills and the surgeon’s knowledge of a specific procedure and flow of an operation. OSATS has been used to evaluate robotic training. However, since it was not specifically designed for robotic surgery, it cannot evaluate all aspects of robotic surgical skills properly [7, 8]. Therefore, the Robotic Objective Structured Assessment of Technical Skills (ROSATS) was developed. This is an assessment tool specifically created for evaluation of robotic surgical skills in which four categories of skills are assessed: depth perception and accuracy, force and tissue handling, dexterity, and efficiency. Each category is scored subjectively from 1 to 5 [62].
In 2012, the Global Evaluative Assessment of Robotic Skills (GEARS) tool was developed by Goh et al. [7] by including features unique to robotic into a validated tool for intraoperative laparoscopic skill assessment surgery, Global Operative Assessment of Laparoscopic Skills (GOALS). GEARS is the first consistent, validated, and standardized clinical assessment tool for intraoperative robotic surgical skills. It was modeled after global rating scales for open and laparoscopic surgery by expert robotic surgeons.
In practice, GEARS is a rating scale in which six domains (depth perception, bimanual dexterity, efficiency, force sensitivity, autonomy, and robotic control) are subjectively evaluated by use of a Likert scale ranging from 1 to 5 (Fig. 5.11) [7]. An overall score is created by summing all scores, in which higher scores resemble better performances. GEARS hereby provides a valid, reliable, and reproducible measure of intraoperative robotic surgical skills [7, 8] in dry lab, wet lab, and real-life surgery environments. Studies show that GEARS scores of specific steps in robot-assisted radical prostatectomy are associated with patient outcomes, such as continence and readmission [7, 8].
In 2014, a validated assessment tool was developed related to robotic microsurgery, the Structured Assessment of Robotic Microsurgery Skills (SARMS) [63]. This tool for robotic microsurgical evaluation originates from the Structured Assessment of Microsurgery Skills (SAMS) in which domains strictly related to robotic surgery have been added. The domains included into this tool are dexterity, visuospatial ability, operative flow, camera movement, depth perception, wrist articulation, atraumatic tissue handling, and atraumatic needle handling. The evaluation is assigned with a score ranging from 1 to 5 [63].
The Assessment of Robotic Console Skills (ARCS) [64] is a validated assessment scale which consists of six categories that identify a group of skills to be acquired at the da Vinci Robot console for its proper use: bimanual wristed manipulation, camera control, master clutching activating energy sources, appropriate depth perception, and awareness of forces applied by instruments [64].
The Generic Dedicated Scoring Criteria (GDSC) [19] is a validated evaluation tool used in the European Association of Urology Robotic Training Curriculum to assess the quality of video-recorded surgical steps of trainees. Parameters evaluated were instrument use, tissue handling, errors made, and the end result, with each parameter being scored from 1 to 4.
Global assessment tools such as GEARS are able to evaluate essential and basic robotic surgical skills . Therefore, these tools are primarily used in lab settings and preclinical training in order to evaluate if trainees can safely move on from training labs to the operating theater (Table 5.6) [8].
6.2 Procedure-Specific Assessment Tools
Next to global assessment tools, different procedure-specific assessment tools exist for more detailed evaluation of specific surgical steps (Table 5.7) [8]. These tools provide cognitive evaluation of surgical skills in a task-deconstructive fashion, identifying specific steps for improvement for individual trainees. There are different examples of procedure-specific assessment tools, of which most were created for urological robot-assisted procedures.
The robot-assisted radical prostatectomy (RARP) assessment score [73] is a validated evaluation tool for RARP. The procedure was divided into 17 crucial phases and 41 subprocesses. Unlike other assessment tools, it is the only one that also analyzes the surgeons’ learning curve. All phases are evaluated with a score of 1 to 5 assigned by expert surgeons.
The robot-assisted partial nephrectomy (RAPN) assessment score [75] is a similar tool to evaluate the performance of a surgeon in RAPN. It was created by identifying all possible failure modes and most dangerous steps in the procedure. It consists of 6 phases with 26 processes and 50 subprocesses. The six phases are “preparation of operative field”; “exposure of surgical field”; “dissection and control of hilum”; “preparation for hilar clamping and tumor excision”; “hilar clamping, warm ischemia time, and tumor excision”; and “finalizing and closure” [75, 76].
Another procedure-specific assessment tool for minimally invasive partial nephrectomy is the “Scoring for Partial Nephrectomy” (SPaN) tool [70]. It is a scoring system that can offer objective and structured feedback on technical skills of trainees. This assessment tool was created by deconstruction of the critical steps of a robot-assisted partial nephrectomy into six domains (exposure of the kidney, ureteral and gonadal vessel identification and dissection, hilum dissection, tumor localization and exposure, tumor clamping and resection, and renorrhaphy). Each domain is then assessed for surgical skills by a Likert score from 1 (worst) to 5 (best).
The Robotic Anastomosis Competency Evaluation (RACE) [65] assessment tool analyzes bladder urethral anastomosis in robotic radical prostatectomy. It consists of six domains (needle positioning, needle entry, needle driving and tissue trauma, suture placement, tissue approximation, and knot tying) which are all scored independently. Scores range from 1 (the worst performance) to 3 (intermediate) to 5 (the ideal performance) [65].
The Prostatectomy Assessment and Competency Evaluation (PACE) [23] is a validated assessment tool that was created by the analysis of RARP by 12 expert robotic surgeons. The procedure was subdivided into seven key points (bladder drop, prostate preparation, bladder neck dissection , posterior/seminal vesicle dissection, neurovascular bundle preservation, apical dissection, urethrovesical anastomosis), which are evaluated with a 5-point Likert scale [23].
The Pelvic Lymphadenectomy appropriateness and Completion Evaluation (PLACE) [68] is a validated, structured intraoperative scoring system to measure and quantify pelvic lymph node dissection (PLND) in robot-assisted radical cystectomy. It was created by a panel of 11 surgeons, who divided the PLND template into three zones. PLNDs of trainees may be evaluated using PLACE, in which the performed PLND is compared with a “perfect” PLND [68].
The Cystectomy Assessment and Surgical Evaluation (CASE) tool [69] was developed for radical cystectomy in men and provides a subdivision of the procedure based on eight key steps (pelvic lymph node dissection, development of the peri-ureteral space, lateral pelvic space, anterior rectal space, control of the vascular pedicle, anterior vesical space, control of the dorsal venous complex, apical dissection). Scores on each step are assigned by a 1–5 Likert scale [69].
These procedure-specific assessment tools evaluate both surgical technical skills and surgical knowledge, thereby assessing the competence of a surgeon to perform a specific procedure independently and safely. These tools could be used for robotic surgeon credentialing and licensing for specific robotic procedures. Although promising, there are currently no data on procedure-specific assessment tools that correlate with patient outcomes. Major disadvantages of manual assessment tools are that they are time-consuming to the evaluators, that they are making evaluation of complete procedures difficult, and that they are exposed to subjective bias, limiting inter-rater reliability [8].
6.3 Automated Assessment Tools
Automated performance metrics (APMs) are other tools that allow to evaluate the performance of trainees in surgical curricula (Table 5.8). APMs integrate objective data that is acquired automatically during surgical training using recording devices, robotic instrument kinematic tracing data, system events data, and surgical video data. Many of these APMs have shown a good ability to distinguish different levels of expertise between surgeons. These data are processed by learning algorithms, and meaningful evaluation and feedback are based on automatically recorded data (computer-aided automated evaluation).
The implementation of APMs in evaluation of trainees holds many advantages: APMs eliminate the bias of human judgment and make robotic surgical technical skills quantifiable. Furthermore, the evaluation of trainees does not longer require major time investments of evaluators since data is collected automatically. On top, performance metrics on complete procedures can be recorded, offering comprehensive evaluation of complete surgeries. Large-scale surgical evaluation, surgeon credentialing, and recredentialing could be performed by computer-aided automated evaluation of surgical technical skill. However, assessment of surgical skills by computer-aided evaluation of APMs is still in early stages of development [8].
6.4 Nontechnical Skills (NTS) Assessments
Next to training and evaluation of technical skills, nontechnical skills (NTS) play an important role in robotic surgery and have the potential to impact patient safety and adverse events [16]. Different assessment tools for NTS have been developed and validated, such as the Non-Technical Skills for Surgeons (NOTSS) [80] and the observational Teamwork Assessment for Surgery (OTAS) [81]. However, specific assessment tools for NTS evaluation in robotic surgery do not exist [16, 82].
7 Conclusions
Over the past decades, a rapid diffusion of robot-assisted surgery in different surgical fields was observed. In order to introduce robotic surgery in a safe and efficient way without compromising surgical outcomes and patient safety, training is mandatory and should be structured in specific, validated proficiency-based training curricula.
Currently, there is no international consensus on credentialing for robotic surgeons. General, centralized competency standards do not exist. Validated training curricula in which the performance of trainees is evaluated by validated assessment tools are a crucial first step toward robotic surgery credentialing. These training curricula should be organized in a modular fashion with a well-structured road map in which trainees start with knowledge development, followed by basic and advanced skills training in dry- and wet lab environments before moving on to console training. Besides technical robotic surgical skills training, nontechnical skills training should be included in these robotic surgery training curricula as well. The validation of training programs is essential since this proves their educational impact and potential to differentiate between different levels of competence. Validation of robotic surgery training curricula can be obtained by well-powered, randomized studies in which the performance of trained and untrained participants is compared by independent and blind assessors in a center of excellence. Several training curricula exist; however, only few were validated. Of these validated training programs, only two followed the aforementioned structure and offer online education, dry- and wet lab training, and real-life surgical modular training under direct supervision. These training programs are the ERUS training curriculum [19] and the SERGS curriculum [44]. The ERUS training curriculum is the first validated training curriculum in which participants are trained in a modular fashion to perform a complete surgical procedure alone. It is feasible, acceptable, and effective in improving the robotic technical skills and abilities of young surgeons with limited robotic experience to perform the crucial steps of robot-assisted radical prostatectomy.
Technological evolution will continue to bring new innovations in the field of minimally invasive surgery, and training should evolve accordingly. The evaluation of surgical skills is essential, and great future lies within computer-aided automated evaluation of surgical technical skills.
References
Barbash GI, Glied SA. New technology and health care costs — the case of robot-assisted surgery. N Engl J Med. 2010;363(8):701–4.
Sridhar AN, Briggs TP, Kelly JD, Nathan S. Training in robotic surgery—an overview. Curr Urol Rep. 2017;18:58.
Schreuder HWR, Wolswijk R, Zweemer RP, Schijven MP, Verheijen RHM. Training and learning robotic surgery, time for a more structured approach: a systematic review. BJOG Int J Obstet Gynaecol. 2012;119:137–49.
Ahmed K, Khan R, Mottrie A, Lovegrove C, Abaza R, Ahlawat R, et al. Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int. 2015;116(1):93–101.
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST, et al. Developing a comprehensive, proficiency-based training program for robotic surgery. Surgery. 2012;152(3):477–88.
Intuitive. About Intuitive [Internet]. 2019 [updated 2019, cited 2019 Feb 17]. Available from: https://www.intuitive.com/en/about-us/company.
Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ. Global evaluative assessment of robotic skills: validation of a clinical assessment tool to measure robotic surgical skills. J Urol. 2012;187(1):247–52.
Chen J, Cheng N, Cacciamani G, Oh P, Lin-Brande M, Remulla D, et al. Objective assessment of robotic surgical technical skill: a systematic review. J Urol. 2019;201(3):461–9.
Mottrie A, Novara G, van der Poel H, Dasgupta P, Montorsi F, Gandaglia G. The European Association of Urology robotic training curriculum: an update. Eur Urol Focus [Internet]. 2016;2(1):105–8. Available from: https://doi.org/10.1016/j.euf.2015.09.002.
Moglia A, Ferrari V, Morelli L, Ferrari M, Mosca F, Cuschieri A. A systematic review of virtual reality simulators for robot-assisted surgery. Eur Urol. 2016;69(6):1065.
Moglia A. Pilot study of Society of European Robotic Gynecological Surgery (SERGS) curriculum for robot-assisted surgery. Arch Gynecol Obstet. 2018;297(6):1595–6.
Brook NR, Dell’Oglio P, Barod R, Collins J, Mottrie A. Comprehensive training in robotic surgery. Curr Opin Urol. 2019;29(1):1–9.
Smith R, Patel V, Satava R. Fundamentals of robotic surgery: a course of basic robotic surgery skills based upon a 14-society consensus template of outcomes measures and curriculum development. Int J Med Robot Comput Assist Surg. 2014;10(3):379–84.
Devices H. Top 10 health technology hazards for 2015: a report from health devices November 2014. ECRI Inst. 2015;(November 2014):1–31.
Buffi N, Van Der Poel H, Guazzoni G, Mottrie A. Methods and priorities of robotic surgery training program. Eur Urol. 2014;65(1):1–2.
Collins JW, Dell’Oglio P, Hung AJ, Brook NR. The importance of technical and non-technical skills in robotic surgery training. Eur Urol Focus [Internet]. 2018;4(5):674–6. Available from: https://doi.org/10.1016/j.euf.2018.08.018e.
Julian D, Tanaka A, Mattingly P, Truong M, Perez M, Smith R. A comparative analysis and guide to virtual reality robotic surgical simulators. Int J Med Robot Comput Assist Surg. 2018;14(1).
Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R, et al. Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology. 2013;81(4):767–74.
Volpe A, Ahmed K, Dasgupta P, Ficarra V, Novara G, Van Der Poel H, et al. Pilot validation study of the European Association of Urology Robotic training curriculum. Eur Urol. 2015;68(2):292–9.
Bahler CD, Sundaram CP. Towards a standardised training curriculum for robotic surgery. BJU Int. 2015;116(1):4–5.
Wass V, Van Der Vleuten C, Shatzer J, Jones R. Pgcert_Wass_Mod4_15. 2001;357:945–9.
Abboudi H, Khan MS, Aboumarzouk O, Guru KA, Challacombe B, Dasgupta P, et al. Current status of validation for robotic surgery simulators a systematic review. BJU Int. 2013;111(2):194–205.
Hussein AA, Ghani KR, Peabody J, Sarle R, Abaza R, Eun D, et al. Development and validation of an objective scoring tool for Ro1. Wass V, Vleuten C Van Der, Shatzer J, Jones R. Pgcert_Wass_Mod4_15. 2001;357:945–9. bot-Assisted radical prostatectomy: prostatectomy assessment and competency evaluation. J Urol [Internet]. 2017;197(5):1237–44. Available from: https://doi.org/10.1016/j.juro.2016.11.100.
Ahmed K, Miskovic D, Darzi A, Athanasiou T, Hanna GB. Observational tools for assessment of procedural skills: a systematic review. Am J Surg [Internet]. 2011;202(4):469–80. Available from: https://doi.org/10.1016/j.amjsurg.2010.10.020.
Walliczek-Dworschak U, Mandapathil M, Förtsch A, Teymoortash A, Dworschak P, Werner JA, et al. Structured training on the da Vinci Skills Simulator leads to improvement in technical performance of robotic novices. Clin Otolaryngol. 2017;42(1):71–80.
Kumar A, Smith R, Patel VR. Current status of robotic simulators in acquisition of robotic surgical skills. Curr Opin Urol. 2015;25(2).
Tanaka A, Graddy C, Simpson K, Perez M, Truong M, Smith R. Robotic surgery simulation validity and usability comparative analysis. Surg Endosc Other Interv Tech. 2016;30(9):3720–9.
Hung AJ, Patil MB, Zehnder P, Cai J, Ng CK, Aron M, et al. Concurrent and predictive validation of a novel robotic surgery simulator: a prospective, randomized study. J Urol. 2012;187(2):630–7.
Kelly DC, Margules AC, Kundavaram CR, Narins H, Gomella LG, Trabulsi EJ, et al. Face, content, and construct validation of the da Vinci Skills Simulator. Urology. 2012;79(5):1068–72.
Finnegan KT, Meraney AM, Staff I, Shichman SJ. Da Vinci skills simulator construct validation study: correlation of prior robotic experience with overall score and time score simulator performance. Urology. 2012;80(2):330–5.
Korets R, Mues AC, Graversen JA, Gupta M, Benson MC, Cooper KL, et al. Validating the use of the Mimic dV-trainer for robotic surgery skill acquisition among urology residents. Urology. 2011;78(6):1326–30.
Lee JY, Mucksavage P, Kerbl DC, Huynh VB, Etafy M, McDougall EM. Validation study of a virtual reality robotic simulator – role as an assessment tool? J Urol. 2012;187(3):998–1002.
Kim JY, Bin KS, Pyun JH, Kim HK, Cho S, Lee JG, et al. Concurrent and predictive validation of robotic simulator tube 3 module. Korean J Urol. 2015;56(11):756–61.
Kang SG, Cho S, Kang SH, Haidar AM, Samavedi S, Palmer KJ, et al. The tube 3 module designed for practicing vesicourethral anastomosis in a virtual reality robotic simulator: determination of face, content, and construct validity. Urology. 2014;84(2):345–50.
Whittaker G, Aydin A, Raison N, Kum F, Challacombe B, Khan MS, et al. Validation of the RobotiX Mentor robotic surgery simulator. J Endourol. 2016;30(3):338–46.
Sessa L, Perrenot C, Xu S, Hubert J, Bresler L, Brunaud L, et al. Face and content validity of Xperience™ team trainer: bed-side assistant training simulator for robotic surgery. Updates Surg. 2018;70(1):113–9.
Xu S, Perez M, Perrenot C, Hubert N, Hubert J. Face, content, construct, and concurrent validity of a novel robotic surgery patient-side simulator: the Xperience™ team trainer. Surg Endosc Other Interv Tech. 2016;30(8):3334–44.
Xu Y-M, Song L-J, Wang K-J, Lin J, Sun G, Yue Z-J, et al. Changing trends in the causes and management of male urethral stricture disease in China: an observational descriptive study from 13 centres. BJU Int. 2015;116(6):938–44.
Gavazzi A, Bahsoun AN, Van Haute W, Ahmed K, Elhage O, Jaye P, et al. Face, content and construct validity of a virtual reality simulator for robotic surgery (SEP Robot). Ann R Coll Surg Engl. 2011;93(2):152–6.
Chandra V, Nehra D, Parent R, Woo R, Reyes R, Hernandez-Boussard T, et al. A comparison of laparoscopic and robotic assisted suturing performance by experts and novices. Surgery. 2010;147(6):830–9.
Attalla K, Raza SJ, Rehman S, Din R, Stegemann A, Field E, et al. Effectiveness of a dedicated robot-assisted surgery training program. Can J Urol. 2013;20(6):7084–90.
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KM, Arain NA, Tesfay ST, et al. Proficiency-based training for robotic surgery: construct validity, workload, and expert levels for nine inanimate exercises. Surg Endosc. 2012;26(6):1516–21.
Foell K, Finelli A, Yasufuku K, Bernardini MQ, Waddell TK, Pace KT, et al. Robotic surgery basic skills training: evaluation of a pilot multidisciplinary simulation-based curriculum. Can Urol Assoc J. 2013;7(11-12):430–4.
Rusch P, Kimmig R, Lecuru F, Persson J, Ponce J, Degueldre M, et al. The Society of European Robotic Gynaecological Surgery (SERGS) Pilot Curriculum for robot assisted gynecological surgery. Arch Gynecol Obstet [Internet]. 2018;297(2):415–20. Available from: https://doi.org/10.1007/s00404-017-4612-5.
Valdis M, Chu MWA, Schlachta CM, Kiaii B. Validation of a novel virtual reality training curriculum for robotic cardiac surgery: a randomized trial. Innov Technol Tech Cardiothorac Vasc Surg. 2015;10(6):383–8. Available from: https://doi.org/10.1097/imi.0000000000000222.
Macgregor JM, Kim RS, Gallagher JT, Soliman MK, Ferrara A, Baldwin K, et al. Fundamentals of robotic surgery, Society of American Gastrointestinal and Endoscopic Surgeons Annual Meeting 2012; San Diego. 2012.
Association of Program Directors for Colon and Rectal Surgery. APDCRS Homepage [Internet]. 2019 [cited 2019 Feb 17]. Available from: http://www.apdcrs.org/wp/
Chitwood WR, Nifong LW, Chapman WHH, Felger JE, Bailey BM, Ballint T, et al. Robotic surgical training in an academic institution. Ann Surg. 2001;234(4):475–86.
Hanly EJ, Zand J, Bachman SL, Marohn MR, Talamini MA. Value of the SAGES Learning Center in introducing new technology. Surg Endosc Other Interv Tech. 2005;19(4):477–83.
University of Pittsburgh Medical Center (UPMC). Center for advanced robotics training (CART) [Internet]. 2015 [updated 2015, cited 2019 Feb 17]. Available from: https://www.upmc.com/healthcare-professionals/education/advanced-robotic-surgery-training.
BAUS business: robotic surgery curriculum, guidelines for training. British Association of Urological Surgeons Web site. Updated 17 August 2015. https://www.baus.org.uk/professionals/baus_business/publications/83/robotic_surgery_curriculum.
University of Alabama at Birmingham. Robotic surgery Curriculum [Internet]. [cited 2019 Feb 17]. Available from: https://www.uab.edu/medicine/obgynresidency/18-academic-curriculum/academic-curriculum/78-robotics-curriculum-v15-78.
Madureira FAV, Varela JLS, Madureira Filho D, D’Almeida LAV, Madureira FAV, Duarte AM, et al. Modelo de programa de treinamento em cirurgia robótica e resultados iniciais. Rev Col Bras Cir [Internet]. 2017;44(3):302–7. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-69912017000300302&lng=pt&tlng=pt.
Lyons C, Goldfarb D, Jones SL, Badhiwala N, Miles B, Link R, et al. Which skills really matter? Proving face, content, and construct validity for a commercial robotic simulator. Surg Endosc Other Interv Tech. 2013;27(6):2020–30.
Robotic Training Network. Robotic Training Network Homepage [Internet]. 2019 [updated 2015, cited 2019 Feb 17]. Available from: https://robotictraining.org/.
International College of Robotic Surgeons. Fellowship of International College of Robotic Surgeons (FICRS) [Internet]. 2012 [updated 2012, cited 2019 Feb 17]. Available from: http://icrsonline.org/fellowship.html.
White J, Sharma A. Development and assessment of a transoral robotic surgery curriculum to train otolaryngology residents. ORL J Otorhinolaryngol Relat Spec. 2018;80(2):69–76.
Emory University School of Medicine. Department of Surgery: Training [Internet]. 2019 [updated 2019, cited 2019 Feb 17]. Available from: http://www.surgery.emory.edu/training/index.html.
Fisher RA, Dasgupta P, Mottrie A, Volpe A, Khan MS, Challacombe B, et al. An over-view of robot assisted surgery curricula and the status of their validation. Int J Surg. 2015;13:115–23.
Raza SJ, Froghi S, Chowriappa A, Ahmed K, Field E, Stegemann AP, et al. Construct validation of the key components of fundamental skills of robotic surgery (FSRS) curriculum - a multi-institution prospective study. J Surg Educ. 2014;71(3):316–24.
Dulan G, Rege RV, Hogg DC, Gilberg-Fisher KK, Tesfay ST, Scott DJ. Content and face validity of a comprehensive robotic skills training program for general surgery, urology, and gynecology. Am J Surg. 2012;203(4):535–9.
Siddiqui NY, Galloway ML, Geller EJ, Green IC, Hur H-C, Langston K, et al. Validity and reliability of the robotic objective structured assessment of technical skills. Obstet Gynecol. 2014;123(6):1193–9.
Alrasheed T, Liu J, Hanasono MM, Butler CE, Selber JC. Robotic microsurgery. Plast Reconstr Surg. 2014;134(4):794–803.
Liu M, Purohit S, Mazanetz J, Allen W, Kreaden US, Curet M. Assessment of Robotic Console Skills (ARCS): construct validity of a novel global rating scale for technical skills in robotically assisted surgery. Surg Endosc Other Interv Tech. 2018;32(1):526–35.
Raza SJ, Field E, Jay C, Eun D, Fumo M, Hu JC, et al. Surgical competency for urethrovesical anastomosis during robot-assisted radical prostatectomy: development and validation of the robotic anastomosis competency evaluation. Urology [Internet]. 2015;85(1):27–32. Available from: https://doi.org/10.1016/j.urology.2014.09.017.
Ghani KR, Miller DC, Linsell S, Brachulis A, Lane B, Sarle R, et al. Measuring to improve: peer and crowd-sourced assessments of technical skill with robot-assisted radical prostatectomy. Eur Urol. 2016;69(4):547–50.
Peabody J, Miller D, Lane B, Sarle R, Brachulis A, Linsell S, et al. PD30-05 wisdom of the crowds: use of crowdsourcing to assess surgical skill of robot-assisted radical prostatectomy in a statewide surgical collaborative. J Urol. 2015;193:e655.
Hussein AA, Hinata N, Dibaj S, May PR, Kozlowski JD, Abol-Enein H, et al. Development, validation and clinical application of Pelvic Lymphadenectomy Assessment and Completion Evaluation: intraoperative assessment of lymph node dissection after robot-assisted radical cystectomy for bladder cancer. BJU Int. 2017;119(6):879–84.
Hussein AA, Sexton KJ, May PR, Meng MV, Hosseini A, Eun DD, et al. Development and validation of surgical training tool: cystectomy assessment and surgical evaluation (CASE) for robot-assisted radical cystectomy for men. Surg Endosc [Internet]. 2018;32(11):4458–64. Available from: https://doi.org/10.1007/s00464-018-6191-3.
Hussein AA, Abaza R, Rogers C, Boris R, Porter J, Allaf M, et al. PD07-09 development and validation of an objective scoring tool for minimally invasive partial nephrectomy: Scoring for Partial Nephrectomy (SPAN). J Urol [Internet]. 2018;199(4):e159–60. Available from: https://doi.org/10.1016/j.juro.2018.02.442.
Frederick PJ, Szender JB, Hussein AA, Kesterson JP, Shelton JA, Anderson TL, et al. Surgical competency for robot-assisted hysterectomy: development and validation of a robotic hysterectomy assessment score (RHAS). J Minim Invasive Gynecol. 2017;24(1):55–61.
Petz W, Spinoglio G, Choi GS, Parvaiz A, Santiago C, Marecik S, et al. Structured training and competence assessment in colorectal robotic surgery. Results of a consensus experts round table. Int J Med Robot Comput Assist Surg. 2016;12(4):634–41.
Lovegrove C, Novara G, Mottrie A, Guru KA, Brown M, Challacombe B, et al. Structured and modular training pathway for robot-assisted radical prostatectomy (RARP): validation of the RARP assessment score and learning curve assessment. Eur Urol [Internet]. 2016;69(3):526–35. Available from: https://doi.org/10.1016/j.eururo.2015.10.048.
Lovegrove C, Ahmed K, Novara G, Guru K, Mottrie A, Challacombe B, et al. Modular training for robot-assisted radical prostatectomy: where to begin? J Surg Educ. 2017;74(3):486–94.
Lovegrove C, Bruce E, Raison N, Challacombe B, Novara G, Mottrie A, et al. Development and content validation of a training and assessment tool for RAPN. J Urol. 2017;197(4S, Supplement):e700.
Bruce E, Lovegrove C, Raison N, Challacombe B, Novara G, Mottrie A, et al. Development and content validation of the assessment tool for robot-assisted partial nephrectomy. J Urol. 2016;195(4S, Supplement):e217.
Tausch TJ, Kowalewski TM, White LW, McDonough PS, Brand TC, Lendvay TS. Content and construct validation of a robotic surgery curriculum using an electromagnetic instrument tracker. J Urol. 2012;188(3):919–23.
Kumar R, Jog A, Vagvolgyi B, Nguyen H, Hager G, Chen CCG, et al. Objective measures for longitudinal assessment of robotic surgery training. J Thorac Cardiovasc Surg. 2012;143(3):528–34.
Hung AJ, Chen J, Jarc A, Hatcher D, Djaladat H, Gill IS. Development and validation of objective performance metrics for robot-assisted radical prostatectomy: a pilot study. J Urol. 2018;199(1):296–304.
Yule J, Hill K, Yule S. Development and evaluation of a patient-centred measurement tool for surgeons’ non-technical skills. BJS [Internet]. 2018;105(7):876–84. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/bjs.10800.
Undre S, Healey AN, Darzi A, Vincent CA. Observational assessment of surgical teamwork: a feasibility study. World J Surg [Internet]. 2006;30(10):1774–83. Available from: https://doi.org/10.1007/s00268-005-0488-9.
Raison N, Wood T, Brunckhorst O, Abe T, Ross T, Challacombe B, et al. Development and validation of a tool for non-technical skills evaluation in robotic surgery---the ICARS system. Surg Endosc [Internet]. 2017;31(12):5403–10. Available from: https://doi.org/10.1007/s00464-017-5622-x.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lambert, E., Palagonia, E., Wisz, P., Mottrie, A., Dell’Oglio, P. (2021). Validating Robotic Surgery Curricula. In: Gharagozloo, F., Patel, V.R., Giulianotti, P.C., Poston, R., Gruessner, R., Meyer, M. (eds) Robotic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-53594-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-53594-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53593-3
Online ISBN: 978-3-030-53594-0
eBook Packages: MedicineMedicine (R0)