Abstract
Patients should be evaluated and deemed appropriate for such surgical intervention. Smaller eyelid defects can be repaired using direct closure with or without canthotomy and cantholysis. Larger defects may require more elaborate surgical techniques such a Hughes tarsoconjunctival flap with an independently rotated myocutaneous flap for anterior lamellar reconstruction. Patients with moderate-sized upper or lower lid defects are ideal candidates for this procedure, though some surgeons extend the application to significantly larger defects, particularly in those who would not be good candidates for an eyelid sharing procedure (monocular patients and children at risk of amblyopia). An additional advantage of the Tenzel flap is that any remaining temporal eyelashes are transposed centrally, minimizing the potential cosmetic penalty of surgical madarosis. The choice of technique for eyelid reconstruction should be discussed with the patient once the size of the defect is known and the appropriate procedure tailored to the individual patient’s needs and anatomy. Patients should be educated about the risks and benefits of the procedure as well as about any alternatives.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Indications
The patient had a moderate (25–50%) (upper/lower) eyelid defect due to (trauma/neoplasm).
Essential Steps
-
1.
Transfer patient to operating room.
-
2.
Measure eyelid lid defect.
-
3.
Semicircular flap marked.
-
4.
Flap incised and dissected.
-
5.
Lateral canthotomy performed.
-
6.
Posterior lamellar reconstructed with periosteal flap (optional).
-
7.
Full-thickness eyelid defect closed.
-
8.
Flap closure.
Complications
-
Infection
-
Bleeding/hematoma
-
Pain
-
Poor cosmesis
-
Visible scarring
-
Asymmetry
-
Need for further procedures
-
Retrobulbar hemorrhage
-
Postoperative dry eye
-
Corneal trauma
-
Lagophthalmos
Template Operative Dictation
Preoperative diagnosis:
(Right/Left) (upper/lower) eyelid defect secondary to (trauma/neoplasm)
Procedure:
(Right/Left) (upper/lower) Tenzel semicircular flap
Postoperative diagnosis:
Same
Indication:
This ____-year-old (male/female) has an (upper/lower) eyelid defect constituting __ % of the horizontal dimension, secondary to trauma/neoplasm. The risks, benefits, and alternatives to the procedure were discussed with the patient including the risk for infection, bleeding, pain, lagophthalmos, scarring, poor cosmesis, postoperative dry eye symptoms, asymmetry, corneal trauma, and need for further procedures. Afterwards, the patient requested that we perform surgery and signed the required consent forms.
Description of the procedure:
The patient was brought to the operating room where the (right/left) eye, adnexal structures, and face were sterilized with 5% betadine ophthalmic solution. The patient was draped in the standard sterile fashion for oculoplastic surgery. A time-out was then performed confirming the correct patient, correct sites, correct surgery, and any known drug allergies.
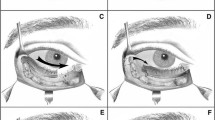
Attention was drawn to the (right/left) (upper/lower) eyelid defect. The nasal and temporal lower lid remnants were grasped with toothed forces and brought together using gentle tension. The resulting horizontal defect was not amenable to primary closure with canthotomy and cantholysis alone. Accordingly, a semicircular flap was marked approximately 2 cm vertically and horizontally from the lateral canthus, with the apex of the marking extending (superiorly – for lower lid defects/inferiorly – for upper lid defects). The subcutaneous tissues underlying the semicircular flap and the eyelid remnants adjacent to the defect were infiltrated with 2% lidocaine with epinephrine (1:100,000).
An incision was made through the skin and underlying orbicularis muscle along the previously created marking, and a myocutaneous flap was elevated. Westcott scissors were used to perform a lateral canthotomy, which was extended into the previously created incision. The cut margin of the lower lid was then elevated with forceps, and the scissor tips were pointed towards the ipsilateral nasal ala and used to strum the inferior crus of the lateral canthal tendon. Once identified, the (inferior – for lower lid defects/superior – for upper lid defects) cantholysis was performed. The completed Tenzel flap was then rotated (superiorly – for upper lid defects/inferiorly – for lower lid defects) into the eyelid defect.
If reconstruction of the posterior lamellar tissues was performed:
The lateral orbital rim periosteum was exposed with a Freer elevator. A periosteal flap, hinged at the lateral orbital rim, was then outlined with a surgical marking pen. The previously marked incisions were then completed with a #15 Bard-Parker blade. The flap was then elevated from the underlying bone and reflected into the temporal lower lid defect in order to recreate the absent posterior lamellar tissues. It was anchored to the temporal tarsal margin of the Tenzel flap using lamellar passes of 5-0 Vicryl suture.
Attention was then redirected to the eyelid defect, where a 5-0 silk suture was placed through the Meibomian gland orifices on either side of the defect in a vertical mattress fashion and clipped to the drape. The orbicularis muscle was then bluntly dissected for 2–3 mm on either side of the incision in order to expose the underlying tarsal plate. _#_ interrupted 5-0 Vicryl sutures were then passed through the cut edges of the tarsal plate in lamellar fashion. The silk lid margin suture was then tied, and the ends left long. The lamellar Vicryl sutures were then tied and trimmed. The lash margin and skin were then closed with interrupted 7-0 Vicryl sutures, and the tails of the silk suture were incorporated to prevent corneal contact. The flap was then closed with deep 6-0 Vicryl sutures and superficial 6-0 Nylon sutures.
Antibiotic ophthalmic ointment was then applied to the surgical site. A pressure dressing was applied which was to be left in place until the next visit. The patient tolerated the procedure well without any intraoperative or immediate postoperative complications. All needle and sponge counts were correct at the end of the procedure. The patient was then taken to the recovery room in stable condition and will be seen in the oculoplastics clinic in ___ week(s).
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Crane, A.M., Erickson, B., Lee, W.W. (2021). Tenzel Semicircular Flap. In: Rosenberg, E.D., Nattis, A.S., Nattis, R.J. (eds) Operative Dictations in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-030-53058-7_169
Download citation
DOI: https://doi.org/10.1007/978-3-030-53058-7_169
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53057-0
Online ISBN: 978-3-030-53058-7
eBook Packages: MedicineMedicine (R0)