Abstract
Socio-economically disadvantaged individuals and societies suffer a disproportionately high burden of oral diseases than their advantaged counterparts almost universally. Studies that examine socio-economic inequalities in oral health have applied many individual- and household-level measures of social position: income, education, occupation and social class. Social inequalities in oral health are also evidenced between populations using measures of area-level disadvantage, including country-level income, gross domestic product, gross national income, deprivation, social development and income inequality. Despite capturing some form of social disadvantage, each measure uniquely represents an underlying social and economic process that is shaped politically and historically; ignoring which can be misleading in understanding the extent of oral health inequalities, and most importantly, its solutions. Apart from the choice of measure, the scale on which socio-economic inequality in oral health is measured is of key importance. Oral health inequalities can be presented in absolute and relative scales. Strategies to reduce inequalities on one scale may insufficiently address inequalities on the other scale. Finally, discussion on epidemiological tools and theoretical explanations that enhance the current understanding of socio-economic inequalities in oral health is vital. This chapter discusses oral epidemiological research on socio-economic inequalities in oral health with an emphasis on the measurement of socio-economic inequalities in oral health, theoretical explanations and epidemiological methods that can assist in improving current knowledge on social inequalities in oral health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning ObjectivesAfter reading this chapter you will be able to:
-
Identify reasons why examining socio-economic inequalities in oral health is important
-
Understand theoretical explanations for socio-economic inequalities in oral health
-
Recognise different methodological aspects of examining socio-economic inequalities in oral health
-
Identify opportunities in recent developments in epidemiology that can enhance current understanding of socio-economic inequalities in oral health
1 Introduction
More socially advantaged people and societies are reported to have better health outcomes and life expectancy than their disadvantaged counterparts, almost universally. Oral health outcomes do not differ from other health outcomes in this regard. Systematic reviews have confirmed associations between socio-economic disadvantage and oral health outcomes of dental caries, dental care utilisation, oral cancer, tooth loss and traumatic dental injuries, periodontal disease and poor quality of life [1,2,3,4,5,6,7,8,9,10,11]. Individual studies have confirmed socio-economic inequalities in oral health outcomes in both high as well as low- and middle-income countries [12,13,14,15,16]. When socio-economic inequalities in oral health outcomes are compared with general health outcomes within a country, often inequalities in oral health outcomes are more pronounced than those in general health outcomes [17, 18]. Studies that have examined trends in oral health inequalities over time have also confirmed that improvements in oral health outcomes have not been consistent across socio-economic groups [13, 19,20,21]. Majority of the research on socio-economic inequalities in oral health is descriptive, reporting associations between one or more measures of socio-economic disadvantage and oral health outcomes at the national and sub-national level. This body of evidence has helped establish the extent and nature of oral health inequalities across societies and the persistent and pervasive nature of socio-economic inequalities in oral health [22]. However, it also places onus on oral health researchers and advocates to have an improved understanding of the causes of oral health inequalities with the motive to find solutions that can address this societal challenge.
Several shifts have acted as fulcrum points for the change in the theoretical understanding of oral health inequalities and potential solutions. Major ones include the shift from attention to determinants of oral health at the individual level to those at the population level [23, 24], from biomedical aetiological models of oral diseases to a social determinants model of disease aetiology [22, 25], and the failings of individually oriented behavioural change strategies [26], paving ways to interventions targeting environments and placing lesser responsibility on already disadvantaged individuals. Achievements in the theoretical understanding of oral health inequalities are to be supported with robust and actionable evidence from oral epidemiological investigations to help policymakers make evidence-informed decisions on solutions to address oral health inequalities. Often, equity impacts of public health interventions are not studied, and even well-intended interventions (media campaigns, workplace smoking bans) can increase socio-economic inequalities in health outcomes [27]. Therefore, oral epidemiologists have a vital role to play in checking and confirming such popular assumptions.
It is now widely recognised in oral epidemiology that socio-economic determinants of oral health exist beyond the control of individuals. This is substantiated by increased application of the multilevel analytical framework and its corresponding techniques [28]. Traditionally, randomised controlled trials have dominated as the most reliable source of evidence for the effectiveness of public health interventions. However, large-scale trials with sufficient follow-up are next to impossible with many social exposures as they are determined politically (e.g. changes in income distribution as an intervention). In epidemiology and social epidemiology, there is increased utilisation of observational data by using methods based on potential outcome approaches to estimate and inform the causal effects of exposures onto health outcomes [29]. However, their application has been relatively limited in oral epidemiology, mainly to explain the relationship between socio-economic disadvantage and oral health outcomes. There is also a greater emphasis on the need for conducting more ‘consequential’ research that leads to inform specific interventions for improving population health [30]. Epidemiology is also witnessing an interesting intersection of methods from data science such as machine learning for better prediction of exposure groups [31] and computational simulation models [32] that provide unique opportunities to understand better the potential of public health interventions in reducing the population burden of diseases as well as associated inequalities. The shift mentioned above in theoretical thinking related to the understanding of drivers of oral health inequalities at the population level needs to be occurring similarly in oral epidemiological studies of oral health inequalities, without neglecting the fundamental concepts related to investigations on social inequalities in health.
In this chapter, we discuss important methodological aspects related to investigating socio-economic inequalities in oral health. Core methodological aspects, along with some recent developments in the social epidemiology will be highlighted, keeping in mind their relevance to operationalisation in oral health research. Additionally, social epidemiology and the studies of socio-economic inequalities in health are plagued with terminologies that are overlapping but have different meanings. Often, naively there has been interchangeable use of these terminologies (e.g. health inequalities, health inequities, health disparities; social position, socio-economic position, social class and social status) in health research. Although they may generally refer to a similar phenomenon, they involve different underlying theories, whose interchangeable use often masks nuances of definition. New researchers to health inequalities research and students may find this daunting to grasp and difficult in circumventing this issue. Readers will be directed in this section towards some useful glossaries that they may find helpful for avoiding such practices. Measurement of oral health inequalities requires attention to scales on which they are measured [33]. Discussion on different scales of measurement is critical as policy responses to address oral health inequalities are likely to be different based on the choice of scales [34]. Additionally, we discuss some of the main social and epidemiological theories advanced to explain why and how social inequalities in oral health occur.
Certain caveats of this chapter must be highlighted to the readers. In this chapter, we have not attempted to review the extent and magnitude of socio-economic inequalities in every oral health outcome. We opted to provide a general theoretical overview along with a stronger emphasis on the methodological issues related to oral health inequalities research. Additionally, due to the evolving nature of research on social inequalities in health, readers are advised to use the presented material more as a platform to enhance their understanding of research on socio-economic inequalities in oral health rather than as a definitive set of rules to follow.
2 Key Motivations for Investigating Oral Health Inequalities
The World Health Organization defines health inequalities as the differences in health status, or in the distribution of health determinants, between different population groups [35]. Gene expressions and constitutional variations among individuals can result in variations in health status within populations. Due to the ageing process, with increasing age people may have relatively worse health outcomes than their younger counterparts. For example, the prevalence of periodontal disease is negligible among children and adolescents. Consequently, periodontal disease varies according to age-groups within populations. However, variations in health outcomes according to social disadvantage (social inequalities in health) have three distinguishing features that separate them from variations in health according to other characteristics. They are systematic, socially produced (hence modifiable) and unfair. Despite differences in magnitude and extent of inequalities, social patterning in health outcomes is universal. Therefore, they are intrinsically systematic. Second, health differences of this nature are not produced biologically but rather are a consequence of social processes. Therefore, social inequalities in health can be addressed by altering the underlying social processes. Finally, social inequalities in health are unjust and unfair [36].
The case for understanding and addressing social inequalities in health (and oral health) is profound. Social epidemiology as a discipline strives to understand how social interactions and purposive human activity affect health. Innumerable past and present social arrangements that exist within societies lead to differential exposures and differences in health status between individuals that comprise a population. The Nobel Prize winner and developmental economist Amartya Sen argues that ‘in any discussion of social equity and justice, illness and health must figure as a major concern’. He justifies his arguments using a social justice framework. Health equity should be a central feature of the justice of social arrangements. Being healthy allows human capabilities to flourish as they get free from escapable illness, avoidable afflictions and premature mortality. Under this notion, it is serious injustice to preclude some individuals from these opportunities due to the inadequate social arrangements. Of note, illnesses that are not prevented and go untreated for social reasons such as lack of resources, rather than out of personal choice, have a particularly negative implication to social justice [37].
Despite being largely preventable, oral diseases continue to affect individuals due to social reasons. Socially disadvantaged people suffer a double burden because they face significant challenges concerning preventive and routine dental care in addition to already established social inequalities expressed in major oral health risk factors including tobacco use, unhealthy diet and oral hygiene in societies [38,39,40,41,42,43,44]. Epidemiological research on social inequalities in oral health is vital to document the extent of social inequalities in oral health within and between societies [13]. For example, it allows assessing whether social inequalities in oral health within a population has increased or decreased over time. Comparisons in social inequalities in oral health between population groups are also essential to understand the underlying social, economic and political reasons due to which one population may have lower social inequality in oral health than another [45,46,47]. Other motivations may include identifying social groups that are most vulnerable to poor oral health, and strategies may be adopted to scale existing policies to reduce the high levels of disease within specific population sub-groups [48, 49]. Equity impacts of health policies are equally important as is their ability to lead to reductions in overall rates of diseases. Surveillance activities to track and monitor oral health inequalities play a central role in generating hypotheses on the effectiveness of oral health policies and healthcare arrangements in reducing oral health inequalities. Oral epidemiology also has a central role in providing a better understanding of causal pathways through which social disadvantage leads to specific poor oral health outcomes [50, 51]. A better understanding of causal pathways is fundamental to the development of policies and strategies to reduce existing and future levels of oral health inequalities within and between societies.
3 Theoretical Explanations for Socio-Economic Inequalities in Oral Health
Theoretical explanations for explaining socio-economic inequalities in oral health have a crucial role to play in determining the potential of interventions in reducing inequalities. Therefore, substantial debates in the discipline of epidemiology and social epidemiology have emerged on the relevance of theoretical pathways. Although outstanding records of historical discussions on the relationship between different forms of social disadvantage and health were reported historically in works of Edwin Chadwick, Rudolf Virchow, John Snow and Frederick Engels, formal theories for the relationship between social inequality and health were only first reviewed in the Black Report [52].
Four theoretical categories were proposed to explain socio-economic inequalities in health in the Black Report – artefact; theories of natural or social selection; materialist or structuralist explanations and behavioural/cultural explanations [52, 53].
Artefact: The artefact explanations explain inequalities in health as a construct of the measurement process. It posits that the association between social position and health is a statistical artefact, which is a consequence of how social status has been classified or measured over time [52]. The fact that social inequalities in health outcomes, including oral health outcomes, have been presented with so many different markers of social disadvantage over time raises severe doubts on the validity of the Artefact category [54].
Theories of Natural or Social Selection : This theory is based on the premise of reverse causation – health leads to social disadvantage and not the other way around [52]. This theory can also be refuted on the basis that large number of longitudinal studies [55, 56], including birth cohort studies [57,58,59], establish that prior exposure to social disadvantage leads to poor health outcomes in future [54].
The two theoretical categories (artefact and natural/social selection) do not hypothesise how social disadvantage leads to poor health outcomes or the causal relationship between social disadvantage and poor health outcomes. On the contrary, materialist or structuralist explanations and behavioural/cultural explanations provide causal hypotheses on how social disadvantage may lead to poor health outcomes.
Materialist or Structuralist Explanations : The materialist explanation places importance on the role of economic and socio-structural factors in the distribution of health and well-being. This line of explanation for variations in health status is consistent with the radical Marxian critique of the direct impact of economic conditions on health outcomes. Variations in rates of mortality are attributed to exploitation and poverty. The theoretical framework stresses the role of material deprivation in the social production of disease. The materialist explanation is contested because variations in health status are still observed in societies that have achieved high levels of economic development. Material deprivation and labour exploitation in such societies are minimal due to trade-union organisations and wage council machinery. A counter-argument to this limitation is that in countries that have achieved high levels of economic development, relative rather than absolute deprivation in terms of health resources and material circumstances are more relevant. Consequently, relative deprivation leads to variations in health status according to social positions [52].
Behavioural/Cultural Explanations: A behavioural/cultural approach is based upon the independent and autonomous causal role of health behaviours in morbidity and mortality. One version of this theoretical approach values individuals as a unit of analysis. Consequently, this approach stresses lifestyle and irresponsible behaviour of individuals among certain social groups as the reasons for poorer health. The underlying reasons for such behaviour include lack of education, knowledge and attitude towards healthy behaviour. Another more theoretically developed version relates to the ‘culture of poverty’ hypothesis. This approach considers the process of biological and social adaptation at lower levels of social position leading to a structure of norms, ideas and behaviours. This culture develops integrity and stability over time due to its role in helping individuals cope with their environments and impacts on their socialisation practices, and therefore, on their health behaviours [52].
Theories of social epidemiology, including materialist/structural and behavioural/cultural explanations, are grounded in social relations and systematic distribution and misallocation of social resources relevant to health.
A psychosocial theory focusing on the role of constant stress arising from feelings of lack of control and relative disadvantage among individuals lower in the social hierarchy to those who are more advantaged in the aetiology of poor health outcomes is also postulated [41, 43, 50, 60].
The Black Report concluded that choosing between these complex and competing theoretical approaches may be difficult; whereas the authors believe that the best answer lies in the materialist explanations [52]. The theoretical approaches discussed in the Black Report have been both used to explain health inequalities (differences in health among social groups within a society) as well as differences in average health of societies according to their level of social inequality (studies of social ecology) [53]. However, some specific theories/theoretical approaches aim only to explain the relationship between social inequality and average health status at the levels of different geopolitical units [53]. These theoretical explanations are synthesised below.
-
1.
Materialist: The materialist explanations stress the role of environmental factors on health, which tend to vary according to the degree of income inequality of society. Macroeconomic factors such as unemployment and levels of economic development lead to hazardous work and living environments that lead to poorer health on average [61].
-
2.
Behavioural: The behavioural explanations state that more unequal societies produce more unhealthy behaviours compared to equal societies. This fact is either due to individual inadequacies and/or due to the presence of social gradients in health behaviours [61].
-
3.
Psychosocial: At an individual level, the psychosocial explanation claims that inequality impacts on health in two different ways. First, people’s perception of their position in the social hierarchy affects health. Second, lack of control and lower levels of social hierarchy leads to persistent stress that can physiologically lead to poor health or health-damaging behaviours that consequently lead to poorer health. Compared to an equal society, in a more unequal society, there is a higher degree of social evaluative threats (comparisons between people). When added to the lack of control and coping strategies, it leads to higher levels of persistent stress. Therefore, a more significant decrement in power and control across the social hierarchy in more unequal societies leads to poorer health on average [53, 62,63,64].
-
4.
Social Capital: Social capital explanations branch out from the psychosocial explanation as this theory posits that an unequal distribution in income undermines trust and damages social relationships at a population level [65]. The lack of trust and social support are the critical reasons for poorer population health in unequal societies [66].
-
5.
Neo-Material: In contrast to the psychosocial and the social capital theories, the neo-material theory posits that more unequal societies tend to have a cluster of lack of material resources and systematic underinvestment in social infrastructure, such as public policies in health, which leads to poorer health at a population level [67,68,69].
Among the different theoretical explanations, a significant debate in social epidemiology persists about the relevance of psychosocial and social capital pathways in comparison to the neo-material pathway to explain the negative impact of social inequality on population health [53, 62,63,64, 67,68,69,70,71]. An underlying sociological distinction between the two positions is that while the psychosocial and social capital pathways originate from a Durkheimian perspective on collective consciousness and social integration, the neo-material pathway stems from Marxist or rational choice orientation [65]. Due to the difference in the origin of the theories, a conceptual challenge also relates to the interpretation of what aspects of social inequality does income inequality capture that is related to poor health or higher mortality rates at the population level. Those supporting the neo-material pathway identify income inequality as a product of structural socio-political determinants such as the dominant political paradigm, the welfare state, social class relations, including exploitation due to unequal distribution of production resources. On the other hand, supporters of psychosocial and social capital pathways identify income inequality as an operational measure of social stratification and hierarchy. They argue that the detrimental impacts of income inequality are related to a higher degree of social stratification. A high degree of social stratification in unequal societies results in loss of trust, social support and social cohesion. Through jealousy, it leads to adverse psychological impacts on individuals across the social hierarchy.
4 Operationalisation of Theoretical Explanations for Socio-Economic Inequalities in Oral Health
Sisson [50] reviewed the application of theoretical explanations for social inequalities in health, particularly in the context of oral health. Four theoretical explanations (materialist, cultural/behavioural, psychosocial and life-course perspective) were discussed.
Concerning the materialist explanation, lack of access to dental services, low purchasing power for a healthy diet and lack of access to fluoridated water due to social disadvantage were identified as primary forms of material disadvantage.
Despite the criticism of behavioural/cultural explanations for social inequalities in health in the Black Report itself, interventions for improving oral health at the population level have been directed mainly to changing individual health behaviours [26]. Studies from Australia and the US have confirmed that adjustment of oral health behaviours could not explain observed socio-economic inequalities in oral health outcomes [39, 41, 43].
Studies that tested psychosocial factors (psychological distress, allostatic load and cognitive ability) as explanations for oral health inequalities found limited support [42, 60, 72].
Oral health presents all requisites to adopt a life-course framework. Most oral diseases and disorders of public health importance are relatively common, they are cumulative and chronic, take time to develop and are mostly preventable. Different theories are proposed to explain how harmful and beneficial exposures to ill-health over the lifespan act. Programming or critical period effect states that exposure occurring during the crucial developmental period leads to a condition later in life. The critical period with effect modifier postulates that critical early-life exposures interact with later ones. The accumulation of risk models proposes that detrimental and beneficial exposures accumulated through life, affect health and finally, the chain of risk model states that one exposure leads in a reasonably linear way to another to influence health later in life [73].
Evidence on life-course theory in oral health is available from very few population-based birth cohorts which included dental/oral health clinical assessments over time. Notably, The Dunedin Multidisciplinary Health and Development Study, which started in 1972 in New Zealand and 1982, 1993, 2005 and 2015 Pelotas (Brazil) birth cohort studies are still active. The Dunedin Study used a mix of socio-economic indicators to assess socio-economic position at cohort participants in childhood. Dental plaque, gingival bleeding, periodontal diseases and decayed surfaces at aged 26 were negatively associated with childhood socio-economic status. As socio-economic status increased, the amount of poor oral health indicators decreased even after controlling for childhood health and adult socio-economic status. Moreover, low adult socio-economic status had a significant effect on poor adult dental health after controlling for low childhood socio-economic status [57].
Findings from the 1982 Pelotas birth cohort studies showed that poverty over at least one stage of life had harmful effects on adolescent’s (aged 15) dental caries, oral health-related behaviours and dental service usage. Upwardly mobile income between childhood and adolescence improved dental care [59]. At 24 years of age, the study findings showed that poverty experience in early life was associated with unsound teeth. Moreover, the number of episodes of poverty over life increased the prevalence of unsound teeth [74]. Later on, at the age of 31 years, Schuch et al. showed that adults belonging to low and fluctuating income trajectories from childhood to adulthood had twice as much the prevalence of periodontitis than participants with stable high-income trajectories [75]. The direct effect of early in life occurrences of poverty on periodontitis in adulthood was also reported [56]. On the other hand, in the 2004 Pelotas birth cohort study, differences in income trajectories from childhood to young adulthood were associated with the management of dental caries-treated and untreated rather than in the experience of the disease [76].
A scoping review examined evidence on the application of theories in the relationship between area-level social inequality and population oral health outcomes [51]. Authors noted that psychosocial theories were the most used. Although studies often mentioned theories, the majority of selected studies did not test any theory. Therefore, there is a need for explicit testing of theoretical explanations for oral health inequalities.
5 Measurement of Socio-Economic Inequalities in Oral Health
5.1 Different Types of Measures of Social Inequality
Conceptual clarity on what socioeconomic parameters must be measured and why is vital for monitoring and understanding socio-economic inequalities in oral health [77]. Of critical importance is the difference between social class, socio-economic position and socio-economic status as they continuously appear and are mistakenly used interchangeably in studies on social inequalities in (oral) health.
Social class refers to groups originating from relationships that are economical and are determined by a society’s forms of property, ownership, labour and dependencies through production, distribution and consumption of goods, services and information. It is not an ‘a priori’ property of individual human beings, but it is an outcome of a social relationship created by societies [77]. Of significant value is the importance of power and exploitation in the class relationships where resource owners gain economically from non-owners. Therefore, the relational aspect of social class distinguishes it from the stratification-based approaches. For more information on applied measures of social class, check the references (78,79,80,81,82,83). Several studies have applied social class measures in oral health literature [84,85,86,87].
Socio-economic position is an aggregate concept that comprises of both resource-based and prestige-based measures and relates to both childhood and adulthood social position. Resource-based measures are material and social resources and assets such as income, wealth and education. While prestige-based measures reflect an individual’s rank in a social hierarchy, referring to people’s access to and consumption of goods, services and knowledge as an outcome of their occupational prestige, income and education [77]. A good description of measures of socio-economic position, including advantages, disadvantages and relevance at different life-stages is described in the cited glossary [88]. Several reviews have summarised evidence on these socio-economic measures and oral health outcome(s) [3, 11, 55, 89, 90].
A study on German and Swedish adults reported low correlations between education, income and occupational class and reported a varying magnitude of associations between each of the measures and outcomes of diabetes, mortality and morbidity due to myocardial infarction and all-cause mortality [91]. It is usual in epidemiological research to mutually adjust for another measure of social position when estimating the causal association between one measure and a health outcome, for example, adjusting for education or occupation when examining the association between income and oral health. However, careful consideration is needed because the effect of education on health can be both direct and mediated through occupation and income. Similarly, the effect of occupation can be both direct and mediated via income but confounded by education. Finally, the effect of income can be confounded by occupation and income [92]. Clarity on the inter-relationships between social exposures and their roles as mediators, confounding factors and effect measure modification is key to assessing social inequalities in oral health and remove systematic sources of bias.
5.2 Levels of Aggregation
5.2.1 Socio-Economic Variations in Oral Health Between Populations
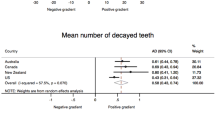
Majority of studies on socio-economic inequalities in oral health examine variations in oral health outcomes within a population according to a measure of social position (e.g., variations in dental caries according to educational attainment within Australia or test association between education and oral health outcome within Australia). Mainly, these are attributes of individuals or households. Alternatively, one can examine variations in oral health between populations. Populations and societies differ in their socio-economic characteristics. For instance, countries have differences in average income, distribution of income, proportion educated, level of social development and so on. Variations in oral health outcomes are confirmed according to country-level socio-economic characteristics [93,94,95,96]. At the sub-national level, studies have reported associations between area-level social disadvantage and oral health outcomes [97,98,99,100,101,102,103,104]. The reasons why variations in oral health outcomes must be examined between populations were described in detail previously [28]. The main reasons are as follows: there is growing evidence on the independent contribution of contexts in shaping oral health; variations in population oral health reveal underlying societal determinants; oral health determinants have a socio-political and multilevel nature; individual-level studies have a limited explanatory potential for population oral health ; and finally, the need of informing strategies for prevention of oral diseases.
5.2.2 Fallacies Arising due to Misspecification of Variables or Level
Four different types of fallacies (ecological, atomistic, sociologistic and psychologistic) can occur due to either measurement issues or when the variable(s) from other levels of social organisation are ignored. An ecological fallacy can occur when associations between individual-level socio-economic exposure (e.g., individual-level income) and oral health outcomes are inferred from the observed associations at the group level (ecologic exposures (e.g., area-level mean income) and aggregate outcomes). Alternatively, if an association between ecologic exposures (e.g., area-level mean income) and aggregate outcomes is inferred from observed associations between individual-level socio-economic exposure (e.g., individual-level income) and oral health outcomes then it is a case of atomistic fallacy. The other types of fallacies, the sociologistic and psychologistic, may occur when the variable(s) from other levels of social organisation are ignored. The sociologistic fallacy occurs when the role of individual-level factors (confounding, effect modification and mediation) is ignored in the group-level associations. Alternatively, psychologistic fallacy may occur when the role of group-level is ignored in the individual-level associations [28].
There are two main reasons for the use of area-level measures of socio-economic position. First, when there is a lack of individual-level data on socio-economic position, area-level socio-economic measures may be used as proxies. However, the individual-level socio-economic position often varies among areas and, therefore, using area-based measures can be misleading. When individual-level inferences are drawn from such studies, then the ecological fallacy cannot be ruled out [105, 106]. Second, area-level measures must be used when the socio-economic status of the context is the ecologic exposure of interest. Aggregated measures of socio-economic position have meanings that cannot be attributed to individuals, for example, income inequality is a measure of the distribution of income within a population and cannot be measured in an individual. A large volume of evidence in epidemiology [69] as well as in oral health [51] has examined income inequality as exposure of interest. In this case, measures of social disadvantage at the area level are treated as independent exposures rather than proxies for individual socio-economic disadvantage. Hence, the use of area-level socio-economic exposures must be theoretically supported. In addition to conceptual clarity and theoretical relevance of an area-level socio-economic exposure, several methodological aspects related to operationalising their research must be considered (types of cross-level associations, meaningful population groups, scale and unique characteristics, power and sample size, role of lag times and confounding by measures at alternate level of social organisation) [28].
5.2.3 Analytical Approaches
Ecological analysis and multilevel modelling are two main analytical approaches when dealing with area-level socio-economic exposures and oral health outcomes. In ecological analysis, associations are tested between group-level exposures (e.g. area-level mean income, area-level income inequality and the proportion of adults with university education) and aggregated oral health outcomes (e.g. proportion of adults with tooth loss, oral cancer notification rates). The ecological analysis is valuable for hypothesis generation and for examining variations in aggregated oral health outcomes according to policies implemented at group level [94,95,96, 107, 108]. However, they have many limitations among which ecological fallacy is critical. Additionally, the ecological analysis uses data generated only at one level (group level).
Multilevel modelling has many benefits as it utilises data across multiple levels of social organisation. First, inter-individual variations in oral health outcomes can be partitioned at different levels of social organisation to quantify how much context matters. Then, the contribution of specific group-level socio-economic exposures (e.g., area-level mean income, area-level income inequality, the proportion of adults with university education) in area- and individual-level variations in oral health outcomes can be quantified. Finally, associations between specific group-level socio-economic exposures and oral health outcomes of interest can be tested accounting for both group- and individual-level covariates simultaneously. Therefore, providing the opportunity to comprehensively examine the relationship between area-level socio-economic exposures and oral health outcomes [28, 109,110,111,112]. Multilevel modelling has been adopted with enthusiasm in oral health literature [110, 112,113,114,115,116,117,118,119,120]. However, most multilevel analyses in oral epidemiology is cross-sectional where the temporal order between exposure and outcome cannot be established.
5.3 Composite Measures of Socio-Economic Inequalities in Oral Health
For comparisons between populations and within populations over time, socio- economic inequalities in oral health outcomes can be estimated using composite or summary measures of inequality as they provide a common reference point for comparisons. Different types of measures are described below [33]:
-
1.
The Rate Ratio of Lowest versus Highest Socio-Economic Group: The two groups must not be so extreme that composite measures ignore the majority of health inequalities and are sensitive to the idiosyncrasies of the two groups. However, they should also not be broad that composite measures do not reflect the extent of inequalities [33].
-
2.
The Rate Difference of Lowest versus Highest Socio-Economic Group: Compared to rate ratio, this measure is the difference in health status between the lowest and highest socio-economic group [33].
-
3.
Regression-Based Relative Effect Index: A regression model is fitted whereby morbidity and mortality rates are regressed onto socio-economic measures. The measures for the socio-economic position must be on an interval scale [33].
-
4.
Regression-Based Absolute Effect Index: Untransformed morbidity and mortality rates are regressed onto continuous measures of socio-economic exposures [33].
-
5.
Population-Attributable Risk (Relative): This is the proportional reduction in overall morbidity and mortality rates occurring when hypothetically everyone experiences the rates of the highest socio-economic group. It is estimated as the difference between the overall rate and the rate for the highest socio-economic group [33].
-
6.
Population-Attributable Risk (Absolute): The absolute population-attributable risk is obtained by multiplying population attributable risk with the overall rate.
-
7.
Regression-Based Population-Attributable Risk (Relative): First, the regression-based relative effect index is estimated. The population-attributable risk is estimated from the predicted rate estimated for the highest socio-economic group [33].
-
8.
Regression-Based Population-Attributable Risk (Absolute): This is obtained by multiplying by the morbidity or mortality rate in the whole population [33].
-
9.
Index of Dissimilarity: This index shows the percentage of all cases that should be redistributed to obtain a similar rate of morbidity and mortality for all socio-economic groups [33].
-
10.
Relative Index of Inequality: The relative index of inequality takes into account both the population size and the relative socio-economic position of groups. For its calculation, the morbidity and mortality rates of socio-economic groups are regressed onto the proportion of the population having a higher position in the social hierarchy. The estimated relative index of inequality can be interpreted as the ratio of morbidity/mortality rates of those at the bottom to those at the top of the hierarchy on the basis of association between morbidity/mortality and socio-economic position for all groups [33].
-
11.
Slope Index of Inequality: This measure is the absolute analogue of the slope index of inequality. Inequality is presented as rate differences rather than rate ratios [33]. It represents the linear regression coefficient showing association between level of health in each socio-economic category and the ranking of socio-economic category on the social scale [121].
-
12.
Concentration Index: This index is based on a ‘concentration curve’ where the x-axis is the cumulative proportion of people by their socio-economic position starting with those lowest and finishing with those highest and the y-axis represents the cumulative total proportion of health in these people. It ranges from −1 to 1; if all health was concentrated at the highest socio-economic position, then the concentration index will be 1 and vice-versa [121].
-
13.
Symmetrized Theil Index: A Symmetrized Theil Index is the average of Theil Index and Mean Log Deviation (widely used measures of income inequality (a measure of divergence)). [122].
-
14.
Gini Index: The Gini Index is based on the Lorenz curve, where the x-axis represents the cumulative proportion of people by health status as ranked in increasing order and the y-axis represents the cumulative total proportion of health of individuals [121].
Several examples exist on the application of composite measures of inequality in oral health outcomes [17, 103, 123,124,125,126].
5.4 Measurement of Socio-Economic Inequalities in Oral Health: Scale of Measurement
When presenting socio-economic inequalities in oral health, the scales on which they are presented are of critical importance – particularly, in cases where inequality is to be compared over time. Variations in oral health outcomes between socio-economic groups can be quantified both on absolute (difference) and relative (ratio) scales. The choice between absolute and relative measures of inequality is an important consideration given the fact that progress in reducing inequalities in one scale may not apply to the other.
Harper et al. [127] reported a case in which inequality increased overtime on a relative scale and decreased overtime on an absolute scale for the same context. Celeste and Fritzell [128] examined socio-economic inequalities in oral health outcome in Sweden within a population that was followed up for 43 years. Authors found different results on the absolute and relative scale. While relative inequalities were highest earlier in life and then decreased, absolute inequalities showed an increase up to middle adulthood, and then only marginally declined. When socio-economic inequalities were compared between European countries according to their welfare typology using measures of Relative Index of Inequality and Slope Index of Inequality, again, different groups of countries emerged as problematic on the absolute as well as the relative scale of inequality [46]. Therefore, it is possible in certain situations to see a reduction in inequality on one scale and not another. In such cases, some authors preferentially may select to report inequalities on a chosen scale with favourable results providing partial or incorrect evidence. Relying exclusively on one scale of measurement rather than the other can be misleading and may not provide the complete picture of progress in the reduction of inequalities [33, 34, 129]. Ways to plot both absolute and relative inequalities over time simultaneously have also been developed and can be used for communicating the scale of inequalities comprehensively [129].
The choice of scale to assess inequalities is also relevant when the study outcomes have two bounds; e.g. attainments, as being free of caries and shortfalls, as disease manifestation. In such cases, Kjellsson et al. [130] proposed assessing inequalities using attainment-relative, absolute and shortfall-relative measures, thus avoiding the suspicion that a perspective was chosen to favour some premise.
6 Advancements
In this section, we present recent advancements in the field of epidemiology and social epidemiology that provide unique opportunities to improve current knowledge on the understanding of socio-economic inequalities in oral health.
6.1 Intersectionality Theory
Theoretical advancements in social epidemiology endorse clarifying the roles of intersection between multiple forms of social disadvantage (intersectionality) in determining health and health inequalities [131]. How one form of socio-economic position may interact with other forms of social advantage (or disadvantage) in determining oral health outcomes is not well understood. Despite knowing that social exposures and identities such as gender, ethnicity, age, education, disability, indigenous status and income are shaped by societal systems of oppression and privilege [131, 132], studies treat these measures as independent to each other concerning health. Such exercise risks considering these exposures as measures of individual risk and ignores the intersection between different forms of social identities [133]. Therefore, there is a compelling argument to apply an intersectionality framework to examine interlocking between income and other social exposures when studying the determinants of oral health and oral health inequalities [131, 132].
One way to deal with intersectionality is to test interactions between different forms of social disadvantage. However, large sample sizes with sufficient statistical power are necessary for this purpose. Multilevel regression models [28] are demonstrated to address this issue and quantify the effect of intersection between social identities in determining health status [132, 133]. Random intercepts for all possible combinations of categories of multiple exposures are fitted, and each socio-economic exposure is also included in the same model to explain variation in health status between different ‘intersections’ of social advantage and social disadvantage. The remaining variation in health status after including all social exposures in fixed part signifies the total interactive effect of multiple social exposures. Predicted estimates from multilevel models can also help profile intersectional strata according to their risk or advantage in oral health. Otherwise, when the role of other forms of social disadvantage in the relationship between income and oral health outcomes is studied through modelling interaction or effect modification, it must be assessed and reported appropriately on both additive and multiplicative scales [134].
6.2 Causal Inference and the Potential Outcome Approach
Typically, randomised controlled trials were considered as the only source of any causal evidence on the effect of an intervention on an outcome. However, they are often not possible with social exposures. Additionally, most randomised controlled trials have small follow-up periods where the life-course effects of social exposures are impossible to be studied. Instead, there is a surge in the development and application of statistical and epidemiological techniques that are based on the ‘potential outcome approach’ framework and allow for examining causal effects with observational data. By emulating randomised controlled trials in their operation, achieving exchangeability between the exposed and non-exposed, these methods are able to quantify total causal effects under strong assumptions. Examples include the estimation of causal effects of social disadvantage on health [135] or modelling utility of interventions in reducing existing socio-economic inequalities in health [136]. Also, the total causal effect can be further decomposed into natural indirect effect, the proportion of effect transmitted through measured pathways and the natural direct effect, the proportion of effect transmitted through other possible pathways by mediation analysis. This form of mediation analysis has several advantages over traditional methods such as allowing for interactions between exposure and mediators and accounting for the exposure-induced mediator outcome confounding.
It is of paramount importance that oral epidemiologists capitalise this opportunity. First, theoretical pathways through which social disadvantage lead to oral health outcomes can be quantified and better understood through causal mediation analysis. An excellent example is how sequential causal mediation analysis is applied to quantify causal effect of disability acquisition on mental health and further decomposed into material, psychosocial and behavioural pathways [137]. Policy interventions as mediators can also be set to a specific value to simulate their effectiveness in reducing oral health inequalities through estimation of the controlled direct effects [138]. It must be noted that causal modelling approaches have strong assumptions of no confounding among others. Therefore, theoretically informed directed acyclic graphs and clarity on exposure definitions will be the foundation of any causal investigation between socio-economic disadvantage and oral health outcomes [139]. Selection bias and information bias leading to differential or nondifferential misclassification of socioeconomic exposure and oral health outcomes must be carefully considered as they reduce confidence in causal estimates.
6.3 Decomposition of Socio-Economic Inequalities in Oral Health
Once health inequalities are estimated, the next step is to find explanations for the observed inequalities. Decomposing health inequalities into the factors that contribute to it can achieve this. A decomposition method was implemented by Blinder and Oaxaca (Oaxaca-Blinder decomposition technique) [140, 141], which has also been applied to decompose health inequalities into contributing factors [142, 143]. In this technique, the outcome gap between two groups is divided in a component due to differences in magnitudes of determinants of the outcome between groups and another component that is attributable to group differences in the effects of these determinants. Recently, this method has been applied in oral health to quantify the contribution of modifiable factors to area-level socio-economic inequalities in oral health in Australia [144]. It has also been applied to examine the contribution of the municipal Human Development Index in estimated mean differences in indicators of the public dental services between fluoridated and non-fluoridated municipalities in Brazil [107]. Similarly, the decomposition technique has been used to assess the contribution of demographic and socio-economic factors to oral health inequalities over time within and between Canada and the USA [145].
6.4 Simulation Modelling
Policymakers are often faced with the difficulty of making policy decisions within finite resources and political windows of opportunity. Comparisons across public health interventions in terms of their overall population health impacts as well as equity impacts are therefore necessary to make informed decisions. Programs of research that quantify health impacts of interventions (example: Assessing Cost-Effectiveness (ACE)-Prevention study) [146] allow for such comparisons, both among interventions targeting a specific risk factor and also across different health interventions. Computer simulation models help quantify the potential impact of public health interventions. Evidence confirms their application in tobacco control [147, 148], human papillomavirus (HPV) vaccination [149], dietary interventions [150], colorectal cancer screening [151] and transport [152]. In New Zealand, they have been applied to examine equity impacts of multiple tobacco control interventions [147, 153]; however, they have sparingly been applied in oral health to model equity impact of oral health interventions. This is a fertile research area, and oral epidemiologists again have an opportunity to utilise simulation modelling methods to generate evidence on long-term equity impact of dental public health interventions.
7 Way Forward and Conclusion
The burden of oral diseases and oral health inequalities is well established [22]. The recent publication of the Lancet Series on oral health recognises this challenge within the health community and provides a strong impetus to strengthen policy and research on oral health inequalities, an almost permanent associate of the burden of oral diseases [154]. Oral epidemiology will have to play a crucial role in generating quality evidence on policy solutions for reducing unfair and unjust socio-economic inequalities in oral health.
Harnessing the strengths from methodological advancements to enhance current knowledge on oral health inequalities will be a critical step. New techniques like prediction methods and machine learning, ‘a set of methods that can automatically detect patterns in data, and then use the uncovered patterns to predict future data, or to perform other kinds of decision-making under uncertainty’, are being applied within epidemiology to improve contemporary causal inference methods and exploit big data [31]. Enormous opportunities will be created to exploit such advancements for better understanding of oral health inequalities. Additionally, the use of geographic information systems, complex spatial statistics, systems science and qualitative research methods [155,156,157] can be further integrated into research on socio-economic inequalities in oral health.
In summary, it is vital to increase knowledge on policy solutions for addressing socio-economic inequalities in oral health. Theoretical and methodological aspects related to socio-economic inequalities in oral health must be considered carefully by oral epidemiologists. Methodological developments in epidemiology should be capitalised for improving the current understanding of the relationship between socio-economic disadvantage and oral health, and more importantly, the solutions for addressing oral health inequalities.
References
Almeida A, Nunes BP, Duro SMS, Facchini LA. Socioeconomic determinants of access to health services among older adults: a systematic review. Rev Saude Publica. 2017;51:50.
Boing AF, Bastos JL, Peres KG, Antunes JL, Peres MA. Social determinants of health and dental caries in Brazil: a systematic review of the literature between 1999 and 2010. Rev Braz J Epidemiol. 2014;17(Suppl 2):102–15.
Costa SM, Martins CC, Pinto MQC, Vasconcelos M, Abreu M. Socioeconomic Factors and Caries in People between 19 and 60 Years of Age: An Update of a Systematic Review and Meta-Analysis of Observational Studies. Int J Environ Res Public Health. 2018;15(8):1775.
Harris R, Nicoll AD, Adair PM, Pine CM. Risk factors for dental caries in young children: a systematic review of the literature. Community Dent Health. 2004;21(1 Suppl):71–85.
Klein J, von dem Knesebeck O. Inequalities in health care utilization among migrants and non-migrants in Germany: a systematic review. Int J Equity Health. 2018;17(1):160.
Nobrega J, Dantas E, Ferreira-Filho JC, Limao N, Rodrigues-de-Melo AC, Protasio AP, et al. Contextual social inequities and occurrence of dental caries in adolescents: a systematic review. Oral Health Prev Dent. 2017;15(4):329–36.
Rai NK, Tiwari T. Parental factors influencing the development of early childhood caries in developing nations: a systematic review. Front Public Health. 2018;6:64.
Raison H, Harris RV. Interventions to reduce socio-economic inequalities in dental service utilisation – a systematic review. Community Dent Health. 2019;36(1):39–45.
Reda SF, Reda SM, Thomson WM, Schwendicke F. Inequality in utilization of dental services: a systematic review and meta-analysis. Am J Public Health. 2018;108(2):e1–7.
Reda SM, Krois J, Reda SF, Thomson WM, Schwendicke F. The impact of demographic, health-related and social factors on dental services utilization: systematic review and meta-analysis. J Dent. 2018;75:1–6.
Schwendicke F, Dorfer CE, Schlattmann P, Foster Page L, Thomson WM, Paris S. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 2015;94(1):10–8.
Amarasena N, Ekanayaka AN, Herath L, Miyazaki H. Socio-demographic risk indicators for tooth mortality in rural Sri Lankans. Asia Pac J Public Health/Asia Pac Acad Consort Public Health. 2003;15(2):105–10.
Celeste RK, Nadanovsky P, Fritzell J. Trends in socioeconomic disparities in oral health in Brazil and Sweden. Community Dent Oral Epidemiol. 2011;39(3):204–12.
Do LG. Distribution of caries in children: variations between and within populations. J Dent Res. 2012;91(6):536–43.
Do LG, Spencer AJ, Slade GD, Ha DH, Roberts-Thomson KF, Liu P. Trend of income-related inequality of child oral health in Australia. J Dent Res. 2010;89(9):959–64.
Lopez R, Fernandez O, Baelum V. Social gradients in periodontal diseases among adolescents. Community Dent Oral Epidemiol. 2006;34(3):184–96.
Ravaghi V, Quinonez C, Allison PJ. Comparing inequalities in oral and general health: findings of the Canadian Health Measures Survey. Can J Public Health. 2013;104(7):e466–71.
Sabbah W, Tsakos G, Chandola T, Sheiham A, Watt RG. Social gradients in oral and general health. J Den Res. 2007;86(10):992–6.
Dye BA, Arevalo O, Vargas CM. Trends in paediatric dental caries by poverty status in the United States, 1988-1994 and 1999-2004. Int J Paediatr Dent. 2010;20(2):132–43.
Li KY, Okunseri CE, McGrath C, Wong MCM. Trends in self-reported oral health of US adults: National Health and Nutrition Examination Survey 1999-2014. Community Dent Oral Epidemiol. 2018;46(2):203–11.
Holst D. Oral health equality during 30 years in Norway. Community Dent Oral Epidemiol. 2008;36(4):326–34.
Watt RG, Heilmann A, Listl S, Peres MA. London charter on oral health inequalities. J Den Res. 2016;95(3):245–7.
Holst D. Causes and prevention of dental caries: a perspective on cases and incidence. Oral Health Prev Dent. 2005;3(1):9–14.
Holst D, Schuller AA, Aleksejuniene J, Eriksen HM. Caries in populations – a theoretical, causal approach. Eur J Oral Sci. 2001;109(3):143–8.
Watt RG. Social determinants of oral health inequalities: implications for action. Community Dent Oral Epidemiol. 2012;40(Suppl 2):44–8.
Watt RG. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol. 2007;35(1):1–11.
Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190–3.
Singh A, Harford J, Peres MA. Investigating societal determinants of oral health-opportunities and challenges in multilevel studies. Community Dent Oral Epidemiol. 2018;46(4):317–27.
Little RJ, Rubin DB. Causal effects in clinical and epidemiological studies via potential outcomes: concepts and analytical approaches. Annu Rev Public Health. 2000;21:121–45.
Nandi A, Harper S. How consequential is social epidemiology? A review of recent evidence. Curr Epidemiol Rep. 2014;2(1):61–70.
Blakely T, Lynch J, Simons K, Bentley R, Rose S, Reflection on modern methods: when worlds collide—prediction, machine learning and causal inference. Int J Epidemiol. dyz132, https://doi.org/10.1093/ije/dyz132.
Briggs ADM, Wolstenholme J, Blakely T, Scarborough P. Choosing an epidemiological model structure for the economic evaluation of non-communicable disease public health interventions. Popul Health Metrics. 2016;14(1):17.
Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44(6):757–71.
Mackenbach JP, Martikainen P, Menvielle G, de Gelder R. The arithmetic of reducing relative and absolute inequalities in health: a theoretical analysis illustrated with European mortality data. J Epidemiol Community Health. 2016;70(7):730–6.
WHO. Health Impact Assessment (HIA): Glossary of terms used Geneva: WHO. Available from: https://www.who.int/hia/about/glos/en/.
Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: levelling up part 1. WHO Regional Office for Europe: Copenhagen; 2006.
Sen A. Why health equity? Health Econ. 2002;11(8):659–66.
Singh A, Arora M, English DR, Mathur MR. Socioeconomic gradients in different types of tobacco use in India: evidence from global adult tobacco survey 2009-10. Biomed Res Int. 2015;2015:837804.
Sanders A, Slade G, Turrell G, John Spencer A, Marcenes W. The shape of the socioeconomic-oral health gradient: implications for theoretical explanations. Community Dent Oral Epidemiol. 2006;34(4):310–9.
Sanders AE, Spencer AJ. Social inequality in perceived oral health among adults in Australia. Aust N Z J Public Health. 2004;28(2):159–66.
Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behaviour in oral health inequalities. Community Dent Oral Epidemiol. 2006;34(1):71–9.
Sabbah W, Watt RG, Sheiham A, Tsakos G. The role of cognitive ability in socio-economic inequalities in oral health. J Den Res. 2009;88(4):351–5.
Sabbah W, Tsakos G, Sheiham A, Watt RG. The role of health-related behaviors in the socioeconomic disparities in oral health. Soc Sci Med. 2009;68(2):298–303.
Singh A, Rouxel P, Watt RG, Tsakos G. Social inequalities in clustering of oral health related behaviors in a national sample of British adults. Prev Med. 2013;57(2):102–6.
Guarnizo-Herreno CC, Tsakos G, Sheiham A, Marmot MG, Kawachi I, Watt RG. Austin Powers bites back: a cross sectional comparison of US and English national oral health surveys. BMJ. 2015;351:h6543.
Guarnizo-Herreno CC, Watt RG, Pikhart H, Sheiham A, Tsakos G. Socioeconomic inequalities in oral health in different European welfare state regimes. J Epidemiol Community Health. 2013;67(9):728–35.
Peres MA, Luzzi L, Peres KG, Sabbah W, Antunes JL, Do LG. Income-related inequalities in inadequate dentition over time in Australia, Brazil and USA adults. Community Dent Oral Epidemiol. 2015;43(3):217–25.
Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216–21.
Vanderbilt AA, Isringhausen KT, VanderWielen LM, Wright MS, Slashcheva LD, Madden MA. Health disparities among highly vulnerable populations in the United States: a call to action for medical and oral health care. Med Educ Online. 2013;18:1–3.
Sisson KL. Theoretical explanations for social inequalities in oral health. Community Dent Oral Epidemiol. 2007;35(2):81–8.
Singh A, Harford J, Schuch HS, Watt RG, Peres MA. Theoretical basis and explanation for the relationship between area-level social inequalities and population oral health outcomes - A scoping review. SSM Popul Health. 2016;2:451–62.
Townsend P, Davidson N, Black DS. Inequalities in health : the Black report. Townsend P, Davidson N, Black DS, Great Britain. Working group on inequalities in health, editors. Harmondsworth: Penguin; 1982.
Bartley M. Health inequality : an introduction to theories, concepts, and methods. Cambridge, UK: Polity Press; 2004.
McCartney G, Collins C, Mackenzie M. What (or who) causes health inequalities: theories, evidence and implications? Health Policy. 2013;113(3):221–7.
Schuch HS, Peres KG, Singh A, Peres MA, Do LG. Socioeconomic position during life and periodontitis in adulthood: a systematic review. Community Dent Oral Epidemiol. 2017;45(3):201–8.
Schuch HS, Nascimento GG, Peres KG, et al. The Controlled Direct Effect of Early-Life Socioeconomic Position on Periodontitis in a Birth Cohort. Am J Epidemiol. 2019;188(6):1101–1108.
Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, et al. Association between children's experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360(9346):1640–5.
Peres MA, de Oliveira LMR, Sheiham A, Peres KG, Barros FC, Hernandez PG, et al. Social and biological early life influences on severity of dental caries in children aged 6 years. Community Dent Oral Epidemiol. 2005;33(1):53–63.
Peres MA, Peres KG, de Barros AJ, Victora CG. The relation between family socioeconomic trajectories from childhood to adolescence and dental caries and associated oral behaviours. J Epidemiol Community Health. 2007;61(2):141–5.
Sanders AE, Slade GD, Turrell G, Spencer AJ, Marcenes W. Does psychological stress mediate social deprivation in tooth loss? J Den Res. 2007;86(12):1166–70.
MacIntyre S. The Black report and beyond: what are the issues? Soc Sci Med. 1997;44:723–45.
Wilkinson RG. Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ. 1997;314(7080):591–5.
Marmot M, Wilkinson R. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. BMJ. 2000;322:1233–6.
Martikainen P, Bartley M, Lahelma E. Psychosocial determinants of health in social epidemiology. Int J Epidemiol. 2002;31(6):1091–3.
Macinko JA, Shi L, Starfield B, Wulu JT Jr. Income inequality and health: a critical review of the literature. Med Care Res Rev. 2003;60(4):407–52.
Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–8.
Lynch J. Income inequality and health: expanding the debate. Soc Sci Med. 2000;51(7):1001–5; discussion 9-10.
Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320(7243):1200–4.
Lynch J, Smith GD, Harper S, Hillemeier M, Ross N, Kaplan GA, et al. Is income inequality a determinant of population health? Part 1. A Systematic Review. Milbank Q. 2004;82(1):5–99.
Muntaner C, Lynch J. Income inequality, social cohesion, and class relations: A critique of Wilkinson's neo-Durkheimian research program. Int J Health Serv. 1999;29(1):59–81.
Muntaner C, Rai N, Ng E, Chung H. Social class, politics, and the spirit level: why income inequality remains unexplained and unsolved. Int J Health Serv. 2012;42(3):369–81.
Sabbah W, Watt RG, Sheiham A, Tsakos G. Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: evidence from the Third National Health and Nutrition Examination Survey. J Epidemiol Community Health. 2008;62(5):415–20.
Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–93.
Peres MA, Peres KG, Thomson WM, Broadbent JM, Gigante DP, Horta BL. The influence of family income trajectories from birth to adulthood on adult oral health: findings from the 1982 Pelotas birth cohort. Am J Public Health. 2011;101(4):730–6.
Schuch HS, Peres KG, Demarco FF, Horta BL, Gigante DP, Peres MA, et al. Effect of life-course family income trajectories on periodontitis: birth cohort study. J Clin Periodontol. 2018;45(4):394–403.
Peres MA, Liu P, Demarco FF, Silva AER, Wehrmeister FC, Menezes AM, et al. Income trajectories affect treatment of dental caries from childhood to young adulthood: a birth cohort study. Braz Oral Res. 2018;32:e36.
Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78.
Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121.
Lombardi C, Bronfman M, Facchini LA, Victora CG, Barros FC, Beria JU, et al. Operationalization of the concept of social class in epidemiologic studies. Rev Saude Publica. 1988;22(4):253–65.
Berkman LF, Macintyre S. The measurement of social class in health studies: old measures and new formulations. IARC Sci Publ. 1997;138:51–64.
Barata RB, Ribeiro MC, Silva ZP, Antunes JL. Social class: concepts and operationalization models in health research. Rev Saude Publica. 2013;47(4):647–55.
Muntaner C, Borrell C, Vanroelen C, Chung H, Benach J, Kim IH, et al. Employment relations, social class and health: a review and analysis of conceptual and measurement alternatives. Soc Sci Med. 2010;71(12):2130–40.
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey SG. Indicators of socioeconomic position (part 2). J Epidemiol Community Health. 2006;60(2):95–101.
Castaneda H, Carrion IV, Kline N, Tyson DM. False hope: effects of social class and health policy on oral health inequalities for migrant farmworker families. Soc Sci Med. 2010;71(11):2028–37.
Delgado-Angulo EK, Bernabe E. Comparing lifecourse models of social class and adult oral health using the 1958 National Child Development Study. Community Dent Health. 2015;32(1):20–5.
Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. The effects of social class and dental attendance on oral health. J Den Res. 2008;87(1):60–4.
Novrinda H, Han DH, Jung-Choi K, Ryu JI. Neo-Marxian social class inequalities in oral health among the south Korean population. Community Dent Oral Epidemiol. 2019;47(2):162–70.
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey SG. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12.
Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LM. Socioeconomic inequalities and oral cancer risk: a systematic review and meta-analysis of case-control studies. Int J Cancer. 2008;122(12):2811–9.
Singh A, Peres MA, Watt RG. The relationship between income and oral health: A critical review. J Dent Res. 2019:0022034519849557.
Geyer S, Hemstrom O, Peter R, Vagero D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health. 2006;60(9):804–10.
Green MJ, Popham F. Interpreting mutual adjustment for multiple indicators of socioeconomic position without committing mutual adjustment fallacies. BMC Public Health. 2019;19(1):10.
Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J. 2003;53(5):285–8.
Hobdell MH, Lalloo R, Myburgh NG. The human development index and per capita gross national product as predictors of dental caries prevalence in industrialized and industrializing countries. Ann N Y Acad Sci. 1999;896:329–31.
Hobdell MH, Oliveira ER, Bautista R, Myburgh NG, Lalloo R, Narendran S, et al. Oral diseases and socio-economic status (SES). Br Dent J. 2003;194(2):91–6; discussion 88
Lalloo R, Myburgh NG, Hobdell MH. Dental caries, socio-economic development and national oral health policies. Int Dent J. 1999;49(4):196–202.
Aurelio Peres M, Glazer Peres K, Ferreira Antunes JL, Renno Junqueira S, Frazao P, Capel NP. The association between socioeconomic development at the town level and the distribution of dental caries in Brazilian children. Rev Panam Salud Publica. 2003;14(3):149–57.
Ekstrand KR, Christiansen ME, Qvist V, Ismail A. Factors associated with inter-municipality differences in dental caries experience among Danish adolescents. An ecological study. Community Dent Oral Epidemiol. 2010;38(1):29–42.
Tickle M, Craven R, Worthington HV. A comparison of the subjective oral health status of older adults from deprived and affluent communities. Community Dent Oral Epidemiol. 1997;25(3):217–22.
Sanders AE, Turrell G, Slade GD. Affluent neighborhoods reduce excess risk of tooth loss among the poor. J Den Res. 2008;87(10):969–73.
Locker D, Ford J. Using area-based measures of socioeconomic status in dental health services research. J Public Health Dent. 1996;56(2):69–75.
Locker D, Ford J. Evaluation of an area-based measure as an indicator of inequalities in oral health. Community Dent Oral Epidemiol. 1994;22(2):80–5.
Jagger DC, Sherriff A, Macpherson LM. Measuring socio-economic inequalities in edentate Scottish adults--cross-sectional analyses using Scottish health surveys 1995-2008/09. Community Dent Oral Epidemiol. 2013;41(6):499–508.
Jones CM, Woods K, Taylor GO. Social deprivation and tooth decay in Scottish schoolchildren. Health Bull (Edinb). 1997;55(1):11–5.
Blakely TA, Woodward AJ. Ecological effects in multi-level studies. J Epidemiol Community Health. 2000;54(5):367–74.
Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. 1998;88(2):216–22.
Godoi H, Singh A, de Mello ALSF, Brennan DS, Peres MA. Area-level social development and indicators of public dental services in Southern Brazil. Community Dent Oral Epidemiol. 2019;47(3):274–80.
Bernabe E, Hobdell MH. Is income inequality related to childhood dental caries in rich countries? J Am Dent Assoc. 2010;141(2):143–9.
Merlo J, Wagner P, Ghith N, Leckie G. An original stepwise multilevel logistic regression analysis of discriminatory accuracy: the case of Neighbourhoods and health. PLoS One. 2016;11(4):e0153778.
Antunes JL, Peres MA, de Campos Mello TR, Waldman EA. Multilevel assessment of determinants of dental caries experience in Brazil. Community Dent Oral Epidemiol. 2006;34(2):146–52.
Freire MDM, Reis SCGB, Figueiredo N, Peres KG, Moreira RD, Antunes JLF. Individual and contextual determinants of dental caries in Brazilian 12-year-olds in 2010. Rev Saude Publica. 2013;47:40–9.
Guedes RS, Piovesan C, Antunes JL, Mendes FM, Ardenghi TM. Assessing individual and neighborhood social factors in child oral health-related quality of life: a multilevel analysis. Qual Life Res. 2014;23(9):2521–30.
Aida J, Ando Y, Oosaka M, Niimi K, Morita M. Contributions of social context to inequality in dental caries: a multilevel analysis of Japanese 3-year-old children. Community Dent Oral Epidemiol. 2008;36(2):149–56.
Aida J, Kondo K, Kondo N, Watt RG, Sheiham A, Tsakos G. Income inequality, social capital and self-rated health and dental status in older Japanese. Soc Sci Med. 2011;73(10):1561–8.
Bernabe E, Marcenes W. Income inequality and tooth loss in the United States. J Den Res. 2011;90(6):724–9.
Bower E, Gulliford M, Steele J, Newton T. Area deprivation and oral health in Scottish adults: a multilevel study. Community Dent Oral Epidemiol. 2007;35(2):118–29.
Choi YH, Lee SG. Does regional socioeconomic context affect the dental caries experience? A multilevel study of Korean adults. Eur J Oral Sci. 2011;119(4):294–300.
Koltermann AP, Giordani JM, Pattussi MP. The association between individual and contextual factors and functional dentition status among adults in Rio Grande do Sul state, Brazil: a multilevel study. Cad Saude Publica. 2011;27(1):173–82.
Peres MA, Peres KG, Frias AC, Antunes JL. Contextual and individual assessment of dental pain period prevalence in adolescents: a multilevel approach. BMC Oral Health. 2010;10:20.
Turrell G, Sanders AE, Slade GD, Spencer AJ, Marcenes W. The independent contribution of neighborhood disadvantage and individual-level socioeconomic position to self-reported oral health: a multilevel analysis. Community Dent Oral Epidemiol. 2007;35(3):195–206.
Regidor E. Measures of health inequalities: part 2. J Epidemiol Community Health. 2004;58(11):900.
Borrell LN, Talih M. A symmetrized Theil index measure of health disparities: an example using dental caries in U.S. children and adolescents. Stat Med. 2011;30(3):277–90.
Antunes JL, Narvai PC, Nugent ZJ. Measuring inequalities in the distribution of dental caries. Community Dent Oral Epidemiol. 2004;32(1):41–8.
Singh A, Peres MA, Watt RG. The relationship between income and Oral health: A critical review. J Den Res. 2019;98(8):853–60.
Shen J, Wildman J, Steele J. Measuring and decomposing oral health inequalities in an UK population. Community Dent Oral Epidemiol. 2013;41(6):481–9.
Ravaghi V, Quinonez C, Allison PJ. The magnitude of oral health inequalities in Canada: findings of the Canadian health measures survey. Community Dent Oral Epidemiol. 2013;41(6):490–8.
Harper S, King NB, Meersman SC, Reichman ME, Breen N, Lynch J. Implicit value judgments in the measurement of health inequalities. Milbank Q. 2010;88(1):4–29.
Celeste RK, Fritzell J. Do socioeconomic inequalities in pain, psychological distress and oral health increase or decrease over the life course? Evidence from Sweden over 43 years of follow-up. J Epidemiol Community Health. 2018;72(2):160–7.
Blakely T, Disney G, Atkinson J, Teng A, Mackenbach JP. A typology for charting socioeconomic mortality gradients: "Go Southwest". Epidemiology. 2017;28(4):594–603.
Kjellsson G, Gerdtham UG, Petrie D. Lies, damned lies, and health inequality measurements: understanding the value judgments. Epidemiology. 2015;26(5):673–80.
Kapilashrami A, Hankivsky O. Intersectionality and why it matters to global health. Lancet. 2018;391(10140):2589–91.
Merlo J. Multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) within an intersectional framework. Soc Sci Med. 2018;203:74–80.
Evans CR, Williams DR, Onnela JP, Subramanian SV. A multilevel approach to modeling health inequalities at the intersection of multiple social identities. Soc Sci Med. 2018;203:64–73.
Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–20.
Nandi A, Glymour MM, Kawachi I, VanderWeele TJ. Using marginal structural models to estimate the direct effect of adverse childhood social conditions on onset of heart disease, diabetes, and stroke. Epidemiology. 2012;23(2):223–32.
Blakely T, Disney G, Valeri L, Atkinson J, Teng A, Wilson N, et al. Socioeconomic and tobacco mediation of ethnic inequalities in mortality over time: repeated census-mortality cohort studies, 1981 to 2011. Epidemiology. 2018;29(4):506–16.
Aitken Z, Simpson JA, Gurrin L, Bentley R, Kavanagh AM. Do material, psychosocial and behavioural factors mediate the relationship between disability acquisition and mental health? A sequential causal mediation analysis. Int J Epidemiol. 2018;47(3):829–40.
Chittleborough CR, Mittinty MN, Lawlor DA, Lynch JW. Effects of simulated interventions to improve school entry academic skills on socioeconomic inequalities in educational achievement. Child Dev. 2014;85(6):2247–62.
Fleischer NL, Diez Roux AV. Using directed acyclic graphs to guide analyses of neighbourhood health effects: an introduction. J Epidemiol Community Health. 2008;62(9):842–6.
Blinder AS. Wage discrimination: reduced form and structural estimates. J Hum Resour. 1973;8(4):436–55.
Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev. 1973;14(3):693–709.
Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. The gap of visual impairment between economic groups in Shahroud, Iran: A Blinder-Oaxaca decomposition. Am J Epidemiol. 2011;173(12):1463–7.
Jiménez-Rubio D, Hernández-Quevedo C. Inequalities in the use of health services between immigrants and the native population in Spain: what is driving the differences? The Eur J Health Econ. 2011;12(1):17–28.
Peres MA, Ju X, Mittinty M, Spencer AJ, Do LG. Modifiable factors explain socioeconomic inequalities in children’s dental caries. J Den Res. 2019;98(11):1211–8.
Farmer J, McLeod L, Siddiqi A, Ravaghi V, Quiñonez C. Towards an understanding of the structural determinants of oral health inequalities: A comparative analysis between Canada and the United States. SSM Popul Health. 2016;2:226–36.
Carter R, Moodie M, Markwick A, Magnus A, Vos T, Swinburn B, et al. Assessing cost-effectiveness in obesity (ACE-obesity): an overview of the ACE approach, economic methods and cost results. BMC Public Health. 2009;9:419.
Blakely T, Cobiac LJ, Cleghorn CL, Pearson AL, van der Deen FS, Kvizhinadze G, et al. Health, health inequality, and cost impacts of annual increases in tobacco tax: multistate life table modeling in New Zealand. PLoS Med. 2015;12(7):e1001856.
Singh A, Petrović-van der Deen FS, Carvalho N, Lopez AD, Blakely T. Impact of tax and tobacco-free generation on health-adjusted life years in the Solomon Islands: a multistate life table simulation. Tob Control. 2020;29(4):388–97.
Blakely T, Kvizhinadze G, Karvonen T, Pearson AL, Smith M, Wilson N. Cost-effectiveness and equity impacts of three HPV vaccination programmes for school-aged girls in New Zealand. Vaccine. 2014;32:2645–56.
Cobiac L, Tam K, Veerman L, Blakely T. Taxes and subsidies for improving diet and population health in Australia: A cost-effectiveness modelling study. PLoS Med. 2017;14(2):e1002232.
McLeod M, Kvizhinadze G, Boyd M, Barendregt J, Sarfati D, Wilson N, et al. Colorectal cancer screening: how health gains and cost-effectiveness vary by ethnic group, the impact on health inequalities, and the optimal age-range to screen. Cancer Epidemiol Biomark Prev. 2017;26(9):1391–400.
Mizdrak A, Blakely T, Cleghorn CL, Cobiac LJ. Potential of active transport to improve health, reduce healthcare costs, and reduce greenhouse gas emissions: A modelling study. PLoS One. 2019;14(7):e0219316.
Van der Deen FS, Wilson N, Cleghorn C, Kvizhinadze G, Cobiac L, Nghiem N, et al. Impact of five tobacco endgame strategies on future smoking prevalence, population health and health system costs: two modelling studies to inform the tobacco endgame. Tob Control. 2018;27(3):278–86.
Watt RG, Daly B, Allison P, Macpherson LMD, Venturelli R, Listl S, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394(10194):261–72.
Broomhead T, Baker SR. Systems science and oral health: implications for dental public health? Community Dent Health. 2019;36(1):55–62.
Broomhead T, Ballas D, Baker SR. Application of geographic information systems and simulation modelling to dental public health: where next? Community Dent Oral Epidemiol. 2019;47(1):1–11.
Gupta A, Keuskamp D. Use and misuse of mixed methods in population oral health research: A scoping review. Community Dent Health. 2018;35(2):109–18.
Further Reading
Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106.
Bartley M. Health inequality : an introduction to theories, concepts, and methods. Cambridge, UK: Polity Press; 2004.
Costa-Font J, Hernandez-Quevedo C. Measuring inequalities in health: what do we know? What do we need to know? Health Policy. 2012;106(2):195–206.
Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56(8):588–94.
Galobardes B, Shaw M, Lawlor DA, et al. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12.
Galobardes B, Shaw M, Lawlor DA, et al. Indicators of socioeconomic position (part 2). J Epidemiol Community Health. 2006;60(2):95–101.
Harper S, King NB, Meersman SC, et al. Implicit value judgments in the measurement of health inequalities. Milbank Q. 2010;88(1):4–29.
Kawachi I, Subramanian SV, Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health. 2002;56(9):647–52.
Krieger N. A glossary for social epidemiology. J Epidemiol Community Health. 2001;55:693–700.
Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44(6):757–71.
Sen A. Why health equity? Health Econ. 2002;11(8):659–66.
Singh A, Harford J, Schuch HS, et al. Theoretical basis and explanation for the relationship between area-level social inequalities and population oral health outcomes - A scoping review. SSM Popul Health. 2016;2:451–62.
Singh A, Harford J, Peres MA. Investigating societal determinants of oral health-opportunities and challenges in multilevel studies. Community Dent Oral Epidemiol. 2018;46(4):317–27.
Townsend P, Davidson N, Black DS. Inequalities in health : the Black report. Harmondsworth: Penguin; 1982.
Watt RG, Heilmann A, Listl S, et al. London charter on Oral health inequalities. J Dent Res. 2016;95(3):245–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Singh, A., Antunes, J.L.F., Peres, M.A. (2021). Socio-Economic Inequalities in Oral Health. In: Peres, M.A., Antunes, J.L.F., Watt, R.G. (eds) Oral Epidemiology. Textbooks in Contemporary Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-030-50123-5_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-50123-5_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-50122-8
Online ISBN: 978-3-030-50123-5
eBook Packages: MedicineMedicine (R0)