Abstract
Dynamic arterial elastance (Eadyn) is the reapplication of effective arterial elastance into a practical bedside derivative useful for assessing blood pressure response to various interventions. Typically, the complex interaction of ventricular and arterial systems requires the use of invasive and technically difficult monitors. Now, with the advent of Eadyn the dynamics of arterial load become available with minimally invasive monitors. Furthermore, the introduction of Eadyn into current algorithms for perioperative and critical care fluid management has been shown valid and impactful on clinical outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Dynamic arterial elastance
- Perioperative fluid management
- Ventriculo-arterial coupling
- Arterial elastance
- Excess pressure
- Arterial tone
- Dynamic systemic vascular resistance
- Dynamic
- Arterial waveform
- Impedance
- Norepinephrine
- Mean arterial pressure
- Fluid responsiveness
- Pressure responsiveness
- Anesthesia
- Critical care
-
1.
Stroke volume variation and pulse pressure variation predict cardiac output responsiveness to intravenous fluid administration, not mean arterial pressure responsiveness.
-
2.
The ratio of pulse pressure variation to stroke volume variation predicts mean arterial pressure responsiveness to intravenous fluid administration and norepinephrine titration.
-
3.
The use of Dynamic Arterial Elastance decreases length of time in the cardiothoracic intensive care unit when employed as part of post-operative management.
-
4.
The generalizability of the clinical utility of Dynamic Arterial Elastance is modest and further study is still needed.
Introduction
Blood pressure is the potential energy needed to overcome resistive forces in capillary beds and achieve blood flow through tissues. This flow delivers the necessary substrate for energy production, allows immune surveillance, and transfers various ligands and waste products in order to maintain homeostasis. Insufficient flow risks cellular disruption and tissue dysfunction manifesting as pathologic states such as kidney injury, heart failure, liver failure, poor wound healing, and infection. This crucial link between blood pressure and flow emphasizes the need to balance flow with an adequate mean arterial pressure, especially in the operating room and critical care settings.
Interventions employed to achieve a favorable hemodynamic balance are not without risk and prediction of their utility is of great importance to the anesthesiologist. The historic trend has been empiric fluid administration as the mainstay of managing hypotension, but this trend has shifted. It is now recognized that excessive intravascular fluid administration can be detrimental for patients [1]. The use of excessive vasopressor is also problematic. While there are numerous predictive methods of determining the cardiovascular responsiveness to various interventions, the most accurate lack the efficacy for widespread use. Thus, the search for non-invasive, user-friendly methods has progressed.
Two commonly employed methods are stroke volume variation and pulse pressure variation. While useful, these modalities predict increases in cardiac output (CO), not MAP, offering an incomplete assessment of the arterial system [2, 3]. Interestingly, by simply comparing pulse pressure variation (PPV) to stroke volume variation (SVV) a more complete hemodynamic picture emerges. Coined “Dynamic Arterial Elastance,” PPV/SVV can predict MAP responsiveness to fluid administration and norepinephrine titration with promising accuracy [4,5,6,7,8,9].
This chapter explores the physiology of dynamic arterial elastance (Eadyn) in terms of the influence of arterial system characteristics on arterial waveforms. Subsequently, the chapter examines the clinical evidence followed by a proposed method for implementing dynamic arterial elastance (Eadyn) into clinical practice.
Arterial Waveforms and the Arterial Tree
Pulse pressure is the transformation of stroke volume to a pressure wave in accordance with arterial system properties. Likewise, the variation of pulse pressure as stroke volume varies is a result of arterial system properties. These primary arterial system properties are effective arterial elastance (Ea) and impedance (Z). Essentially, the degree to which PPV couples with SVV depicts the relative states of effective arterial elastance (Ea) and impedance (Z).
Effective arterial elastance and impedance are the dynamic equivalents of systemic vascular resistance. The static approach, where CO = MAP/SVR, assumes a quasi-steady hemodynamic state, smoothing over the pulsatile nature of the cardiovascular system. Amongst other things, this results in a false depiction of SVR as the sole proportioning factor for the transformation of energy between pressure and flow. This results in an over appreciation of vessel radius in determining pressure and flow dynamics, ignoring arterial tone. By embracing the pulsatility of the cardiovascular system arterial tone becomes a codominant factor. In fact, arterial tone and vessel radius are major elements of both effective arterial elastance (Ea) and impedance (Z).
Effective arterial elastance (Ea) describes the pressure wave of a stroke volume as the result of arterial tone and peripheral vascular resistance in accordance with the 2-element Windkessel model of arterial waveforms. For clarification, elastance is synonymous with tone, and is an intrinsic property of the arterial walls. Its measure is the rate of pressure rise as volume is introduced into an elastic structure. Depicted physiologically, the large central arteries stretch and temporarily store a volumetric portion of a stroke volume. These vessels resist this stretch and attempt to return to their original size, causing a rise in pressure upon systole with subsequent steady decline in pressure as blood discharges to the periphery during diastole. Due to the finite ability of arterial vessels to stretch an increase in total arterial volume results in an exponential increase in rate of pressure rise (See Fig. 5.1). Because PVR controls outflow from the large elastic capacitance vessels it also controls their total volume at a given heart rate and thus effective arterial elastance. The incorporation of PVR into arterial elastance is the distinction between arterial elastance as an intrinsic property and effective arterial elastance as an in vivo property. Effective arterial elastance (Ea) is the result of arterial tone (AKA elastance) and peripheral vascular resistance [10,11,12,13]
Vascular Compliance curve (Top) and its inverse, Elastance (bottom). The elastance curve may be altered at baseline, for example in atherosclerosis. Elastance also varies by vascular bed and arterial tone. The dashed line depicts the change in the pressure volume relationships for compliance and elastance
.
The 2-element Windkessel model uses Ea to accurately predict end systolic pressure and diastolic pressure, but is inaccurate in predicting peak systolic pressure [10] (see Fig. 5.2). The difference between peak systolic pressure and end systolic pressure in the aorta is relatively minor. However, as the pressure wave traverses the arterial system end systolic pressure and peak systolic pressure vary quite drastically [12]. The phenomenon is known as distal pulse pressure amplification and can be attributed to excess pressure (Pex) [14, 15]
Excess Pressure waveform represented by the Joukowsky equation plus the 2-element Windkessel. The summation illustrates their gross contributions to the arterial waveform. The peak of the pressure volume graph is end systolic pressure, whereas the peak of the arterial waveform summation graph is the systolic pressure
.
Excess pressure (Pex) is the result of reverberation or pressure wave reflection perpendicular to flow beginning and ending in systole. This pressure wave adds to the pressure-volume wave predicted by the 2-element Windkessel in early systole and its effects are negligible by end systole. Excess pressure (Pex) explains the discrepancy between peak systolic pressure and end systolic pressure [15].
The Joukowsky equation elegantly describes how Pex results in peak systolic pressures greater than end systolic pressures. The equation is: dP = QZ, where Q = wave speed, Z = impedance and dP approximates excess pressure (Pex) [16]. Wave speed (Q) is determined by ventricular contractility and arterial elastance. Impedance (Z) is proportional to elastance and SVR. This is all to show Pex increases as elastance, SVR, and contractility increase [16, 17]. As suggested, the phenomenon of distal pulse pressure amplification illustrates the role of excess pressure in stroke volume to pulse pressure transformation and serves as an important example of its role in Eadyn.
Impedance (Z) increases from the proximal to distal arterial tree because of a change in intrinsic properties of the arterial walls and total caliber of vessel lumen. The main intrinsic property resulting in increased impedance is the increased smooth muscle to elastin ratio in peripheral arteries resulting in increased elastance or intrinsic tone. In addition, the typical taper of total vessel radius near the periphery results in increased SVR. Together the changing arterial properties as the pressure wave traverses the arterial system results in an increase in Pex and thus distal pulse pressure amplifications [15]. The concept is quite obvious when observing arterial waveform tracings at proximal sites versus more distal sites.
Altogether, PPV/SVV describes the relative state of Ea and Z as described by Pex and the 2-element Windkessel. Arterial tone, peripheral vascular resistance, impedance, and LV contractility determine the rate of left ventricular energy dissipated to arterial walls via perpendicular wave reflections (Pex) and vessel wall recoil (Windkessel). The fact that theoretical and experimental data predict a PPV/SVV around 0.8 as the threshold value at which a patient is not likely to respond to a fluid bolus is proof of concept. Furthermore, studies validating PPV/SVV find its predictive capabilities to be independent of SVR. Thus, PPV/SVV offers an assessment of dynamic arterial characteristics beyond the ability of static hemodynamic models.
Combining Joukowsky and Windkessel
Data and Utility
Clinically, the elegance of PPV/SVV is the ability to assess complex hemodynamic characteristics with minimally invasive to potentially non-invasive monitors. Because PPV/SVV is a ratio of change absolute values are not necessary. More specifically, PPV and SVV are derivatives of the Frank Starling curve and PPV/SVV is the derivative of Z and/or Ea curves. This means, theoretically at least, any measure of SVV and PPV would suffice as long as these methods can track change with reasonable accuracy.
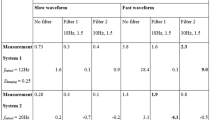
Monge et al., one of the first groups to assess the validity of Eadyn, used two separate methods of measurement in the intensive care unit (ICU). Both study patient populations were mechanically ventilated, preload dependent (by SVV or PPV), without evidence of cardiac pathology. Over half of the patients were septic. Interestingly, there was no difference in hypotensive and normotensive patients in the ability of Eadyn to predict MAP response of >10% after a 500 mL bolus of NS (Fig. 5.3). Also, over half of the patients received norepinephrine or dopamine infusions, which were not titrated during the study. Moreover, MAP response continued with repeat boluses until subsequent measure of PPV/SVV decreased. The end result of the two validation studies: PPV/SVV of 0.73 (grey zone 0.72–0.88) predicted MAP increase >10% with a 500 cc bolus of NS with a sensitivity of 90.9% and a specificity of 91.5% [6].
The first validation study by Monge et al. was challenged on the possibility of “mathematical coupling.” In this study, the FloTrac/Vigileo platform was used to measure both PPV and SVV from radial arterial line tracings. Because the Vigileo uses waveform characteristics to modify its assessment of stroke volume it was thought the use of the same waveform tracing for both PPV and SVV would erroneously couple the two, invalidating the results of the study [18]. In response, the follow-up study used an esophageal Doppler for SVV and radial arterial waveforms for PPV. The studies had similar results [5, 6].
As with the utilization of different platforms for tracking PPV/SVV, cautious interpretation and implementation is warranted for different patient populations. The Ea value is different in patients with and without hypertensive disease [19]. Pertinent to anesthesia and critical care, a study in cirrhotic patients undergoing liver transplantation did not show Eadyn to be predictive of MAP response to fluid bolus [20]. Furthermore, Eadyn was not predictive of pressure response to fluid administration in a study of which >50% of participants were undergoing vascular procedures secondary to atherosclerosis [21]. On a positive note, Eadyn has been validated in patients undergoing robot assisted laparoscopic prostatectomies [9].
An area of increasing investigation is the use of PPV/SVV to predict MAP responsiveness for the titration of norepinephrine (NE). The end point of three studies showed PPV/SVV to be useful for predicting which patients would have a MAP decrease >10% with an unspecified decrease in NE [4, 7, 8]. Most importantly, one study showed decreased time of NE infusion and time in the ICU when using Eadyn as part of an algorithm for weaning NE [7]. The cutoff values for predicting MAP decrease with NE decrease are ~0.85–0.90 with a near 100% sensitivity and ~ 70% specificity [4, 7, 8].
As a caveat, the physiology of PPV and SVV coupling has brought with it the debate as to whether or not it is a measure of ventriculo-arterial coupling. Nomenclature aside, based on its physiology, its importance as a measure of arterial system characteristics likely requires normal cardiac and autonomic function [14, 19, 22,23,24]. Patients with normal cardiac reserve and effective baroreceptor responses will respond harmoniously with changes in arterial load. Whereas patients with alteration in cardiac function, whether it be acute, chronic, and/or pharmacologically induced, the threshold value for prediction may be altered [19, 22,23,24].
While there is no substitute for clinical judgment, the ratio of PPV/SVV is another tool to help predict hemodynamic status. It is different, although representative of SVR as a dynamic arterial load on stroke volume. Data are limited and suggest unique considerations in certain patient populations warranting further studies before use in these groups (i.e. atherosclerosis, cirrhosis, cardiac dysfunction). Furthermore, different methods of measurement and algorithms may alter validity and optimal predictive values. An understanding of the physiology will help the clinician interpret Eadyn in a given clinical scenario. Currently, only general recommendations for the clinical implementation of Eadyn can be provided.
Eadyn should be used in patients who are expected to or are actively suffering from hypotension to determine the role of vasopressors and/or fluid administration. Cardiac variables should be considered if Eadyn is below threshold and a patient is not fluid responsive by PPV or SVV.
Recommendations can be made in the setting of hypotension or anticipated hypotension for patients not receiving pharmacologic hemodynamic support. Vasopressors and/or inotropes should be administered prior to or in lieu of giving a fluid bolus to patients who are below the pressure responsiveness threshold. Fluids should be administered if Eadyn is predictive of a pressure response to a fluid bolus and Eadyn reassessed. If Eadyn remains above threshold after a fluid bolus the patient may warrant an additional bolus of fluid. If Eadyn decreases below threshold after a fluid bolus the patient is likely no longer pressure responsive to fluids, and therefore vasopressors or inotropes should be considered if hypotension persists.
Patients receiving norepinephrine infusion with Eadyn below threshold should continue norepinephrine with further investigation into the etiology for vasoplegia. Norepinephrine should be decreased if Eadyn is above a threshold, though the decrement has yet to be empirically determined. The use of Eadyn for the titration of norepinephrine is the only clinically positive outcome associated with Eadyn [7].
A challenging area of Eadyn interpretation is the scenario of preload dependence by SVV or PPV with an Eadyn below threshold. Pharmacologic support should be given but administration of a fluid bolus is unclear. There are two potential paths as Eadyn reaches threshold following vasopressor administration: 1. either the patient remains hypotensive, or 2. the MAP goal is achieved. If Eadyn reaches threshold while titrating pharmacologic support, yet the patient remains hypotensive a fluid bolus should be given. In the patient who achieves MAP goals after pharmacologic support the clinician should question whether or not flow is being sacrificed for pressure. A fluid bolus should be considered when Eadyn is above threshold in a preload responsive patient receiving vasopressor/inotropic support in an attempt to wean pharmacologic support. Aside from norepinephrine, there are currently no studies examining the effect of vasopressors/inotropes on Eadyn. Therefore, the validity of Eadyn and/or its threshold value may be altered when interpreting in the setting of vasopressors/inotropes other than norepinephrine.
The many caveats to the day-to-day use of Eadyn warrant a reminder of the physiology of Eadyn. Its role in hemodynamic assessment is as an indicator of dynamic systemic vascular resistance. As with all clinical tools an understanding of its physiology should guide its bedside implementation.
Conclusion
Eadyn adds a unique tool to the clinician’s armamentarium for the assessment of hemodynamic status. The pulse pressure varies according to stroke volume variation as the result of Z and Ea. Studies validating Eadyn are promising in predicting pressure responsiveness to fluid bolus and norepinephrine titration. The use of Eadyn for decreasing norepinephrine use is associated with a decreased length of ICU stay and should be considered for this purpose. Further studies on outcomes in various populations need to be conducted. There may be a role for Eadyn in Enhanced Recovery After Surgery protocols with cautious interpretation based upon patient characteristics and clinical circumstances. Clinicians should start tracking Eadyn in practice to further assess the validity and outcomes associated with its use.
References
Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth [Internet]. 2002 Oct 1 [cited 2019 Mar 9];89(4):622–32. Available from http://linkinghub.elsevier.com/retrieve/pii/S0007091217370666.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: A systematic review of the literature*. Crit Care Med [Internet]. 2009 Sep [cited 2019 Mar 9];37(9):2642–7. Available from http://www.ncbi.nlm.nih.gov/pubmed/19602972.
Zhang Z, Lu B, Sheng X, Jin N. Accuracy of stroke volume variation in predicting fluid responsiveness: a systematic review and meta-analysis. J Anesth [Internet]. 2011 Dec 4 [cited 2019 Mar 9];25(6):904–16. https://doi.org/10.1007/s00540-011-1217-1
Bar S, Leviel F, Abou Arab O, Badoux L, Mahjoub Y, Dupont H, et al. Dynamic arterial elastance measured by uncalibrated pulse contour analysis predicts arterial-pressure response to a decrease in norepinephrine. Br J Anaesth [Internet]. 2018 Sep [cited 2019 Apr 20];121(3):534–40. Available from https://linkinghub.elsevier.com/retrieve/pii/S0007091218300941.
García MIM, Romero MG, Cano AG, Aya HD, Rhodes A, Grounds RM, et al. Dynamic arterial elastance as a predictor of arterial pressure response to fluid administration: a validation study. Crit Care [Internet]. 2014 Dec 19 [cited 2019 Mar 9];18(6):626. Available from http://www.ncbi.nlm.nih.gov/pubmed/25407570.
Monge García MI, Guijo González P, Gracia Romero M, Gil Cano A, Rhodes A, Grounds RM, et al. Effects of arterial load variations on dynamic arterial elastance: An experimental study. Br J Anaesth [Internet]. 2017 Jun 1 [cited 2019 Feb 1];118(6):938–46. Available from https://linkinghub.elsevier.com/retrieve/pii/S0007091217300600.
Guinot P-G, Abou-Arab O, Guilbart M, Bar S, Zogheib E, Daher M, et al. Monitoring dynamic arterial elastance as a means of decreasing the duration of norepinephrine treatment in vasoplegic syndrome following cardiac surgery: a prospective, randomized trial. Intensive Care Med [Internet]. 2017 May 24 [cited 2019 Apr 26];43(5):643–51. Available from http://www.ncbi.nlm.nih.gov/pubmed/28120005.
Guinot P-G, Bernard E, Levrard M, Dupont H, Lorne E. Dynamic arterial elastance predicts mean arterial pressure decrease associated with decreasing norepinephrine dosage in septic shock. Crit Care [Internet]. 2015 Jan 19 [cited 2019 Apr 27];19(1):14. Available from http://www.ncbi.nlm.nih.gov/pubmed/25598221.
Seo H, Kong Y-G, Jin S-J, Chin J-H, Kim H-Y, Lee Y-K, et al. Dynamic arterial elastance in predicting arterial pressure increase after fluid challenge during robot-assisted laparoscopic prostatectomy. Medicine (Baltimore) [Internet]. 2015 Oct [cited 2019 Mar 9];94(41):e1794. Available from http://www.ncbi.nlm.nih.gov/pubmed/26469925.
Westerhof N, Lankhaar J-W, Westerhof BE. The arterial Windkessel. Med Biol Eng Comput [Internet]. 2009 Feb 10 [cited 2019 May 30];47(2):131–41. Available from https://doi.org/10.1007/s11517-008-0359-2
Stergiopulos N, Meister JJ, Westerhof N. Determinants of stroke volume and systolic and diastolic aortic pressure. Am J Physiol [Internet]. 1996;270(6 Pt 2):H2050-9. Available from http://www.ncbi.nlm.nih.gov/pubmed/8764256.
Stergiopulos N, Westerhof BE, Westerhof N. Total arterial inertance as the fourth element of the windkessel model. Am J Physiol Circ Physiol. 2017;276(1):H81–8.
Wang J-J, O’Brien AB, Shrive NG, Parker KH, Tyberg JV. Time-domain representation of ventricular-arterial coupling as a windkessel and wave system. Am J Physiol Circ Physiol [Internet]. 2003 Apr [cited 2019 Mar 17];284(4):H1358–68. Available from http://www.physiology.org/doi/10.1152/ajpheart.00175.2002.
Gaddum N, Alastruey J, Chowienczyk P, Rutten MCM, Segers P, Schaeffter T. Relative contributions from the ventricle and arterial tree to arterial pressure and its amplification: an experimental study. Am J Physiol Heart Circ Physiol [Internet]. 2017 Sep 1 [cited 2019 May 30];313(3):H558–67. Available from http://www.ncbi.nlm.nih.gov/pubmed/28576835.
Narayan O, Parker KH, Davies JE, Hughes AD, Meredith IT, Cameron JD. Reservoir pressure analysis of aortic blood pressure: an in-vivo study at five locations in humans. J Hypertens [Internet]. 2017 [cited 2019 May 1];35(10):2025–33. Available from http://www.ncbi.nlm.nih.gov/pubmed/28582283.
Tijsseling AS, Anderson A. The Joukowsky equation for fluids and solids [Internet]. 2006 [cited 2019 May 1]. Available from http://www.win.tue.nl/analysis/reports/rana06-08.pdf
Nourbakhsh SA, Jaumotte BA, Hirsch C, Parizi HB. Water Hammer. In: Turbopumps and pumping systems. Heidelberg: Springer; 2007. p. 122–42. https://doi.org/10.1007/978-3-540-68214-1_9.
Jozwiak M, Monnet X, Teboul J-L, Monge García MI, Pinsky MR, Cecconi M. The dynamic arterial elastance: a call for a cautious interpretation. Intensive Care Med [Internet]. 2017 Sep 11 [cited 2019 Apr 26];43(9):1438–9. Available from http://springerlink.bibliotecabuap.elogim.com/10.1007/s00134-017-4836-7.
Borlaug BA, Lam CSP, Roger VL, Rodeheffer RJ, Redfield MM. Contractility and ventricular systolic stiffening in hypertensive heart disease. J Am Coll Cardiol [Internet]. 2009 Jul 28 [cited 2019 May 31];54(5):410–8. Available from http://www.ncbi.nlm.nih.gov/pubmed/19628115.
Wu C-Y, Cheng Y-J, Liu Y-J, Wu T-T, Chien C-T, Chan K-C, et al. Predicting stroke volume and arterial pressure fluid responsiveness in liver cirrhosis patients using dynamic preload variables. Eur J Anaesthesiol [Internet]. 2016 Sep [cited 2019 May 6];33(9):645–52. Available from http://www.ncbi.nlm.nih.gov/pubmed/27167058.
Lanchon R, Nouette-Gaulain K, Stecken L, Sesay M, Lefrant JY, Biais M. Dynamic arterial elastance obtained using arterial signal does not predict an increase in arterial pressure after a volume expansion in the operating room. Anaesth Crit Care Pain Med [Internet]. 2017 Dec 1 [cited 2019 Mar 20];36(6):377–82. Available from https://www.sciencedirect.com/science/article/abs/pii/S2352556816301370?via%3Dihub.
Chirinos JA. Ventricular-arterial coupling: Invasive and non-invasive assessment. Artery Res [Internet]. 2013 Mar [cited 2019 May 6];7(1). Available from http://www.ncbi.nlm.nih.gov/pubmed/24179554.
Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA. Coupled systolic-ventricular and vascular stiffening with age: implications for pressure regulation and cardiac reserve in the elderly. J Am Coll Cardiol [Internet]. 1998 Nov [cited 2019 May 31];32(5):1221–7. Available from http://www.ncbi.nlm.nih.gov/pubmed/9809929.
Borlaug BA, Kass DA. Ventricular-vascular interaction in heart failure. Cardiol Clin. 2011;29:447–59.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ramirez, P., Troianos, C., Farag, E., Tovar-Camargo, O. (2020). Dynamic Arterial Elastance: Physiology, Data and Implementation. In: Farag, E., Kurz, A., Troianos, C. (eds) Perioperative Fluid Management. Springer, Cham. https://doi.org/10.1007/978-3-030-48374-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-48374-6_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-48373-9
Online ISBN: 978-3-030-48374-6
eBook Packages: MedicineMedicine (R0)