Abstract
Management of facial trauma is a broad and complex field. Significant, often life-threatening, comorbidities need always be considered when evaluating patients with head and neck trauma. After stabilizing the airway and cardiovascular issues, prudent evaluation involves assessment of soft tissue, orbital region, dentition, facial skeleton, and calvarium. The diverse and complex anatomy of the region requires special considerations regarding injuries to the parotid gland/duct, periocular area, nose, lips, and facial nerve, among others. Additionally, proper and timely repair of facial skeletal fractures is important to optimize both functional and aesthetic results. Avoiding large facial incisions often requires special approaches to the facial skeleton, and an adequate understanding of the anatomy and technique is imperative to minimize complications while achieving adequate reduction/fixation. Special consideration is indicated in panfacial fractures where determining premorbid anatomy may be difficult. Accurate diagnosis and careful reduction and fixation will result in better outcomes while minimizing complications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Facial trauma
- Facial fracture
- Soft tissue injury
- Orbital fracture
- Mandible fracture
- Panfacial fracture
- Nasal fracture
Trauma Evaluation
Primary survey – ABCs (airway, breathing, circulation).
Acute life-threatening injuries in facial trauma patients (most to least common) [1]:
-
Cerebral trauma (hematoma most common)
-
Hemorrhagic shock
-
Airway compromise (the midface falls back posteriorly with pterygoid plate fractures)
-
Pulmonary injury
-
Cervical spine injury (very low incidence)
-
Basic airway management: Clear all debris/blood/secretions → Jaw thrust (caution: can cause up to 5 mm of distraction in patients with C5/6 instability).
-
Indications for airway intervention: Apnea/inadequate oxygenation, GCS <9, unstable midface trauma, laryngeal injuries, aspiration risk, large flail segment.
-
Types of airway intervention: Oral airway, LMA, nasopharyngeal intubation (good for spontaneous ventilating patient, contraindicated in skull base fx), oral intubation (minimize C-spine manipulation), tracheostomy, cricothyroidotomy.
-
Hemorrhagic shock: Indicated by hypotension/tachycardia → Initial treatment is 2L crystalloid bolus (20–30% stays intravascular) in adults (20 ml/kg in children) → colloid bolus → consider PRBCs if patient is still unstable after 2L crystalloid bolus [2]:
-
3:1 crystalloid solution replacement for volume of estimated blood loss
-
PRBCs indicated for >30% blood volume loss
-
Correct acid/base/electrolytes
-
Secondary survey – complete physical exam, allergies, medications, past medical history, last meal, details of injury, tetanus status.
Screening C-spine, chest, and pelvic x-rays.
Type/screen, CBC, electrolytes, coagulation status, UA, pregnancy test, drug screen. Consider cardiac enzymes, ABG, and serum amylase.
Soft Tissue Injuries
Lacerations
-
Low risk of infection in the face and scalp due to abundant vascularity. Wounds <24 hours old can be closed primarily with low risk of infection. Wounds >6 hours old or grossly contaminated should be irrigated. Contaminated wounds should be repaired in delayed fashion. High velocity/shotgun GSW should be closed in delayed fashion, treated with debridement, drainage, and packing [3].
-
Preserve all facial tissue unless obvious necrosis. Utilize atraumatic techniques. Freshen edges as appropriate. Layered closure removes dead space and facilitates soft tissue alignment. Undermine as needed to reduce tension at dermal subcutaneous junction. Evert wound edges.
-
Antiseptics have harmful effects on wound healing – should only be used on intact skin around wound. Chlorhexidine better than iodine or alcohol. Hydrogen peroxide harmful to fibroblasts – shouldn’t be used for cleaning open wounds.
-
Antibiotics should be given for bite wounds, infected wounds, smoking, alcoholism, diabetes, coronary artery disease, immunosuppression/immunocompromised, prosthetic valves, or prosthetic joints. Cover skin flora (gram-positives), and include coverage for mixed flora/anaerobes (penicillin, clindamycin) in cases of oropharyngeal exposure.
-
Tetanus risk from contaminated wounds, devitalized tissue, deep wounds, avulsion, stellate lacerations:
-
Low tetanus risk: Tetanus toxoid (Td) if <3 doses of vaccination or uncertain vaccination history; Td if three doses of vaccination and last dose >10 years ago
-
High tetanus risk: Td and tetanus immunoglobulin (TIG) if <3 doses or uncertain vaccination history; Td only if three doses and last dose >5 years ago
-
Bite Wounds
-
Animal bites: Cat bites more likely to become infected than dog bites (Pasteurella, Staphylococcus aureus, Streptococcus viridans). Low rabies risk if animal is a known pet without exposure to virus (no prophylaxis required). If rabies history unsure, quarantine and observe animal. If rabies suspected, kill animal and examine brain tissue. Rabies treatment: immunoglobulin on day 0, vaccine on days 0, 3, 7, 14, 28.
-
Human bites: More likely than animal bites to become infected (Eikenella, Bacteroides, Hep B, Hep C, HSV, HIV). Treat with broad-spectrum abx; cover aerobes and anaerobes.
Facial Nerve
-
Management depends on degree, mechanism, and location of injury.
-
Temporal bone fractures: Incomplete or delayed paralysis can be managed with initial observation. Complete paralysis → ENoG after 72 hours → if >90% degeneration surgical exploration recommended. For immediate, complete paralysis in the presence of temporal bone fracture, immediate exploration is advocated if patient is otherwise stable.
-
Penetrating trauma: High likelihood of nerve transection if paralysis is present. If extratemporal lesion proximal (lateral to lateral canthus), explore within 72 hours so that nerve is identifiable with stimulation. Distal lesions (medial to lateral canthus) → observation with higher likelihood of recovery.
Parotid Gland
Most risk from penetrating injuries occurring below line from the tragus to upper lip. Inspect for facial nerve injury and salivary leak. Buccal branch runs with the parotid duct, most at risk for injury. Risk of damage to the parotid duct stratified by regions:
-
Region A – posterior to masseter, low risk of facial nerve injury, close wound in layers.
-
Region B – area over masseter, highest risk of ductal injury; cannulate duct with stent and anastomose duct over stent or perform superficial parotidectomy.
-
Region C – anterior to masseter, anastomosis not possible; create new duct opening.
Eyelid
-
Traumatic lacerations to the eyelid can create a series of problems, including telecanthus, ptosis, and nasolacrimal disruption. It is important to evaluate all of these at time of repair. The general order is to repair posterior medial canthal tendon first → nasolacrimal system second → marginal eyelid lacerations → peripheral lacerations → ptosis repair at a later date.
-
Medial canthus injury: Disruption of the posterior tendon results in telecanthus, and repair/attachment to lacrimal crest should be done with microplating or transcanthal wires.
-
Marginal lacerations should be meticulously repaired to align lid margin. Topical and injected local anesthetic as well as corneal protectors should be used. Slight eversion with vertical mattress suture helps prevent notching. Primary repair of the tarsus may be necessary at this time.
-
Peripheral lacerations should be repaired only after margin alignment is satisfactory [4].
-
Primary closure can be performed with defects up to ¼ of the lid length. >¼ lid length involvement may require skin graft. Lateral canthotomy may add up to 10 mm of additional lid length.
Nasolacrimal Duct
-
Anatomy : Superior and inferior puncta 5 mm lateral to medial canthus. A 2 mm vertical limb → 8 mm horizontal limb → common canaliculus → lacrimal sac sitting in lacrimal fossa → emptying into the inferior meatus.
-
Lacerations through the medial eyelid should raise suspicion for ductal injury. Symptoms (epiphora) may not present initially especially in the setting of multiple injuries. Before closing the laceration, the puncta and proximal duct should be cannulated to identify proximal segment. If a complete laceration exists, identifying the distal segment can be difficult. Cannulation of the opposing lid affords ability to flush air or dye into the system to locate distal end. Once identified, a silastic or silicone stent is placed and reanastomosis is performed. Tarsal anchoring sutures aid is decreasing tension on repair.
Facial Basics
Bone Healing
Bone healing occurs in several stages:
-
Inflammatory phase (immediate): hematoma, inflammatory response, granulation tissue formation; osteoclasts remove necrotic bone.
-
Soft callus (2–3 weeks): differentiation into osteoblasts, fibroblasts, and chondrocytes; granulation replaced by vessels, ECM, cartilage.
-
Hard callus (3–4 months): endochondral ossification, woven bone formed.
-
Remodeling (months–years): woven bone replaced by lamellar bone.
Fracture Fixation
-
Splinting : Applying rigid device to the fracture (i.e., MMF) helps to reduce fracture segments, but there will always be some movement at the fracture site.
-
Compression: Can be achieved with plates or lag screws. Works by compressing two pieces of bone together, creating a friction and a “preload” on the bone. As long as functional forces do not exceed “preload,” the bone will not move.
Surgical Approaches to Facial Skeleton
Mandible
-
Intraoral: Used to access parasymphyseal, body, and mandibular angle. Relatively safe; be sure to identify mental nerve and resuspend the mentalis muscle.
-
Submandibular: Used to access the mandibular body and angle, often used for complex comminuted fractures or in the setting of an edentulous, atrophic mandible. Care must be taken to avoid the marginal branch of the facial nerve.
-
Submental: Provides access to the anterior body, parasymphyseal, and symphyseal regions. Relatively safe approach, leaves external scar.
-
Retromandibular: Access to the entire ramus and up to the subcondylar region. Risk of external scar and facial nerve injury.
-
Preauricular: Provides access similar to the retromandibular.
-
Facelift: Similar access to retromandibular and preauricular incisions with a more cosmetically favorable incision.
Orbit
-
Subciliary: Lower lid blepharoplasty incision, direct or stair-step incision to orbital rim/floor. Risk of visible incision, soft tissue descent, lower lid malposition → resuspend soft tissues; place Frost stitch.
-
Transconjunctival: Incision at inferior edge of the tarsus, followed by dissection through the septum (retroseptal) or anterior to the septum (preseptal). Orbital fat enters field with retroseptal approach. May need to add lateral canthotomy and cantholysis to improve exposure to orbital floor and lateral rim. No visible incision.
-
Transcaruncular: Incision through caruncle to access medial orbital wall → dissection plane between Horner’s muscle and medial orbital septum (Horner’s muscle inserts onto posterior lacrimal crest, orbital septum along posterior surface of Horner’s muscle). Risk of inferior oblique muscle disinsertion [5]. Inferior fornix incision extends exposure to orbital floor → requires disinsertion of Lockwood ligament and inferior oblique muscle (need to reconstruct when closing).
-
Lateral brow: Incision along lateral eyebrow, provides access to superior orbital rim and zygomaticofrontal suture. No significant neurovascular structures are involved with this approach. Incision hidden within brow.
-
Upper blepharoplasty: More cosmetically appealing access to the superolateral orbital rim.
Maxilla
-
Vestibular/sublabial: Access to inferior orbital rim, zygomaticomaxillary suture, and majority of anterior midface. Infraorbital nerve located 7–10 mm below infraorbital rim, just medial to the zygomaticomaxillary suture. Incisions can be combined with intranasal incisions for midfacial degloving. Nasal support needs to be re-established for adequate projection and tip support. If incision extends bilaterally, nasal base must be resuspended and upper lip advanced with V-Y flap.
-
Zygoma: Isolated zygomatic arch fractures can be approached via two incisions:
-
1.
Gilles: Incision within temporal scalp, 2.5 cm superior and anterior to root of the helix → dissection through superficial temporal fascia and deep temporal fascia → elevator dissection between deep temporal fascia and temporalis muscle until zygomatic arch
-
2.
Keen: Intraoral incision at ZM suture → subperiosteal dissection up to arch
-
1.
Bicoronal Approach
Provides access to superior facial skeleton, ZMC complex, nasal bones, and NOE region. Incision placed 1 cm behind hairline and extends to root of the helix. Raise flap in supraperiosteal plane until supraorbital rim. Pericranial flap can be raised for facial reconstruction. If supraorbital nerve bundle exits from the foramen, use osteotome to release bundle and expose superior orbit.
Lateral to temporal line, dissection is along the deep temporal fascia (frontal branch of CN VII travels within superficial temporal fascia a.k.a. temporoparietal fascia). Avoid trauma to temporal fat pad to prevent temporal wasting. Periosteum over zygomatic arch is incised to expose fracture for reduction and plating.
Endoscopic Browlift Approach
Used for anterior table fractures → vertical working incision and adjacent endoscope incision → subperiosteal elevation to expose fracture and surrounding bone. Minimal risk with approach and cosmesis.
Facial Fractures
Nasal Fractures
Most common facial fracture. Despite the high frequency, controversy still exists on proper management of nasal fractures. Classically, these are best treated with closed nasal reduction within 7–10 days.
While closed reduction does achieve adequate results a majority of the time, open treatment has been shown to get better results. For complex fractures, those involving a largely deviated septum, or those outside of a 2-week window, open reduction +/− osteotomies should be considered. Furthermore, if there is significant septal deformity, releasing the ULCs as well as raising mucoperichondrial flaps can release deformational forces and allow proper realignment [6].
Osteotomies are avoided by many during the acute time period due to fear of instability; however, it has been shown to be an effective maneuver for achieving symmetry (often only need to osteotomize one side, due to trauma already breaking the first).
In the setting of severely comminuted nasal bones, fixation should always be attempted first with miniplating systems. If there are not enough fragments remaining, calvarial (or iliac) bone grafting should be done with the initial repair. This should not be placed over any remaining bone to avoid over-augmentation.
Zygomaticomaxillary Complex (ZMC) Fractures
Combination of fractures at the ZF suture, ZM suture, zygomatic arch, infraorbital rim, and zygomaticosphenoid suture. Strongest bone is ZF buttress; weakest bone is orbital floor. Nondisplaced fractures can be treated conservatively. If zygoma is displaced or comminuted, then ORIF is needed. Malar eminence typically located 2 cm inferior to lateral canthus. Malar flattening can occur due to posterior inferior rotation → reduce fracture segment with anterior superior rotation.
Zingg classification of zygoma fractures:
-
A – one component of tetrapod fracture
-
B – injury to all four supporting structures
-
C – comminution of zygomatic bone
Isolated zygomatic arch fractures:
-
Medially displaced arch – approach with either Keen incision or Gilles incision
-
Laterally displaced arch – approach with coronal incision
ZMC fractures typically treated with 2- or 3-point fixation using ZF suture, ZM suture, and infraorbital rim. Expose all fractures and reduce zygoma before plating. If zygoma is inferomedially displaced, the zygoma can be reduced with elevator or Carroll-Girard screw (screw placed through small skin incision into body of zygoma). Ensure ZS suture is adequately reduced before plating :
-
ZF suture plated first.
-
Thickest plates at lateral buttress (1.5–2 mm); thinnest plates at infraorbital rim and ZF suture (1–1.5 mm).
-
Zygomatic arch is plated when buttresses are comminuted or when arch is not anatomically reduced (arch is plated first before ZF suture); arch has straight configuration, not curved [7].
Cheek numbness commonly due to damage to infraorbital nerve, less commonly zygomaticotemporal and zygomaticofacial nerves. Diplopia results from trauma to extraocular muscles, muscle entrapment, or nerve damage. Enophthalmos – displacement of 1 ml of soft tissue or increase in 1 ml of orbital volume produces 1 mm of enophthalmos (3 mm enophthalmos becomes perceptible). Reduction of medially impacted zygoma can unmask enophthalmos caused by orbital floor/wall fractures .
Naso-Orbito-Ethmoid Fractures
Involves rigid bones (nasofrontal process of maxilla, origin of nasal bones, internal angular process of frontal bone) and fragile bones (ethmoid labyrinth and orbital floor/wall).
Medial canthal tendon → extension of tarsal plates. Receives contributions from preseptal/pretarsal orbicularis oculi, Whitnall’s superior suspensory ligament, and Lockwood’s inferior suspensory ligament. Three heads: superior limb attaches to frontal process of maxilla, posterior limb attaches to lacrimal fossa, and anterior limb fans out to attach to nasal bones.
Normal intercanthal distance 30–35 mm (intercanthal distance = ½ interpupillary distance). Pathologic posterolateral movement of lacrimal bone from fracture may cause telecanthus → almost impossible to correct telecanthus in delayed fashion if not repaired well initially.
Fracture classification :
-
Type 1: single non-comminuted central fragment without MCT disruption
-
Type 2: comminution of central fragment without MCT disruption
-
Type 3: comminution of central fragment with MCT disruption
Approaches: Bicoronal, transconjunctival, vestibular/sublabial, open sky, or existing lacerations.
Treatment: medial orbital wall must be reconstructed prior to MCL:
-
Type 1:
-
Nondisplaced → observation
-
Displaced → 2-point fixation (frontal bone to central fragment, maxilla to central fragment); exposure requires above (bicoronal) and below (sublabial).
-
-
Type 2: more extensive exposure required to locate the MCT and central segment of bone. Treat with ORIF +/− transnasal wiring:
-
Transnasal wiring: Drill holes are placed above and below the tendinous insertion, and 26–28 gauge wire is passed through the drill holes. Transnasal wires are then passed posterior and superior to the lacrimal fossa on the contralateral side and secured to a screw or plate, reducing the central bone segment. Drilling must always be done below the frontoethmoid suture to avoid damage to the cribriform plate. Lastly, microplates are used as in type 1 fractures to get adequate reduction [8].
-
-
Type 3: wide exposure required to locate MCT, treat with transnasal wiring, reconstruct MCT, and ORIF if fracture segments large enough to handle microplates. Bone grafts may be required for tissue loss .
-
Cantilevered calvarial bone grafts used to establish nasal projection after loss of nasal bone structure. Calvarial bone graft length determined intraoperatively based on patient anatomy. Donor site easily accessible from bicoronal incision. Graft secured with screws or miniplate. Care must be taken to establish the proper nasofrontal angle. Drilling a groove into the glabella may facilitate a more secure graft and cosmetically favorable angle.
-
Nasolacrimal duct injuries addressed at the time of fracture repair. Silastic stents placed to maintain patency.
Excessive nasoethmoid width can persist due to:
-
Failure to reduce medial orbital rims.
-
Unrecognized lateral displacement of zygoma (zygoma position sets up reduction of medial maxilla).
-
Failure to reconstruct MCT, MCT stripped from bone during procedure.
-
Scar tissue thickening may mimic telecanthus.
-
Suturing of canthal ligament from inside coronal incision approach rather than externally at eyelid commissure.
Frontal Sinus Fractures
Development: not present at birth, starts at age 2, radiographically detectable at age 6, reaches adult size at ages 12–15. Unilateral in 10%, rudimentary in 5%, absent in 4% of population.
Frontal sinus closely associated with orbit, frontal lobe, and cribriform plate. Anterior table is thick, and posterior table is thin. Sinus drains posteromedially into the nasofrontal duct.
Frontal sinus fractures involve the anterior table only in 50% and anterior and posterior table in 50%. Isolated posterior table fractures rare. Structures to consider when evaluating frontal sinus fractures: anterior table, posterior table, nasofrontal duct. Other injuries to consider: dural tears, CSF leak, cerebral trauma.
Classification [9]:
-
Type 1: isolated anterior table fx
-
Type 2: comminuted anterior table fx +/− NOE, orbital rim fx
-
Type 3: anterior + posterior table fx
-
Type 4: anterior + posterior table fx + CSF leak/dural injury
-
Type 5: anterior + posterior table fx, CSF leak, tissue loss, severe disruption
Treatment :
-
Observation – anterior table fx (type 1) without displacement or deformity
-
Endoscopic – anterior table fx (type 1) with deformity:
-
Fx camouflage easier and more efficacious compared to endoscopic reduction. Wait 3–4 months for edema to subside before repairing fracture. Subperiosteal dissection is similar to endoscopic browlift approach. Porous polyethylene implant carved, inserted over defect, secured with one or two screws. Implant is palpable, but has no discomfort, contour deformity, or mobility [10].
-
-
ORIF – anterior table fractures (types 1, 2) with no nasofrontal duct injury
-
Obliteration – anterior + posterior table fx (types 2, 3) with nasofrontal duct injury:
-
Bicoronal incision, remove all mucosa from frontal sinus, pack frontal sinus and outflow tract with fat, finish with ORIF of frontal sinus
-
-
Cranialization – CSF leak and extensive injury (types 4, 5):
-
Similar approach as obliteration, remove posterior table fragments, place pericranial flap to separate sinus from nasal cavity
-
-
CSF leak – send fluid for tau transferrin to diagnose, can look for “halo” sign (bloody drainage on gauze will have the appearance of halo or target if CSF present). Can manage conservatively initially with head of bed elevation, stool softeners, lumbar drain. Antibiotics administration debated (Fig. 12.1).
Orbital Fractures
-
Anatomy: The orbit is a four-sided pyramid with many bony contributions. The orbital apex houses the optic nerve, while the superior orbital fissure contains CNs III, IV, V1, and VI and the inferior orbital fissure CN V2. The superior aspect of the orbit is formed largely by frontal bone, while laterally it is the zygoma and greater wing of sphenoid. Medially are the ethmoid and lacrimal bones, and inferiorly are the maxilla, palate, and zygoma.
-
Hydraulic Theory: Direct force to the orbit increases orbital pressure which is transmitted to the point of greatest weakness resulting in inferior displacement of the orbital floor contents into the maxillary sinus. Medial wall and floor most fragile.
-
Buckling Theory: Direct force applied to inferior rim transmits anterior to posterior force resulting in fracture of orbital floor. Can be associated with soft tissue injury.
-
Fracture Classification: Important to identify all the structures involved, displacement, size, and location of orbital defects . Orbital floor fracture patterns determined by location of force transduction:
-
Type 1 fracture pattern – force applied to rim, no herniation of orbital contents
-
Type 2 fracture pattern – force applied to globe, larger defect, typically involves medial wall and orbital floor as well as herniation of contents
-
-
Evaluation: Extraocular mobility (forced duction), pupil reactivity, visual acuity, ocular pressure. Comorbid injuries to globe are common; obtain ophthalmology consultation. Emergent issues include severely elevated intraocular pressure (due to retrobulbar hematoma, emphysema, or severe shift in orbital contents) resulting in vision loss/ischemic damage to the retina and optic nerve:
-
Traumatic optic neuropathy (2–5% of severe facial trauma) – vision loss, diminished color perception, APD. Ophtho consult. Consider high-dose corticosteroids, osmotic diuresis, and nerve decompression. For bony nerve impingement, consider urgent decompression.
-
Oculocardiac reflex – vagal stimulation causes nausea, vomiting, bradycardia, and heart block.
-
Diplopia may be due to entrapment (especially in peds) or enophthalmos. Entrapment associated with severe pain, decreased ocular mobility.
-
Enophthalmos >2 mm clinically noticeable – occurs with fracture defect >2 cm2, >2 ml of herniation, or change in shape of orbit from conical to round.
-
Treatment is typically more conservative in adults and more aggressive in peds. Approaches include existing lacerations, subciliary, transconjunctival +/− lateral canthotomy and cantholysis, or transcaruncular +/− inferior fornix extension. No matter the approach, once the orbital rim is reached, it is important to dissect and elevate the periosteum/septum to help retract orbital contents. The contents of the fracture are elevated completely with ribbon retractor, and the floor is reconstructed. Implant materials include split calvarial bone graft, titanium mesh, porous polyethylene, and Silastic sheets.
Recommendations for repair of isolated orbital floor fractures [11]:
-
Immediate repair
-
Oculocardiac reflex
-
White eye fx (entrapment and diplopia in peds)
-
Significant asymmetry (>50% floor involvement +/− soft tissue distortion)
-
-
Within 2 weeks
-
Diplopia without improvement
-
>50% floor involvement without diplopia
-
Infraorbital nerve hypesthesia (according to some case series)
-
-
Observation
-
Minimum diplopia
-
Good motility
-
No significant enophthalmos
-
Complications include dry eye, vision loss, ectropion, lid malposition, diplopia, and enophthalmos.
Post-op diplopia more likely in older patients (28 years vs 46 years) and delayed reconstruction (>2 weeks). Sex, location of defect, and reconstruction materials have no effect on post-op diplopia [12]. Early surgery likely minimizes fibrosis and contracture.
Delayed enophthalmos typically from enlargement of orbital volume → rounding of soft tissues, loss of ligamentous support, globe moves posteriorly, lateral/inferior displacement of lateral rim. Enlargement most common at (1) the inferior orbital fissure, followed by (2) medial orbit and (3) the greater wing of the sphenoid [13]. Fat atrophy is not a major cause of late enophthalmos [14]. Secondary orbital reconstruction less likely to resolve persistent diplopia.
Surgical contraindications : hyphema, open globe, retinal tears/detachment, monocular, frozen globe.
Maxillary/Le Fort Fractures
Large air-filled sinus cavities predispose the midface to fracture with far less force than adjacent facial bones. All Le Fort fx involve pterygoid plate fx. Fracture patterns:
-
Le Fort I: horizontal fx between maxilla and palate, involving nasomaxillary (medial) and zygomaticomaxillary (lateral) buttresses. Seen in 30% of Le Fort fx.
-
Le Fort II: involves nasal bones, frontal process of maxilla, lacrimal bone, orbital floor, infraorbital rim, and lateral maxillary sinus. Seen in 60% of Le Fort fx.
-
Le Fort III: craniofacial disjunction, involves nasofrontal suture, frontal process of maxilla, lacrimal bones, lateral orbital wall, and ZF suture.
-
Palatal and alveolar ridge fractures may be seen in combination with the abovementioned fx patterns.
Early intervention associated with earlier return to function, less infection, decreased scarring, and fewer overall complications. Delay repair in patients with GCS <6, intracranial hemorrhage, or midline cerebral shifts.
Oral intubation allows manipulation of the midface, but may interfere with occlusion. Nasal intubation allows occlusion, but can make nasal and maxillary reduction difficult. Tracheostomy an option for maintaining safe airway while allowing occlusion and MMF.
Multiple approaches used to access the midface. Disimpact and reduce the midface with Rowe forceps. Establish occlusion with MMF. Duration of MMF dependent on degree of fracture and stability achieved with repair. Bone graft may be needed for tissue loss. Low-profile titanium plates used for fixation of fx. Direct plating of palatal fx establishes width, but MMF required to prevent rotation of alveolus.
Titanium mesh can be used to reconstruct large defects in bone along the maxilla [15]. Fibrous capsules form around the implant. Increased thickness of the capsule correlates with increased risk of implant complications: coarse plates form thinnest capsule; smooth plates form the thickest capsule. Neo-mucosa forms over titanium mesh – shows evidence of ciliated respiratory epithelium, goblet cells, chronic inflammation, and squamous metaplasia.
Anterior open bite deformity results when the pterygoid buttress descends inferiorly and posteriorly after midface fx. Persistence of anterior open bite after surgery is due to early release from MMF, late fracture reduction, or placing elastic traction on posterior dentition only.
Class II occlusion (overbite) persists if an anteriorly displaced and impacted maxilla is placed in MMF. The TMJ can slide forward to allow the mandible to accommodate MMF, but slides back after the MMF is released .
Mandible Fractures
Symphysis, parasymphysis, body, angle, ramus, condyle.
Dental numbering (adults) – 8 teeth per quadrant (3 molar, 2 premolar, 1 canine, 2 incisors):
-
Right maxillary third molar (1) → Left maxillary third molar (16)
-
Left mandibular third molar (17) → Right mandibular third molar (32)
Occlusion:
-
Class I (normal occlusion): first maxillary mesiobuccal cusp sits in first mandibular mesiobuccal groove.
-
Class II (overbite): first maxillary mesiobuccal cusp anterior to first mandibular mesiobuccal groove, retrognathia.
-
Class III (underbite): first maxillary mesiobuccal cusp posterior to first mandibular mesiobuccal groove, prognathia.
-
Open bite: normal relationship of molars; anterior dentition doesn’t contact.
-
Cross bite: upper dentition fits into wrong side of lower dentition.
Evaluation : ABCs, C-spine status, intraoral exam (occlusion, missing dentition, laceration/open fractures, stability of the mandible), facial lacerations, lower face deviation, condylar head through EACs. Abx for open fractures. Teeth in fracture site don’t necessarily need to be pulled unless carious or fractured through root. Removal leaves entry point for infection and point of weak fixation. Timely treatment important but rarely an emergency (classic teaching was within 24 hours, but increasing date and practice trends point to repair within 6–10 days without increased risk of complication).
Fracture Classification
Largely based on the location of the fracture (see Fig. 12.2).
-
Fracture favorability: Determined by direction of fracture line and muscle force on mandibular segment. Masseter and temporalis muscles (elevators) can create horizontally unfavorable force of angle fractures. Lateral pterygoid muscles (protrusor) and medial pterygoid muscles (elevator) can pull apart body and symphyseal fractures due to vertically unfavorable forces.
-
Treatment considerations: Take into consideration location of fracture, comminuted vs simple, open vs closed, favorable vs unfavorable fractures. Fractures treated with MMF +/− ORIF depending on the abovementioned factors.
-
Closed treatment (MMF) for comminuted fractures that are minimally displaced/nondisplaced. External pin recommended for severe comminution and soft tissue disruption. Closed treatment avoids removing too many displaced fragments and minimizes risk of devitalizing tissue from open approaches in setting of severe soft tissue damage [16]. External pins and gunshot wounds increase the risk of non-occlusal complications. The number of fragments in fracture has no impact on development of non-occlusal complications. Number of fragments, mechanism of injury, and treatment method don’t have any impact on development of malocclusion. Can be removed 2–6 weeks post placement depending upon fracture and age: condyle/subcondylar, 2 weeks; body/angle: 4 weeks; symphyseal/parasymphyseal, 6 weeks.
-
Subcondylar fractures typically treated conservatively with MMF and early mobilization. Indications for ORIF include condylar neck/subcondylar displacement (>15°) and ramus height instability/loss (>5%), bilateral fractures, and foreign body in TMJ. Indications for MMF include good range of motion, good occlusion, minimal pain, or isolated condylar head fx. Under similar conditions, ORIF should be performed over MMF. Approaches include retromandibular, preauricular, and endoscopic. Compression plates should be used for ORIF, as adaptation plates are less favorable. Risks of ORIF include scars and temporary paralysis from external approaches. MMF risks include pain, malocclusion, asymmetry, and limited mobility [17]. Bilateral fractures at risk for airway compromise (consider tracheotomy/intubation). Present as anterior bite deformity. Need early movement to prevent TMJ ankylosis.
-
Body and parasymphyseal fractures: Tend to be vertically unfavorable. Generally best treated with ORIF through intraoral incisions. Severely comminuted, greenstick, or unstable patients can be treated with closed reduction [16]. Intraoral incision is made leaving cuff of gingival soft tissues, dissection subperiosteally to expose fracture and mental nerves. A 2.3 or 2.7 mm compression plate is placed inferiorly with ≥2 bicortical screws on each side. Next, a tension band (2.0 mm plate) is placed superiorly over the fracture (two monocortical screws on either side). For oblique fractures a bicortical lag screw can be used for fixation.
-
Angle fractures can be repaired in several ways. Nondisplaced or favorable fractures can be treated with 6 weeks of MMF. Champy plate can be placed with intraoral incision. This utilizes compressional forces; the plate is placed after MMF and is located along the oblique ridge. Alternatively, two miniplates can be placed inferiorly and superiorly over the fracture (frequently need percutaneous screw placement). Severe fractures may require an external approach. Highest rate of complications due to location and vector forces from the masseter.
-
Symphyseal fractures : Look for coexisting condylar/subcondylar fractures due to mechanism of injury. Anterior-posterior force transmitted to condyles resulting in fracture. Can be managed with tension/compression plates or lag screw placement.
-
Ramus fractures : Rare due to overlying protection from masseter muscle. ORIF indicated for displaced or multiple fragments.
-
Complications: Chin/lip hypesthesia most common complication secondary to mental nerve injury. Osteomyelitis from unstable segments, loss hardware, infected tooth root in fracture site, poor oral hygiene. Treatment involves removal of unstable hardware and infected teeth and debridement of nonviable bone and IV abx. Malunion, nonunion (fibrous union), exposed hardware, aseptic necrosis of condylar head, TMJ ankylosis, dental injury.
Panfacial Fractures
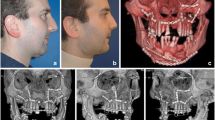
Anatomy: See Fig. 12.3.
Four vertical buttresses: Nasomaxillary, vertical portion of the mandible, zygomaticomaxillary, pterygomaxillary.
Three horizontal buttresses: Frontal bar, infraorbital rim/nasal bones, maxillary alveolus/hard palate.
Establishment of the facial width is one of the primary goals in repairing panfacial fx. If untreated, the face becomes spherical due to increased width and decreased projection.
The sequence of repair varies depending on the text (i.e., known to unknown, superior to inferior, inferior to superior, inside out, outside in). Manson et al. [13] divide the face into upper and lower halves at the Le Fort I level and sequence the lower face and upper face starting at the most stable structure in each half:
-
Lower face composed of occlusal unit (teeth, palate, alveolar processes) and mandibular unit (condyle, ramus, angle, body, symphysis):
-
Reduction sequence: palate → vertical mandible → horizontal mandible
-
-
Upper face composed of upper face (frontal bone, supraorbital rim, orbital roof, frontal sinus) and upper midface (zygoma, nasoethmoid, lateral and inferior orbit):
-
Reduction sequence: cranial base and orbital roof → frontal sinus and frontal bone → nasoethmoid → zygoma
-
Pediatric Facial Fractures
Pediatric facial fx differ significantly from adult facial fx due to anatomic and physiologic differences, developmental and functional impact of treatment, and different treatment algorithms.
Anatomy: The midface is much more protected in peds than in adults. Facial trauma less common in peds due to increased cranial to facial volume (8:1 at birth, 2.5:1 in adults), retruded position of the face relative to the skull, flexible suture lines, lack of sinus pneumatization, and increased mandibular density from tooth buds. The orbit reaches adult size at age 5. The mandible undergoes lingual bone absorption and labial bone deposition and increases in size during puberty. Primary dentition erupts by age 3, and permanent teeth erupt starting at age 6, becoming stable for surgical intervention by age 14.
Bone healing in peds is much faster due to greater osteogenic potential in the periosteum. Faster fracture healing rates result in fracture union at 3 weeks (compared to 6 weeks in adults).
Mandible fx: Irregular fx lines due to tooth buds and crypts. Condylar head/neck fx most common. Conservative management favored due to high osteogenic potential, presence of primary and secondary dentition, and potential adverse effects of ORIF on craniofacial growth:
-
Nonsurgical management (ORIF, PT, pain control): used for condylar fx and nondisplaced/greenstick fx of body and ramus, has advantage of decreased immobilization, muscle atrophy, ankyloses, and improved oral hygiene [18]. Not indicated for significantly displaced fx.
-
Surgical management for body, angle, and parasymphyseal fx:
-
Closed reduction: interdental wires if dentition stable, occlusal splints if dentition unstable.
-
ORIF for displaced fx, decreases immobilization time and improves dental hygiene. Use of titanium plates is controversial because of potential growth impediment from periosteal stripping and removal of growth stimulus, possible dental trauma from screw tips (avoid bicortical screws), and need for secondary surgeries to remove plates. Absorbable plates (poly-L-lactic acid, polyglycolic acid) are bulkier and less malleable and require pre-drilling and pre-tapping, but don’t require secondary surgeries for plate removal.
-
Orbital floor fractures are most common in peds, but there is an increased risk of orbital roof fractures in children <10 years due to decreased sinus pneumatization. Peds orbital trauma presents with less swelling, but more likely to have serious sequela of diplopia and EOM limitation. Greenstick/trapdoor fx more likely in children → entrapment of inferior rectus → muscle necrosis and fibrosis → diplopia. Peds orbital fx are managed more conservatively – surgery reserved for enophthalmos, entrapment, and oculocardiac symptoms only [19]. Repair should be undertaken <7 days, but trapdoor fx are true surgical emergencies and should be repaired <24 hours [20].
Nasal trauma is common in this population. The nasal bones have not fused yet, and the cartilage is relatively larger and more pliable than adults. Conservative reduction is recommended and there should always be a high index of suspicion for septal hematoma.
Questions
-
1.
When evaluating a patient in the ED with complex laceration to the right cheek and orbital area, you note the patient has a full-thickness eyelid laceration through the upper lid, extending medially, as well as MRD1 of 1. Which is of least concern when repairing at bedside?
-
(a)
Meticulous alignment of the tarsus
-
(b)
Evaluating for corneal integrity
-
(c)
Correction of ptosis by reapproximating lid retractors
-
(d)
Evaluating and stenting lacrimal duct
-
(a)
-
2.
When evaluating the same patient in the ED, you note another knife wound to the right cheek, approximately 2 cm anterior to the tragus and just below the zygomatic arch. Facial motion is intact throughout. Upon massage, you note some saliva within the wound. Next step in management?
-
(a)
Allow to granulate in, place on abx.
-
(b)
Cannulate the duct and perform anastomosis.
-
(c)
Close the parotid parenchyma and layered wound closure, abx.
-
(d)
Close skin only, ENOG after 72 hours, repair facial nerve if needed.
-
(a)
-
3.
A 7-year-old male presents to the emergency room after falling off a bicycle. Physical examination showed trismus secondary to pain and tenderness over the left condyle. His dentition is intact and stable. CT scan showed only a minimally displaced left subcondylar fracture and a nondisplaced right parasymphyseal fracture. What is the best treatment plan?
-
(a)
MMF only for 3 weeks
-
(b)
MMF and ORIF for 3 weeks
-
(c)
MMF only for 6 weeks
-
(d)
MMF and ORIF for 6 weeks
-
(a)
-
4.
A 9-year-old female presents to the emergency room after a MVC. Examination of the mandible showed multiple absent and unstable teeth as well as a mucosal laceration over the right mandibular gingiva. CT scan showed a nondisplaced fracture over the right mandibular parasymphysis. What is the best treatment option?
-
(a)
Interdental wiring
-
(b)
Occlusal splints with circum-mandibular wiring
-
(c)
MMF with drop wires
-
(d)
ORIF with titanium plates
-
(a)
-
5.
Compared to adult orbital fractures, pediatric orbital fractures have more of the following signs and symptoms except:
-
(a)
Greenstick fracture on CT
-
(b)
Entrapment with diplopia
-
(c)
Periorbital edema
-
(d)
Clinically detectable enophthalmos
-
(a)
-
6.
A 6-year-old male presents to the emergency room after being struck in the eye by a baseball. He had no loss of consciousness. He is resting comfortably without nausea. His visual acuity is normal. He has 3 mm of enophthalmos on exam. CT shows a defect over 60% of the orbital floor. Which part of the history and physical is the indication for surgical intervention?
-
(a)
Enophthalmos of 3 mm
-
(b)
Orbital floor defect 60%
-
(c)
Oculocardiac symptoms
-
(d)
None of the above
-
(a)
-
7.
All of the following are characteristics of the pediatric facial skeleton EXCEPT:
-
(a)
Decreased sinus pneumatization
-
(b)
Increased cranial volume to facial volume
-
(c)
Decreased osteogenic potential
-
(d)
Increased mandibular angle
-
(a)
-
8.
Which of the following statements regarding ORIF and pediatric mandible growth is true?
-
(a)
The symphysis is the growth center of the mandible.
-
(b)
Load-bearing potential from titanium plates doesn’t impact growth potential.
-
(c)
Periosteal stripping has no impact on mandibular growth.
-
(d)
Titanium plate migration may occur if not removed at a second surgery.
-
(a)
-
9.
A 25-year-old male presents with a gunshot wound through the right mandibular body. CT scan shows multiple comminuted fracture segments. Which of the following confers the highest risk for non-occlusal complications?
-
(a)
Number of bone fragments
-
(b)
Closed treatment with external pins
-
(c)
Open treatment with MMF
-
(d)
Open treatment with rigid internal fixation
-
(a)
-
10.
A 58-year-old male suffered a severely displaced left ZMC fracture after a MVC. On questioning, he complains of new visual disturbances since the trauma. Which of the following symptoms is NOT associated with traumatic optic neuropathy?
-
(a)
Vision loss
-
(b)
Diminished color perception
-
(c)
Afferent pupillary defect
-
(d)
Diplopia
-
(a)
-
11.
When treating a ZMC fracture with displacement of the arch and comminution of the ZF buttress, ZM buttress, and infraorbital rim, which location should be plated first?
-
(a)
Zygomatic arch
-
(b)
Zygomaticofrontal buttress
-
(c)
Zygomaticomaxillary buttress
-
(d)
Infraorbital rim
-
(a)
-
12.
What is the most common life-threatening injury associated with facial fractures?
-
(a)
Cervical spine injury
-
(b)
Cerebral trauma
-
(c)
Airway compromise
-
(d)
Hemorrhagic shock
-
(a)
-
13.
A 42-year-old female involved in an MVC suffered a frontal sinus fracture. CT scan shows comminuted anterior table fracture and nondisplaced posterior table fracture. After visualizing the frontal sinus via a bicoronal approach, a dural tear and CSF leak are identified. What is the best treatment option?
-
(a)
Terminate the procedure, place a lumbar drain, and start antibiotics.
-
(b)
ORIF of the anterior table and place a lumbar drain.
-
(c)
Remove the posterior table, cranialization, and ORIF of the anterior table.
-
(d)
Remove the frontal sinus mucosa and obliterate the frontal sinus with fat.
-
(a)
-
14.
A 35-year-old male undergoes a transcaruncular approach to repair an isolated medial orbital wall fracture. Repair is performed by placing a porous polyethylene implant over the defect after elevating the orbital contents out of the defect. The incision is extended into the inferior fornix in order to insert the implant. The surgery is completed without complication, but the patient complains of diplopia on downward gaze after surgery. What is the most likely reason for diplopia?
-
(a)
Change in orbit shape from conical to round
-
(b)
Entrapment of medial rectus muscle
-
(c)
Occult orbital floor fracture
-
(d)
Disinsertion of the inferior oblique muscle
-
(a)
-
15.
A 20-year-old male presents after blunt trauma to the jaw. He has minimal pain and no trismus. His dentition appears intact. CT scan shows a left condylar head fracture that is comminuted. What is the best treatment option?
-
(a)
Soft diet
-
(b)
MMF
-
(c)
ORIF with compression plate
-
(d)
ORIF with adaptation plate
-
(a)
-
16.
A 20-year-old male presents after blunt trauma to the jaw. He has minimal pain and mild trismus. His dentition appears intact. CT scan shows a minimally displaced left subcondylar fracture. Considering the long-term complications of condylar fracture treatment, which of the following is the best treatment option?
-
(a)
Soft diet
-
(b)
MMF
-
(c)
ORIF with compression plate
-
(d)
ORIF with adaptation plate
-
(a)
-
17.
When determining the timing of pure orbital fracture repair, which of the following clinical scenarios could be repaired 1–2 weeks after trauma?
-
(a)
An adult with intractable nausea and vomiting
-
(b)
A pediatric patient with motility restriction but without ecchymosis or edema
-
(c)
An adult with progressive infraorbital hypesthesia
-
(d)
A pediatric patient with minimal diplopia and good ocular motility
-
(a)
-
18.
A combined transcaruncular and inferior fornix approach is used to repair a combined medial orbital wall and orbital floor fracture. Which of the following statements is correct?
-
(a)
Dissection is between Horner’s muscle and orbital septum, and the inferior oblique muscle and Lockwood’s ligament are disinserted.
-
(b)
Dissection is between the inferior oblique muscle and Lockwood’s ligament, and Horner’s muscle and the orbital septum are disinserted.
-
(c)
Dissection is between Horner’s muscle and inferior oblique muscle, and the orbital septum and Lockwood’s ligament are disinserted.
-
(d)
Dissection is between the orbital septum and Lockwood’s ligament, and Horner’s muscle and the inferior oblique muscle are disinserted.
-
(a)
-
19.
A 50-year-old male presents 1 week after trauma with an orbital blowout fracture. He has diplopia on exam. CT scan shows an orbital floor defect involving approximately 60% of the floor. He undergoes immediate reconstruction with a Medpor implant. Which of the following is the biggest risk factor for postoperative diplopia?
-
(a)
Gender
-
(b)
Age
-
(c)
Location of defect
-
(d)
Reconstruction material
-
(a)
-
20.
Which of the following does NOT cause late enophthalmos after orbital trauma?
-
(a)
Enlarged posterior orbit volume
-
(b)
Lateral displacement of the lateral orbital rim
-
(c)
Loss of ligamentous support
-
(d)
Fat atrophy
-
(a)
-
21.
A 44-year-old woman presents 5 years after a right ZMC fracture. She underwent initial reconstructive surgery but presents today with persistent enophthalmos and diplopia. In addition, her physical exam is notable for hypoglobus and superior sulcus deformity. After undergoing revision surgery involving osteotomies and repositioning of the ZMC, which of the following is NOT expected to improve?
-
(a)
Diplopia
-
(b)
Enophthalmos
-
(c)
Hypoglobus
-
(d)
Superior sulcus
-
(a)
-
22.
After performing an endoscopic approach to a displaced anterior table frontal sinus fracture with placement of a Medpor implant, what is the most likely complaint in the postoperative period?
-
(a)
Implant mobility
-
(b)
Discomfort at the implant site
-
(c)
Persistent contour deformity
-
(d)
Implant palpability
-
(a)
-
23.
True or false? Reconstruction of a large anterior maxillary wall defect with titanium mesh prevents soft tissue ingrowth with respiratory mucosa.
-
(a)
True
-
(b)
False
-
(a)
-
24.
A patient is released from MMF 4 weeks after undergoing ORIF and MMF for panfacial fractures, including bilateral Le Fort I and II fractures. Shortly thereafter, he complains of his incisors not contacting when he bites. All of the following are possible reasons for his complaint EXCEPT:
-
(a)
Late release from MMF
-
(b)
Late fracture reduction
-
(c)
Placing elastic traction on posterior dentition
-
(d)
Placing an anteriorly displaced and impacted maxilla on MMF
-
(a)
-
25.
Telecanthus after treating nasoethmoid fractures can be due to all of the following EXCEPT:
-
(a)
Medially displaced zygoma fractures
-
(b)
Anteriorly positioned transnasal wires
-
(c)
Hematoma and scarring at the canthal area
-
(d)
Resuspending the medial canthal tendon via the coronal incision
-
(a)
Answers
-
1.
(c)
-
2.
(b)
-
3.
(a)
-
4.
(b)
-
5.
(c)
-
6.
(a)
-
7.
(c)
-
8.
(d)
-
9.
(b)
-
10.
(d)
-
11.
(a)
-
12.
(b)
-
13.
(c)
-
14.
(d)
-
15.
(b)
-
16.
(d)
-
17.
(c)
-
18.
(a)
-
19.
(b)
-
20.
(d)
-
21.
(a)
-
22.
(d)
-
23.
(b)
-
24.
(a)
-
25.
(a)
References
Tung TC, Tseng WS, Chen CT, Lai JP, Chen YR. Acute life threatening injuries in facial fracture patients: a review of 1025 patients. J Trauma. 2000;49(3):420–4.
Papel ID. Facial plastic and reconstructive surgery. 3rd ed. New York: Thieme Medical Publishers, Inc.; 2002.
Leach J. Proper handling of soft tissue in the acute phase. Facial Plast Surg. 2001;17(4):227–38.
Sykes JM, Dugan FM Jr. Evaluation and management of eyelid trauma. Facial Plast Surg. 1994;10(2):157–71. NY: Thieme
Goldberg RA, Mancini R, Demer JL. The transcaruncular approach: surgical anatomy and technique. Arch Facial Plast Surg. 2007;9(6):443–7.
Staffel JG. Optimizing treatment of nasal fractures. Laryngoscope. 2002;112(10):1709–19.
Hollier LH, Thorton J, Pazmino P, Stal S. The management of orbitozygomatic fractures. Plast Reconstr Surg. 2003;111(7):2386–92.
Markowitz BL, Manson PN, Sargent L, Vander Kolk CA, Yaremchuk M, Glassman D, et al. Management of the medial canthal tendon in nasoethmoid orbital fractures: the importance of the central fragment in classification and treatment. Plast Reconstr Surg. 1991;87(5):843–53.
Manolidis S. Frontal sinus injuries: associated injuries and surgical management of 93 patients. J Oral Maxillofac Surg. 2004;62(7):882–91.
Kim KK, et al. Endoscopic repair of anterior table frontal sinus fractures with medpor implant. Otolaryngol Head Neck Surg. 2007;136(4):568–72.
Burnstine MA. Clinical recommendations for repair of isolated orbital floor fractures. Ophthalmology. 2002;109(7):1207–11.
Hosal BM, Beatty RL. Diplopia and enophthalmos after surgical repair of blowout fracture. Orbit. 2002;21(1):27–33.
Manson PN, et al. Subunit principles in midface fractures: the importance of sagittal buttresses, soft-tissue reductions, and sequencing treatment of segmental fractures. Plast Reconstr Surg. 1999;103(4):1287–306.
Kellman RM, Bersani T. Delayed and secondary repair of posttraumatic enophthalmos and orbital deformities. Facial Plast Surg Clin North Am. 2002;10(3):311–23.
Schubert W, et al. Incorporation of titanium mesh in orbital and midface reconstruction. Plast Reconstr Surg. 2002;110(4):1022–30.
Ellis E 3rd, Muniz O, Anand K. Treatment of considerations for comminuted mandibular fractures. J Oral Maxillofac Surg. 2003;61(8):861–70.
Brandt MT, Hag RH. Open versus closed reduction of adult mandibular condyle fractures: a review of the literature regarding the evolution of current thoughts on management. J Oral Maxillofac Surg. 2003;61(11):1324–32.
Smith DM, et al. 215 mandible fractures in 120 children: demographics, treatment, outcomes, and early growth data. Plast Reconstr Surg. 2013;131(6):1348–58.
Losee JE, et al. Pediatric orbital fractures: classification, management, and early follow-up. Plast Reconstr Surg. 2008;122(3):886–97.
Gerbino G, et al. Surgical management of orbital trapdoor fracture in a pediatric population. J Oral Maxillofac Surg. 2010;68(6):13010–1316.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s)
About this chapter
Cite this chapter
Teng, J., Harbison, J.M. (2021). Trauma. In: Wong, B.JF., Arnold, M.G., Boeckmann, J.O. (eds) Facial Plastic and Reconstructive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-45920-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-45920-8_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45919-2
Online ISBN: 978-3-030-45920-8
eBook Packages: MedicineMedicine (R0)