Abstract
Pituitary magnetic resonance imaging (MRI) is an important diagnostic step in children suspected to have central nervous system (CNS) lesions based on growth failure, abnormalities in pubertal timing, symptoms of mass effect such as visual field changes, or known pituitary deficiencies. This chapter reviews the specifics regarding how pituitary MRIs should be ordered as well as basic principles of interpretation, in order to aid in initial evaluation and triaging of these children. Of note, MRI is nearly always preferred over computed tomography (CT) for initial evaluation of the pituitary, both to avoid ionizing radiation and to better visualize anatomy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Important Imaging Considerations
Ordering an MRI
In order to assess for pituitary abnormalities, brain magnetic resonance imaging (MRI) should typically be ordered with the “pituitary protocol,” meaning that the brain is imaged using “thin cuts” (1-mm cuts) through the sellar and suprasellar region, with imaging performed both pre- and post-administration of gadolinium-containing contrast. Depending on the radiology services available, radiologists may further refine the scanning methodology based on clinical history.
Planning for Sedation or Child Life Services
Younger children will typically require conscious sedation or anesthesia, in order to undergo an MRI of acceptable quality, and older children may benefit from Child Life services to help them tolerate the scanning procedures. The need for anesthesia, conscious sedation, and/or child life support should be planned in advance with the imaging facility.
Other Patient-Related Considerations
Pituitary MRIs should be performed with contrast; thus, children will require intravenous (IV) catheter placement. Gadolinium-containing contrast agents are typically used for MRI and are generally safe, but children with known previous allergic reactions to gadolinium may require pre-treatment with diphenhydramine and/or glucocorticoids. In these cases, radiology should be contacted prior to scanning so that a different contrast agent can be used if possible.
Children with metal implants may not be able to safely undergo an MRI, and consultation with a radiologist regarding whether the implant is MRI-safe may be warranted. Children with braces may safely undergo MRI, but the images are often quite poor because of artifact from the braces. Whenever possible, it is best to have braces removed before a brain MRI to ensure that the images are usable.
Interpretation of Scans
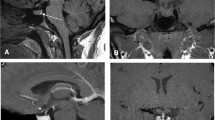
Interpretation by a radiologist is required for definitive reading of pituitary MRI scans, but we encourage treating physicians to look at the images as well. Helpful pituitary landmarks on coronal and sagittal scans are shown in Fig. 37.1. Table 37.1 lists common imaging terms and anatomical terms that may be helpful when reading pituitary MRI reports. Table 37.2 describes common pathological findings in imaging reports and discusses next steps for managing these findings. Please note that Table 37.2 does not include all possible suprasellar findings, and a finding of suprasellar tumor should generally prompt emergent referral to oncology or an emergency department, as well as urgent endocrine assessment. A pituitary MRI showing a craniopharyngioma is shown in Fig. 37.2. Further management of pituitary and suprasellar lesions is described in Chap. 56.
Figure shows T1 coronal (a) and sagittal (b) pituitary MRIs without visible abnormalities to illustrate landmarks on Pituitary MRI. 1A, Coronal View: The Cavernous Sinuses lie on either side of the pituitary gland and are outlined in yellow. The internal carotid arteries (ICA), indicated with red arrows, run through the cavernous sinuses. The pituitary gland, pointed to by the white arrowhead, lies in the sella turcica, between the cavernous sinuses. The optic chiasm lies above the pituitary gland; its left and right boundaries are demarcated by the white arrows. The stalk is not highly visible on this cut and lies between the pituitary and the optic chiasm. The hypointense (nearly black) area below the pituitary is the sphenoid sinus (SS). 1B, Sagittal View: Again the pituitary is pointed to by the white arrowhead. The pituitary stalk can be seen leading from the hypothalamus to the pituitary, as demarcated by the white arrows. The hyperintense “posterior pituitary bright spot,” which results from granules of stored vasopressin, is noted by the red arrow. Again the hypointense (nearly black) area below and anterior to the pituitary is the sphenoid sinus (SS). The pons and corpus callosum (CC) are also noted as important landmarks for the sagittal pituitary view
A coronal scan showing a craniopharyngioma (white arrows) in a female child. The optic chiasm is displaced upward, as noted by the white arrowhead, in comparison to the normal horizonal appearance noted by the yellow arrowhead in the coronal reference scan from Fig. 37.1
Tips on discussing results with patients are shown in Table 37.3. Pituitary or suprasellar lesions ≥ 10 mm should almost always prompt urgent or emergent referral, but smaller lesions need not necessarily raise substantial alarm. For example, most Rathke’s cleft cysts are completely benign and do not require intervention, and most pituitary microadenomas are benign as well, although some will require medical or surgical intervention. Please see Table 37.3 for suggested language around these findings.
References
Hall WA, Luciano MG, Doppman JL, Patronas NJ, Oldfield EH. Pituitary magnetic resonance imaging in normal human volunteers: occult adenomas in the general population. Ann Intern Med. 1994;120:817–20.
Zada G. Rathke cleft cysts: a review of clinical and surgical management. Neurosurg Focus. 2011. 31:1–6. https://doi.org/10.3171/2011.5.FOCUS1183.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stanley, T. (2021). Pituitary MRI. In: Stanley, T., Misra, M. (eds) Endocrine Conditions in Pediatrics. Springer, Cham. https://doi.org/10.1007/978-3-030-52215-5_37
Download citation
DOI: https://doi.org/10.1007/978-3-030-52215-5_37
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-52214-8
Online ISBN: 978-3-030-52215-5
eBook Packages: MedicineMedicine (R0)