Abstract
The field of Nuclear Cardiology utilizes the unique properties of radiopharmaceuticals to characterize the pathophysiology of cardiovascular diseases. The images can be used to calculate global and regional function, perfusion, innervation, and apoptosis, among other characteristics. The ability to perform these measurements is the aggregate result of thousands of investigations and publications by dedicated investigators. This chapter describes some of the key contributions made by a few of these investigators and the role of their contributions in the development of this vibrant field.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
The field of Nuclear Cardiology utilizes the unique properties of radiopharmaceuticals to characterize the pathophysiology of cardiovascular diseases. The images can be used to calculate global and regional function, perfusion, innervation, and apoptosis, among other characteristics. The ability to perform these measurements is the aggregate result of thousands of investigations and publications by dedicated investigators. This chapter describes some of the key contributions made by a few of these investigators and the role of their contributions in the development of this vibrant field.
Discovery of Natural Radioactivity: Antoine Henri Becquerel
Nuclear Cardiology began in 1896 with the discovery of natural radioactivity by Antoine Henri Becquerel (Fig. 1.1). Less than 1 year after the description of x-rays by Roentgen in November 1895, Becquerel hypothesized that substances demonstrating phosphorescence in the form of visible light would also emit invisible light in the form of x-rays. (According to Merriam-Webster, a substance is phosphorescent if it absorbs radiation at one wavelength followed by reradiation at a different wavelength.) One of the phosphorescent materials tested was potassium uranyl sulfate (238U emits energetic alpha particles, and < 1% gammas.)
Henri Becquerel [2]
Becquerel tested his hypothesis by exciting these materials with sunlight. After “exciting” the specimen, he put the specimen in front of a photographic plate wrapped in black paper (to prevent exposure from ambient light). He also wrapped pieces of metal to absorb some of the invisible rays, to create a pattern on the photographic plate. When he developed the plate he saw the pattern of the attenuator on the photographic plate. Becquerel was surprised to see that the photographic plate was exposed even on a cloudy day, suggesting that factors other than exposure to sunlight caused the exposure. In 1896, Becquerel reported that these invisible rays are similar to the rays studied by Röntgen, but were due to something in the uranium itself. These rays were the result of ‘radioactivity’, a name given by Marie Curie [1].
The importance of the observation of “natural” radioactivity by Becquerel and his colleagues, Pierre and Marie Curie, was recognized by awarding these investigators the Nobel Prize in 1903 [2].
Understanding the Nature of Radiation
In 1899, Ernest Rutherford, working in the laboratory of his mentor J.J Thompson (discoverer of the electron), discovered that there were at least two different forms of radiation: a positively charged particle, which Rutherford called alpha , and the other one, more penetrating and negatively charged, which he called beta . In 1900, Paul Villard, a French physicist, discovered rays that were much more penetrating than alpha or beta particles and were not affected by electrical or magnetic fields. Rutherford named these gamma rays.
Other curious minds enhanced our understanding of the atom and radioactivity. Many of these contributions were recognized with the Nobel prize. Table 1.1 is an incomplete list of Nobel Laureates who contributed to our understanding of the heart and the physics and chemistry of radioactivity.
First Tracer Study in Humans: Herrmann Blumgart
Thirty years after Becquerel described radioactivity, Herrmann Ludwig Blumgart (Fig. 1.2), a 30-year-old physician, working with a medical student, Otto C. Yens, performed the first radiotracer examination in a human subject, to measure the velocity of blood flow [3]. The seminal manuscript described the criteria for a clinically useful radiotracer and the importance of matching the instrument to the clinical measurement.
Blumgart developed his interest in physiology as a medical student, working under the famed physiologist Walter Cannon [4]. As indicated in the 1927 publication in the Journal of Clinical Investigation [3], other investigators had measured the circulation time with other methods, such as injection of methylene blue and observing changes in transillumination of blood in the carotid artery, injection of hypertonic saline while observing changes in conductivity of blood between nonpolarizable electrodes in another vein, or injecting fluorescein in one antecubital vein and taking blood samples every 5 seconds from the contralateral cubital vein. The authors point out the weaknesses in each of these techniques, including difficulty cannulating a vessel, resulting in frequent clotting. There was also a requirement for continuous sampling, which was difficult to control. They noted that “the velocity measurements which depend on the insertion of a mechanical device into the blood stream defeats its ends…and cannot be considered for clinical application. The most feasible method appears to be the injection of some substance at one point in the body, and the measurement of the time of its arrival at another point.”
The authors specified the requirements for the tracer material:
-
The substance must not be toxic in the amounts utilized.
-
The substance should not be present previously in the body.
-
The substance must not in any way disturb the very phenomena under investigation.
-
It is desirable that the substance disappear from the body with sufficient rapidity to allow repeated measurements.
-
The substance must be readily detectable in minute amounts.
After considering many alternatives, they settled on the use of a saline solution containing dissolved radon gas. They tested it on themselves, with Blumgart as the first subject, and concluded that the radiotracer was safe.
Selection of an appropriate detector presented additional challenges. The initial choice was an electroscope, but there were problems with shielding, and difficulty judging the onset of response. An early version of the Geiger counter was also tested, but the “relatively high number of spontaneous discharges discouraged the choice of this mode of detection.” The Shimizu modification of the Wilson cloud chamber, a device capable of making measurements 1 to 5 times per second with a rapid response to the arrival of ionizing radiation, was selected. In normal subjects, the time required for the tracer to travel from a vein in one arm to an artery in the other was found to be “from 15 to 21 seconds.” In contrast, the velocities in three patients with cardiac decompensation were 53, 65, and 50 seconds.
The Radiocardiogram: Myron Prinzmetal
Two decades later, Myron Prinzmetal (Fig. 1.3) and colleagues (yes, the same Myron Prinzmetal of Prinzmetal’s variant angina [5]) used a collimated Geiger tube placed over the precordium and 24Na as the tracer in a 1948 publication [6] describing the curves recorded during the passage of the tracer through the heart and lungs. The biphasic curve was analyzed to determine cardiac output, right and left ventricular chamber volume, stroke volume, and pulmonary blood volume [7].
Radionuclide Imaging
In addition to analyzing curves, instruments were being developed to allow images of the distribution of radiotracers. The rectilinear scanner, developed to image the thyroid by Ben Cassen in 1951, was used to image the cardiac blood pool in 1958. The rectilinear scanner consisted of a collimated radiation detector connected to an apparatus that placed dots on a piece of paper each time a certain number of events were detected. The radiation detector moved along a line; when it reached the end of the line it stepped down to the next line, and moved back to reach the end of the line again and repeat the process. The result was a map of the distribution of radioactivity in the field of view
Rejali [8] used 131I-human serum albumin as the blood pool tracer to detect pericardial effusion. He compared the blood pool image to the size of the cardiac silhouette on a chest radiograph (Fig. 1.4). A blood pool that was smaller than the cardiac silhouette (or had a “halo” around it) was evidence of a pericardial effusion [9].
Scan demonstrating marked discrepancy in transverse diameters between the cardiac blood pool and cardiac silhouette seen on the roentgenogram [9]
Scintillation Camera: Hal Anger
In parallel with the development of blood pool imaging, a “Quiet Genius,” Hal Anger (Fig. 1.5), was developing a series of nuclear medicine instruments, including the gamma well counter and several imaging devices [10]. Anger recognized the need to record the distribution of all the tracer in a field of view simultaneously, like a photographic camera, rather than point by point, as recorded with a rectilinear scanner. From 1952 to 1960, Anger evolved his “camera.” He enlarged the field of view from about 4 inches to 11 inches, and increased the sensitivity by changing from multiple pinhole collimators to parallel-hole collimation. To determine the location of each scintillation in the sodium iodide crystal, Anger used a hexagonal array of 19 photomultiplier tubes (PMTs). The scintillation was localized by comparing the relative amount of light “seen” by each PMT. Each scintillation was displayed as a flash of light on a cathode ray tube in the same relative position as they occurred in the crystal. A record of the distribution of the flashes was recorded on Polaroid film. By 1962, Anger had improved the scintillation camera to a clinically usable and commercially viable instrument. A visionary businessman, John Kuranz, the founder of the Nuclear Chicago Company, produced the first commercial instrument, an early version of which is on display in the Smithsonian Institute [11]. Anger not only developed a single photon gamma camera, but also a positron version [12]. The positron version used a small second detector placed beneath the patient to identify coincidence events.
Hal O. Anger. (From Tapscott [10], with permission from The Society of Nuclear Medicine and Molecular Imaging)
In 1962, Alex Gottschalk, a young clinical radiologist from Paul Harper’s laboratory in Chicago, arrived at the Donner Laboratory to work with Anger on clinical applications of the new imaging device. Gottschalk recognized the substantial advantages of the gamma camera over the rectilinear scanner, particularly the clinical value of simultaneous imaging of tracers in large regions of the body, including the brain and heart [13].
Initially, the positron-emitter gallium-68 (as 68Ga-EDTA) was imaged with Anger’s positron camera to detect brain tumors (based on loss of integrity of the blood-brain barrier) [14]. Although the instrument worked, the dose of 68Ga was limited to 750 microcuries to avoid paralysis of the coincidence detector. Even with that limitation, the imaging results were impressive (Fig. 1.6).
A 68Ga-EDTA brain scan acquired with the Anger positron camera circa 1962, showing the tomographic capability. (From Gottschalk [14], with permission from The Society of Nuclear Medicine and Molecular Imaging)
In 1964, Anger and Gottschalk started working with 99mTc generators. The combination of a thin scintillation crystal in the camera, the 140 keV gamma emissions from metastable Tc-99 m, and the 6-hour physical half-life made this radionuclide the preferred agent for labeling radiopharmaceuticals for clinical use. Gottschalk and Anger recorded cerebral angiograms and first-pass cardiac studies.
Cardiac Studies
Left Ventricular Ejection Fraction
In 1975, Schelbert and colleagues used the gamma camera to record a first-pass radionuclide angiogram. Instead of recording the data on Polaroid film, the investigators used a video camera. In addition to the images, Schelbert recorded the patient’s electrocardiogram on the sound track of the videotape. The EKG served as an indicator of the phase of the cardiac cycle, allowing the images recorded at end-diastole (the P-R interval) and end-systole (the downslope of the T wave) to be summed, to compute the end diastolic, end systolic, and stroke volume counts to calculate the ejection fraction (correlated with cineangiocardiography − r = 0.94) [15] (Fig. 1.7). Although this technique worked well in patients with well-maintained cardiac function, the method did not work well in patients with impaired ventricular function.
Selected images from videotape replay of a first pass radionuclide angiogram. (a) Summed image of right and left heart phases; (b) Region of interest (ROI) placed over the RV and LV; (c) Graph of time (x axis) and counts (y axis) as tracer traverses the right and left ventricles; (d) Summed image of the left ventricular phase of the first pass; (e) ROI over LV and background (bkg) during LV phase; (f) Time activity curve of background corrected activity
Measuring ventricular function in patients with impaired function required high count density images, which were difficult to record with a first-pass technique. In 1971, Strauss and Zaret introduced the concept of equilibrium blood pool imaging. 99mTc-labeled albumin had been developed to replace radioiodinated albumin for the detection of pericardial effusions. Equilibrium blood pool imaging, with EKG gating to record data only at end-systole or end-diastole, or throughout the cardiac cycle (when sufficient computer memory was available), allowed high-resolution images of both global and regional ventricular function [16, 17] (Fig. 1.8). The outline of the left ventricle at end-diastole or end-systole was traced, and the outline measured with a planimeter. The relative size of the left ventricle was determined at diastole and systole. The difference represented the stroke volume. Ejection fraction was calculated as the stroke volume area divided by the end diastolic area. Regional wall motion was determined by comparing the outlines traced at end systole and end diastole. Areas of akinesis and dyskinesis were readily identified. Subsequently, Secker-Walker et al. [18] developed a count-based approach to calculate left ventricular ejection fraction.
Gated blood pool imaging. (From Strauss et al. [16], with permission from Elsevier)
Myocardial Perfusion
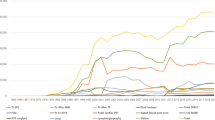
Several approaches were tested to measure myocardial perfusion. The first used the inert gas clearance method, with intracoronary administration of 133xenon recorded with a single detector. This approach did not work well, because the clearance is dominated by normal tissue, making it very difficult to identify regions of decreased perfusion. To measure regional perfusion in all regions of the myocardium required multiple detectors. The multicrystal camera, designed by Bender and Blau [19], allowed the simultaneous independent measurement of tracer clearance from multiple myocardial locations, allowing identification of regions of normal and reduced perfusion. Figure 1.9 shows the relationship of coronary stenoses to the slightly reduced regional perfusion at rest [20]. The requirement for intracoronary injection of the tracer limited this technique to research studies.
In the early 1960s, Edward Carr, a nuclear physician working at the University of Michigan with William (Bill) Beierwaltes (the co-inventor of MIBG), was interested in myocardial imaging to detect acute myocardial infarction. Carr explored two techniques: One used myocardial perfusion imaging to detect areas of infarction as a “cold” spot (using the perfusion tracer 86Rb) [21]; the other detected the area of infarction as a hot spot, using the agent employed to detect brain tumors, 203Hg-chlormeridrin [22]. The selection of an isotope of rubidium as the cold spot tracer was based on the observations of the famous cardiologist from Tulane University, George Burch. Burch studied the kinetics of several potassium analogues in human subjects, including isotopes of rubidium [23]. Burch observed rapid clearance of 86Rb from the blood and rapid uptake in multiple tissues (including the myocardium), suggesting that the tracer distribution would reflect myocardial perfusion. Carr selected the beta- and gamma-emitting tracer 86Rb (gamma 1.076 MeV), with an 18.6-day half-life, to image experimental infarcts in dogs as “cold spots” in the myocardium. Areas of infarction appeared as regions of decreased tracer uptake on the scans. These pioneering studies by Carr led Ken Poggenburg, a radiochemist at the Oak Ridge National Laboratory, to synthesize potassium-43 in the Oak Ridge reactor using the 43Ca(n,p)43K reaction. The half-life of 22 hours and major gamma energy of 373 keV was better suited than the rubidium isotopes for imaging with the rectilinear scanner. First-in-man studies with 43K by Hurley et al. in control subjects and patients with acute infarction demonstrated a “cold” area in the myocardial images of each of the five patients with acute infarction [24].
Zaret [25] and Strauss [26] extended the utility of myocardial perfusion imaging to detect ischemia by recording two myocardial perfusion scans: one with the tracer injected with the patient at rest (to distinguish regions of normal perfusion from areas of scar) and a second tracer injection during exercise stress followed by immediate scanning (to distinguish regions capable of increasing perfusion at stress from areas with decreased perfusion reserve (typically supplied by vessels with significant stenoses) (Fig. 1.10).
The development of thallium-201 as a myocardial perfusion agent, with its low-energy photons, facilitated the utilization of the gamma camera to record the rest and stress images [27]. Studies by Pohost and colleagues [28] revealed the dynamic nature of myocardial tracer retention. Patients were injected during exercise stress, and images recorded after exercise demonstrated myocardial regions of decreased tracer uptake. When the images were repeated several hours later, the areas of decreased tracer uptake on initial images, appeared to fill in (redistribute). This phenomenon occurred because of more rapid tracer clearance from regions of normally perfused myocardium than in regions of ischemia [29]. Based on these observations, stress and redistribution imaging, rather than stress and rest-injected images, became the preferred approach to detect ischemia.
In 1984, the synthesis of 99mTc-sestamibi as a myocardial perfusion tracer allowed administration of much larger doses [30] (20–30 mCi) compared to the typical 4 mCi dose of thallium-201). The high-count-density images recorded with 99mTc sestamibi enhanced image quality, allowing the measurement of both regional perfusion and ventricular function by gating the acquisition of myocardial perfusion data. Instrumentation improved with the development of the rotating gamma camera [31] to record myocardial perfusion single photon emission computed tomography (SPECT) images. Standardization of image presentation and improvements in the quantitation of perfusion and ventricular function at rest and stress [32,33,34] enhanced the acceptance of myocardial perfusion imaging by the medical community.
Dr. K. Lance Gould (Fig. 1.11) and colleagues performed a series of laboratory studies that defined the quantitative relationship between the percentage of stenosis on coronary arteriography and myocardial perfusion at rest and at maximum vasodilator stress [35]. The studies demonstrate that a stenosis of about 75% of the luminal diameter is required to decrease resting coronary blood flow. Using hyperemia as a stimulus (induced by intracoronary injection of contrast material or intravenous administration of dipyridamole), coronary narrowing’s of only 47% of luminal diameter could be detected. These studies led to the validation of pharmacologic vasodilators (eg, dipyridamole), as an alternative to exercise to induce maximal coronary blood flow in patients who cannot perform maximal exercise [36]. The pathophysiologic rationale for the use of these agents is probably inadequate vasodilatation in coronary vessels with inflamed atheroma. Vessels without inflammatory lesions in the subintima dilate in response to the drug, delivering additional blood flow (and tracer) to the distal myocardium.
In parallel with advances in single photon imaging, numerous investigators were working on advanced instrumentation to image the annihilation radiation resulting from the mass-to-energy conversion of positron-emitting tracers. Pioneers included investigators at the Massachusetts General Hospital [37], at the Mallinckrodt Institute of Radiology at Washington University in St. Louis [38] and at the Crump Institute at the University of California Los Angeles [37, 38] among many others. The results of their investigations resulted in the ring detector, allowing high-count-density images and quantitation of absolute myocardial blood flow and perfusion reserve [39], as well as increased certainty of diagnosis through the high-resolution images. In addition to higher-quality images of myocardial perfusion and ventricular function, direct detection of myocardial viability in patients with myocardial infarction was reported by the UCLA group in 1983 [40]. Ischemia was depicted as an area of decreased perfusion which maintained metabolic activity. Perfusion was usually imaged with 13N-ammonia and myocardial glucose metabolism was imaged with 18F-FDG. Patients demonstrating this disparity had an improved prognosis when treated with revascularization [41].
The remarkable development of hybrid PET/CT instrumentation in the laboratory of David Townsend [42] (Fig. 1.12) resulted in high-quality CT based attenuation correction and enhanced registration of anatomic and radionuclide data. These advances allow more precise characterization of the degree of inflammation in the coronary arterial wall with FDG [43], and more precise determination of the degree of ongoing necrosis in atheroma with fluoride imaging [44, 45].
Investigators and practitioners of Nuclear Cardiology have much to be proud of, and much to look forward to. For example, the development of genetic markers will identify imageable markers to characterize specific abnormalities of contractile proteins in patients with heart failure and inflammatory lesions in atheroma.
The field has a scintillating future.
Myocardial perfusion pattern in a patient with coronary stenoses [20]
Studies of myocardial perfusion. (From Zaret et al. [25], with permission of the Massachusetts Medical Society)
References
Berkeley Lab. The discovery of radioactivity. https://www2.lbl.gov/abc/wallchart/chapters/03/4.html.
The Nobel Prize in Physics. 1903. http://www.nobelprize.org/nobel_prizes/physics/laureates/1903.
Blumgart HL, Yens OC. Studies on the velocity of blood flow: I. The method utilized. J Clin Invest. 1927;4:1–13.
Patton DD. The birth of nuclear medicine instrumentation: Blumgart and Yens, 1925. J Nucl Med. 2003;44:1362–5.
Roguin A. Myron Prinzmetal 1908-1987: the man behind the variant angina. Int J Cardiol. 2008;123:129–30.
Prinzmetal M, Corday E, Bergman HC, Schwartz L, Spritzler RJ. Radiocardiography: a new method for studying blood flow through the chambers of the heart in human beings. Science. 1948;108:340–1.
Donato L, Holmes RA, Wagner HN. The circulation. In: Wagner HN, editor. Principles of nuclear medicine. Philadelphia: WB Saunders; 1968. p. 531–83.
Rejali AM, MacIntyre WJ, Friedell HL. A radioisotope method of visualization of blood pools. Am J Roentgenol Radium Therapy Nucl Med. 1958;79:129–37.
Rosenthall L. Detection of pericardial effusion by radioisotope heart scanning. Can Med Assoc J. 1964;90:447–51.
Tapscott E. Nuclear medicine pioneer, Hal O. Anger, 1920-2005. J Nucl Med Technol. 2005;33:250–3.
Anger HO. Scintillation camera with multichannel collimators. J Nucl Med. 1964;5:515–31.
Gottschalk A, McCormack KR, Adams JE, Anger HO. A comparison of results of brain scanning using 68Ga EDTA and the positron scintillation camera, with 203Hg neohydrin and the conventional focused collimator scanner. Radiology. 1965;84:502–6.
Gottschalk A. The early years with Hal Anger. Semin Nucl Med. 1996;26:171–9.
Gottschalk A. Hal Anger, nuclear medicine's quiet genius. J Nucl Med. 2004;45:13N–26N.
Schelbert HR, Verba JW, Johnson AD, Brock GW, Alazraki NP, Rose FJ, Ashburn WL. Nontraumatic determination of left ventricular ejection fraction by radionuclide angiocardiography. Circulation. 1975;51:902–9.
Strauss HW, Zaret BL, Hurley PJ, Natarajan TK, Pitt B. A scintiphotographic method for measuring left ventricular ejection fraction in man without cardiac catheterization. Am J Cardiol. 1971;28:575–80.
Zaret BL, Strauss HW, Hurley PJ, Natarajan TK, Pitt B. A noninvasive scintiphotographic method for detecting regional ventricular dysfunction in man. N Engl J Med. 1971;284:1165–70.
Secker-Walker RH, Resnick L, Kunz H, Parker JA, Hill RL, Potchen EJ. Measurement of left ventricular ejection fraction. J Nucl Med. 1973;14:798–802.
Harris CC. Hevesy nuclear medicine pioneer lecture (Monte Blau, Merrill A. Bender). J Nucl Med. 1980;21:609–11.
Cannon PJ, Schmidt DH, Weiss MB, Fowler DL, Sciacca RR, Ellis K, Casarella WJ. The relationship between regional myocardial perfusion at rest and arteriographic lesions in patients with coronary atherosclerosis. J Clin Invest. 1975;56:1442–54.
Carr EA Jr, Beierwaltes WH, Wegst AV, Bartlett JD Jr. Myocardial scanning with rubidium-86. J Nucl Med. 1962;3:76–82.
Carr EA Jr, Beierwaltes WH, Patno ME, Bartlett JD Jr, Wegst AV. The detection of experimental myocardial infarcts by photoscanning. A preliminary report. Am Heart J. 1962;64:650–60.
Burch G, Threefoot S, Ray C. The rate of disappearance of Rb86 from the plasma, the biologic decay rates of Rb86, and the applicability of Rb86 as a tracer of potassium in man with and without chronic congestive heart failure. J Lab Clin Med. 1955;45:371–94.
Hurley PJ, Cooper M, Reba RC, Poggenburg KJ, Wagner HN Jr. 43KCl: a new radiopharmaceutical for imaging the heart. J Nucl Med. 1971;12:516–9.
Zaret BL, Strauss HW, Martin ND, Wells HP Jr, Flamm MD. Noninvasive regional myocardial perfusion with radioactive potassium. Study of patients at rest, with exercise and during angina pectoris. N Engl J Med. 1973;288:809–12.
Strauss HW, Zaret BL, Martin ND, Wells HP Jr, Flamm MD. Noninvasive evaluation of regional myocardial perfusion with potassium 43. Technique in patients with exercise-induced transient myocardial ischemia. Radiology. 1973;108:85–90.
Lebowitz E, Greene MW, Fairchild R, Bradley-Moore PR, Atkins HL, Ansari AN, et al. Thallium-201 for medical use. I J Nucl Med. 1975;16:151–5.
Pohost GM, Zir LM, Moore RH, McKusick KA, Guiney TE, Beller GA. Differentiation of transiently ischemic from infarcted myocardium by serial imaging after a single dose of thallium-201. Circulation. 1977;55:294–302.
Pohost GM, Okada RD, O'Keefe DD, Gewirtz H, Beller G, Strauss HW, et al. Thallium redistribution in dogs with severe coronary artery stenosis of fixed caliber. Circ Res. 1981;48:439–46.
Holman BL, Jones AG, Lister-James J, Davison A, Abrams MJ, Kirshenbaum JM, et al. A new Tc-99m-labeled myocardial imaging agent, hexakis(t-butylisonitrile)-technetium(I) [Tc-99m TBI]: initial experience in the human. J Nucl Med. 1984;25:1350–5.
Keyes JW Jr, Orlandea N, Heetderks WJ, Leonard PF, Rogers WL. The humongotron–a scintillation-camera transaxial tomograph. J Nucl Med. 1977;18:381–7.
Prigent FM, Maddahi J, Garcia E, Friedman J, Van Train K, Bietendorf J, et al. Thallium-201 stress-redistribution myocardial rotational tomography: development of criteria for visual interpretation. Am Heart J. 1985;109:274–81.
Germano G, Kavanagh PB, Berman DS. An automatic approach to the analysis, quantitation and review of perfusion and function from myocardial perfusion SPECT images. Int J Card Imaging. 1997;13:337–46.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, et al. European Association of Nuclear Medicine (EANM). EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929–40.
Gould KL. Coronary artery stenosis. New York: Elsevier; 1991.
Albro PC, Gould KL, Westcott RI, Hamilton GW, Ritchie JL, Williams DL. Noninvasive assessment of coronary stenoses by myocardial imaging during pharmacologic coronary vasodilation III. Clinical trial. Am J Cardiol. 1978;42:751–60.
Hoop B Jr, Smith TW, Burnham CA, Correll JE, Brownell GL, Sanders CA. Myocardial imaging with 13 NH 4+ and a multicrystal positron camera. J Nucl Med. 1973;14:181–3.
Ter-Pogossian MM, Phelps ME, Hoffman EJ, Mullani NA. A positron-emission transaxial tomograph for nuclear imaging (PETT). Radiology. 1975;114:89–98.
Dorbala S, Di Carli MF. Cardiac PET perfusion: prognosis, risk stratification, and clinical management. Semin Nucl Med. 2014;44:344–57.
Marshall RC, Tillisch JH, Phelps ME, Huang SC, Carson R, Henze E, Schelbert HR. Identification and differentiation of resting myocardial ischemia and infarction in man with positron computed tomography, 18F-labeled fluorodeoxyglucose and N-13 ammonia. Circulation. 1983;67:766–78.
Bax JJ, Visser FC, Poldermans D, Elhendy A, Cornel JH, Boersma E, et al. Relationship between preoperative viability and postoperative improvement in LVEF and heart failure symptoms. J Nucl Med. 2001;42:79–86.
Townsend DW, Cherry SR. Combining anatomy and function: the path to true image fusion. Eur Radiol. 2001;11:1968–74.
Vallabhajosula S, Fuster V. Atherosclerosis: imaging techniques and the evolving role of nuclear medicine. J Nucl Med. 1997;38:1788–96.
Derlin T, Richter U, Bannas P, Begemann P, Buchert R, Mester J, Klutmann S. Feasibility of 18F-sodium fluoride PET/CT for imaging of atherosclerotic plaque. J Nucl Med. 2010;51:862–5.
Nakahara T, Dweck MR, Narula N, Pisapia D, Narula J, Strauss HW. Coronary artery calcification: from mechanism to molecular imaging. JACC Cardiovasc Imaging. 2017;10:582–93.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Strauss, H.W. (2021). History of Nuclear Cardiology. In: Dilsizian, V., Narula, J. (eds) Atlas of Nuclear Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-030-49885-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-49885-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-49884-9
Online ISBN: 978-3-030-49885-6
eBook Packages: MedicineMedicine (R0)