Abstract
The amount of residual tooth structure is considered as the main factor to determine the survival of an endodontically treated tooth. Over the last years all the efforts in endodontics and restorative dentistry have been directed toward a paradigm shift from the traditional rules to a more conservative and minimally invasive approach, in order to preserve as much tooth structure as possible in all the procedures: from the access cavity preparation to the choice of the type of coronal restoration. In this perspective new trends in access cavity opening, the introduction of heat-treated NiTi alloys for root canal preparation and fiber-reinforcement for post fabrication have represented a great achievement.
The restorative choice should be assessed even taking into high consideration the occlusion rules that still remain crucial to guide the clinician in a correct management of coronal restorations. Furthermore, most destructive decays can be detrimental for periodontal health: biological width and crown-root ratio become important concepts to be focused and orthodontic extrusion and surgical crown lengthening can be performed to provide a favorable ferrule effect and improve biomechanical behavior of the restored tooth.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Minimally invasive dentistry
- Endodontically treated teeth
- Post-endodontic restoration
- Fiber post
- Crown-root ratio
- Residual tooth structure
8.1 Introduction
Numerous articles have been published about endodontically treated teeth over the past decades. Among all the articles on this topic the conclusion of a Cochrane review [1] is particularly interesting: until more evidence becomes available, clinicians should continue to choose how to restore root-filled teeth based on their own clinical experience. In fact, a lot of variables may play a great role in the restoration of endodontically treated teeth and, lacking a strong evidence, individual circumstances and patients’ preferences may determine the rehabilitation strategy.
Endodontically treated teeth have a minimum loss of water content [2] and the proprioceptive perception of these teeth may change [3, 4], but the variations in their structure summarized by Gutmann [5] do not affect the mechanical properties of dentin, as demonstrated by several tests (punch shear strength, toughness test, load to flexural fracture) performed on both vital and contralateral teeth endodontically treated at least 10 years before and then extracted for orthodontic reasons [6].
Researches on this topic mainly focused on the amount of the residual tooth structure as the most important issue influencing endodontically treated teeth resistance [7, 8]. Panitvisai and Messer [9] showed that the deflection of the cusps increases with increasing cavity size from an occlusal cavity to a mesio-occlusal (MO) or disto-occlusal (DO) cavity to a mesio-occluso-distal (MOD) cavity. Nevertheless, only performing the endodontic procedures showed a small effect on tooth stiffness. In this case, the 5% reduction in relative stiffness from endodontic treatment is contributed entirely by the access opening [7]. An occlusal cavity preparation due to an occlusal caries can show a fourfold greater decrease in tooth stiffness (20%) than the only endodontic access cavity preparation [7]. Both procedures involve the same tooth occlusal area, but a greater extension of the caries and consequently of the occlusal cavity on the marginal ridge area may explain this difference. Therefore, the relevance of the marginal ridge integrity comes out and its violation can be considered as the greatest contribution to loss of tooth strength. A two-surface cavity preparation requires the removal of only one marginal ridge, like in a MO or DO cavity. It results in a 46% loss in tooth stiffness, while extending the cavity preparation to a MOD cavity results in an average of 63% loss of cuspal relative stiffness [7].
Clearly, even if endodontic access cavity preparation itself was thought to make teeth more susceptible to fracture as a result of the loss of tooth vitality, restorative procedures due to the loss of tooth structures are the major factor in weakening the tooth [10]. Thus, the decision on the type of restoration for an endodontically treated tooth should take in greater account the loss of tooth structure, in particular of the marginal ridges rather than the endodontic procedure itself.
The golden rule in common with access cavity and root canal preparation is to preserve as much sound dentin as possible, following a minimally invasive approach. The prognosis of an endodontically treated tooth improves proportionally to the amount of sound tooth structure, regardless of the type of restoration that is subsequently provided [11, 12]. Factors that can impair resistance of the tooth removing enamel and dentin structure during the access approach and the root canal preparation have been clearly reported in the Chapters 3 and 4 of this book.
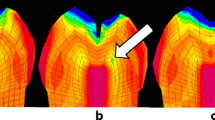
8.2 Minimally Invasive Approach to Restorative Procedures
Minimally invasive approaches in endodontic procedures may guarantee less sacrifice of sound tooth structure, especially at the level of the cervical area of the tooth, that is where coronal fractures mostly happen, thus influencing also the restorative algorithm [13]. In fact, clinicians should always start their endodontic procedures keeping in mind that endodontics does not represent only “white lines” on a radiograph, but should be part of a more complex treatment plan that aims to restore the tooth to its original function in the mouth system. Following this principle, endodontists should always perform their procedures having the vision on the final aim of their work: to put the tooth in function again. The great indiscriminate removal of dentin given by a traditional endodontic access cavity, which recommends in all cases a predefined shape of the occlusal cavity and a straight-line access for the stainless-steel files to the apical curvatures removing the coronal interferences [14,15,16], may reduce the resistance of the tooth [17] and impair the long-term prognosis [18]. A more conservative approach that takes in higher consideration the peri-cervical dentin, the axial wall dentin, and the soffit, representing the most relevant tooth structure to be maintained and preserved, may increase the resistance to fracture of an endodontically treated tooth and its long-term retention, following the simple principle that the greater amount of dentin is kept, the longer the tooth may be maintained [18] (Fig. 8.1). The possibility to perform more conservative treatments with a dynamic approach given by the technological advancement of instruments, materials, and techniques [19], as demonstrated throughout all this book, permits the clinician to save tooth structure and influence the treatment plan from a restorative point of view (Fig. 8.2).
Conservative approach in endodontics in a 15-year-old case demonstrating the way of thinking even when the actual technologies were not present. Preoperative view of the first lower left molar tooth with a deep occlusal caries (a). Conservative access cavity (b). Scouting of the root canals (c, d). The final root canal therapy with the preservation of sound dentine permits a direct restoration without post placement (e, f). A 15-year control radiograph (g)
Conservative approach in endodontics. Preoperative view of the second lower right molar with an old mesial restoration (a). Thanks to their higher flexibility, heat-treated NiTi alloys permits to shape successfully even severely curved canals, like the distal (b), with the preservation of the original anatomy (c) and to be conservative even in the access cavity (d). Restoration with an indirect composite onlay (e) and 2- and 4-years follow-up radiographs (f, g) and image (h)
Technological advancements on the restorative field also permit today more conservative tooth preparations: the most modern restorative materials may be highly performant in much less thickness than before [20, 21], and the advancements in bonding technology [22] permit to create adhesive restorations in most of the cases of endodontically treated teeth except when a full crown is already present. Both these important technological advancements reduce the sacrifice of sound tooth structure required during restorative procedures and cavity preparation, as partial adhesive restorations with complete or partial cuspal coverage may be performed in most of the teeth endodontically treated following the minimally invasive procedures described in this book and given the fact that less extensive tooth preparation is today required for a full-crown restoration, when necessary [23, 24]. In any case, the dogmatic correlation between endodontics and full-crown restoration given by classic studies [25,26,27], in which a complete cuspal coverage with a full crown was advocated for any endodontically treated tooth, independently of the amount of residual tooth structure, to reduce the risk for fracture and improve the prognosis of these teeth, may be no more actual, given the present advancements described above.
8.3 Post-endodontic Restoration: How and Why
The type of restoration on an endodontically treated tooth may be strongly influenced by the amount of residual tooth structure and the need or not for a partial or complete cuspal coverage [28]. In case that a cuspal coverage may be not needed, an inlay restoration (direct or indirect) may be performed, while when a partial or complete cuspal coverage will be required it may be usually performed with an indirect restoration. The onlay restoration is represented by a partial cuspal coverage, usually involving the cusps and tooth structure near a marginal ridge missing, while an overlay restoration is a complete cuspal coverage with a partial tooth preparation that differs from a 360° full crown preparation because of coronal exposed margins saving more cervical toot structure [29]. Usually the cuspal coverage with onlays/overlays is performed with an indirect restoration, even if in some cases it can be accomplished even with a direct restoration [30]. A direct restoration involving partial or complete cuspal coverage should be considered as a compromise respect to an indirect one, not because it may reduce the fracture strength of the tooth, as it has demonstrated no difference between the two different types of restoration [31], but because it may be more related to the operator skills, given the higher difficulties to perform the correct occlusal and interproximal shape directly in the mouth.
An analysis of the variables that may influence the type of restoration required for an endodontically treated tooth is mainly needed in order to reduce the risk for tooth fracture, which is the most common reason for their failure [32]. The decision on cuspal coverage (and also post placement, as reported later on this chapter) is mainly based on the following parameters: the quantity and quality of residual tooth structure, mainly given by the number and thickness of the remaining cavity walls and the height and thickness of the prepared dentin to be covered (ferrule effect), in case of full-crown restorations.
Generally speaking, in the presence of only an occlusal endodontic cavity, cuspal coverage and post are not necessary and the clinician should only perform a simple direct filling of this space. If only one marginal ridge is lost, usually a post is not needed [33, 34], while the cuspal coverage may be suggested in posterior teeth depending on the quantity and quality of residual tooth structure [35]. Despite the rule should be to cover the cusps near the marginal ridge lost, in these cases the thickness of residual walls near the marginal ridge lost is a determining factor to decide when the cuspal coverage of the adjacent cusps is required: when this thickness is less than 2 mm, cuspal coverage may be suggested [36,37,38]. However, in these cases, a modern most conservative access cavity design and root canal preparation may preserve critical tooth structure [17], thus permitting in some selected situations a direct (or indirect) restoration without any cuspal coverage even when a marginal ridge is missing.
When both marginal ridges are lost, the result is a strong reduction in tooth stiffness [7] and complete cuspal coverage and post are usually required in almost all these cases. Given the most modern and conservative endodontic approaches described above and throughout all this book, most of these cases may be solved performing a complete cuspal coverage with a partial restoration adhesively cemented, while in case of further tooth structure loss, post and cuspal coverage with a full crown are more indicated. A direct restoration without cuspal coverage and post placement in these cases should be considered an extreme compromise for patients requiring it for a particular socio-economical situation [39].
The height and thickness of the prepared dentin to be covered by a full crown is related to the ferrule effect. A ferrule effect is defined as a “360° collar of the crown surrounding the parallel walls of the dentin extending coronal to the most cervical point of the preparation. The result is an elevation in resistance form of the crown from the extension of dentinal tooth structure” [40]. Therefore, the presence of circumferential 2 mm high parallel walls of dentin extending coronally from the crown margin provide a “ferrule”: after being encircled by a crown, it provides a protective effect by reducing stresses within a tooth, called the “ferrule effect” [41]. Maintaining sound coronal and radicular tooth structure and cervical tissue to create a ferrule effect is crucial to optimize the biomechanical behavior of the restored tooth and to guarantee a better prognosis [12]. In fact, in addition to the relative consistency in literature supporting the 2 mm height rule, some authors have implicated even the thickness of residual axial tooth structure after coronal preparation to be significant for fracture resistance [42]. The thickness of the residual dentin after the preparation for the crown should be at least 1 mm [43]. Jotkowitz and Samet [42] also stressed the number of walls as another aspect that should be re-thought. Usually caries brings down some walls, and more frequently the proximal ones, while erosion and abrasion more commonly affect only the buccal walls. If the clinical situation does not provide a circumferential ferrule, an incomplete ferrule is always preferable than a complete lack of ferrule [44]. Furthermore, when an incomplete ferrule is present in anterior teeth, the presence of the palatal wall becomes more important than the other walls in terms of fracture resistance [44].
The clinician should also take a decision when to insert a root canal post or not, and this procedure is determined by more factors than just the number and thickness of the residual cavity walls and the height and quality of the ferrule present, as it will be reported in the last part of this chapter.
Additional parameters to be taken into consideration for the restoration of endodontically treated teeth that may influence the type of restoration required are: the position of the tooth in the arch (anteriors, premolars, molars), the role of the tooth in the rehabilitation (single-tooth, part of a bridge or of a full mouth restoration), and the strength of occlusal and shear stress (parafunctions, antagonist teeth, orthodontic class). In particular, if a tooth is part of a most complex restoration, it must be considered in a different way rather than if it is a single tooth restoration, as the loss of a tooth with a poor prognosis, but included in a full-arch restoration may impair the prognosis of the entire rehabilitation.
8.4 Parameters Influencing Restoration of Endodontically Treated Anterior Teeth
In anterior teeth, in cases of an intact crown where only the access cavity has been opened, a simple direct composite restoration may be performed to fill the palatal access [45] (Fig. 8.3). When a more incisal conservative access with a direction parallel to the long axis of the root following the principles given in Chap. 3 is performed (Fig. 8.4), a greater attention should be given to clean the mesial and distal pulp horns to prevent future crown discoloration and voids in the restoration in these points [46]. As a general rule, gutta-percha filling should be limited 2 mm below the root canal orifices that should be adhesively sealed and filled with resin composite during the restorative process or by the endodontist specialist before to send back the case to the referral dentist (in cases in which a post will be not needed). This is of particular importance in the anterior teeth to prevent crown discoloration by the root canal filling materials in the cervical area, through the dentinal tubules that in this region of the tooth proceed in an apico-coronal direction from the canal to the enamel [47]. Thus, the dentinal tubules starting from the buccal part of the canal 2 mm below the CEJ will finish in the CEJ area, which in case of cemental defects may be stained by endodontic materials. In retreatment cases in which this discoloration is already present, an internal bleaching may be needed to solve it before completing the restoration [48, 49]. A flowable resin composite may be the material of choice to seal the root canal up to the orifices, moved by a thin sharp probe to reduce the inclusion of air bubbles between the gutta-percha and composite layers. In fact, inclusion of air bubbles in between the different layers of restorative materials may be difficult to be prevented when restoring a conservative access cavity with four walls, especially between the different layers of standard packable resin composite that should then be used in 2 mm thickness to complete the filling of the coronal access up to the occlusal surface [50]. In these cases, especially in posterior teeth with less esthetic requirements, clinicians may take the advantage of using bulk-fill flowable injectable resin composites with layer thickness of 4 mm to better fill undercuts and reduce air bubble inclusion [51]. The occlusal 1.5–2 mm layer should then always be filled with a packable standard composite with better mechanical properties than a flowable material.
In endodontically treated anterior teeth with a moderate loss of tooth structure, the clinician can decide case by case according to the different tooth characteristics to put a post or not and to perform a full crown or a veneer or a direct composite restoration. Usually, a fiber post or a full crown is not required in these cases [45] (Fig. 8.5), but some clinical exceptions to this rule should be considered. In case of the reattachment of a fragment, when a coronal fracture occurred in an anterior tooth, a strategical short post may be used to connect the fragment to the residual tooth structure, thus contrasting the harmful effects of lateral forces (Fig. 8.6). A strategical post may be also suggested in endodontically treated anterior teeth with incomplete root formation in young patients in which usually an apical plug with MTA has been performed to seal the open apex. Afterwards, a restoration using a fiber post may be performed to improve the resistance of the low thickness residual dentinal walls (Fig. 8.7). Similar indications to the use of a strategical post may exist when an unexpected big loss of coronal tooth structure may be a consequence of a complex endodontic clinical situation, such as to remove coronal calcifications to find a calcified root canal deep inside the root of a traumatized anterior tooth or in the presence of massive internal root resorptions (Fig. 8.8). Even the change of teeth axis during a prosthetic preparation in complex prosthetic rehabilitations may require the use of a strategical post to better maintain the core that will be extensively reduced by the circumferential tooth preparation.
Crown fracture of the maxillary left central incisor (a). The preoperative radiograph shows an incorrect endodontic treatment (b). The restoration was performed before the endodontic retreatment for esthetic request of the patient (c). Postoperative radiograph of the endodontic retreatment (d). Then a 2-week internal bleaching and a final direct restoration of the palatal access were performed because of tooth discoloration. 2-year follow-up of the endodontic treatment and the direct restoration (e, f)
An anterior tooth with a severe loss of tooth structure usually needs a fiber post placement and a full-crown restoration (Fig. 8.9). In these cases, a post is mainly needed to maintain the core and to better dissipate the functional stresses, especially to withstand the lateral forces, thus reducing the risks for a possible dramatic failure, and a full crown on a 2 mm circumferential ferrule is mandatory for a better long-term prognosis. In fact, it has been demonstrated that in these cases of big amount of loss of coronal tooth structure the presence of a post may reduce the number of catastrophic failures (mainly given by vertical unrestorable root fractures leading to the extraction of the tooth), increasing the possibility that the eventual failure may be more favorable and thus restorable, postponing the extraction of the tooth [52, 53]. When an old full crown should be substituted in the anterior teeth, different strategies may be followed and depending on the quantity and quality of the residual tooth structure a post may be inserted or not before performing a new restoration (Fig. 8.10).
Post and full crown need in a maxillary right lateral incisor with severe loss of tooth structure. Preoperative frontal (a) and occlusal (b) views. The preoperative radiograph shows an old retrograde filling with amalgam and a periapical lesion (c). After endodontic retreatment (d), post placement and full-crown restoration (Lab Loreti, Rome—Italy) (e). 2-year follow-up radiographical (f) and intraoral (g) views
Maxillary central incisors with bad conditions of the old full crowns and the surrounding soft tissues (a). Unacceptable root canal treatment for both quality and extent of the filling, with radiographic signs of periapical lesions (b). Full-crown restoration (Lab Loreti, Rome—Italy) (c) and post placement was performed in the right central incisor for the poor amount of residual tooth structure, while a post was not necessary in the other tooth (d). 5-year follow-up intraoral (e) and radiographical (f) views
Given the less occlusal stress and masticatory forces acting on the anterior teeth [54], in some situation when the loss of tooth structure involves the incisal tooth part up to the middle third of the crown and there are ideal conditions in terms of occlusion, a direct esthetic composite restoration may also be performed by a skilled clinician to restore the entire missing tooth structure. In these cases, the use of a post may be useful to better maintain the restoration and, above all, to withstand the lateral forces that may act to the restoration and promote its mechanical failure and detachment (Fig. 8.11).
On the contrary, when a complete loss of coronal tooth structure leaves the root without any ferrule, conservative treatments alternative to dental extraction and implant placement, such as orthodontic or surgical extrusion, should be taken into great consideration, as described in the following chapter of this book. A surgical crown lengthening may be also performed in these cases, but with more contraindications being an esthetic anterior zone.
8.5 Parameters Influencing Restoration of Endodontically Treated Premolar Teeth
In premolars with intact crowns and only the presence of an endodontic access cavity, no fiber post nor full-crown or partial coverage is required, and the clinician can only perform a direct composite restoration to fill the occlusal cavity (Fig. 8.12). Generally speaking, the use of a liquid etchant may be suggested in a contracted access to reach the undercuts and penetrate such small spaces, given its decreased viscosity rather than acid gels. For the same reason, liquid acid can guarantee better etching in the apical region during post cementation [55]. Liquid etchants have better wettability and lower surface energy than acid gels, improving the capability of reaching the most difficult regions [55]. The use of small endodontic brushes to apply the adhesive system may be also suggested to better reach the less accessible areas [56]. Light curing of the adhesive and the deepest layers of the restoration should be extended to 40 s in cases of areas with limited direct access [57]. Furthermore, the use of a flowable resin composite to build-up the deepest layer of the restoration may be helpful to permit the clinician to move this material inside the cavity [58], thus reaching more easily the undercuts and permitting to reduce the possible inclusion of air bubbles in the material layer [59]. Flowable bulk-fill materials may be used in these cases, having the possibility to increase the thickness of each layer to 4 mm instead of the standard 2 mm [60]. A standard light-curing highly filled packable resin composite is then used for the reconstruction of the last occlusal 1.5–2 mm layer, being more easily sculptable and more resistant to wear [50].
Conservative approach in premolars. The second maxillary premolar tooth with a periapical lesion became necrotic probably for trauma (a). The absence of caries permitted a conservative access cavity and root canal treatment (b, c) and the restoration with a direct composite (d). Radiograph of the 2-year follow-up (e)
In premolar teeth with a loss of one marginal ridge, usually a fiber post and/or a full crown are not required and an adhesively cemented indirect restoration that will partially cover the cusps near the marginal ridge lost represents the solution of choice in these cases (Fig. 8.13). The decision generally is determined case by case depending on the amount of sound tooth structure, the thickness of the cusps near the marginal ridge lost, and the presence of further restorations (i.e., buccal restorations). In fact, in cases of interproximal caries-driven opportunistic access cavity with the loss of only one marginal ridge with a well-represented thickness of the dentin at the bases of the buccal and lingual cusps, normally a direct resin composite restoration without any post can be also considered (Fig. 8.14). Conversely, when an indirect restoration with a partial cuspal coverage should be more indicated for the higher loss of sound tooth structure near the marginal ridge lost and a reduced cusp thickness, but the patient cannot afford it economically, a strategical post may be used to dissipate the stresses in a better way and a direct restoration removing all the undermined tooth structure may be performed with or without the direct cuspal coverage, as a compromise from an esthetic and functional point of view, given the difficulties in modelling the occlusal surface in such big restorations. This choice may also allow the clinician to perform an indirect restoration even later.
Indirect restoration in a premolar with loss of one marginal ridge. The second maxillary premolar tooth shows a big mesial caries penetrating the pulp chamber (a). Preparation for the impression after the restoration with a fiber post (b, c). Radiographical (d) and intraoral (e) views after onlay cementation (Lab Loreti, Rome—Italy)
When a full crown is indicated in cases of only one marginal ridge lost in premolars, because of the extension of the tooth structure lost, the presence of already existing restorations in other parts of the tooth, and/or the reduced thickness of both cusps, the use of a post may be recommended to better retain the core and dissipate the stress in a more favorable way, because of the further amount of tooth structure that will be lost after circumferential tooth preparation for the full crown (Fig. 8.15).
Post and full-crown restoration in a first maxillary premolar tooth showing a significant loss of tooth structure in occlusal, mesial, and buccal area with a big old MO restoration and an extended cervical caries and an incomplete root canal treatment (a–c). After the endodontic retreatment, it was restored with a post and a full crown (Lab Loreti, Rome—Italy) (d–f). 3-year follow-up radiographical (g) and intraoral (h, i) views
Clinicians may proceed similarly when in premolars the loss of both mesial and distal marginal ridges occurs: in these cases, a fiber post may be suggestable and a complete cuspal coverage is always needed. A full crown or an overlay adhesive restoration may be performed depending on the quantity, quality, and thickness of the residual amount of tooth structure (Fig. 8.16).
In premolars with the loss of both marginal ridges together with a severe or complete loss of tooth structure, after the insertion of a post, a cuspal coverage with a full-crown restoration is the only possible choice. A surgical tooth crown lengthening (Fig. 8.17) or an orthodontic extrusion (Fig. 8.18) must be considered in these cases if there is not enough residual ferrule [61]. Crown lengthening has a significant biological cost that must be considered into the treatment decision-making process; in fact Gegauff [61] demonstrated a more favorable crown-root ratio with orthodontic extrusion than with crown lengthening that impairs tooth static load failure to a greater extent.
Surgical crown lengthening. The second maxillary premolar tooth reported a fracture of the palatal cusp that invades the periodontal support (a), requiring endodontic treatment and crown lengthening (b). 3-year follow-up radiographical (c) and intraoral (d) views. (Surgical crown lengthening Dr. Guerino Paolantoni, prosthetic rehabilitation Dr. Fabio Teodori)
Orthodontic extrusion. The second maxillary premolar tooth reported a fracture of the palatal cusp that invades the periodontal support caused by and extensive caries lesion (a, b). After endodontic treatment and post placement, orthodontic extrusion was performed in 40 days (c–e) and a full crown was chosen as final restoration (Lab Loreti, Rome—Italy) (f–h). 3-year follow-up radiograph (i). (Orthodontic extrusion Dr. Ferruccio Torsello)
Patients may not accept the orthodontic extrusion because of longer treatment time and also because sometimes after the orthodontic extrusion a crown lengthening may be necessary if the clinician does not perform the fibrotomy weekly or if the bone follows the root [62,63,64]. Even if crown lengthening is performed after orthodontic extrusion, the same crown-root ratio is maintained in a more favorable way than with crown lengthening only, but in these cases an alternative treatment such as the surgical extrusion may be also taken into consideration as reported in Chap. 9. Extraction and implant placement remain the last option, having in any case a high success rate [65].
8.6 Parameters Influencing Restoration of Endodontically Treated Molar Teeth
In molar teeth with an intact crown and an occlusal endodontic access cavity only, no fiber post nor full-crown or partial coverage restorations are needed, and the clinician can perform a direct composite restoration or eventually an indirect inlay without any cuspal coverage to fill the occlusal cavity, as already reported for premolar teeth (Fig. 8.19). The step-by-step restoration in these cases is similar to what has been already described for similar situations in anterior and premolar teeth with only an occlusal endodontic cavity.
In some cases, after the endodontic treatment both marginal ridges may be still present, but a greater extension of the caries (i.e., on the buccal-lingual surfaces) may cause a significant loss of tooth structure: a post is not needed to retain the material, but the clinician may perform an indirect onlay, with a partial cuspal coverage to better reconstruct the occlusal anatomy. Sometimes, when a big primary occlusal caries or a big old occlusal restoration with recurrent caries are present, their removal can still lead to a class I cavity, but undermining the tooth structure with a poor amount of thickness of the residual walls circumferentially. In these cases, apparently intact teeth may also present mesial and/or distal vertical cracks, especially in amalgam-filled teeth [66, 67]. Sometimes cracks penetrate inside the pulp chamber, thus requiring an endodontic treatment [68] and an overlay adhesively cemented indirect restoration with a complete cuspal coverage to prevent cracks extension (Fig. 8.20). In these cases, usually clinicians should also perform a preventive cuspidectomy at the beginning of the endodontic treatment to reduce the risk for fracture of the thin residual walls under masticatory load between the appointments. When an indirect restoration is needed, a flowable bulk-fill resin composite may be used for the core build-up and the preparation for the cuspal coverage may be performed in tooth areas that are no more sustained by dentin. The cementation of a strategical fiber post may also be taken into consideration in these cases.
Post and overlay restoration in molars. Old restoration with a big decay in the right mandibular first molar tooth (a). After the removal of the old restoration, a crack was appreciated in the cavity floor (b), that continued inside the pulp chamber and on the distal aspect (c). The tooth was endodontically treated, restored with fiber posts and an adhesively cemented lithium-disilicate ceramic overlay restoration (Lab Loreti, Rome—Italy) (d–f)
In molars with the loss of only one marginal ridge, a fiber post and a full crown are not usually needed because of the big amount of tooth structure maintained in the part of the tooth not involved in the pathology. A partial coverage of both the two cusps near the marginal ridge lost would be the ideal solution in these cases, even if a simple direct composite restoration may be performed without any cuspal coverage, depending on the amount of residual tooth structure and the thickness of the cusps near the marginal ridge lost. In fact, no post and a direct restoration can be a good solution for cases with a caries lesion penetrating the pulp, thus requiring endodontic treatment but involving only one marginal ridge, when a caries-driven conservative dynamic enlargement of the access is performed (Fig. 8.21). The stiffness of the cusps in this situation is similar to a class II cavity for the restoration of an interproximal caries, regardless that endodontic treatment is performed or not [69]. Treatment planning should be very important in these cases when the patient cannot afford a more expensive indirect restoration: performing a conservative endodontic treatment as described throughout all this book may help the clinician to perform a simple and less expensive direct resin composite class II restoration without cuspal coverage, without impairing too much the long-term outcome of these teeth. In similar cases but with a bigger loss of tooth structure, when the access is not much conservative and the thickness at the base of a cusp is less than 2 mm, a restoration can be performed also with the cementation of a strategical post and a direct partial coverage of the involved cusps (Fig. 8.22). In these cases, it may be advantageous to reduce these cusps 1.5–2 mm occlusally and restore the occlusal anatomy even with a direct restoration, thus not impairing the fracture resistance of these teeth with respect to an indirect restoration with cuspal coverage [31]. Direct restorations in these cases should be considered as an interim restoration waiting to perform a more performant indirect restoration: this is the reason of the insertion of the post. Strategical posts can be also used for prosthetic reasons after the endodontic treatment to better retain the core and avoid exposure of gutta-percha when root hemisection should be performed for periodontal reasons.
Caries-driven interproximal conservative dynamic access and direct restoration. The mesial deep extension of the caries in the lower left second molar (a) required the root canal treatment (b), but a direct restoration without post was performed because of the only one marginal ridge lost and the conservative access opening (c–m). 1-year follow-up radiographical (n) and intraoral (o, p) views
In molar teeth with the loss of both two marginal ridges, the use of a fiber post is suggestable and a complete cuspal coverage is always needed to protect the tooth from the high risk for fracture given by the reduced stiffness of the residual cusps and their higher deflection rate. As soon as both buccal and lingual walls are adequately maintained in these cases, a partial indirect adhesively cemented restoration with complete cuspal coverage (overlay) with or without the cementation of a fiber post may be the solution of choice to be conservative maintaining as much tooth structure as possible, while reducing the risk for cusp fracture (Fig. 8.23). Both a fiber post and a full-crown restoration are usually required in less conservative cases, with a massive loss of tooth structure because of big old restorations, caries, or fracture (Fig. 8.24). Surgical tooth crown lengthening should be also taken into consideration in cases of partial or complete lack of ferrule or loss of the biologic as width, but, if no ferrule is present at all, the clinician should also consider the extraction and implant placement as a predictable therapy or the surgical extrusion when ideal conditions are present for atraumatic extraction or tooth autotransplantation when an adequate donor tooth is available as described in Chap. 9.
Post and overlay restoration in molars. Mesial old restoration and distal caries under an old restoration in a mandibular first molar (a). After the endodontic therapy (b), the tooth was restored with a post (c) and prepared with cusp reduction and a build-up (e) for the cementation of a composite overlay (Lab Loreti, Rome—Italy) (f). 6-year follow-up radiographical (d) and intraoral (g) views
Post and full-crown restoration in molars. Big amount of loss of tooth structure distally and big restoration mesially in an upper left first molar (a). After a pre-endodontic build-up with a bulk-fill material, the root canal treatment and the cementation of a fiber post were performed (b) and the tooth was prepared for a full crown (c, d). A monolithic full zirconia crown (Lab Loreti, Rome—Italy) was cemented (e). 3-year follow-up radiographical (f) and intraoral (g, h) views
8.7 Restoration of Endodontically Treated Teeth with Fiber Posts
8.7.1 Basic Concepts
Restoration of root-filled teeth may be carried out with or without a post [70]. The main reason to use a post is to retain a core when there is not enough residual coronal tooth structure [5, 71]. Different types of post have been available on the market. To achieve optimum results in post restoration, the materials that should be used to restore root-filled teeth should have physical and mechanical properties similar to that of dentin; they should be able to bond to the tooth structure and should be biocompatible in the oral environment [70]. Thus, it was suggested that the modulus of elasticity of a post should be as much as similar to that of dentin for a more uniform distribution of the stress along the post length [72,73,74].
Both cast gold post-and-cores and metal preformed posts distribute the stress along the post, concentrating it at the root area around the tip of the post, with a higher risk of root fracture [75]. On the other hand, the biomechanical properties of preformed fiber-reinforced posts have been reported to be close to that of dentin in terms of elastic modulus [76, 77], so that today they may be considered the gold standard for the restoration of endodontically treated teeth. In fact, the mean value of elastic modulus of dentin (Young’s modulus) is around 15–20 GPa [77, 78], while fiber posts have registered the most similar modulus of elasticity to that of dentin, having the “white” glass fiber posts values nearer to that of dentin (24–28 GPa) [77] than “black” carbon fiber posts, that registered a little bit higher values (around 34 GPa) [77]. White fiber posts are recommended especially in esthetic areas, but today they are the most commonly used fiber posts in general [79], while in posterior teeth carbon fiber posts may be used to better withstand to the occlusal forces because they have a little bit higher modulus of elasticity. Metal posts registered much higher values of elastic modulus than fiber posts (110 GPa for stainless-steel and 65 GPa for titanium), with gold posts having the lowest value (53 GPa) among different metals, more similar to that of fiber posts [77]. For this reason, when no more ferrule is present, the only alternative to fiber posts may be the use of a gold cast post-and-core [80], but in these cases clinicians should evaluate the long-term prognosis of no-ferrule teeth and also consider the possible implant alternative [81,82,83,84].
Teeth restored using fiber posts have demonstrated a good survival rate in clinical studies, with similar performance to cast post-and-cores [85]. Even metallic posts had a good clinical survival, but the associated failures were mostly irreversible, differently from what happened with fiber posts that reported with more restorable failures [85]. This is the most important reason today for using a fiber post instead of a metallic post. Several in vitro studies also confirmed that teeth restored with non-rigid (low modulus) posts (fiber posts) showed fewer catastrophic irreversible root fractures rather than teeth restored with rigid (high modulus) posts (metal posts) [84,85,86,87]. Endodontically treated teeth restored with glass fiber posts showed an increased fracture strength and a more favorable mode of fracture and therefore the use of fiber posts was highly recommended to achieve better clinical outcomes [88, 89], with also a higher survival rate of this type of restoration and of the tooth itself [90].
Furthermore, both in vivo and in vitro studies reported that teeth restored with fiber posts showed mostly restorable fractures, while the ones restored without posts displayed unrestorable failures, both when full coverage restorations were used or not [91,92,93]. Based on this statement, the use of strategical fiber posts to dissipate the stresses and protect against failure even when they are not strictly required only to retain the core have been mentioned several times previously in the present chapter.
8.7.2 Strategical Fiber Posts
Strategical fiber posts can be thus used in several clinical situations to enhance the biomechanical behavior to better dissipate the occlusal stresses on the tooth and to reduce the risks of a possible catastrophic non-restorable mechanical failure, even when it is not mandatory for their function to retain the core. This is the case, for example, of interproximal cavities with a marginal ridge lost in which an indirect adhesive restoration should be indicated in order to partially cover the undermined cusps near the marginal ridge lost, but the patient cannot afford an indirect restoration after the endodontic treatment [94]. In this border-line situation it is important to plan the treatment since the beginning, thus aiming to be as much conservative as possible, as indicated throughout all this book, to maintain as much tooth structure that may increase the prognosis of these teeth in which a compromise will be taken in the restorative phases. Thus, the clinician may perform in these cases a direct restoration with or without the partial reduction of the two cusps near the marginal ridge lost and a fiber post may be used to improve the mechanical behavior of the tooth (Fig. 8.22). Ideally, this restorative choice should be considered as a temporary compromise restoration and should be substituted by a more effective cuspal coverage as soon as possible.
A strategical post to better dissipate the forces can be also used when indirect adhesive restorations with partial/complete cuspal coverage (onlays/overlays) are performed and its use is not mandatory to retain the core (Fig. 8.13). As the absence of a post may impair fracture resistance and increase cusp strain, depending on the remaining tooth structure [95], the strategic purpose of inserting a post is to make an eventual mechanical failure more favorable and restorable, even if it will occur after several years [92, 96]. Being a circumferential tooth preparation for a full crown, the further step of the treatment, this strategy will make the reintervention easier, because a post placement is suggestable to retain the core in most of the cases when a full crown is required, as today this type of restoration is mainly performed in teeth with a severe loss of tooth structure.
8.7.3 Minimally Invasive Procedures for the Cementation of Fiber Posts
Fiber post placement, and a strategical post in particular, may also be suggested because of the possibility to perform these procedures with the maximum conservation of tooth structure, following the minimally invasive concepts described below.
In particular, the clinician must approach the phase of post-space preparation with the maximum conservative attitude, preserving as much sound dentin as possible, through the removal of the root canal filling material only and cleaning the root canal walls without an additional enlargement of the root canal after the endodontic treatment [11]. Removing a bigger amount of the remaining radicular and coronal tooth structure after the endodontic root canal preparation to insert a post does not lead to a concrete benefit and, on the contrary, it is detrimental for the long-term prognosis [97]. Thus, the most important message is that to insert a post the clinician should not enlarge the coronal part of the root canal more than what was required to perform the endodontic treatment. For this reason, the post-space tapered drills normally suggested to be used by post manufacturer are not compatible with a conservative preparation, because they are too big and rigid and always remove more dentin than needed and over-enlarge the canal. Gates-Glidden are the most preferable and conservative burs to be used in all cases: the rule to follow is to use a bur that is smaller than the root canal diameter, just to remove the filling material and respect the apical seal, maintaining at least 4–5 mm of gutta-percha apically [98, 99]. Largo burs may be also used but they are bigger and more rigid for their longer active part. If a vertical compaction of the gutta-percha technique is used to fill the root canals and a post is needed, it may be useful not to fill back the canal or to fill it back just as much as needed to leave the correct post-space length and just chemically clean the root canal walls before cementation.
Another important topic about the conservative approach in post-space preparation is the length of the post-space in relationship with the post length. In the metal post era, the length of a post was considered important since it was directly proportional to the amount of support offered to its retention and the resistance to root fracture [100]. From this retentive standpoint, not adhesively cemented metal posts were performed as long as possible, to increase the retaining and resistance properties [11, 101, 102]. These classic concepts are not valid anymore with fiber posts thanks to the adhesive procedures and because the insertion length does not influence the biomechanical performance and the fracture resistance of endodontically treated teeth restored with fiber posts [53, 79]. Therefore, the insertion of short posts became a valid alternative in the restoration of root-filled teeth [103], as adequate retentive values are achieved even with shorter posts [104]. The advantage of shortening the length of a post with the use of fiber posts is represented by the possibility to reduce the risks connected to a post-space preparation deep inside the root and the inevitable removal of more sound tooth structure. There are several factors that may influence the post length: when a strategical post is used post length may be reduced, as the main aim is not to retain the core (Fig. 8.13); the less is the residual tooth structure present, the longer should the post be to increase the retention and the fracture resistance (Fig. 8.24); the presence of a severe canal curvature in the middle third of the root canal may result in a reduction of the ideal post length up to the beginning of the curvature, regardless of the residual coronal tooth structure, as the clinician cannot straighten the curvature and reduce tooth resistance just to increase the length of the post [70, 105] (Fig. 8.16); usually the insertion of one fiber post is enough for the restoration of endodontically treated, but in multirooted teeth with severe loss of tooth structure the use of more than one post may be suggested: the length of the additional posts may be reduced in these cases as they only have an antirotational effect to act against lateral forces and/or act as support near the most damaged tooth areas; even in cases with a great amount of coronal tooth structure, a reduced periodontal support requires a longer post, as the crown-to-root ratio in these cases may be unfavorable because of the alveolar bone loss and the center of rotation moves apically reducing the tooth resistance to lateral forces [106]. To act against lateral forces in cases of alveolar bone loss, the clinician should insert the post below the bone level near the fulcrum, despite the amount of residual tooth structure.
While the post-space preparation is the most important step to increase the resistance of the tooth, being as much minimally invasive as possible [107], the post-space cleaning and disinfection is the crucial step to increase the retention of fiber posts. In fact, the most common type of failure with fiber-reinforced composite posts is not root fracture, but debonding [108, 109]. The post-space should be chemically cleaned using 17% EDTA or 2% CHX for 1–2 min after post-space preparation to remove debris and smear layer [110]. EDTA could also enhance the performance of self-etching primers [111, 112] and CHX may increase the retention of fiber post and the long-term stability of the adhesive system [113, 114]. A mechanical cleaning is also needed while using chemicals, performing a passive or active ultrasonic activation [115, 116] and/or using manual or mechanical brushes. Hydrogen peroxide and sodium hypochlorite liquids must be avoided in this cleaning step because they may interfere with the adhesive procedures [117, 118]. Even other materials can impair adhesives polymerization, for example, if the endodontic treatment and post placement are scheduled in the same visit, eugenol-based root canal sealers should be avoided [119], while bioceramic and resin-based root canal sealers are suggested. When bleaching is performed, adhesively cemented fiber post should also be performed at least 7–14 days after bleaching to reduce influence of peroxides generated by the bleaching agent on the adhesive procedures [48]. To increase retention of the fiber posts, posts with surface treatments made by the manufacturer should be selected to increase surface roughness and improve the surface area available for adhesion [120] and create a surface layer that may increase the bond strength of the composite resin to the fiber post [121, 122].
The shape of the post is also important in a minimally invasive restorative concept, as cylindrical fiber posts with parallel walls requests a less conservative preparation in the apical portion of the post-space removing sound dentin [123]. For this reason, a conical post with the same coronal taper of the last endodontic mechanical file used for the preparation of the root canal is the best choice possible to respect the original canal anatomy and do not further remove sound tooth structure important for its resistance. Furthermore, there was no statistical difference in the retention between tapered and parallel-sided posts when they were cemented with the same resin cement [104].
Following the concept that the post should be as similar as the residual canal after the endodontic treatment without further removal of tooth structure and that it must be the post to be adapted to the existing canal anatomy and not the canal to be adapted to the post, the golden rule to be followed in the choice of the correct tapered fiber post size should be that the biggest possible post that passively adapt to the root canal at the correct chosen length, without any friction on the walls and without any additional root canal enlargement is the correct post for that root canal. Usually, if the minimally invasive concepts described in this book will be followed, a very small post will be needed, but this will not affect the biomechanical performance of teeth restored with glass fiber posts to a significant degree [79].
It may be difficult to follow these concepts when the coronal portion of the canal is oval and a single circular preformed post should be inserted in a noncircular root canal. More than one post may be used in the same canal to fill the remaining space, reduce the amount of cement and contrast the C-factor during the polymerization, and increase the resistance of the tooth-restoration complex [124]. When using more posts, the amount of sealer is reduced, but a one-piece oval post would be even better to also increase its mechanical properties. For this reason, a minimally invasive technique to create anatomical fiber posts have been introduced [125] to reduce the amount of surrounding cement, thus reducing air bubble inclusion during cementation, distribute it in a regular thickness that may increase the retention of the post, while having a single piece of fiber-reinforced composite post that may increase the mechanical proprieties of the post and the tooth-post complex [77, 126, 127].
Once cemented, the fiber post should not be exposed to the oral environment for long time because humidity can alter the mechanical properties of fiber posts [128], so it is suggestable to always completely cover the post by the build-up material.
8.8 Conclusive Remarks
The survival of an endodontically treated tooth is dependent primarily on the amount of residual tooth structure. For this reason, over the last years all the efforts in endodontics and restorative dentistry have been directed toward a paradigm shift from the traditional rules to a more conservative and minimally invasive approach. The “golden rule” is now to preserve as much tooth structure as possible in all the procedures: from the access cavity preparation to the choice of the type of coronal restoration. The technical evolution has led to important changes in the clinical management of endodontically treated teeth, because new instruments, materials, and techniques have been introduced. In this perspective, the introduction of heat-treated NiTi alloys and new trends in access cavity opening has represented a conservative revolution in endodontics, such as the introduction of fiber-reinforcement for post fabrication has guaranteed a safer stress distribution and a higher preservation of sound intracanal dentin in post-space preparation than with the stiffer and wider metallic posts [129].
Despite all the innovations, a deep knowledge of occlusion still remains crucial to guide the clinician in a correct management of coronal restoration: direct composite, cusp reduction with an indirect restoration (onlay or overlay) and full crown are the treating options that the clinician can perform always taking into account both the amount and quality of the residual coronal tooth structure. In most destructive decays, even periodontal health must be considered, because usually a biological width violation may occur in these cases [130]. A particular concern should be reserved for crown-root ratio, and orthodontic extrusion and surgical crown lengthening can be performed to provide a favorable ferrule effect and improve biomechanical behavior of the restored tooth [131].
On the basis of these concepts it can be concluded that, before starting an endodontic treatment, the clinician should always keep in mind the final result of this procedure that must involve its restoration and the need to put the tooth in function again.
References
Fedorowicz Z, Carter B, de Souza RF, de Andrade Lima Chaves C, Nasser M, Sequeira-Byron P. Single crowns versus conventional fillings for the restoration of root filled teeth. Cochrane Database Syst Rev. 2012;5:CD009109.
Helfer AR, Melnick S, Schilder H. Determination of the moisture content of vital and pulpless teeth. Oral Surg Oral Med Oral Pathol. 1972;34:661–70.
Loewenstein WR, Rathkarnp R. A study on the pressoreceptive sensibility of the tooth. J Dent Res. 1955;34:287–94.
Randow K, Glantz PO. On cantilever loading of vital and non-vital teeth: an experimental clinical study. Acta Odontol Scand. 1986;44:271.
Gutmann JL. The dentin-root complex: anatomic and biologic considerations in restoring endodontically treated teeth. J Prosthet Dent. 1992;67:458–67.
Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18:332–5.
Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512–6.
Reeh ES, Douglas WH, Messer HH. Stiffness of endodontically-treated teeth related to restoration technique. J Dent Res. 1989;68:1540–4.
Panitvisai P, Messer HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod. 1995;21:57–61.
Taha NA, Palamara JE, Messer HH. Cuspal deflection, strain and microleakage of endodontically treated premolar teeth restored with direct resin composites. J Dent. 2009;37:724–30.
Stankiewicz NR, Wilson PR. The ferrule effect: a literature review. Int Endod J. 2002;35:575–81.
Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. Ferrule effect: a literature review. J Endod. 2012;38:11–9.
Gutmann JL. Minimally invasive dentistry (Endodontics). J Conserv Dent. 2013;16:282–3.
Riitano F. La Tecnica Tre Tempi. Dental Cadmos. 1976;4:10–7.
Ruddle CJ. Current concepts for preparing the root canal system. Dent Today. 2001;20:76–83.
Ruddle CJ. Cleaning and shaping root canal systems. In: Cohen S, Burns RC, editors. Pathways of the pulp. 8th ed. St. Louis, MO: Mosby; 2002. p. 231–91.
Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, Gambarini G, Testarelli L. Fracture strength of endodontically treated teeth with different access cavity designs. J Endod. 2017;43:995–1000.
Clark D, Kadhemi J. Modern molar endodontic access and directed dentin conservation. Dent Clin N Am. 2010;54:249–73.
Shen Y, Zhou HM, Zheng YF, Peng B, Haapasalo M. Current challenges and concepts of the thermomechanical treatment of nickel-titanium instruments. J Endod. 2013;39:163–72.
Wilson NHF. Minimally invasive dentistry—the management of caries. London: Quintessence Publishing Co.; 2007.
Kidd E. Clinical threshold for caries removal. Dent Clin N Am. 2010;54:541–9.
Sabbagh J, McConnell RJ, McConnell MC. Posterior composites: update on cavities and filling techniques. J Dent. 2017;57:86–90.
Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford TR. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J Prosthet Dent. 2002;88:297–301.
Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent. 2005;93:164–70.
Sorensen JA, Martinoff JT. Intracornal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent. 1984;51:780–4.
Sorensen JA, Martinoff JT. Clinically significant factors in dowel design. J Prosthet Dent. 1984;52:28–35.
Goodacre CJ, Spolnik KJ. The prosthodontic management of endodontically treated teeth: a literature review. Part I. Success and failure data, treatment concepts. J Prosthodont. 1994;3:243–50.
Seow LL, Toh CG, Wilson NH. Remaining tooth structure associated with various preparation designs for the endodontically treated maxillary second premolar. Eur J Prosthodont Restor Dent. 2005;13:57–64.
Veneziani M. Posterior indirect adhesive restorations: updated indications and the Morphology Driven Preparation Technique. Int J Esthet Dent. 2017;12:204–30.
Jackson RD. Indirect resin inlay and onlay restorations: a comprehensive clinical overview. Pract Periodontics Aesthet Dent. 1999;11:891–900.
Plotino G, Buono L, Grande NM, Lamorgese V, Somma F. Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J Prosthet Dent. 2008;99:225–32.
Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Top. 2006;13:57–83.
Sorrentino R, Monticelli F, Goracci C, Zarone F, Tay FR, García-Godoy F, Ferrari M. Effect of post-retained composite restorations and amount of coronal residual structure on the fracture resistance of endodontically-treated teeth. Am J Dent. 2007;20:269–74.
Zhu Z, Dong XY, He S, Pan X, Tang L. Effect of post placement on the restoration of endodontically treated teeth: a systematic review. Int J Prosthodont. 2015;28:475–83.
Salameh Z, Sorrentino R, Papacchini F, Ounsi HF, Tashkandi E, Goracci C, Ferrari M. Fracture resistance and failure patterns of endodontically treated mandibular molars restored using resin composite with or without translucent glass fiber posts. J Endod. 2006;32:752–5.
Magne P, Harrington D, Harrington S. Semi-direct techniques. Chapter III. In: Esthetic and biomimetic restorative dentistry. Manual for posterior esthetic restorations. St. Louis (MO): Elsevier Mosby; 2005. p. 44–59.
Deliperi S, Bardwell DN. Multiple cuspal-coverage direct composite restorations: functional and esthetic guidelines. J Esthet Restor Dent. 2008;20:300–12.
Scotti N, Rota R, Scansetti M, Paolino DS, Chiandussi G, Pasqualini D, Berutti E. Influence of adhesive techniques on fracture resistance of endodontically treated premolars with various residual wall thicknesses. J Prosthet Dent. 2013;110:376–82.
Leprince JG, Leloup G, Hardy CMF. Considerations for the restoration of endodontically treated molars. In: The guidebook to molar endodontics. Berlin Heidelberg: Springer-Verlag; 2017. p. 169–205.
Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63:529–36.
Stankiewicz N, Wilson P. The ferrule effect. Dent Update. 2008;35:222–4.
Jotkowitz A, Samet N. Rethinking ferrule—a new approach to an old dilemma. Br Dent J. 2010;209:25–33.
Tjan AH, Whang SB. Resistance to root fracture of dowel channels with various thicknesses of buccal dentin walls. J Prosthet Dent. 1985;53:496–500.
Ng CC, Dumbrigue HB, Al-Bayat MI, Griggs JA, Wakefield CW. Influence of remaining coronal tooth structure location on the fracture resistance of restored endodontically treated anterior teeth. J Prosthet Dent. 2006;95:290–6.
Morgano S. Restoration of pulpless teeth: application of traditional principles in present and future contexts. J Prosthet Dent. 1996;75:375–80.
Ahmed HMA, Abbott PV. Discolouration potential of endodontic procedures and materials: a review. Int Endod J. 2012;45:883–97.
Ioannidis K, Beltes P, Lambrianidis T, Kapagiannidis D, Karagiannis V. Crown discoloration induced by endodontic sealers: spectrophotometric measurement of Commission International de I’Eclairage’s L∗, a∗, b∗ chromatic parameters. Oper Dent. 2013;38:E1–12.
Plotino G, Buono L, Grande NM, Pameijer CH, Somma F. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008;34:394–407.
Del Curto F, Rocca GT, Krejci I. Restoration of discolored endodontically treated anterior teeth: a minimally invasive chemomechanical approach. Int J Esthet Dent. 2018;13:302–17.
Ferraris F, Diamantopoulou S, Acunzo R, Alcidi R. Influence of enamel composite thickness on value, chroma and translucency of a high and a non-high refractive index resin composite. Int J Esthet Dent. 2014;9:382–401.
Jang P, Hwang I, Hwang IN. Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent. 2015;40:172–80.
Salameh Z, Ounsi HF, Aboushelib MN, Sadig W, Ferrari M. Fracture resistance and failure patterns of endodontically treated mandibular molars with and without glass fiber post in combination with a zirconia-ceramic crown. J Dent. 2008;36:513–9.
Borelli B, Sorrentino R, Zarone F, Ferrari M. Effect of the length of glass fiber posts on the fracture resistance of restored maxillary central incisors. Am J Dent. 2012;25:79–83.
Kumagai H, Suzuki T, Hamada T, Sondang P, Fujitani M, Nikawa H. Occlusal force distribution on the dental arch during various levels of clenching. J Oral Rehabil. 1999;26:932–5.
Salas MM, Bocangel JS, Henn S, Pereira-Cenci T, Cenci MS, Piva E, Demarco FF. Can viscosity of acid etchant influence the adhesion of fibre posts to root canal dentine? Int Endod J. 2011;44:1034–40.
Ferrari M, Vichi A, Grandini S, Geppi S. Influence of microbrush on efficacy of bonding into root canals. Am J Dent. 2002;15:227–31.
Akram S, Ali Abidi SY, Ahmed S, Meo AA, Qazi FU. Effect of different irradiation times on microhardness and depth of cure of a nanocomposite resin. J Coll Physicians Surg Pak. 2011;21:411–4.
Lokhande NA, Padmai AS, Rathore VP, Shingane S, Jayashankar DA, Sharma U. Effectiveness of flowable resin composite in reducing microleakage - an in vitro study. J Int Oral Health. 2014;6:111–4.
Baroudi K, Rodrigues JC. Flowable resin composites: a systematic review and clinical considerations. J Clin Diagn Res. 2015;9:ZE18–24.
Benetti AR, Havndrup-Pedersen C, Honoré D, Pedersen MK, Pallesen U. Bulk-fill resin composites: polymerization contraction, depth of cure, and gap formation. Oper Dent. 2015;40:190–200.
Gegauff AG. Effect of crown lengthening and ferrule placement on static load failure of cemented cast post-cores and crowns. J Prosthet Dent. 2000;84:169–79.
Potashnick SR, Rosenberg ES. Forced eruption: principles in periodontics and restorative dentistry. J Prosthet Dent. 1982;48:141–8.
Pontoriero R, Celenza F Jr, Ricci G, Carnevale G. Rapid extrusion with fiber resection: a combined orthodontic-periodontic treatment modality. Int J Periodontics Restorative Dent. 1987;7:30–43.
Kozlovsky A, Tal H, Lieberman M. Forced eruption combined with gingival fiberotomy. A technique for clinical crown lengthening. J Clin Periodontol. 1988;15:534–8.
Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80:476–91.
Seo D-G, Yi Y-A, Shin S-J, Park J-W. Analysis of factors associated with cracked teeth. J Endod. 2012;38:288–92.
Danley BT, Hamilton BN, Tantbirojn D, Goldstein RE, Versluis A. Cuspal flexure and stress in restored teeth caused by amalgam expansion. Oper Dent. 2018;43:300–7.
PradeepKumar AR, Arunajatesan S. Cracks and fractures in teeth. Restor Dent Endod. 2017;2:25–30.
Burke FJ. Tooth fracture in vivo and in vitro. J Dent. 1992;20:131–9.
Fernandes AS, Shetty S, Coutinho I. Factors determining post selection: a literature review. J Prosthet Dent. 2003;90:556–62.
Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 1994;71:565–7.
Grandini S, Goracci C, Tay FR, Grandini R, Ferrari M. Clinical evaluation of the use of fiber posts and direct resin restorations for endodontically treated teeth. Int J Prosthodont. 2005;18:399–404.
Naumann M, Sterzenbac G, Alexandra F, Dietrich T. Randomized controlled clinical pilot trial of titanium vs. glass fiber prefabricated posts: preliminary results after up to 3 years. Int J Prosthodont. 2007;20:499–503.
Al-Omiri MK, Rayyan MR, Abu-Hammad O. Stress analysis of endodontically treated teeth restored with post-retained crowns: a finite element analysis study. J Am Dent Assoc. 2011;142:289–300.
Martínez-Insua A, da Silva L, Rilo B, Santana U. Comparison of the fracture resistances of pulpless teeth restored with a cast post and core or carbon-fiber post with a composite core. J Prosthet Dent. 1998;80:527–32.
Duret B, Reynaud M, Duret F. Un nouveau concept de reconstitution corono-radiculaire: le composipost. Chir Dent France. 1990;60:131–41.
Plotino G, Grande NM, Bedini R, Pameijer CH, Somma F. Flexural properties of endodontic posts and human root dentin. Dent Mater. 2007;23:1129–35.
Kinney JH, Marshall SJ, Marshall GW. The mechanical properties of human dentin: a critical review and re-evaluation of the dental literature. Crit Rev Oral Biol Med. 2003;14:13–29.
Rodríguez-Cervantes PJ, Sancho-Bru JL, Barjau-Escribano A, Forner-Navarro L, Pérez-González A, Sánchez-Marín FT. Influence of prefabricated post dimensions on restored maxillary central incisors. J Oral Rehabil. 2007;34:141–52.
Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NHJ. Up to 17-year controlled clinical study on post-and-cores and covering crowns. J Dent. 2007;35:778–86.
Iqbal MK, Kim S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J Endod. 2008;34:519–29.
Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J. 2009;42:757–74.
Soares CJ, Valdivia AD, da Silva GR, Santana FR, Menezes Mde S. Longitudinal clinical evaluation of post systems: a literature review. Braz Dent J. 2012;23:135–40.
Asmussen E, Peutzfeldt A, Heitmann T. Stiffness, elastic limit, and strength of newer types of endodontic posts. J Dent. 1999;27:275–8.
Mannocci F, Sherriff M, Watson TF. Three-point bending test of fiber posts. J Endod. 2001;27:758–61.
Drummond JL, Bapna MS. Static and cyclic loading of fiber-reinforced dental resin. Dent Mater. 2003;19:226–31.
Lassila LV, Tanner J, Le Bell AM, Narva K, Vallittu PK. Flexural properties of fiber reinforced root canal posts. Dent Mater. 2004;20:29–36.
Ferrari M, Cadigiaco MC, Goracci C, Vichi A, Mason PN, Radovic I, Tay F. Long-term retrospective study of the clinical performance of fiber posts. Am J Dent. 2007;20:287–91.
Jindal S, Jindal R, Mahajan S, Dua R, Jain N, Sharma S. In vitro evaluation of the effect of post system and length on the fracture resistance of endodontically treated human anterior teeth. Clin Oral Investig. 2012;16:1627–33.
Signore A, Benedicenti S, Kaitsas V, Barone M, Angiero F, Ravera G. Long-term survival of endodontically treated, maxillary anterior teeth restored with either tapered or parallel-sided glass-fiber posts and full-ceramic crown coverage. J Dent. 2009;37:115–21.
Salameh Z, Sorrentino R, Ounsi HF, Goracci C, Tashkandi E, Tay FR, Ferrari M. Effect of different all-ceramic crown system on fracture resistance and failure pattern of endodontically treated maxillary premolars restored with and without glass fiber posts. J Endod. 2007;33:848–51.
Salameh Z, Sorrentino R, Ounsi HF, Sadig W, Atiyeh F, Ferrari M. The effect of different full-coverage crown systems on fracture resistance and failure pattern of endodontically treated maxillary incisors restored with and without glass fiber posts. J Endod. 2008;34:842–6.
Sherfudhin H, Hobeich J, Carvalho CA, Aboushelib MN, Sadig W, Salameh Z. Effect of different ferrule designs on the fracture resistance and failure pattern of endodontically treated teeth restored with fiber posts and all-ceramic crowns. J Appl Oral Sci. 2011;19:28–33.
Hurst D. Indirect or direct restorations for heavily restored posterior adult teeth? Evid Based Dent. 2010;11:116–7.
Santana FR, Castro CG, Simamoto-Jùnior PC, Soares PV, Quagliatto PS, Estrela C, Soares CJ. Influence of post system and remaining coronal tooth tissue on biomechanical behavior of root filled molar teeth. Int Endod J. 2011;44:386–94.
Hitz T, Ozcan M, Göhring TN. Marginal adaptation and fracture resistance of root-canal treated mandibular molars with intracoronal restorations: effect of thermocycling and mechanical loading. J Adhes Dent. 2010;12:279–86.
Pilo R, Tamse A. Residual dentin thickness in mandibular premolars prepared with gates glidden and ParaPost drills. J Prosthet Dent. 2000;83:617–23.
Mattison GD, Delivanis PD, Thacker RW Jr, Hassel KJ. Effect of post preparation on the apical seal. J Prothet Dent. 1984;51:785–9.
Kvist T, Rydin E, Reit C. The relative frequency of periapical lesions in teeth with root canal-retained posts. J Endod. 1989;15:578–80.
De Sort KD. The prosthodontic use of endodontically treated teeth: theory and biomechanics of post preparation. J Prosthet Dent. 1983;49:203–6.
Standlee JP, Caputo AA, Hanson EC. Retention of endodontic dowels: effects of cement, dowel length, diameter, and design. J Prosthet Dent. 1978;39:400–5.
Macedo VC, Faria e Silva AL, Martins LR. Effect of cement type, relining procedure, and length of cementation on pull-out bond strength of fiber posts. J Endod. 2010;36:1543–6.
Scotti N, Scansetti M, Rota R, Pera F, Pasqualini D, Berutti E. The effect of the post length and cusp coverage on the cycling and static load of endodontically treated maxillary premolars. Clin Oral Investig. 2011;15:923–9.
Borer RE, Britto LR, Haddix JE. Effect of dowel length on the retention of 2 different prefabricated posts. Quintessence Int. 2007;38:e164–8.
Nissan J, Dmitry Y, Assif D. The use of reinforced composite resin cementas compensation for reduced post length. J Prosthet Dent. 2001;86:304–8.
Grossmann Y, Sadan A. The prosthodontic concept of crown-to-root ratio: a review of the literature. J Prosthet Dent. 2005;93:559–62.
Büttel L, Krastl G, Lorch H, Naumann M, Zitzmann NU, Weiger R. Influence of post fit and post length on fracture resistance. Int Endod J. 2009;42:47–53.
Cagidiaco MC, Goracci C, Garcia-Godoy F, Ferrari M. Clinical studies of fiber posts: a literature review. Int J Prosthodont. 2008;21:328–36.
Ferrari M, Vichi A, Fadda GM, Cagidiaco MC, Tay FR, Breschi L, Polimeni A, Goracci C. A randomized controlled trial of endodontically treated and restored premolars. J Dent Res. 2012;91:72S–8S.
Zehnder M. Root canal irrigants. J Endod. 2006;32:389–98.
Guerisoli DM, Marchesan MA, Walmsley AD, Lumley PJ, Pecora JD. Evaluation of smear layer removal by EDTAC and sodium hypochlorite with ultrasonic agitation. Int Endod J. 2002;35:418–21.
Zhang L, Huang L, Xiong Y, Fang M, Chen JH, Ferrari M. Effect of post-space treatment on retention of fiber posts in different root regions using two self-etching systems. Eur J Oral Sci. 2008;116:280–6.
da Silva RS, de Almeida Antunes RP, Ferraz CC, Orsi IA. The effect of the use of 2% chlorhexidine gel in post-space preparation on carbon fiber post retention. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:372–7.
Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine in endodontics. Int Endod J. 2009;42:288–302.
Serafino C, Gallina G, Cumbo E, Monticelli F, Goracci C, Ferrari M. Ultrasound effects after post space preparation: an SEM study. J Endod. 2006;32:549–52.
Plotino G, Pameijer CH, Grande NM, Somma F. Ultrasonics in endodontics: a review of the literature. J Endod. 2007;33:81–95.
Morris MD, Lee KW, Agee KA, Bouillaguet S, Pashley DH. Effects of sodium hypochlorite and RC-prep on bond strengths of resin cement to endodontic surfaces. J Endod. 2001;27:753–7.
Erdemir A, Ari H, Güngüneş H, Belli S. Effect of medications for root canal treatment on bonding to root canal dentin. J Endod. 2004;30:113–6.
Linard GL, Davies EH, von Fraunhofer JA. The interaction between lining materials and composite resin restorative materials. J Oral Rehabil. 1981;8:121–9.
Monticelli F, Osorio R, Sadek FT, Radovic I, Toledano M, Ferrari M. Surface treatments for improving bond strength to prefabricated fiber posts: a literature review. Oper Dent. 2008;33:346–55.
Magni E, Mazzitelli C, Papacchini F, Radovic I, Goracci C, Coniglio I, Ferrari M. Adhesion between fiber posts and resin luting agents: a microtensile bond strength test and an SEM investigation following different treatments of the post surface. J Adhes Dent. 2007;9:195–202.
Rathke A, Haj-Omer D, Muche R, Haller B. Effectiveness of bonding fiber posts to root canals and composite core build-ups. Eur J Oral Sci. 2009;117:604–10.
Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont. 2001;14:355–63.
Haralur SB, Al Ahmari MA, AlQarni SA, Althobati MK. The effect of intraradicular multiple fiber and cast posts on the fracture resistance of endodontically treated teeth with wide root canals. Biomed Res Int. 2018;1:1–6.
Grande NM, Butti A, Plotino G, Somma F. Adapting fiber-reinforced composite root canal posts for use in noncircular-shaped canals. Pract Proced Aesthet Dent. 2006;18:593–9.
Plotino G, Grande NM, Pameijer CH, Somma F. Influence of surface remodelling using burs on the macro and micro surface morphology of anatomically formed fibre posts. Int Endod J. 2008;41:345–55.
Grande NM, Plotino G, Ioppolo P, Bedini R, Pameijer CH, Somma F. The effect of custom adaptation and span-diameter ratio on the flexural properties of fiber-reinforced composite posts. J Dent. 2009;37:383–9.
Vichi A, Vano M, Ferrari M. The effect of different storage conditions and duration on the fracture strength of three types of translucent fiber posts. Dent Mater. 2008;24:832–8.
Sterzenbach G, Franke A, Naumann M. Rigid versus flexible dentine-like endodontic posts—clinical testing of a biomechanical concept: seven-year results of a randomized controlled clinical pilot trial on endodontically treated abutment teeth with severe hard tissue loss. J Endod. 2012;38:1557–63.
Schmidt JC, Sahrmann P, Weiger R, Schmidlin PR, Walter C. Biologic width dimensions—a systematic review. J Clin Periodontol. 2013;40:493–504.
Mamoun JS. On the ferrule effect and the biomechanical stability of teeth restored with cores, posts, and crowns. Eur J Dent. 2014;8:281–6.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Plotino, G., Turchi, M. (2021). Strategies for the Restoration of Minimally Invasive Endodontically Treated Teeth. In: Plotino, G. (eds) Minimally Invasive Approaches in Endodontic Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-45866-9_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-45866-9_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45865-2
Online ISBN: 978-3-030-45866-9
eBook Packages: MedicineMedicine (R0)