Abstract
The human brain is dependent upon the delivery of oxygen and glucose and the removal of waste products for normal activity with the interruption of this cycle resulting in tissue injury. A reduction of oxygen content within the brain parenchyma is the state of anoxia, while the cessation of blood flow is ischemia. There are many different etiologies of anoxia including a reduction in blood flow—stagnant anoxia; lack of oxygenation—hypoxic anoxia; insufficient oxygen transport—anemic anoxia; and a disturbance in the intracellular oxygen transport—histotoxic anoxia. In adults the most common cause is a combined hypoxic and ischemic injury caused by cardiac arrest. For a neurological disease state with such high prevalence, surprisingly little is understood about the precise patterns of impairment or about the natural history of recovery. There are robust early predictors of outcome of anoxic-ischemic coma (Nolan et al., Intensive Care Med 41: 2039–2056, 2015; Wijdicks, Neurology 67: 203–210, 2006), but the outcome has rarely been specified beyond good, poor, and death. This chapter is designed to examine the etiology, pathology, neurological sequelae, treatment, and outcome of patients who survive a cardiac arrest.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cardiac arrest
- Anoxia
- Global cerebral ischemia
- Cerebral performance category (CPC)
- Therapeutic hypothermia
9.1 Introduction
The human brain is dependent upon the delivery of oxygen and glucose and the removal of waste products for normal activity with the interruption of this cycle resulting in tissue injury. A reduction of oxygen content within the brain parenchyma is the state of anoxia, while the cessation of blood flow is ischemia. There are many different etiologies of anoxia including a reduction in blood flow—stagnant anoxia; lack of oxygenation—hypoxic anoxia; insufficient oxygen transport—anemic anoxia; and a disturbance in the intracellular oxygen transport—histotoxic anoxia. In adults the most common cause is a combined hypoxic and ischemic injury caused by cardiac arrest.
For a neurological disease state with such high prevalence, surprisingly little is understood about the precise patterns of impairment or about the natural history of recovery. There are robust early predictors of outcome of anoxic-ischemic coma (Nolan et al., 2015; Wijdicks, 2006), but the outcome has rarely been specified beyond good, poor, and death.
This chapter is designed to examine the etiology, pathology, neurological sequelae, treatment, and outcome of patients who survive a cardiac arrest.
9.2 Epidemiology and Clinical Burden
Cardiac disease has been the leading cause of death in the United States since 1921, currently accounting for 30% of all deaths (Minino & Smith, 2001). In 1998 in the United States, 456,076 deaths, or 63% of all cardiac disease deaths were caused by cardiac arrest (Zheng, Croft, Giles, & Mensah, 2001)—a 7% increase over the previous 10 years. The average age of the cardiac arrest patients is approximately 65 years (Eisenburger et al., 1998; Kuilman, Bleeker, Hartman, & Simoons, 1999). Estimates of short-term survival from large population surveys of patients who have undergone resuscitation for cardiac arrest vary from 1.4% (Becker, Ostrander, Barrett, & Kondos, 1991; Lombardi, Gallagher, & Gennis, 1994) up to 20%(Fischer, Fischer, & Schüttler, 1997; Kuisma & Maata, 1996; Sedgwick, Dalzeil, Watson, Carrington, & Cobbe, 1993; Waalewijn, de Vos, & Koster, 1988). The best survival rate in the United States of about 15–20% comes from a suburban community in Washington State (Cummins, Ornato, Thies, & Pepe, 1991; Rea, Eisenberg, Becker, Murray, & Hearne, 2003), while the worst is the urban communities (Gaieski et al., 2017; Lombardi et al., 1994). With a mean survival rate of 8% (Chan, McNally, Tang, Kellermann, & CARES Surveillance Group, 2014), there would be 36,500 survivors of cardiac arrest every year in the United States alone. The long-term survival of these patients has been reported as 70–85% at 1 year (Chan et al., 2016; Fischer et al., 1997; Graves et al., 1997; Kuilman et al., 1999; Sedgwick et al., 1993), 66% between 2 and 5 years (Ladwig et al., 1997), 52% at 3.5 years (Earnest, Yarnell, Merrill, & Knapp, 1980), 44–77% at 5 years (Graves et al., 1997; Kuilman et al., 1999), 73% at 7 years (1999), and 18% at 10 years (Graves et al., 1997). Improvement in medical care has resulted in a steady increase in survival (Rea, 2003; Smith, Andrew, Lijovic, Nehme, & Bernard, 2015; Wong et al., 2014) and neurological outcomes (Chan et al., 2014) over time.
Chart reviews (Graves et al., 1997), telephone interviews (Ladwig et al., 1997), and neuropsychological testing (Roine, Kajaste, & Kaste, 1993) on patients who have survived a cardiac arrest have shown that one-quarter to two-thirds of all survivors have neurological deficits, and one-half of all survivors have cognitive or motor deficits of a magnitude that requires a major lifestyle change (Bergner, Hallstrom, Bergner, Eisenberg, & Cobb, 1985; Earnest et al., 1980; Graves et al., 1997).
Based on the reported rates for survival and impairment, we would estimate a yearly incidence of approximately 5/100,000 (12,000) survivors of cardiac arrest who will have persistent neurological deficits and a rolling prevalence of 50,000 impaired survivors in the United States. This is roughly equivalent to the number of patients diagnosed with multiple sclerosis in the United States every year (National Multiple Sclerosis Society, 2005). These numbers are increasing with the improvement of the “chain of survival” concept (Cummings et al., 1991), implementation of disease modifying therapy (The Hypothermia after Cardiac Arrest Study Group, 2002), and further refinement of the implantable defibrillator (Hlatky, Saynina, McDonald, Garber, & McClellan, 2002). This improvement also reflects an improvement in neurological outcomes (Chan et al., 2014). For example, a nationwide study in Japan (Kitamura et al., 2012) demonstrated a near doubling (from 1.6% to 2.8%) of favorable neurological outcomes in 2009 compared to 2005.
9.3 Neuropathology
During a cardiac arrest, brain tissue can survive for about 4–5 min without oxygen and blood before irreversible damage occurs (Bass, 1985). The severity of brain damage is dependent upon the duration of ischemia, the degree of ischemia, the core temperature, and the blood glucose level (Auer & Benveniste, 1994). Even though cardiac arrest causes global ischemia and hypoxia, neuronal injury is maximal in specific focal regions, a concept known as selective vulnerability. For reasons still not entirely understood, the small- and medium-sized neurons of the striatum, the Purkinje cells of the cerebellum, the layer III neurons of the cerebral cortex, and thalamic neurons are the first areas to show degenerative changes (Auer & Benveniste, 1994; Kuroiwa & Okeda, 1994). The pyramidal neurons of the hippocampal formation may not show the earliest damage but undergo delayed neuronal death (Horn & Schlote, 1992; Petito, Feldmann, Pulsinelli, & Plum, 1987). The etiology of this delayed neuronal death is unknown, but factors thought to play a role include the intracellular formation of oxygen free-radicals and excessive neuronal excitability because the hippocampal pyramidal neurons are at the end of a major excitatory pathway (Auer & Benveniste, 1994; Murayama, Bouldin, & Suzuki, 1990).
There have been several studies on the temporal sequences of cell death after anoxia. Horn and Schlote (Horn & Schlote, 1992) examined the brains of 26 cardiac arrest patients and found the earliest damage occurring in cortical layers three, five, and six, appearing within the first few days. Purkinje cell necrosis was observed up to day 6. Rapid hippocampal pyramidal neuronal cell death was seen from days 4 to 7. Petito et al. (1987) found a similar pattern in their review of 14 cases and concluded that the cortex and basal ganglia suffered early damage (occurring within the first 18 h) while the hippocampus suffered delayed necrosis at greater than 24 h.
The pathology literature is dominated by patients who suffered a severe anoxic injury and early death. Little is known about possible regionally specific brain pathology in patients suffering less severe anoxia. Although selective vulnerability is the accepted theory to account for the patterns and distribution of neuronal damage and patterns of clinical impairment, the precise relationship between pathology and clinical signs is incompletely understood.
Hypoxic–ischemic damage to specific regions of the brain is, nevertheless, certainly responsible for the diverse, specific neurological deficits. Immediate (hours to days) complications of cardiac arrest include death, coma (Levy et al., 1985; Yarnell, 1976), severe encephalopathy (Sawada et al., 1990), seizures (Madison & Niedermeyer, 1970), myoclonus (Lance & Adams, 1963), and cortical blindness (Sabah, 1969). Long-term complications include persistent vegetative state (Sazbon, Zabreba, Ronen, Solzi, & Costeff, 1993; Yarnell, 1976), diffuse injury (Parkin, Miller, & Vincent, 1987), amnestic syndrome (Volpe & Hirst, 1983), frontoexecutive dysfunction (Armengol, 2000; Reich, Regestein, Murawski, DeSilva, & Lown, 1983), visuospatial dysfunction (Howard, Trend, & Ross Russell, 1987; Kase, Troncoso, Court, Tapia, & Mohr, 1977), pyramidal tract weakness (Allison, Bedford, & Meyer, 1956), extra-pyramidal disorders (Hawker & Lang, 1990), ataxia (Lance & Adams, 1963), spinal cord infarct (Silver & Buxton, 1974), and other very rare disorders. The frequency of each of these complications and whether they co-occur in any particular pattern are not known. Whether the course of recovery or specific outcome conditions (other than death) is tightly related to the severity of the hypoxic–ischemic event is unknown. It is also unknown if any pattern of early deficits is systematically linked to long-term sequelae.
For the clinician, there are several levels of importance: (1) predicting acute survival as a basis for judgment about intensive support, (2) managing and predicting short- and long-term recovery among survivors, (3) recognizing the range of residual deficits and the implications for specific vulnerability, and (4) working knowledge of the utility of proposed treatments.
9.4 Acute Prediction of Survival and Quality of Recovery
The bulk of outcome prediction research was collected before the advent of targeted temperature management (TTM). While targeted temperature management improved survival (Bernard et al., 2002; The Hypothermia after Cardiac Arrest Study Group, 2002), it was initially unclear how it affected outcome prediction (Nielsen et al., 2013). Pooled data suggests that TTM incurs a survival and neuroprotective benefit (Schenone et al., 2016). It has also become clear that it impacts the prognostic utility of clinical examination and laboratory testing. TTM may alter or delay the course of neurological recovery, and hence, the timing of assessing prognosis remains unknown. Validated protocols for assessing outcomes following TTM are rare, biased by withdrawal of care (Gold et al., 2014; Mulder et al., 2014), and in the absence of a standard consensus protocol, continue to rely on pre-temperature management data.
9.4.1 Examination
There is no measure of injury that has proven uniformly informative about severity. Duration of anoxia, time to CPR and defibrillation, or cause of cardiac arrest accurately does not predict the outcome (Wijdicks, 2006), although one study showed that >99% of patients with favorable outcomes, defined as cerebral performance categoryFootnote 1 (CPC) of 1–2, had CPR of less than 35 min (Goto, Funada, & Goto, 2016).
Only about 25% of out-of-hospital cardiac arrest patients survive to hospital admission (McNally et al., 2011), with approximately 25% awake (Longstreth, Inui, Cobb, & Copass, 1983). Relying on the level of consciousness to predict outcome, Longstreth et al. (1983) found that of those patients who awakened after 24 h, 73% had cognitive or motor deficits. After 4 days of coma, no patient ever fully recovered. This predictive method may not apply to those who have not received targeted temperature therapy because several recent studies have found that over 80% of patients who received targeted temperature therapy who awakened after 72 h were discharged with a CPC 1–2 (Gold et al., 2014; Grossestreuer et al., 2013). While this may not be a true discrepancy since CPC of 1 includes patients with minor neurological deficits, there are reports of patients in coma for greater than 7 days, who received TTM, with good outcomes (Greer, 2013; Grossestreuer et al., 2013). Other studies confirmed that the early awakeners generally have good outcomes with only between 13% and 23% having any motor or cognitive deficits compared to 52% and 73% of the patients awakening after 12 h having deficits (Earnest, Breckinridge, Yarnell, & Oliva, 1979; Snyder et al., 1980). Sazbon et al. (1993) and others (Estraneo et al., 2013) followed patients with a history of 30 days or more of unconsciousness for at least 5 years and found that not a single patient recovered to a state of moderate disability or better.
The most straightforward and predictively useful applied evaluation is the clinical examination. The critical aspects of the acute, clinical examination are description of the depth of coma and the status of the critical vegetative brainstem functions. Assessment of coma may be complicated by intensive care management. The reliance on using the neurological examination to predict neurological outcome was initially based on the work by Levy et al. (1985). They and others (Edgren, Hedstrand, Kelsey, Sutton-Tyrrell, & Safar, 1994; Zandbergen et al., 2006) have shown that the absent pupillary light reflex after 24 h has a 100% positive predictive value (PPV) for a poor outcome. The sensitivity of this test is only around 20%. Subsequent to TTM, there have been reports of patients who did not have one or more brainstem reflexes at day 3 (Bouwes et al., 2012; Dragancea et al., 2015; Rossetti, Oddo, Logroscino, & Kaplan, 2010) with good outcomes (CPC 1–2). An automated pupillometry approach may ultimately have the best predictive value in assessing outcomes (Solari et al., 2017).
Absent motor response to painful stimuli at 72 h is a more sensitive test (around 60%) with two pre-TTM class I studies (Edgren et al., 1994; Levy et al., 1985) having a PPV of 100%, but (Zandbergen et al., 2006) five out of 105 patients with absent motor responses at 72 h were awake after 1 month in the most recent class I study. The motor response appears to have been most affected by TTM (Al Thenayan, Savard, Sharpe, Norton, & Young, 2008; Dragancea et al., 2015; Rossetti et al., 2010) and is no longer felt to be a useful predictor of poor outcome.
9.4.2 Laboratory Studies
Prolonged cardiac arrest results in metabolic cell death with the release of intracellular contents, and recent studies have explored the utility of assays of brain enzymes as a potential marker of injury severity and outcome. Studies have focused on serum neuron-specific enolase (NSE) (Karkela, Bock, & Kaukinen, 1993; Schoerkhuber et al., 1999; Zandbergen et al., 2006), serum astroglial S100 (Pfeifer et al., 2005; Zandbergen et al., 2006), brain-type creatine kinase isoenzyme (Karkela et al., 1993; Karkela, Pasanen, Kaukinen, Morsky, & Harmoinen, 1992), and CSF lactaid (Edgren, Hedstrand, Nordin, Rydin, & Ronquist, 1987). These studies indicate that serum NSE levels >33 μg/L between days 1 and 3 following cardiac arrest most accurately predicts poor outcome with a PPV of 100% and sensitivity around 50%, but again, its predictive value has diminished post-TTM with debates on the cutoff value and timing (Bouwes et al., 2012; Oksanen et al., 2009; Rundgren et al., 2009; Tiainen, Roine, Pettilä, & Takkunen, 2003). One small study showed that abnormal serum astroglial S100 levels at day 3 was associated with low test performance in attention, memory, and executive function (Prohl, Bodenburg, & Rustenbach, 2009).
Recently, an offshoot of the Targeted Temperature Management study (Nielsen et al., 2013) used a novel assay to detect serum levels of axonal injury maker tau in 689 cardiac arrest patients (Mattsson et al., 2017). They found that at 72 h, serum tau levels above 72.7 ng/L had a PPV of 100% in predicting poor outcome (CPC 3–5) with a sensitivity of 42%. Reducing the cutoff to 13.4 ng/L brought up the sensitivity to 65% with a false-positive rate of 1%. Tau did not appear affected by TTM, and low levels or decreasing levels from 24 h to 72 h may predict a good outcome (CPC 1–2), although sensitivity and specificity were not discussed.
Serum tau has the potential to be a more practical test because it may have utility in other disease such as traumatic brain injury (Liliang et al., 2010; Ost et al., 2006) and dementia (Shekhar et al., 2016). These tests currently offer little practical utility because many hospitals cannot provide rapid turnover of these test results.
.
9.4.3 Electrophysiology
Electroencephalography (EEG) and somatosensory evoked potentials (SSEP) supplement the clinical examination and laboratory tests as predictive measures of poor outcome. Generalized suppression, burst suppression, or generalized periodic complexes on a flat background EEG patterns within the week of admission almost invariably resulted in death or vegetative state (Edgren et al., 1987; Rothstein, Thomas, & Sumi, 1991; Scollo-Lavizzari & Bassetti, 1987), although in a single study, two patients with malignant EEG had a good recovery (Chen, Bolton, & Young, 1996). TTM has likely altered the predictive value (or timing) of EEG because the most recent large group analysis demonstrated a false-positive rate of 1.5% (Rossetti et al., 2017) in patients with highly malignant EEGs.
Specific seizure types can also portend a grim prognosis. Initially, several controlled studies have shown that the presence of myoclonic status epilepticus within the first 24 h has grim prognosis (PPV of 100%) (Wijdicks, Parisi, & Sharbrough, 1994; Zandbergen et al., 2006), although there has been a case report of a survivor of myoclonic status epilepticus (Arnoldus & Lammers, 1995). A lack of a clear standard definition of myoclonic status epilepticus continues to cloud prognostication, as some papers have relied on the clinical presence of sustained myoclonus (Arnoldus & Lammers, 1995; Wijdicks et al., 1994) regardless of EEG correlation. When outcomes were examined in post-TTM patients with myoclonus with or without EEG evidence of seizures, those patients with corresponding poor EEG (suppression-burst background with spike-wave discharges in lockset with myoclonic jerks) had a much poorer prognosis (Elmer et al., 2016), but even with these stricter criteria, 1% of these patients have good outcomes (Seder et al., 2015).
Absent SSEP within the first week was also predictive of poor recovery. The only class I study (Zandbergen et al., 2006) and six class III studies (Bassetti, Bomio, Mathis, & Hess, 1996; Berek et al., 1995; Chen et al., 1996; Gendo et al., 2001; Logi, Fischer, Murri, & Mauguiere, 2003; Madl et al., 2000) observed that no patient with bilaterally absent N20 response ever recovered. A single class III study (Young, Doig, & Ragazzoni, 2005) had a false-positive rate of 6%. A meta-analysis of these eight studies (Wijdicks, 2006) demonstrated a PPV of 99.3% with a sensitivity around 50%. Post-TTM studies have generally supported SSEP as a highly specific predictor of poor outcomes (Bisschops, van Alfen, van der Hoeven, & Hoedemaekers, 2011; Bouwes et al., 2009; Leithner, Ploner, Hasper, & Storm, 2010; Rossetti et al., 2010; Tiainen, Kovala, Takkunen, & Roine, 2005) with a few controversial good outcomes (Bouwes et al., 2012; Dragancea et al., 2015).
An earlier meta-analysis and recent comparative, prospective study by a group in the Netherlands (Zandbergen et al., 2006; Zandbergen, de Haan, Stoutenbeek, Koelman, & Hijdra, 1998) evaluating various early prediction of poor outcome, including clinical examination, brain enzymes, and electrophysiology, demonstrated that absence of SSEP at any time within the first week was the most useful predictor of poor outcome. This has been validated (Geocadin et al., 2006) showing that this was the clinical parameter most relied upon by neurologists to estimate prognosis.
9.4.4 Neuroimaging
Imaging is frequently obtained in survivors of cardiac arrest, but to date, there is no datum on the utility of these modalities to predict outcome in survivors of cardiac arrest. While highly informative, the subjective interpretation and day-to-day variability in abnormalities (Greer et al., 2011) has diminished imaging’s utility as a reliable outcome prognosticator. Early CT findings of comatose patients revealed diffuse cerebral edema and occasional low densities in the basal ganglia, thalamus, or watershed distributions (Fujioka, Okuchi, Sakaki, Hiramatsu, & Iwasaki, 1994; Kjos, Brant-Zawadzki, & Young, 1983). MRI in comatose cardiac arrest patients using fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted (DW) imaging demonstrated early signal abnormalities in the cerebral cortex, cerebellum, thalamus, and hippocampus (Wijdicks, Campeau, & Miller, 2001), and in the cerebral white matter (Chalela, Wolf, Maldjian, & Kasner, 2001). (See Fig. 9.1 for a representation of images of a comatose survivor of a cardiac arrest who died 3 days later.)
Not surprisingly after a direct metabolic injury to neurons, there is a significant reduction in brain metabolic activity in patients with acute cardiac arrest. Mean cerebral glucose utilization in vegetative or comatose subjects is reduced by 38% (Roine et al., 1991) to 50% (DeVolder et al., 1990), compared to a 25% reduction in conscious patients. The reduction is in the watershed distributions of the cerebral cortex, the basal ganglia, and the thalamus. Progressive decline of oxygen metabolism may foretell prolonged coma (Edgren, Enblad, Grenvik, & Langstrom, 2003).
Although non-randomized and non-prospective, these imaging studies do offer some useful markers of a bad outcome (death or severe disability): brain swelling on CT scan on day 3 (Morimoto, Kemmotsu, Kitami, Matsubara, & Tedo, 1993), extensive abnormalities on MRI DWI and FLAIR images (Wijdicks et al., 2001), and >50% perfusion deficits of the supratentorial brain on SPECT scan (Roine et al., 1991). The converse is less useful: structural imaging may be normal in patients who will survive with substantial neurological deficits (Alexander, 1997; Carbonnel, Charnallet, David, & Pellat, 1997; De Renzi & Lucchelli, 1993; Rupright, Woods, & Singh, 1996; Speach, Wong, Cattarin, & Livecchi, 1998).
More recently the use of quantitative image analysis at around day 3 can be used as adjunctive information to improve diagnostic accuracy in predicting poor outcome while maintaining specificity using CT measurements (Kim et al., 2013; Wu et al., 2011) or DWI analysis (Hirsch et al., 2016; Kim et al., 2016; Wijman et al., 2009; Wu et al., 2009). Analysis of thresholds remains variable and subjective; thus, its use as a stand-alone prognosticator has not been demonstrated. The advent of resting-state functional connectivity MRI analysis may hold promise because preliminary studies have demonstrated a reduction in the default mode connectivity, maybe associated with poor outcome (Koenig et al., 2014; Norton et al., 2012).
9.4.5 Summary
The recent study by the Netherlands group (Zandbergen et al., 2006) also examined whether the predictive values of various tests and clinical findings were additive in increasing sensitivity. They found that the combination of the SSEP and NSE raised the sensitivity to 66% and the addition of EEG (burst suppression or worse pattern) increased it to 71% while maintaining 100% PPV.
The current recommendations from the American Academy of Neurology (Wijdicks, 2006), updated by the European Resuscitation Council (Nolan et al., 2015) involves a decision tree using the variables pupillary light reflex, corneal reflex, motor response to pain, myoclonic status epilepticus, NSE, and SSEP to aid in the prediction of outcome in survivors of cardiac arrest. This algorithm involves the near certain prognosis of a poor outcome with absent brainstem reflexes (pupillary and corneal reflexes) or absent N20 responses on the SSEP after 72 h, and the likely prognosis of a poor outcome with the presence of status myoclonus, unreactive burst suppression or worse on EEG, or elevated serum NSE after 72 h. Even with the adoption of this algorithm, the sensitivity remains poor.
There remains no clinical finding or test result that reliably predicts a good outcome.
9.5 Course of Recovery
Caronna and Finklestein (1978) have proposed that patients in coma for less than 12 h suffer from a reversible encephalopathy and usually make a rapid and complete recovery, whereas the more severe hypoxic–ischemic patients are in coma for longer than 12 h and suffer structural damage to specific brain regions. In regard to time to awakening, several studies (Earnest et al., 1979; Longstreth et al., 1983; Snyder et al., 1980) found that 15–27% were awake upon arrival to the hospital and 20–43% of survivors would awaken after 12 h. The most common recovery pattern was of early in-hospital awakening to a confusional state to clearing of cognitive deficits (at least overt ones) during the hospitalization (Levy et al., 1985; Longstreth et al., 1983; Snyder et al., 1980). This has been supported by anecdotal case reports of patients progressing from coma to reportedly normal within 24 h (Sabah, 1969) and of isolated amnestic syndromes recovering over 10 days (Finklestein & Caronna, 1978).
As outlined above, there is a fairly inviolate relationship between duration of coma and the quality of recovery. For coma greater than 4 days, the probability of a good outcome falls dramatically (Longstreth et al., 1983). Patients who present comatose who do not wake up will progress to brain death or vegetative state, a state of wakefulness without detectable awareness (Jennett & Plum, 1972). A vegetative state present 1 month after brain trauma is defined as a persistent vegetative state (Multi-Society Task Force on PV, 1994). Among all nontraumatic causes, 53% die, 32% remain in persistent vegetative state, and 15% recover consciousness (1994). Of those who awoke, only 1 out of 15 had a good outcome, but the underlying etiology of that one patient was not clarified. The remaining 14 were severely disabled, many with minimal communication at best and all dependent (Higashi et al., 1981). Estraneo et al. (2013) followed 43 anoxic patients for 2 years after entering persistent vegetative state and found only 9 awoke, all with severe disabilities. Thus, contrary to traumatic brain injury, all patients who remain unresponsive for more than 1 month following anoxic brain injury have poor outcomes.
For those who awaken, the course of recovery is, however, similar for all injuries, except for the severe injuries—slower and incomplete. All patients awaken, that is, their eyes open, marking the end of coma in the narrowest sense. More mildly injured patients progress almost immediately into a confusional state. More severely injured patients remain vegetative—eyes open, random eye movements without fixation, and without any directed responsiveness—before moving into a confusional state.
Confusional states are conditions of impaired attention with or without impaired arousal. They are characterized by reduced ability to sustain attentional focus, easy distractibility, poor registration of new information, and defective recall of experience. Patients are often agitated. Sleep is often disrupted. Over hours to weeks, depending on severity, confusion clears, that is, attention improves. Only when confusion has cleared, can the nature and severity of residual deficits be judged.
Determination of the overall distribution of severity of residual deficits will be influenced by the timing and setting of patient accrual, and by the measure of severity. One prospective study of patients in coma for at least 12 h (Caronna & Finklestein, 1978) demonstrated 3-month mortality of 60%, severe disability or vegetative state of 20%, moderate disability of 8%, and good recovery of 12% (30% of all survivors). Differences in “moderate” and “mild” probably reflect differences in measures used. Another prospective study included patients who had already survived at least 3 weeks and were medically stable enough to be evaluated for definitive cardiac management. The percentages with good recovery was 28% at initial (3 weeks) evaluation, 43% at about 2 months, and 71% at 6 months (Sauve, Doolittle, Walker, Paul, & Scheinman, 1996). This study suggests that there exists a subgroup of patients who will have some late recovery. In a retrospective, population-based chart review, Graves et al. (1997), using the poorly sensitive cerebral performance category (CPC), revealed that after 1 year 29% of patients in CPC3 and 77% of patients CPC2 improved by at least one performance category. Case reports also mention severely impaired patients who make remarkable recovery within the first 1–3 months of injury (Goh, Heath, Ellis, & Oakley, 2002; Kam, Yoong, & Ganendran, 1978; Kaplan, 1999). Contrary to the above studies, Kim et al. (2016), also relying on the CPC, showed that only 4% of their patients improved from CPC 3 to CPC 2 over the first 6 months, and none improved after 6 months.
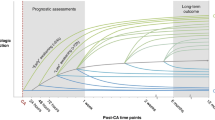
Patients admitted to rehabilitation centers will be the ones with persistent significant deficits once medically stable, but not such severe deficits that they cannot participate in therapies. The point of initial assessment will usually be 2–4 weeks after arrest. Fertl, Vass, Sterz, Gabriel, and Auff (2000) observed that 35% of their patients, all with CPC of 3, improved one performance category and 10% improved two categories during the 3-month rehabilitation. They also noted an improvement of the mean Barthel index of all their patients from 28 to 61. At time of discharge from rehabilitation hospital, 35% had moderate and 55% had severe deficits. Roine et al. (1993) traced cognitive recovery, albeit with a very coarse instrument for this purpose, the Mini Mental State Exam, and found very little change after 3 months. Others have noted no improvement after 4 months (Groswasser, Cohen, & Cosfeff, 1989) or 8 months (Drysdale, Grubb, Fox, & O’Carroll, 2000). We prospectively followed 25 survivors for 1 year and noted (1) the bulk of the recovery occurred within 3 months, (2) there was no further recovery of memory function after 3 months (see Fig. 9.2), (3) memory performance predicted quality of life (Lim, Verfaellie, Schnyer, Lafleche, & Alexander, 2014).
9.6 Residual Deficits
The focus of this discussion will be on the cognitive deficits because those are almost universally most limiting. The majority of the literature consists of case reports motivated by interest in the cognitive impairment rather than the range of neurological consequences of cardiac arrest. Some investigators were indifferent to the etiology of the hypoxic event. Most group studies followed the same approach, with only a few examining the patterns, frequency, and natural history of the survivors of cardiac arrests. In some reports, there was a broad latitude in the diagnosis of a hypoxic event, and in others, multiple etiologies of hypoxia were considered together without isolating the cardiac arrest patients from other etiologies. We will describe the specific persistent cognitive impairments that have been reported as well as where those impairments fit into the more common characterization of arrest outcomes by severity.
The case reports examining some aspects of cognition after cardiac arrest do offer some insight into the nature of possible impairments. We found 22 case reports with 39 patients who suffered an uncomplicated cardiac arrest (Table 9.1). There were two cases presenting with virtually unique clinical syndromes, one with loss of semantic knowledge (Alexander) and the other with delayed dystonia (Boylan). There were three cases with cognitive deficits in a single domain, with two amnestic (Cummings and Volpe) and one with visual perceptive problems (Rizzo). Based on the clinical description of the cases, we arbitrarily divided the patients into three categories: mild, moderate, or severe. One case had no deficits, nine cases had multiple deficits of moderate severity, and 12 cases had severe deficits. The remaining 12 cases had insufficient clinical or neuropsychological information to categorize. A large number of case reports did not have an isolated cardiac arrest.
The patients in the moderate-injury category presented with a very wide range of signs and symptoms. Coma duration ranged from 15 min to 1 week. Some awoke with no initially reported neurological abnormalities (Reich, case 6), and others were confused and disoriented (McNeill). All patients had deficits in more than one domain.
Of the 12 severe cases, eight reported coma duration, and all were comatose for more than 24 h. Two other cases were confirmed to have been in coma, but the duration was not provided. All four patients whose emergence from coma was described had a severe confusional state. All patients had deficits in every domain tested, although not all domains were tested or discussed in each case report.
The group studies, in contrast to the case reports, offer population-based information, but often lack detailed neuropsychological evaluations and frequently involved a mixed population. Roine et al. (1993) observed that the most common deficits among 68 consecutive survivors of cardiac arrest at 3 months were disorders of memory (49%), visuoconstructive dyspraxia (43%), and dyspraxia (42%), followed by problems with motivation (37%), depression (35%), programming of activity (34%), and dyscalculia (31%). Language disorders were uncommon (3%). The high frequency of memory disturbances has been confirmed by others, with ranges from 80% (Grubb et al., 2000) to 100% of patients examined (Kotila & Kajaste, 1984; Pusswald, Fertl, Faltl, & Auff, 2000). Visuospatial impairments have also been common, occurring in 30–100% of these patients. None of these studies specifically examined executive functions.
Wilson (1996) performed neuropsychological assessments in 18 survivors of cerebral hypoxia to explore for consistent cognitive profiles. Equipped with an unusually balanced battery of neuropsychological tests for this literature, she identified five distinct patterns: (1) an amnesic syndrome; (2) memory and executive deficits; (3) memory, executive, and visuospatial deficits; (4) isolated visuospatial impairments; and (5) widespread cognitive deficits. With the analysis restricted to survivors of cardiac arrests, there were three profiles: (1) memory and executive deficits; (2) memory, executive, and visuospatial deficits; and (3) widespread cognitive deficits. There were no isolated amnesic or visuospatial syndromes in her pure cardiac arrest patients, which seemed to occur more frequently from other causes of anoxia. Her patient population was small, but if isolated cognitive deficits occur after cardiac arrest, they must be at a very low frequency.
Volpe, Holtzman, and Hirst (1986) has reported the largest series of patients with isolated amnesia after cardiac arrest. These six patients had memory quotients at least 20 points below full-scale IQ, with normal performance on Ravens Progressive Matrices, the Wisconsin Card Sort task, and the Controlled Oral Word Association test. Clinical data, raw scores, and measures of motor control, mood, or behavior were not reported, but these patients appear to represent a pure amnestic syndrome.
It would seem likely that chronically amnestic patients might have hippocampal atrophy, and more diffusely impaired patients might have cortical atrophy. This hypothesis has been explored, although there are limitations because so many of the arrest survivors have implanted defibrillators now and cannot have an MRI. Grubb et al. (2000) compared MRI-brain volume in memory impaired and memory intact survivors of cardiac arrest. They did not find selective hippocampal atrophy in their memory impaired patients. Reduction in whole brain volume significantly correlated with memory impairment. Hopkins and colleagues have done MRI volumetric on a number of anoxic patients. In a series of papers comparing anoxic patients to controls, they (Hopkins & Kesner, 1995) found a reduction in hippocampal areas but not temporal lobe or parahippocampal gyrus volume. Another study (Hopkins et al., 1995) did suggest a relationship between morphological abnormalities with performance on cognitive testing, but was limited to three patients. The largest study comprised 13 patients, of whom only five had had a cardiac arrest, showed a strong correlation between performance on anterograde memory tests with both hippocampal and regional gray matter volume residuals (Allen, Tranel, Bruss, & Damasio, 2006).
We had the opportunity to study 11 cardiac arrest patients under the age of 80 years who were referred to a memory disorder clinic for persistent memory deficits (Lim, Alexander, LaFleche, Schnyer, & Verfaellie, 2004). Using standardized neuropsychological tests, we assessed their memory, executive function, perception, language and, motor function (see Table 9.2). Ten of our patients had moderate to severe memory impairment, and five had severe executive impairments. There was only one patient impaired in lexical-semantic function and only one with perceptual difficulties. Nine patients had moderate to severe impairments in motor function. We performed a k-means cluster analysis which produced a three-cluster solution that yielded a cluster with no impairments (patient 1), a second cluster with memory and motor impairments and variable executive dysfunction (patients 4–6), and a third cluster with impairments in all domains (patients 7–11). No patient had an isolated neurological disorder.
Our patient 1 and the small number of case reports with no deficit or only subtle deficits presumably exemplify the largest outcome group of survivors of cardiac arrest. These patients with good recovery usually emerge early from coma. Whether the neural injury was entirely transient and reversible, or simply too mild to cause lasting deficits is unknown. As with our patient, there may be relative decrements in performance that are obscured by arbitrary cutoffs on tests, or functional deficits that are not detectable by neuropsychological testing. These patients are likely to be underrepresented in the literature.
Patients in our cluster 2, the four patients reported in the Wilson’s study with memory and executive deficits (Wilson, 1996), and several of the case reports reviewed above uniformly had intermediate outcomes. The relationship between duration of coma and outcome is quite variable. We propose that these patients have not suffered permanent widespread cortical damage and may have damage restricted to the selectively vulnerable brain regions. To our knowledge, this hypothesis has not been directly addressed in any autopsy or adequately sensitive anatomical study. Our patients all had memory and motor impairments. We believe that executive deficits would also consistently have been detected if this group had been evaluated sooner after emergence from coma and confusion.
The patients in our cluster 3 and many of the patients whom we categorized as severe from case reports have similarly poor outcomes. These patients usually have long periods of coma (>24 h). In addition to memory and executive impairments, language and visuospatial functions are disturbed, suggesting that the injury likely involved cortex as well as the more vulnerable subcortical and hippocampal regions. Motor deficits might have been prominent if they had been consistently assessed.
Neither the results from our patient group nor a critical review of the literature support the notion that isolated disorders of visual perception or memory occur frequently following cardiac arrest. Thus, the evidence that classic, abrupt CA results in isolated damage to the hippocampus and produces long-standing isolated amnesia is much weaker than commonly assumed. This is not to conclude that it cannot happen because there are descriptions of amnesia following cardiac arrest. We propose, however, that the residual deficits in most patients who survive cardiac arrest will fall along a continuum reflecting the severity of injury to those electively vulnerable sites. Impairment will range from no or subtle impairments to a mix of executive, learning, and motor control deficits to such severe executive deficits that all cognitive functions are impaired—a virtual, chronic confusional state. Intermixed within these patterns are the rare cases of isolated memory or visuospatial deficits, or unusual presentations such as semantic memory loss or delayed dystonia.
9.7 Treatment
9.7.1 Temperature Management
In 2002, two studies showed that 24 h of therapeutic hypothermia (TH) within the first 4 h of a cardiac arrest will improve overall outcome and survival (Bernard et al., 2002; The Hypothermia after Cardiac Arrest Study Group, 2002). The improved outcomes may not be the result of hypothermia, rather the avoidance of hyperthermia (Gebhardt et al., 2013; Nielsen et al., 2013; Zeiner et al., 2001), although the general evidence still supports the use of TH (Arrich, Holzer, Havel, Müllner, & Herkner, 2016; Schenone et al., 2016). Current consensus guidelines advocates for the maintenance of temperature between 32 and 36 °C, now known as targeted temperature management (Nolan et al., 2015).
There are several distinct epochs of management, each with its own treatment imperatives. There are few therapeutic interventions that directly affect the outcome of survivors of out-of-hospital cardiac arrest. Pharmacological interventions that have proven to be ineffective include nimodipine (Roine et al., 1993), thiopental (Brain Resuscitation Clinical Trial I Study Group, 1986), magnesium and/or diazepam (Fatovich, Prentice, & Dobb, 1997; Longstreth, Fahrenbruch, & Olsufka, 2002), sodium bicarbonate (Vukmir & Katz, 2006), and amiodarone and lidocaine (Kudenchuk et al., 2016).
As described above, patients emerge from coma into vegetative states or confusional states. There are no clinical studies of potential treatments for vegetative state after cardiac arrest. Confusional state is usually a transient condition during recovery, and in milder injuries, it may be rapid enough that no treatment issues emerge. If there is a treatment concern, it is usually agitation. There are no controlled studies of treatment of agitation in this condition. Most adequately controlled studies are in the dementia literature. There are a few basic clinical observations that may assist management of confusion/agitation.
First, confusion and agitation are not synonymous. Treatment of confusion is probably limited to control of the environment around the patient—avoidance of over-stimulation, readily observed orientation material (calendars, clocks, pictures), and vigorous regularization of sleep phases. These should be implemented in every patient. Treatment of agitation should be modulated to the level of distress or inadvertent danger of injury that the patient presents. When possible, use of distractions may be sufficient—visits from family members, opportunities to converse with anyone on staff, recreational activities such as playing cards with a volunteer, watching sports on TV, etc. When the patient is very distressed, possibly becoming in inadvertent danger of injury or disruption of essential medical care, then supervision, passive restraints, and medications are required.
Second, the treatment targets of sleep onset and maintenance and of agitation reduction are not the same. Reduction of agitation should not produce excessive sleep or else sleep phases will become abnormal, probably worsening agitation. Second-generation antipsychotics such as quetiapine and olanzapine probably offer the best proportion of tranquilizing without excess sedation. Sleep onset is a separate problem, probably best addressed with standard hypnotics such as trazodone and short half-life benzodiazepines, but these medications will fail at sleep onset in a patient who is agitated, so they may require a preparatory dosage of antipsychotic to achieve a calm enough state that the hypnotic will be effective. Hypnotics should not be repeated too late at night or there will be further disruption of sleep phases due to daytime somnolence. Thus, management may require both treatments, each targeted at a specific factor.
For patients with significant residual deficits, there is at present little direct treatment. We could not identify any controlled studies or even large case reports of late rehabilitation interventions. We are aware of the off-label use of cholinesterase inhibitors, stimulants, and dopaminergic medications but with minimal sense of success and no reported claims of success. To judge by the reports of Grosswasser and Wilson described above—both reports coming from respected cognitive rehabilitation centers—there is little optimism that the fundamental deficits can be treated behaviorally. Whether patients with executive impairments after cardiac arrest might respond to some of the behavioral strategies that have been implemented in patients with trauma or focal frontal lesions is unknown.
There are many obstacles to the construction of useful interventions for these patients. We are not entirely clear about the nature of the residual deficits. Are they fundamentally executive function deficits? If so, there is a reasonable possibility of importing useful behavioral and medication treatments from the larger literature on treatment of trauma and focal lesions. When do they stabilize? How malleable are they over the post-acute epoch? Or do the patients who do not recover quickly also always have true memory system (hippocampal) injury as well? If so, behavioral treatments are likely to be insufficient to achieve any functional improvement. Until treatments become more effective or until acute management discovers a biological intervention that prevents acute cell death and apoptosis, there will be a growing population of inadequately treated patients at risk for poor quality of life.
9.8 Quality of Life
Impairment does not necessarily lead to disability and handicap, but the reported effects on quality of life have been variable. We found that coma duration of greater than 3 days or presence of memory impairment at 3 months were associated with reduced quality of life (Lim et al., 2014). Cardiac arrest survivors fare significantly worse in all categories of their QOL compared to a random control population (Bergner, Bergner, Hallstrom, Eisenberg, & Cobb, 1984), and when compared to survivors of myocardial infarcts (Bergner et al., 1985; Lim et al., 2014). de Vos, de Haes, Koster, and de Haan (1999) showed that the quality of life of their cardiac arrest survivors were worse than an elderly control population, but better than that of patients with strokes. An 8-year follow-up of cardiac arrest patients found that the quality of life in patients was considered good (Kuilman et al., 1999), but the study lacked age-matched controls.
Evaluating the number of patients able to live independently or return to work may be the most sensitive markers of impairment, disability, and handicap. As many as 30–75% of survivors who awaken early are able to return to their previous level of employment (Bergner et al., 1985; Earnest et al., 1980; Graves et al., 1997; Kragholm et al., 2015; Sauve, 1995; Sunnerhagen, Johansson, & Herlitz, 1996). On the other hand, only 25% of patients who remain in coma for greater than 12 h return to work (Lim et al., 2014), while in those admitted to rehabilitation hospitals, fewer than 10% return to work (Groswasser et al., 1989; Howard et al., 1987). Approximately one-half of all survivors achieve full independence in all aspects of daily living (Earnest et al., 1980; Howard et al., 1987; Sunnerhagen et al., 1996) although many require substantial supervision and assistance for instrumental activities, finances, and social activities (Sauve, 1995). There is no datum on return to driving.
Notes
- 1.
Cerebral performance category: CPC of 1 indicates good cerebral performance but may have minor psychological or neurological deficits. CPC of 2 indicates moderate cerebral disability typically resulting in impairment of activities of daily living. CPC of 3 is severe cerebral disability with dependence upon others for daily support. CPC of 4 is coma or vegetative state, and CPC of 5 is death.
References
Al Thenayan, E., Savard, M., Sharpe, M., Norton, L., & Young, B. (2008). Predictors of poor neurologic outcome after induced mild hypothermia following cardiac arrest. Neurology, 71(19), 1535–1537. https://doi.org/10.1212/01.wnl.0000334205.81148.31
Alexander, M. P. (1997). Specific semantic memory loss after hypoxic-ischemic injury. Neurology, 48, 165–173.
Allen, J. S., Tranel, D., Bruss, J., & Damasio, H. (2006). Correlations between regional brain volumes and memory performance in anoxia. Journal of Clinical and Experimental Neuropsychology, 28(4), 457–476. https://doi.org/10.1080/13803390590949287
Allison, R. S., Bedford, P. D., & Meyer, A. (1956). Discussion on the clinical consequence of cerebral anoxia. Proceedings of the Royal Society of Medicine, 49, 609–619.
Armengol, C. G. (2000). Acute oxygen deprivation: Neuropsychological profiles and implications for rehabilitation. Brain Injury, 14, 237–250.
Arnoldus, E. P., & Lammers, G. J. (1995). Postanoxic coma: Good recovery despite myoclonus status. Annals of Neurology, 38(4), 697–698.
Arrich, J., Holzer, M., Havel, C., Müllner, M., & Herkner, H. (2016). Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation. The Cochrane Database of Systematic Reviews, 2, CD004128. https://doi.org/10.1002/14651858.CD004128.pub4
Auer, R. N., & Benveniste, H. (1994). Hypoxia and related conditions. In S. Greenfield (Ed.), Neuropathology (pp. 263–314). London: Arnold.
Bass, E. (1985). Cardiopulmonary arrest. Annals of Internal Medicine, 103, 920–927.
Bassetti, C., Bomio, F., Mathis, J., & Hess, C. W. (1996). Early prognosis in coma after cardiac arrest: A prospective clinical, electrophysiological, and biochemical study of 60 patients. Journal of Neurology, Neurosurgery and Psychiatry, 61(6), 610–615.
Becker, L. B., Ostrander, M. P., Barrett, J., & Kondos, G. T. (1991). Outcome of CPR in a large metropolitan area – Where are the survivors. Annals of Emergency Medicine, 20, 355–361.
Berek, K., Lechleitner, P., Luef, G., Felber, S., Saltuari, L., Schinnerl, A., … Aichner, F. (1995). Early determination of neurological outcome after prehospital cardiopulmonary resuscitation. Stroke; a Journal of Cerebral Circulation, 26(4), 543–549.
Bergner, L., Bergner, M., Hallstrom, A. P., Eisenberg, M. S., & Cobb, L. A. (1984). Health status of survivors of out-of-hospital cardiac arrest six months later. American Journal of Public Health, 74, 508–510.
Bergner, L., Hallstrom, A. P., Bergner, M., Eisenberg, M. S., & Cobb, L. A. (1985). Health status of survivors of cardiac arrest and of myocardial infarction controls. American Journal of Public Health, 75(11), 1321–1323.
Bernard, S. A., Gray, T. W., Buist, M. D., Jones, B. M., Silvester, W., Gutteridge, G., & Smith, K. (2002). Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. The New England Journal of Medicine, 346, 557–563.
Bisschops, L. L., van Alfen, N., van der Hoeven, J. G., & Hoedemaekers, C. W. (2011). Predictive value of neurologic prognostic indicators in hypothermia after cardiac arrest. Annals of Neurology. https://doi.org/10.1002/ana.22394
Bouwes, A., Binnekade, J. M., Kuiper, M. A., Bosch, F. H., Zandstra, D. F., Toornvliet, A. C., … Horn, J. (2012). Prognosis of coma after therapeutic hypothermia: A prospective cohort study. Annals of Neurology, 71(2), 206–212. https://doi.org/10.1002/ana.22632
Bouwes, A., Binnekade, J. M., Zandstra, D. F., Koelman, J. H., van Schaik, I. N., Hijdra, A., & Horn, J. (2009). Somatosensory evoked potentials during mild hypothermia after cardiopulmonary resuscitation. Neurology, 73(18), 1457–1461. https://doi.org/10.1212/WNL.0b013e3181bf98f4
Brain Resuscitation Clinical Trial I Study Group. (1986). Randomized clinical study of thiopental loading in comatose survivors of cardiac arrest. New England Journal of Medicine, 314(7), 397–403.
Carbonnel, S., Charnallet, A., David, D., & Pellat, J. (1997). One of several semantic systems(s)? Maybe none: Evidence form a case study of modality and category-specific “semantic” impairement. Cortex; A Journal Devoted to the Study of the Nervous System and Behavior, 33, 391–417.
Caronna, J. J., & Finklestein, S. (1978). Neurological syndromes after cardiac arrest. Stroke; A Journal of Cerebral Circulation, 9(5), 517–520.
Chalela, J. A., Wolf, R. L., Maldjian, J. A., & Kasner, S. E. (2001). MRI identification of early white matter injury in anoxic-ischemic encephalopathy. Neurology, 56(4), 481–485.
Chan, P. S., McNally, B., Nallamothu, B. K., Tang, F., Hammill, B. G., Spertus, J. A., & Curtis, L. H. (2016). Long-term outcomes among elderly survivors of out-of-hospital cardiac arrest. Journal of the American Heart Association, 5(3), e002924. https://doi.org/10.1161/JAHA.115.002924
Chan, P. S., McNally, B., Tang, F., Kellermann, A., & CARES Surveillance Group. (2014). Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation, 130(21), 1876–1882. https://doi.org/10.1161/CIRCULATIONAHA.114.009711
Chen, R., Bolton, C. F., & Young, G. B. (1996). Prediction of outcome in patients with anoxic coma: A clinical and electrophysiologic study. Critical Care Medicine, 24, 672–678.
Cummings, R. O., Chamberlain, D. A., Abramson, N. S., Allen, M., Baskett, P., Becker, L., … Theis, W. H. (1991). Recommended guidlines for uniform reporting of data from out-of-hospital cardiac arrest: The utstein style. Annals of Emergency Medicine, 20, 861–874.
Cummins, R. O., Ornato, J. P., Thies, W. H., & Pepe, P. E. (1991). Improving survival from sudden cardiac arrest: The “chain of survival” concept. Circulation, 83, 1832–1847.
De Renzi, E., & Lucchelli, F. (1993). Dense retrograde amnesia, intact learning capability and abnormal forgetting rate: A consolidation deficit? Cortex; A Journal Devoted to the Study of the Nervous System and Behavior, 29, 449–466.
de Vos, R., de Haes, H., Koster, R. W., & de Haan, R. J. (1999). Quality of life after cardiopulmonary resuscitation. Archives of Internal Medicine, 159, 249–254.
DeVolder, A. G., Goffinet, A. M., Bol, A., Michel, C., de Barsy, T., & Laterre, C. (1990). Brain glucose metabolism in postanoxic syndrome. Archives of Neurology, 47, 197–204.
Dragancea, I., Horn, J., Kuiper, M., Friberg, H., Ullén, S., Wetterslev, J., … TTM Trial Investigators. (2015). Neurological prognostication after cardiac arrest and targeted temperature management 33°C versus 36°C: Results from a randomised controlled clinical trial. Resuscitation, 93, 164–170. https://doi.org/10.1016/j.resuscitation.2015.04.013.
Drysdale, E. E., Grubb, N. R., Fox, K. A. A., & O’Carroll, R. E. (2000). Chronicity of memory impairment in long-term out-of-hospital cardiac arrest survivors. Resuscitation, 47, 27–32.
Earnest, M. P., Breckinridge, J. C., Yarnell, P. Y., & Oliva, P. B. (1979). Quality of survival after out-of-hospital cardiac arrest: Predictive value of early neurologic evaluation. Neurology, 29, 56–60.
Earnest, M. P., Yarnell, P. Y., Merrill, S. L., & Knapp, G. L. (1980). Long-term survival and neurologic status after resuscitation from out-of-hospital cardiac arrest. Neurology, 30, 1298–1302.
Edgren, E., Enblad, P., Grenvik, A., & Langstrom, B. (2003). Cerebral blood flow and metabolism after cardiopulmonary resuscitation. A pathophysiologic and prognostic positron emission tomography pilot study. Resuscitation, 57, 161–170.
Edgren, E., Hedstrand, U., Kelsey, S., Sutton-Tyrrell, K., & Safar, P. (1994). Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I study group. Lancet (London, England), 343(8905), 1055–1059.
Edgren, E., Hedstrand, U., Nordin, M., Rydin, E., & Ronquist, G. (1987). Prediction of outcome after cardiac arrest. Critical Care Medicine, 15, 820–825.
Eisenburger, P., List, M., Schörkhuber, W., Walker, R., Sterz, F., & Laggner, A. N. (1998). Long-term cardiac arrest survivors of the Vienna emergency medical service. Resuscitation, 38(3), 137–143.
Elmer, J., Rittenberger, J. C., Faro, J., Molyneaux, B. J., Popescu, A., Callaway, C. W., … Pittsburgh Post-Cardiac Arrest Service. (2016). Clinically distinct electroencephalographic phenotypes of early myoclonus after cardiac arrest. Annals of Neurology, 80(2), 175–184. https://doi.org/10.1002/ana.24697.
Estraneo, A., Moretta, P., Loreto, V., Lanzillo, B., Cozzolino, A., Saltalamacchia, A., … Trojano, L. (2013). Predictors of recovery of responsiveness in prolonged anoxic vegetative state. Neurology, 80(5), 464–470. https://doi.org/10.1212/WNL.0b013e31827f0f31
Fatovich, D. M., Prentice, D. A., & Dobb, G. J. (1997). Magnesium in cardiac arrest (the magic trial). Resuscitation, 35(3), 237–241.
Fertl, E., Vass, K., Sterz, F., Gabriel, H., & Auff, E. (2000). Neurological rehabilitation of severely disabled cardiac arrest survivors. Part I. Course of post-acute inpatient treatment. Resuscitation, 47(3), 231–239.
Finklestein, S., & Caronna, J. J. (1978). Amnestic syndrome following cardiac arrest. Neurology, 28, 389.
Fischer, M., Fischer, N. J., & Schüttler, J. (1997). One-year survival after out-of-hospital cardiac arrest in Bonn city: Outcome report according to the ‘utstein style’. Resuscitation, 33(3), 233–243.
Fujioka, M., Okuchi, K., Sakaki, T., Hiramatsu, K. -I., & Iwasaki, S. (1994). Specific changes in human brain following reperfusion after cardiac arrest. Stroke; a Journal of Cerebral Circulation, 25, 2091–2095.
Gaieski, D. F., Agarwal, A. K., Abella, B. S., Neumar, R. W., Mechem, C., Cater, S. W., … Band, R. A. (2017). Adult out-of-hospital cardiac arrest in Philadelphia from 2008–2012: An epidemiological study. Resuscitation, 115, 17–22. https://doi.org/10.1016/j.resuscitation.2017.03.023
Gebhardt, K., Guyette, F. X., Doshi, A. A., Callaway, C. W., Rittenberger, J. C., & Post Cardiac Arrest Service. (2013). Prevalence and effect of fever on outcome following resuscitation from cardiac arrest. Resuscitation, 84(8), 1062–1067. https://doi.org/10.1016/j.resuscitation.2013.03.038
Gendo, A., Kramer, L., Hafner, M., Funk, G. C., Zauner, C., Sterz, F., … Madl, C. (2001). Time-dependency of sensory evoked potentials in comatose cardiac arrest survivors. Intensive Care Medicine, 27(8), 1305–1311.
Geocadin, R. G., Buitrago, M. M., Torbey, M. T., Chandra-Strobos, N., Williams, M. A., & Kaplan, P. W. (2006). Neurologic prognosis and withdrawal of life support after resuscitation from cardiac arrest. Neurology, 67(1), 105–108.
Goh, W. C., Heath, P. D., Ellis, S. J., & Oakley, P. A. (2002). Neurological outcome prediction in a cardiorespiratory arrest survivor. British Journal of Anaesthesia, 88(5), 719–722.
Gold, B., Puertas, L., Davis, S. P., Metzger, A., Yannopoulos, D., Oakes, D. A., … Lurie, K. G. (2014). Awakening after cardiac arrest and post resuscitation hypothermia: Are we pulling the plug too early? Resuscitation, 85(2), 211–214. https://doi.org/10.1016/j.resuscitation.2013.10.030
Goto, Y., Funada, A., & Goto, Y. (2016). Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out-of-hospital cardiac arrest: A prospective, nationwide, population-based cohort study. Journal of the American Heart Association, 5(3), e002819. https://doi.org/10.1161/JAHA.115.002819
Graves, J. R., Herlitz, J., Bång, A., Axelsson, A., Ekström, L., Holmberg, M., … Holmberg, S. (1997). Survivors of out of hospital cardiac arrest: Their prognosis, longevity and functional status. Resuscitation, 35(2), 117–121.
Greer, D. (2013). Unexpected good recovery in a comatose post-cardiac arrest patient with poor prognostic features. Resuscitation, 84(6), e81–e82. https://doi.org/10.1016/j.resuscitation.2013.02.011
Greer, D., Scripko, P., Bartscher, J., Sims, J., Camargo, E., Singhal, A., & Furie, K. (2011). Serial MRI changes in comatose cardiac arrest patients. Neurocritical Care, 14(1), 61–67. https://doi.org/10.1007/s12028-010-9457-8
Grossestreuer, A. V., Abella, B. S., Leary, M., Perman, S. M., Fuchs, B. D., Kolansky, D. M., … Gaieski, D. F. (2013). Time to awakening and neurologic outcome in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation, 84(12), 1741–1746. https://doi.org/10.1016/j.resuscitation.2013.07.009
Groswasser, Z., Cohen, M., & Cosfeff, H. (1989). Rehabilitation outcome after anoxic brain damage. Archives of Physical Medicine and Rehabilitation, 70, 186–188.
Grubb, N. R., Fox, K. A. A., Smith, K., Best, J., Blane, A., Ebmeier, K. P., … O’Carroll, R. E. (2000). Memory impairment in out-of-hospital cardiac arrest survivors is associated with global reduction in brain volume, not focal hippocampal injury. Stroke; A Journal of Cerebral Circulation, 31, 1509–1513.
Hawker, K., & Lang, A. E. (1990). Hypoxic-ischemic damage of the basal ganglia. Movement Disorders, 5, 219–224.
Higashi, K., Hatano, M., Abiko, S., Ihara, K., Katayama, S., Wakuta, Y., … Yamashita, T. (1981). Five-year follow-up study of patients with persistent vegetative state. Journal of Neurology, Neurosurgery, and Psychiatry, 44(6), 552–554.
Hirsch, K. G., Mlynash, M., Eyngorn, I., Pirsaheli, R., Okada, A., Komshian, S., … Albers, G. W. (2016). Multi-center study of diffusion-weighted imaging in coma after cardiac arrest. Neurocritical Care, 24(1), 82–89. https://doi.org/10.1007/s12028-015-0179-9
Hlatky, M., Saynina, O., McDonald, K., Garber, A., & McClellan, M. (2002). Utilization and outcomes of the implantable cardioverter defibrillator, 1987 to 1995. American Heart Journal, 144(3), 397–403. https://doi.org/10.1067/mhj.2002.125496
Hopkins, R. O., Gale, S. D., Johnson, S. C., Anderson, C. V., Bigler, E. D., Blatter, D. D., & Weaver, L. K. (1995). Severe anoxia with and without concomitant brain atrophy and neuropsychological impairments. JINS, 1, 501–509.
Hopkins, R. O., & Kesner, R. P. (1995). Item and order recognition memory in subjects with hypoxic brain injury. Brain and Cognition, 27, 180–201.
Horn, M., & Schlote, W. (1992). Delayed neuronal death and delayed neuronal recovery in the human brain following global ischemia. Acta Neuropathologica, 85, 79–87.
Howard, R., Trend, P., & Ross Russell, R. W. (1987). Clinicial features of ischemia in cerebral arterial border zones after periods of reduced cerebral blood flow. Archives of Neurology, 44, 934–940.
Jennett, B., & Plum, F. (1972). Persistent vegetative state after brain damage. A syndrome in search of a name. Lancet (London, England), 1(7753), 734–737.
Kam, C. A., Yoong, F. F. Y., & Ganendran, A. (1978). Cortical blindness following hypoxia during cardiac arrest. Anaesthesia and Intensive Care, 6, 143–145.
Kaplan, C. P. (1999). Anoxic-hypotensive brain injury: Neuropsychological performance at 1 month as an indicator of recovery. Brain Injury, 13, 305–310.
Karkela, J., Bock, E., & Kaukinen, S. (1993). CSF and serum brain-specific creatine kinase isoenzymes (CK-BB), neuron-specific enolase (NSE), and neural cell adhesion molecule (NCAM) as prognostic makers for hypoxic brain injury after cardiac arrest in man. Journal of Neurological Sciences, 116, 100–109.
Karkela, J., Pasanen, M., Kaukinen, S., Morsky, P., & Harmoinen, A. (1992). Evaluation of hypoxic brain injury with spinal fluid enzymes, lactate, and pyruvate. Critical Care Medicine, 20, 378–386.
Kase, C. S., Troncoso, J. F., Court, J. E., Tapia, J. E., & Mohr, J. P. (1977). Global spatial disorientation. Journal of the Neurological Sciences, 34, 267–278.
Kim, J., Kim, K., Suh, G. J., Kwon, W. Y., Kim, K. S., Shin, J., … Ha, C. (2016). Prognostication of cardiac arrest survivors using low apparent diffusion coefficient cluster volume. Resuscitation, 100, 18–24. https://doi.org/10.1016/j.resuscitation.2015.12.013
Kim, S. H., Choi, S. P., Park, K. N., Youn, C. S., Oh, S. H., & Choi, S. M. (2013). Early brain computed tomography findings are associated with outcome in patients treated with therapeutic hypothermia after out-of-hospital cardiac arrest. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 21, 57. https://doi.org/10.1186/1757-7241-21-57
Kitamura, T., Iwami, T., Kawamura, T., Nitta, M., Nagao, K., Nonogi, H., … Japanese Circulation Society Resuscitation Science Study Group. (2012). Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation, 126(24), 2834–2843. https://doi.org/10.1161/CIRCULATIONAHA.112.109496.
Kjos, B. O., Brant-Zawadzki, M., & Young, R. G. (1983). Early CT findings of global central nervous system hypoperfusion. AJR. American Journal of Roentgenology, 4, 1043–1048.
Koenig, M. A., Holt, J. L., Ernst, T., Buchthal, S. D., Nakagawa, K., Stenger, V. A., & Chang, L. (2014). MRI default mode network connectivity is associated with functional outcome after cardiopulmonary arrest. Neurocritical Care, 20(3), 348–357. https://doi.org/10.1007/s12028-014-9953-3
Kotila, M., & Kajaste, S. (1984). Neurological and neuropsychological symptoms after cardiac arrest. Acta Neurologica Scandinavica, 69(Suppl 98), 337.
Kragholm, K., Wissenberg, M., Mortensen, R. N., Fonager, K., Jensen, S. E., Rajan, S., … Rasmussen, B. S. (2015). Return to work in out-of-hospital cardiac arrest survivors: A nationwide register-based follow-up study. Circulation, 131(19), 1682–1690. https://doi.org/10.1161/CIRCULATIONAHA.114.011366
Kudenchuk, P. J., Brown, S. P., Daya, M., Rea, T., Nichol, G., Morrison, L. J., … Resuscitation Outcomes Consortium Investigators. (2016). Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. The New England Journal of Medicine, 374(18), 1711–1722. https://doi.org/10.1056/NEJMoa1514204.
Kuilman, M., Bleeker, J. K., Hartman, J. A., & Simoons, M. L. (1999). Long-term survival after out-of-hospital cardiac arrest: An 8-year follow-up. Resuscitation, 41(1), 25–31.
Kuisma, M., & Maata, T. (1996). Out-of-hospital cardiac arrest in Helsinki: Utstein style reporting. Heart, 76, 18–23.
Kuroiwa, T., & Okeda, R. (1994). Neuropathology of cerebral ischemia and hypoxia: Recent advances in experimental studies on its pathogenesis. Pathology International, 44, 171–181.
Ladwig, K. -H., Schoefinius, A., Danner, R., Rolf, G., Herman, R., Koeppel, A., & Hauber, P. (1997). Effects of early defibrillation by ambulance personnel on short- and long-term outcomes of cardiac arrest survival: The Munich experiment. Chest, 112, 1584–1591.
Lance, J. W., & Adams, R. D. (1963). The syndrome of intention or action myoclonus as a sequel to hypoxic encephalopathy. Brain: A Journal of Neurology, 86, 111–136.
Leithner, C., Ploner, C. J., Hasper, D., & Storm, C. (2010). Does hypothermia influence the predictive value of bilateral absent N20 after cardiac arrest? Neurology, 74(12), 965–969. https://doi.org/10.1212/WNL.0b013e3181d5a631
Levy, D. E., Caronna, J. J., Singer, B. H., Lapinski, R. H., Frydman, H., & Plum, F. (1985). Predicting outcome from hypoxic-ischemic coma. JAMA, 253, 1420–1426.
Liliang, P. C., Liang, C. L., Weng, H. C., Lu, K., Wang, K. W., Chen, H. J., & Chuang, J. H. (2010). Tau proteins in serum predict outcome after severe traumatic brain injury. The Journal of Surgical Research, 160(2), 302–307. https://doi.org/10.1016/j.jss.2008.12.022
Lim, C., Alexander, M. P., LaFleche, G., Schnyer, D. M., & Verfaellie, M. (2004). The neurological and cognitive sequelae of cardiac arrest. Neurology, 63(10), 1774–1778.
Lim, C., Verfaellie, M., Schnyer, D., Lafleche, G., & Alexander, M. P. (2014). Recovery, long-term cognitive outcome and quality of life following out-of-hospital cardiac arrest. Journal of Rehabilitation Medicine. https://doi.org/10.2340/16501977-1816
Logi, F., Fischer, C., Murri, L., & Mauguiere, F. (2003). The prognostic value of evoked responses from primary somatosensory and auditory cortex in comatose patients. Clinical Neurophysiology: Official Journal of the International Federation of Clinical Neurophysiology, 114(9), 1615–1627.
Lombardi, G., Gallagher, E. J., & Gennis, P. (1994). Outcome of out-of-hospital cardiac arrest in New York city. JAMA, 271, 678–683.
Longstreth, W. T., Fahrenbruch, C. E., & Olsufka, M. (2002). Randomized clinical trial of magnesium, diazepam, or both after out-of-hospital cardiac arrest. Neurology.
Longstreth, W. T., Inui, T. S., Cobb, L. A., & Copass, M. K. (1983). Neurologic recovery after out-of-hospital cardiac arrest. Annals of Internal Medicine, 98, 588–592.
Madison, D., & Niedermeyer, E. (1970). Epileptic seizures resulting from acute cerebral anoxia. Journal of Neurology, Neurosurgery and Psychiatry, 33, 381–386.
Madl, C., Kramer, L., Domanovits, H., Woolard, R. H., Gervais, H., Gendo, A., … Sterz, F. (2000). Improved outcome prediction in unconscious cardiac arrest survivors with sensory evoked potentials compared with clinical assessment. Critical Care Medicine, 28(3), 721–726.
Mattsson, N., Zetterberg, H., Nielsen, N., Blennow, K., Dankiewicz, J., Friberg, H., … Cronberg, T. (2017). Serum tau and neurological outcome in cardiac arrest. Annals of Neurology, 82(5), 665–675. https://doi.org/10.1002/ana.25067
McNally, B., Robb, R., Mehta, M., Vellano, K., Valderrama, A. L., Yoon, P. W., … Centers for Disease Control and Prevention. (2011). Out-of-hospital cardiac arrest surveillance—Cardiac arrest registry to enhance survival (CARES), United States, October 1, 2005–December 31, 2010. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 60(8), 1–19.
Minino, A. M., & Smith, B. L. (2001). Deaths: Preliminary data for 2000. National vital statistics report. National Vital Statistics Reports, 49, 1–40.
Morimoto, Y., Kemmotsu, O., Kitami, K., Matsubara, I., & Tedo, I. (1993). Acute brain swelling after out-of-hsopital cardiac arrest: Pathogenesis and outcome. Critical Care Medicine, 21, 104–110.
Mulder, M., Gibbs, H. G., Smith, S. W., Dhaliwal, R., Scott, N. L., Sprenkle, M. D., & Geocadin, R. G. (2014). Awakening and withdrawal of life-sustaining treatment in cardiac arrest survivors treated with therapeutic hypothermia. Critical Care Medicine, 42(12), 2493–2499. https://doi.org/10.1097/CCM.0000000000000540
Multi-Society Task Force on PV. (1994). Medical aspects of the persistent vegetative state. The New England Journal of Medicine, 330(22), 1572–1579. https://doi.org/10.1056/NEJM199406023302206
Murayama, S., Bouldin, T. W., & Suzuki, K. (1990). Selective sparing of Betz cells in primary motor area in hypoxia-ischemic encephalopathy. Acta Neuropathologica, 80, 560–562.
National Multiple Sclerosis Society. (2005). Multiple sclerosis: Just the facts. [Pamphlet].
Nielsen, N., Wetterslev, J., Cronberg, T., Erlinge, D., Gasche, Y., Hassager, C., … Friberg, H. (2013). Targeted temperature management at 33°C versus 36°C after cardiac arrest. The New England Journal of Medicine, 369(23), 2197–2206. https://doi.org/10.1056/NEJMoa1310519
Nolan, J. P., Soar, J., Cariou, A., Cronberg, T., Moulaert, V. R., Deakin, C. D., … European Society of Intensive Care Medicine. (2015). European resuscitation council and European society of intensive care medicine 2015 guidelines for post-resuscitation care. Intensive Care Medicine, 41(12), 2039–2056. https://doi.org/10.1007/s00134-015-4051-3.
Norton, L., Hutchison, R. M., Young, G. B., Lee, D. H., Sharpe, M. D., & Mirsattari, S. M. (2012). Disruptions of functional connectivity in the default mode network of comatose patients. Neurology, 78(3), 175–181. https://doi.org/10.1212/WNL.0b013e31823fcd61
Oksanen, T., Tiainen, M., Skrifvars, M. B., Varpula, T., Kuitunen, A., Castrén, M., & Pettilä, V. (2009). Predictive power of serum NSE and OHCA score regarding 6-month neurologic outcome after out-of-hospital ventricular fibrillation and therapeutic hypothermia. Resuscitation, 80(2), 165–170. https://doi.org/10.1016/j.resuscitation.2008.08.017
Ost, M., Nylén, K., Csajbok, L., Ohrfelt, A. O., Tullberg, M., Wikkelsö, C., … Nellgård, B. (2006). Initial CSF total tau correlates with 1-year outcome in patients with traumatic brain injury. Neurology, 67(9), 1600–1604. https://doi.org/10.1212/01.wnl.0000242732.06714.0f
Parkin, A. J., Miller, J., & Vincent, R. (1987). Multiple neuropsychological deficits due to anoxic encephalopathy: A case study. Cortex; A Journal Devoted to the Study of the Nervous System and Behavior, 1987, 655–665.
Petito, C. K., Feldmann, E., Pulsinelli, W., & Plum, F. (1987). Delayed hippocampal damage in humans following cardiorespiratory arrest. Neurology, 37, 1281–1286.
Pfeifer, R., Borner, A., Krack, A., Sigusch, H. H., Surber, R., & Figulla, H. R. (2005). Outcome after cardiac arrest: Predictive values and limitations of the neuroproteins neuron-specific enolase and protein S-100 and the Glasgow coma scale. Resuscitation, 65(1), 49–55.
Prohl, J., Bodenburg, S., & Rustenbach, S. J. (2009). Early prediction of long-term cognitive impairment after cardiac arrest. Journal of the International Neuropsychological Society: JINS, 15(3), 344–353. https://doi.org/10.1017/S1355617709090493
Pusswald, G., Fertl, E., Faltl, M., & Auff, E. (2000). Neurological rehabilitation of severely disabled cardiac arrest survivors. Part II. Life situation of patients and families after treatment. Resuscitation, 47(3), 241–248.
Rea, T. D. (2003). Temporal patterns in long-term survival after resuscitation from out-of-hospital cardiac arrest. Circulation, 108(10), 1196–1201. https://doi.org/10.1161/01.CIR.0000087403.24467.A4
Rea, T. D., Eisenberg, M. S., Becker, L. J., Murray, J. A., & Hearne, T. (2003). Temporal trends in sudden cardiac arrest. Circulation, 107(22), 2780–2785. https://doi.org/10.1161/01.CIR.0000070950.17208.2A
Reich, P., Regestein, Q. R., Murawski, B. L., DeSilva, R. A., & Lown, B. (1983). Unrecognized organic mental disorders in survivors of cardiac arrest. The American Journal of Psychiatry, 140, 1194–1197.
Roine, R. O., Kajaste, S., & Kaste, M. (1993). Neuropsychological sequelae of cardiac arrest. JAMA, 269, 237–242.
Roine, R. O., Launes, J., Nikkinen, P., Phil, L., Lindroth, L., & Kaste, M. (1991). Regional cerebral blood flow after human cardiac arrest. Archives of Neurology, 48, 625–629.
Rossetti, A. O., Oddo, M., Logroscino, G., & Kaplan, P. W. (2010). Prognostication after cardiac arrest and hypothermia: A prospective study. Annals of Neurology, 67(3), 301–307. https://doi.org/10.1002/ana.21984
Rossetti, A. O., Tovar Quiroga, D. F., Juan, E., Novy, J., White, R. D., Ben-Hamouda, N., … Rabinstein, A. A. (2017). Electroencephalography predicts poor and good outcomes after cardiac arrest: A two-center study. Critical Care Medicine, 45(7), e674–e682. https://doi.org/10.1097/CCM.0000000000002337
Rothstein, T. L., Thomas, E. M., & Sumi, S. M. (1991). Predicting outcome in hypoxic-ischemic coma. A prospective clinical and electrophysiological study. Electroencephalography and Clinical Neurophysiology, 79, 101–107.
Rundgren, M., Karlsson, T., Nielsen, N., Cronberg, T., Johnsson, P., & Friberg, H. (2009). Neuron specific enolase and S-100B as predictors of outcome after cardiac arrest and induced hypothermia. Resuscitation, 80(7), 784–789. https://doi.org/10.1016/j.resuscitation.2009.03.025
Rupright, J., Woods, E. A., & Singh, A. (1996). Hypoxic brain injury: Evaluation by single photon emission computed tomography. Archives of Physical Medicine and Rehabilitation, 77, 1205–1208.
Sabah, A. H. (1969). Blindness after cardiac arrest. Postgraduate Medical Journal, 44, 513–516.
Sauve, M. J. (1995). Long-term physical functioning and psychosocial adjustment in survivors of sudden cardiac death. Heart & Lung, 24, 1–20.
Sauve, M. J., Doolittle, N., Walker, J. A., Paul, S. M., & Scheinman, M. M. (1996). Factors associated with cognitive recovery after cardiopulmonary resuscitation. American Journal of Critical Care: An Official Publication, American Association of Critical-Care Nurses, 5(2), 127–139.
Sawada, H., Udaka, F., Seriu, N., Shindou, K., Kameyama, M., & Tsujimura, M. (1990). MRI demonstration of cortical laminar necrosis and delayed white matter injury in anoxic encephalopathy. Neuroradiology, 32, 319–321.
Sazbon, L., Zabreba, F., Ronen, J., Solzi, P., & Costeff, H. (1993). Course and outcome of patients in vegetative state of nontraumatic aetiology. Journal of Neurology, Neurosurgery, and Psychiatry, 56, 407–409.
Schenone, A. L., Cohen, A., Patarroyo, G., Harper, L., Wang, X., Shishehbor, M. H., … Duggal, A. (2016). Therapeutic hypothermia after cardiac arrest: A systematic review/meta-analysis exploring the impact of expanded criteria and targeted temperature. Resuscitation, 108, 102–110. https://doi.org/10.1016/j.resuscitation.2016.07.238
Schoerkhuber, W., Kittler, H., Sterz, F., Behringer, W., Holzer, M., Frossard, M., … Laggner, A. N. (1999). Time course of serum neuron-specific enolase. Stroke; a Journal of Cerebral Circulation, 30, 1598–1603.
Scollo-Lavizzari, G., & Bassetti, C. (1987). Prognostic value of EEG in post-anoxic coma after cardiac arrest. European Neurology, 26, 161–170.
Seder, D. B., Sunde, K., Rubertsson, S., Mooney, M., Stammet, P., Riker, R. R., … International Cardiac Arrest Registry. (2015). Neurologic outcomes and postresuscitation care of patients with myoclonus following cardiac arrest. Critical Care Medicine, 43(5), 965–972. https://doi.org/10.1097/CCM.0000000000000880.
Sedgwick, M. L., Dalzeil, K., Watson, J., Carrington, D. J., & Cobbe, S. M. (1993). Performance of an established system of first responder out-of-hospital defibrillation. The results of the second year of the Heartstart Scotland project in the ‘Utstein style’. Resuscitation, 26, 75–88.
Shekhar, S., Kumar, R., Rai, N., Kumar, V., Singh, K., Upadhyay, A. D., … Dey, S. (2016). Estimation of tau and phosphorylated tau181 in serum of Alzheimer’s disease and mild cognitive impairment patients. PLoS One, 11(7), e0159099. https://doi.org/10.1371/journal.pone.0159099
Silver, J. R., & Buxton, P. H. (1974). Spinal stroke. Brain: A Journal of Neurology, 97, 539–550.
Smith, K., Andrew, E., Lijovic, M., Nehme, Z., & Bernard, S. (2015). Quality of life and functional outcomes 12 months after out-of-hospital cardiac arrest. Circulation, 131(2), 174–181. https://doi.org/10.1161/CIRCULATIONAHA.114.011200
Snyder, B. D., Loewenson, R. B., Gumnit, R. J., Hauser, W. A., Leppik, I. E., & Ramirez-Lassepas, M. (1980). Neurologic prognosis after cardiopulmonary arrest: II. Level of consciousness. Neurology, 30, 52–58.
Solari, D., Rossetti, A. O., Carteron, L., Miroz, J. P., Novy, J., Eckert, P., & Oddo, M. (2017). Early prediction of coma recovery after cardiac arrest with blinded pupillometry. Annals of Neurology, 81(6), 804–810. https://doi.org/10.1002/ana.24943
Speach, D. P., Wong, T. M., Cattarin, J. A., & Livecchi, M. A. (1998). Hypoxic brain injury with motor apraxia following an anaphylactic reaction to hymenoptera venom. Brain Injury, 12, 239–244.
Sunnerhagen, K. S., Johansson, O., & Herlitz, J. (1996). Life after cardiac arrest; a retrospective study. Resuscitation, 31(2), 135–140.
The Hypothermia after Cardiac Arrest Study Group. (2002). Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. The New England Journal of Medicine, 346, 549–556.
Tiainen, M., Kovala, T. T., Takkunen, O. S., & Roine, R. O. (2005). Somatosensory and brainstem auditory evoked potentials in cardiac arrest patients treated with hypothermia. Critical Care Medicine, 33(8), 1736–1740.
Tiainen, M., Roine, R. O., Pettilä, V., & Takkunen, O. (2003). Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke; A Journal of Cerebral Circulation, 34(12), 2881–2886. https://doi.org/10.1161/01.STR.0000103320.90706.35
Volpe, B. T., & Hirst, W. (1983). The characterization of an amnesic syndrome following hypoxic ischemic injury. Archives of Neurology, 40, 436–440.
Volpe, B. T., Holtzman, J. D., & Hirst, W. (1986). Further characterization of patients with amnesia after cardiac arrest: Preserved recognition memory. Neurology, 36, 408–411.
Vukmir, R. B., & Katz, L. (2006). Sodium bicarbonate improves outcome in prolonged prehospital cardiac arrest. The American Journal of Emergency Medicine, 24(2), 156–161.
Waalewijn, R. A., de Vos, R., & Koster, R. W. (1988). Out-of-hospital cardiac arrests in Amsterdam and its surrounding areas: Results from the Amsterdam resuscitation study (ARREST) in Utstein style. Resuscitation, 38, 157–167.
Wijdicks, E. F., Parisi, J. E., & Sharbrough, F. W. (1994). Prognostic value of myoclonus status in comatose survivors of cardiac arrest. Annals of Neurology, 35(2), 239–243.
Wijdicks, E. F. M. (2006). Practice parameter: Prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): Report of the quality standards subcommittee of the American Academy of Neurology. Neurology, 67(2), 203–210. https://doi.org/10.1212/01.wnl.0000227183.21314.cd
Wijdicks, E. F. M., Campeau, N. G., & Miller, G. M. (2001). MR imaging in comatose survivors of cardiac arrest. American Journal of Neuroradiology, 22, 1561–1565.
Wijman, C. A. C., Mlynash, M., Finley Caulfield, A., Hsia, A. W., Eyngorn, I., Bammer, R., … Moseley, M. (2009). Prognostic value of brain diffusion-weighted imaging after cardiac arrest. Annals of Neurology, 65(4), 394–402. https://doi.org/10.1002/ana.21632
Wilson, B. A. (1996). Cognitive functioning of adult survivors of cerebral hypoxia. Brain Injury, 10, 863–874.
Wong, M. K., Morrison, L. J., Qiu, F., Austin, P. C., Cheskes, S., Dorian, P., … Ko, D. T. (2014). Trends in short- and long-term survival among out-of-hospital cardiac arrest patients alive at hospital arrival. Circulation, 130(21), 1883–1890. https://doi.org/10.1161/CIRCULATIONAHA.114.010633
Wu, O., Batista, L. M., Lima, F. O., Vangel, M. G., Furie, K. L., & Greer, D. M. (2011). Predicting clinical outcome in comatose cardiac arrest patients using early noncontrast computed tomography. Stroke; a Journal of Cerebral Circulation, 42(4), 985–992. https://doi.org/10.1161/STROKEAHA.110.594879
Wu, O., Sorensen, A. G., Benner, T., Singhal, A. B., Furie, K. L., & Greer, D. M. (2009). Comatose patients with cardiac arrest: Predicting clinical outcome with diffusion-weighted MR imaging. Radiology, 252(1), 173–181. https://doi.org/10.1148/radiol.2521081232
Yarnell, P. Y. (1976). Neurological outcome of prolonged coma survivors of out-of-hospital cardiac arrest. Stroke; A Journal of Cerebral Circulation, 1976, 279–282.
Young, G. B., Doig, G., & Ragazzoni, A. (2005). Anoxic-ischemic encephalopathy: Clinical and electrophysiological associations with outcome. Neurocritical Care, 2(2), 159–164.
Zandbergen, E. G., de Haan, R. J., Stoutenbeek, C. P., Koelman, J. H., & Hijdra, A. (1998). Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet (London, England), 352(9143), 1808–1812. https://doi.org/10.1016/S0140-6736(98)04076-8
Zandbergen, E. G., Hijdra, A., Koelman, J. H., Hart, A. A., Vos, P. E., Verbeek, M. M., & de Haan, R. J. (2006). Prediction of poor outcome within the first 3 days of postanoxic coma. Neurology, 66(1), 62–68.
Zeiner, A., Holzer, M., Sterz, F., Schörkhuber, W., Eisenburger, P., Havel, C., … Laggner, A. N. (2001). Hyperthermia after cardiac arrest is associated with an unfavorable neurologic outcome. Archives of Internal Medicine, 161(16), 2007–2012.
Zheng, Z. J., Croft, J. B., Giles, W. H., & Mensah, G. A. (2001). Sudden cardiac death in the United States, 1989 to 1998. Circulation, 104(18), 2158–2163.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lim, C., Alexander, M. (2020). Cardiac Arrest. In: Lazar, R., Pavol, M., Browndyke, J. (eds) Neurovascular Neuropsychology. Springer, Cham. https://doi.org/10.1007/978-3-030-49586-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-49586-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-49585-5
Online ISBN: 978-3-030-49586-2
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)