Abstract
Bilateral phrenic nerve paralysis leading to diaphragm paralysis causes significant pulmonary morbidity in patients. Diaphragm pacing (DP) was developed to overcome this problem and provide natural negative pressure ventilation. In spinal cord injured patients dependent on mechanical ventilation, there is strong evidence in the literature to support the use of DP to wean these patients off of mechanical ventilation. Recent evidence supports early implantation which can improve results, decrease intensive care unit time, decrease the morbidity of ventilator associated pneumonias, and decrease early mortality.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Bilateral phrenic nerve paralysis leads to bilateral diaphragm paralysis and significant patient symptoms. In compromised patients this may require continuous positive pressure assistance or even tracheostomy and mechanical ventilation (MV). The most common cause of bilateral diaphragm paralysis is cervical spinal cord injury (SCI). In these patients there is no longer a connection between the respiratory control system in the brainstem or volitional control of breathing area in the cerebral cortex with the phrenic motor neurons in the cervical spinal cord. In the cervical SCI population, 50% of patients are discharged on temporary MV. SCI coupled with MV is a catastrophic life changing event that drastically decreases life expectancy along with increasing yearly costs of care by $185,000. For example, a MV dependent 20 year old SCI patient would be expected to live only 10.6 years compared to 34 years for a similarly injured patient not ventilated. The greatest reason for reduced life expectancy is pneumonia [1].
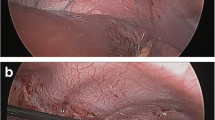
Independent breathing is compromised in SCI patients due to disruption of the signaling pathway, the spinal cord, from the respiratory center in the brain to the diaphragm. In patients with an intact phrenic nerve, the signaling pathway can be bypassed by implanting permanent electrodes to provide direct electrical stimulation to the diaphragm, which is the mechanism of action of diaphragm pacing (DP) (NeuRx DPS, Synapse Biomedical, Oberlin, Ohio). The DP system is implanted via a laparoscopic surgical procedure by placing electrodes into each hemidiaphragm near the phrenic nerve motor point. Each electrode percutaneously exits the body and is connected to a four-channel external stimulator. The laparoscopic surgical technique has been well described [2, 3]. In ventilator-dependent SCI patients, DP effectively functions initially as a powered muscle stimulator for treating disuse atrophy and then, once the diaphragm has been sufficiently reconditioned, as a functional electrical stimulator (or breathing pacemaker) to drive respiration and weaning from mechanical ventilation.
Bilateral diaphragm paralysis from SCI is a rare event in the United States with less than 1000 cases annually. Each trauma unit in the US may only see several cases a year, so additional knowledge and skill will be required to change the standard of care for these patients. The DP device is indicated for stable SCI patients with diaphragms that can be stimulated to contract, but who lack control of their diaphragms. If a patient has complete transection of the phrenic nerves or damage to cervical motor neurons, DP would not be indicated unless phrenic nerve reconstruction would to be done, which is addressed in another chapter. In this chapter the present literature on DP results will be reviewed to help overcome the scarcity of experience and improve management of SCI patients with bilateral phrenic nerve paralysis.
Search Strategy
A search of PubMed with the search criteria (diaphragm OR diaphragmatic) AND (pacer OR pacing OR pacemaker) AND (“spinal cord injury” OR SCI) was completed. Studies from 2014 through 2019 were than manually identified from these search parameters, such that the data included subjects with high-level spinal cord injury concordant with the indication for device use. The Kerwin, Onders, and Posluszny reports were identified in this fashion [4,5,6]. The summary of the Lammertse study was obtained from the authors after the presentation of the abstract at a conference and will be included [7]. A systematic review article by Garara et al. which covered multiple early published studies that consisted of 12 articles from 2006 to 2014 will also be discussed [8]. The initial clinical study data that supported the initial FDA approval will also be presented for historical purposes [9]. The main goal of the intervention of DP is replacement of invasive mechanical ventilation which is summarized in Table 42.1 using the PICO format.
Results
In 2018, Kerwin et al. reported their single center retrospective matched cohort analysis evaluating early use of DP on in-hospital outcomes of patients with acute cervical SCI [4]. The matched cohorts included 40 patients who received DP implants under FDA approved use and 61 matched patients without a DP implant. There were minor demographic differences between the groups in that the DP patients were significantly older (45 ± 16 vs. 39 ± 16 years; p = 0.05) and more likely to be female (28% vs. 11%; p = 0.04). However, there were no differences in the injury severity score or the level of spinal injury. Mean time to implantation was 14 days. Median time to MV liberation after DP implantation was 7 days. Twenty-six DP patients (65%) and 39 patients (64%) in the control group were diagnosed with ventilator-associated pneumonia (VAP) (p = 0.91). The DP patients that developed VAP had significantly fewer vent days as compared to the control patients (24.5 ± 15.2 days vs. 33.2 ± 23.3 days; p = 0.05). Mortality was 15% for the control group compared to 3% for the DP group (p = 0.04). Length of hospital stay was significantly shorter in the DP group: 65 ± 61 vs. 43 ± 24 days for the control and DP groups, respectively (p = 0.03). In this large single institution series of DP implantation for acute cervical SCI, the researchers found that DP implantation was safe and feasible for patients with acute cervical SCI, and that for patients who developed VAP, mean ventilator days were significantly shorter.
Kerwin’s group further expanded on the improvement of respiratory mechanics of diaphragm pacing at the Annual meeting of the American Association for the Surgery of Trauma (AAST) in September of 2019 with a presentation and published abstract [10]. They report on 37 patients with DP and 34 matched patients without DP. DP lead to a statistically increase in spontaneous tidal volume compared to no DP (+88 mL vs. −13 mL; 95% CI 46–131 vs. −78 to 58 mL respectively; p = 0.004). More important was that the median time to ventilator liberation after DP was significantly shorter (10 days vs. 29 days; 95% CI 6.5–13.6 vs. 23.1–35.3 days; p < 0.001). They concluded that: “Comprehensive care of acute cervical spinal cord injury patients should include DP implantation”.
In 2018, Onders et al. reported on the largest long term results in traumatic SCI. From 2000 to 2017, 92 patients underwent laparoscopic diaphragm mapping and implantation of DP for diaphragm strengthening and ventilator weaning. The age at time of injury ranged from birth to 74 years old (average of 27). Time on MV was an average of 47.5 months (6 days to 25 years with median of 1.58 years). As an indicator of DP success in conditioning the diaphragm in the initial patients implanted [35], the stimulated tidal volume relative to basal requirement (7 cc/kg for males and 5 cc/kg for females) over time of conditioning was examined. Overall, in the first week of DP, there was a gain from 7% below basal requirements to 36% over basal requirements . A total of 88% of patients (81/92) achieved the minimum of 4 h of pacing. Seventy (76%) patients used DP at least 12 h per day. Fifty-six (60.8%) patients used DP 24 h per day. Five (5.4%) patients had full recovery of volitional breathing with subsequent DP removal. Five (5.4%) patients were not successfully weaned from MV. Median survival was 22.2 years (95% CI 14.0—not reached) with only 31 deaths. Subgroup analysis showed a trend that earlier DP implantation leads to a greater number of patients utilizing DP for 24 h with no need for any MV. The investigators concluded that DP can successfully decrease need for MV in traumatic SCI and that earlier implantation should be considered. A secondary benefit was also reported, that after DP, 21 of 44 patients (48%) with a chronically cuffed tracheostomy no longer needed a cuffed tracheostomy. Seven patients were completely decannulated from tracheostomy because of DP and an early implanted patient completely avoided a tracheostomy. The clinical significance is that chronic cuffed tracheostomy tubes increase the risks of hemorrhage, tracheomalacia, infections, mucous production, pneumonias, granulation tissue , and stenosis [5].
In 2016, Lammertse et al. presented results of a multicenter longitudinal follow-up of DP patients [7]. The independent study was conducted by six Spinal Cord Injury Model Systems (SCIMS) centers and funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) . The aim of the study was to determine the long term outcomes of patients with SCI that were using DP. The study used questionnaire-based patient reported outcomes with data collected for the years 2011–2016 on patients with implants performed 2007–2014. Thirty-one patients, 23 male and 8 female, with mean age of 34 years (range 19–71 years) were enrolled at six SCIMS centers. Neurological level of injury was C1 32%, C2 45%, C3 19%, and C4 3%. Thirty percent had complete SCI and 70% had incomplete SCI. Mean time to implant post-SCI was 4.5 years (range < 1 month to 28 years). Mean follow-up was 3.2 years (range 15 days to 7.4 years). Patients (n = 28) initiated pacing a mean of 2.5 days and a median of 1 day (range 0–7 days) post-electrode placement. Patients achieved pacing for 6 h per day after a median of 7 days (range 0–60 days) and 24 h per day after a median of 5 days (range 0–30 days). Twenty-four (24) patients (86%) were still using DPS (4–24 h; mean 16 h, median 16 h) at the time of the follow-up and 7 patients (25%) were pacing 24 h per day. Four [4] patients (14%) were not pacing due to “medical issues”, including an adverse reaction to pacing, shoulder pain, or need for pressure support via the ventilator. Device-related adverse events included infection issues at the electrode wire exit site (17%), pain with pacing (14%), and electrode wire issues involving hospitalization (13%). From a subjective patient satisfaction standpoint, 95% were happy or very happy with their decision to have DP; 79% were satisfied or very satisfied with DP; 57% reported improved ability to engage in activities (e.g., air travel, community mobility, conversation, socialization, energy, sex, etc.), although attendant care needs were unchanged in 89%.
Posluszny’s 2014 report was similar to Kerwin’s in that he focused on early implantation of DP in SCI [6]. Their analysis included 29 patients, 22 of whom were implanted; 7 patients had denervated “dead diaphragms ” at surgery. These diaphragms could not be stimulated because of complete destruction of the lower motor neurons from the trauma insult. The average time frame of injury to implant was 3–112 days with a median of 33 days; 72.7% (16 of 22) were completely free of MV in an average of 10.2 days. A subset of patients implanted within 11 days of injury weaned off MV in 5.7 days. Some patients (36%) implanted early after injury had recovery of respiration and were able to wean off of DP. The ability to record dEMG in this SCI population highlighted the potential of electrical stimulation from DP and neuroplasticity of the spinal cord allowing recovery of phrenic nerve function. Also noteworthy was the fact that early identification of those patients with “dead diaphragms” saves significant amounts of time, frustration, and money on futile ventilator weaning and also allows early consideration of the growing use of nerve transfer techniques to allow recovery.
The initial FDA multi-center clinical trial (N = 50) of DP in SCI dependent on tracheostomy MV showed 96% (48/50) of implanted patients were able to breathe for four consecutive hours with DP alone [9]. This was a single arm prospective evaluation. Outcome measures included stimulated tidal volume, use of DP, patient/caregiver satisfaction, and mortality. Fifty-two percent (26/50) were able to replace MV full time. The subjects achieved the primary endpoint of four hours off of MV in a mean of 2.2 months (range 0.2–7.8 months). Patients ranged in age from 18 years to 74 years (mean 36 years). There were 37 males with the majority of injuries resulting from motor vehicle accidents followed by sports injuries. Patients were on MV from 3 months to 27 years prior to DP implant with the average time of injury to implant being 5.6 years. A 1 year psychosocial survey of the effect of DP was completed in 22 subjects. All patients were living at home. Sixty-four percent reported less secretions with 70% of caregivers reporting less suctioning. Seventy-seven percent reported “more normal breathing”. Ninety percent of caregivers stated that caring for DP was less work than MV. Ninety-five percent of patients described an increase in mobility and 91% reported more freedom and feelings of independence. Ninety-six percent of patients and 100% of caregivers would recommend DP to other SCI patients. The most common adverse event was capnothorax ; carbon dioxide from the abdominal cavity used during laparoscopy tracking into the pleural space for which minimal treatment was required.
Earlier studies of DP were summarized by Garara et al. at the Imperial College Healthcare NHS Trust [8]. After analyzing 12 publications from 2004 to 2014, they concluded that DP was safe and effective. They noted between 40% and 72.7% of patients were completely free of MV after conditioning , excluding case reports. They also recommended earlier implantation since it does not appear to be associated with greater surgical risk and had a higher rate of complete success. They also noted that the most frequent post-operative complication was a capnothorax, which was managed successfully with observation, drainage or aspiration.
When comparing the monthly cost of maintaining a patient at home with a portable ventilator including the cost of long-term equipment replacement/rental, medical, and nursing care, DP is cost effective. Onders et al. described the cost savings of $13,000 monthly for one SCI patient who was successfully weaned off the ventilator to full-time pacing [2].
Pacing allows natural negative pressure ventilation , preferentially aerating the posterior lobes of the lungs and increasing respiratory compliance, and therefore should decrease pneumonia rates in this patient population. Hirshfield et al. analyzed 64 spinal cord patients with chronic respiratory insufficiency in whom 32 were able to receive either a phrenic or diaphragm pacer and 32 who did not [11]. Pacing the diaphragm and allowing negative pressure ventilation decreased respiratory infections from 2 per 100 days to 0 with pacing (p < 0.001).
Another report looked at the quality of life of patients with pacing compared to when they were on the ventilator and all patients would recommend pacing to other potential recipients [12]. They found that pacing improved patients’ ability to go outside of the home and participate in leisure activities and relationships with others. This study also showed a significant improvement in olfaction and taste with the use of pacing.
The first four articles that were discussed in the results will form the basis for the conclusions and are summarized in Table 42.2. The strength of the evidence is also reported for each article along with conflicts and limitations. The GRADE approach for recommendations also relies on the benefits and downsides of the proposed therapy. Kim Anderson has been at the forefront in the SCI community of what research should be done based on the expressed needs of the patients with SCI. She states the need to be removed from MV is so inherently obvious and should be at the forefront of research that it is not even posed as a research question to patients [13]. Given the little risk or downside of DP and the significant benefit of being removed from a ventilator allows the final recommendation for DP to be strong in all four highlighted articles. The simplicity of confirming device effectiveness adds to the high quality of the evidence for DP. These are large well performed observational studies that are not randomized, but the patients act as their own controls. If the device is turned off, the patient cannot ventilate and has to be returned to MV. This direct cause and effect gives us the confidence to state there is high quality evidence of the positive effect of DP in these studies.
Conclusions and Recommendations
In conclusion, after over a decade of being approved by the FDA, DP remains underutilized for SCI patients with bilateral phrenic nerve paralysis dependent on MV. A strong recommendation for all SCI patients dependent on MV is warranted. Many patients will be able to have complete weaning from MV. There is strong evidence that DP should be utilized early with significant positive results for this group of patients. If the diaphragm cannot be stimulated because of phrenic nerve injury or death of phrenic motor neurons, the patient can be assessed for intercostal to phrenic nerve transfer. Also, early knowledge of a non-stimulatable diaphragm is confirmation of the inability to wean from MV; long term ventilator management can be immediately begun, which in SCI patients includes high tidal volume ventilation to prevent atelectasis and pneumonias [14, 15]. Timely assessment and implantation can significantly decrease early morbidity, mortality and length of stay which decreases costs.
Recommendations
-
All spinal cord injured patients on mechanical ventilation should have their diaphragms assessed for diaphragm pacing and possible diaphragm pacemaker implantation (evidence quality moderate; strong recommendation).
-
Diaphragm pacing should be implanted early after spinal cord injury (evidence quality moderate ; strong recommendation).
A Personal View of the Data
As part of the team at Case Western Reserve University and University Hospitals Cleveland Medical Center that developed DP technology, I have been involved in use of this technology for over two decades. Recent reports have highlighted the growing benefit of early utilization of DP to wean SCI patients off of the ventilator. This allows earlier transfer to rehabilitation centers to manage the significant other problems of high level quadriplegia. In our current trauma practice, once the initial injury is stabilized, we document if the patient can volitionally move their diaphragm to initiate ventilation. If they can, then standard weaning occurs. If the patient cannot, we go directly to diagnostic laparoscopy to determine if the diaphragm can be stimulated. If the diaphragm can be stimulated, DP is implanted and rapid weaning without tracheostomy begins. It is extremely rewarding to wean a young SCI patient off of MV without a tracheostomy, allowing them verbal communication with family and to begin the rehabilitation process after a life changing injury.
References
National Spinal Cord Injury Statistical Center. http://www.spinal cord.uab.edu. Accessed 25 Oct 2019.
Onders RP, Ignagni AI, Aiyer H, Mortimer JT. Mapping the phrenic nerve motor point: the key to a successful laparoscopic diaphragm pacing system in the first human series. Surgery. 2004;136:819–26.
Onders RP, Ignagni AI, DiMarco AF, Mortimer JT. The learning curve of investigational surgery: lessons learned from the first series of laparoscopic diaphragm pacing for chronic ventilator dependence. Surg Endosc. 2005;19:633–7.
Kerwin AJ, Yorkgitis BK, Ebler DJ, Madbak FG, Hsu AT, Crandall ML. Use of diaphragm pacing in the management of acute cervical spinal cord injury. J Trauma Acute Care Surg. 2018;85:928–31.
Onders RP, Elmo MJ, Kaplan C, Schilz R, Katirji B, Tinkoff G. Long-term experience with diaphragm pacing for traumatic spinal cord injury: early implantation should be considered. Surgery. 2018;164:705–11.
Posluszny JA, Onders R, Kerwin AJ, Weinstein MS, Stein DM, Knight J, Lottenberg L, Cheatham ML, Khansarinia S, Dayal S, Byers PM. Multicenter review of diaphragm pacing in spinal cord injury: Successful not only in weaning from ventilators but also in bridging to independent respiration. J Trauma Acute Care Surg. 2014;76:303–10.
Lammertse DS, Charlifue S, Berliner J. Longitudinal follow-up of individuals with implanted diaphragm pacing systems—a multi-center study. https://clinicaltrials.gov/ct2/show/NCT01815554 and in Topics in Spinal Cord Injury Rehabilitation 2016; 23 supplement 1:57–58. Accessed 25 Oct 2019.
Garara B, Wood A, Marcus H, Tsang K, Wilson MJ, Khan M. Intramuscular diaphragmatic stimulation for patients with traumatic high cervical injuries and ventilator dependent respiratory failure: a systematic review of safety and effectiveness. Injury. 2016;47:539–44.
FDA: HDE H070003. US Food and Drug Administration. NeuRx DPS™, Diaphragm Pacing System. Summary of Safety and Probable Benefit (SSPB). 2008. Retrieved October 15, 2019 from FDA website: https://www.accessdata.fda.gov/cdrh_docs/pdf7/H070003B.pdf.
Kerwin AJ, Yorkgitis YD, Mull R, Hsu AT, Madbak FG, Ebler DJ, Skarupa DJ, Shiber J, Crandal ML. Diaphragm pacing improves respiratory mechanics in acute spinal cord injury. Presented at the 78th annual meeting of the American Association for the Surgery of Trauma. Published in the online abstract book accessed on October 15th, 2019 from website: http://www.aast.org/AnnualMeeting/PastAbstracts.aspx.
Hirchfield S, Exner G, Luukkaala T, Baer GA. Mechanic ventilation or phrenic nerve stimulation for treatment of spinal cord-induced respiratory insufficiency. Spinal Cord. 2008;46:738–42.
Adler D, Gonzalez-Bermejo J, Duguet A, Demoule A, Le Pimpec-Barthes F, Hurbault A, Morelot-Panzine C, Similowski T. Diaphragm pacing restores olfaction in tetraplegia. Eur Respir J. 2009;34:365–70.
Anderson K. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
Fenton JJ, Warner ML, Lammertse D, Charlifue S, Martinez L, Dannels-McClure A, Kreider S, Pretz C. A comparison of high vs standard tidal volumes in ventilator weaning for individuals with sub-acute spinal cord injuries: a site specific randomized clinical trial. Spinal Cord. 2016;54:234–8.
Consortium for Spinal Cord Medicine. Clinical Practice Guidelines: respiratory management following spinal cord injury: a clinical practice guideline for health care professionals. Paralyzed Veterans Am. 2005;28:259–93.
Conflict of Interest Disclosure
Dr. Raymond Onders, University Hospitals of Cleveland and Case Western Reserve University School of Medicine have intellectual property rights involved with the diaphragm pacing system and equity in Synapse Biomedical who manufactures the device.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Onders, R. (2020). Does Diaphragm Pacing for Bilateral Phrenic Nerve Paralysis Improve Function or Quality of Life?. In: Ferguson, M. (eds) Difficult Decisions in Thoracic Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-030-47404-1_42
Download citation
DOI: https://doi.org/10.1007/978-3-030-47404-1_42
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-47403-4
Online ISBN: 978-3-030-47404-1
eBook Packages: MedicineMedicine (R0)