Abstract
The concept of eHealth refers to the use of information and communications technology (ICT) in health. The tools used to achieve this are referred to as eHealth solutions. In light of ambitious internationally agreed targets and declarations, such as the sustainable developments goals (SDGs) and other health-related SDGs, as well as external shocks, such as pandemics or population aging, public health systems worldwide face the challenge of increasing pressures and demands. At the center of these aspirations is universal health coverage, underscored by a number of declarations agreed upon by a number of governments such as the Astana declaration on primary health care. eHealth has been seen as an accelerator to attain these internally agreed aspirations, and to strengthen health systems at the national level. However, systemic and programmatic considerations need serious attention in order to fast track progress made in the past decade regarding the production and use of eHealth solutions. This chapter presents a synopsis of public health eHealth solutions in global health, within the context of health system strengthening, universal health coverage, and person-centric health services. More importantly, for eHealth solutions to deliver value propositions and better health outcomes, there will be a need to strengthen international collaborations on eHealth solutions, interoperability, data protection, regulations, health workforce capacity building, infrastructure, and horizontal financing for eHealth by donors at national level as well as best practice promotion of governance models across all levels.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
eHealth is defined by the World Health Organization (WHO) and the International Telecommunication Union (ITU) as the use of information and communication technologies for health (WHO 2020a; ITU 2020a). eHealth solutions are the tools by which eHealth is implemented (WHO 2016). The WHO has over the years introduced various resolutions and instruments to support the production, use, coordination, management, and evaluation of eHealth solutions (WHO – ITU 2013; WHO AFRO 2020a; WHO 2020b). A pivotal tool that has been used over the years to promote eHealth solutions is the WHO – ITU national eHealth toolkit (WHO – ITU 2013). The toolkit recognizes that to be successful, eHealth solutions much respond to global and national health needs as articulated in various international and national development goals. It proposes an eHealth vision, an action plan with seven pillars (which are leadership and governance, strategy and investment, services and eHealth solutions, standards and interoperability, infrastructure, health workforce capacity building, and eHealth regulations), and a monitoring and evaluation plan (ibid.). The national eHealth toolkit pillars have been strengthened by supportive instruments such as the principles of digital development that provide living guidelines to foster successful eHealth solutions development (Digital Impact Alliance 2020). These principles speak to the development of eHealth solutions with regard to designing electronic solutions with the end user; understanding the existing health ecosystem; designing solutions for scale; building solutions for sustainability; using data as a driving force; use open standards, open data, open source, and open Innovation as much as possible; reusing and improving what has worked; addressing privacy and security aspects of solution introduction; and fostering a collaborative spirit among actors in the eHealth echo system.
While there have been sufficient instruments to govern the production of eHealth solutions, significant systemic and programmatic challenges have hampered the needed progress in the uptake of eHealth solutions. These have included verticalization of eHealth solutions, lack of updated standards to enable semantic interoperability, high costs of maintenance, and unscalable pilots (McCann 2020; Fei Huang 2017). Various governments have struggled to keep up with the pressures arising from various programme based non standards based eHealth solutions. This has brought challenges in health workforce capacity building, financing for eHealth solutions, and continuity of care.
eHealth solutions have been both complex and diverse. They have included telemedicine, electronic health records, electronic learning systems, mobile health systems, data aggregation tools, social media applications, geographic information systems, ICT-enabled medical devices, laboratory, and supply chain information systems (WHO 2016). There have been renewed efforts on primary health care and patient cantered health care. This has been exemplified by the health for all agenda promoted through the SDGs and universal health coverage. The Astana declaration offers a window of opportunity for eHealth solutions. eHealth solutions have the potential to accelerate these global public health targets if deployed in a systematic and holistic manner, thereby ensuring that no one is left behind.
eHealth Solutions and the Public Health Agenda
The need for robust health-care services promoting health and well-being for all has been a subject of international interest. Several approaches have been undertaken to foster good health for all, with sustainable development goal number 3 (SDG3) aspiring to ensure healthy lives and promoting the well-being for all at all ages (UN 2020). A critical pillar of SDG3 is the attainment of universal health coverage (UHC), whose aim is to ensure that all people of all ages have access to health services of the highest quality, and that the people served are safeguarded from public health risks, including protection from impoverishment due to illness, catastrophic health expenditures, and loss of income when a household member falls sick (The World Bank 2020). This has been underscored in recent times through the declaration of Astana on primary health care (PHC), where participating heads of state and government, ministers and representatives of states and governments, at the global conference on primary health care in 2018, reaffirmed earlier visionary commitments expressed in the 1978 Alma-Ata declaration on primary health care, and the need to harness innovative approaches including the use of information and communications technologies to strengthen primary health care and UHC (WHO 2018).
While some countries have attained UHC and shown the benefits thereof, many health-care systems continue to face increasing inefficiencies and rising costs of maintenance, creating inequities and inequalities in health services provision, and disadvantaging the marginalized and poor communities (Rashid and Bashshur 2009). Health-care programs and systems have in recent times experienced increased stresses, challenges, and demands, such as increased health service demands, shortage of health-care staff, erratic supply chain, various epidemics, and aging populations (Velez-Lapão 2019). This has in recent times been more apparent with global epidemics and pandemics such as the Ebola epidemic (WHO 2020c) and the CIVID-19 pandemic (HHS 2020). At the center of these challenges is the ability to establish robust and resilient health systems capable of withstanding external shocks and changing patient demographics. The key drivers of the increasing health costs have been related to repeated redundant medical tests, medical errors, and overstocking of supplies.
ICTs in Public Health
It has been advocated that in order to mitigate health systems challenges, as well as establishing reliable and high quality data for patient care and decision-making, information and communication technology (ICT) systems can play a critical role to change the health landscape. Such ICT systems and tools have in recent times been a subject of focus and interest owing to the growing ubiquitous nature of these systems among health seekers, and their ability to reduce medical errors which improves patient safety, minimizes repeated medical tests, and provides automated decision support. These ICT systems improve health outcomes and automated data analytics thereby improving visibility into health insights and improving public health intelligence. (Rashid and Bashshur 2009). ICT systems used for a particular purpose are collectively referred to as solutions, borrowing from the early business process problems for which the ICT systems became alleviating solutions (Mark and Siska 2011). These solutions themselves are generally made up of computer programs collectively referred to as computer software. When applied to the health context, these computer-based systems assume the term “electronic health,” or as is more common the case, “eHealth.”
The Rise of eHealth in Public Health
The term eHealth has been used to characterize health services enabled or powered by the use of ICTs. The WHO has rightly and succinctly defined this area of work as “the use of information and communication technologies for health.” (WHO 2020a). This compact definition includes several aspects of health areas impacted by ICTs. As such, the International Telecommunications Union (ITU), citing the WHO’s resolution on eHealth, describes eHealth as “the cost-effective and secure use of information and communications technologies in support of health and health-related fields, including health-care services, health surveillance, health literature, and health education, knowledge and research...” (ITU 2020a; WHO 2020a). eHealth has been seen as one of the tools to mitigate national and global health challenges, in pursuit of health and well-being for all.
Good health and well-being have been a major emphasis of nations worldwide. The World health organization, founded on 7 April 1948 (WHO 2020d) and set up as a leading agency in the United Nations (UN) family on global health matters, has in recent times reaffirmed its commitment to ensuring that all people attain the highest possible level of health, promotion of health, keeping the world safe and serving the vulnerable (WHO 2020e). In keeping cadence with global development goals, this commitment has been propagated through the sustainable development goals (SDGs), and more specifically SDG3, which promises health for all in tune with the WHO mission. SDG3, which curries the spirit of universal health coverage (UHC) is a major focus area for the health sector. The WHO Thirteenth General Programme of work (GPW13) serves as a strategic instrument to integrate and focus global health. It strives to accelerate SDG3, in particular universal health coverage, with an aspiration of reaching one billion more people to benefit from universal health coverage, One billion more people better protected from health emergencies and One billion more people enjoying better health and well-being (WHO 2020f).
The Evolution of eHealth
The evolution of eHealth can be traced to the late 1999 (Mea 2001). The field was generally referred to as health informatics or more generally as telemedicine (ibid.). In 2005, the World Health Organization formerly resolved to define the field as described above, setting the ground for monitoring eHealth solutions in multiple dimensions based on a national strategy, which consists of a vision, action plan, and framework for monitoring and evaluation (WHO 2020g).
True to the nature of evolutions in both ICT and innovation, key drivers of eHealth, eHealth has grown over the years, taking a new form referred to in recent times as digital health, moving further the spirit of eHealth in tune with the ever-evolving nature of ICTs. Digital health has augmented eHealth and extended it to include the application to health, frontier technologies such as mobile health (mHealth), artificial intelligence, block chain, wearable devices, personalized medicine, drones, augmented reality, virtual reality, machine learning, and more (FDA 2020; WHO 2020h).
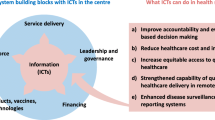
Today, eHealth solutions have been used to support drivers of health care including preventive, promotive, and curative health-care services by automating data collection, collation, storage, processing, communication, and connecting the health-care system (Giedrius Vanagas 2018). As enablers of health care, these solutions are better implemented to support the overall health system – service delivery systems, health workforce capabilities, Health Information Systems strengthening, improving access to essential medicines, strengthened financing systems, enabled leadership and governance mechanisms, all leading to improved health-care outcomes, health-care system responsiveness, resilience, improved social and financial protection, and overall health-care provision efficiency (WHO 2010). eHealth solutions have continued to evolve as ICT technology evolves. They have been classified in a number of ways including by what they do and by the function they perform. Several examples of these solutions exit. The WHO ITU national eHealth toolkit (WHO – ITU 2013) provides the following definitions and examples of eHealth, some of whose global penetration are measured by the WHO global observatory on eHealth (WHO 2020i).
Box: Definitions & Examples of eHealth Sources (WHO – ITU 2013)
Electronic Medical Records (EMRs)
An EMR is a computerized medical record used to capture, store, and share information between health-care providers in an organization, supporting the delivery of health services to patients. EMR systems may stand alone or may be integrated with other information systems in a health services organization. They function as the legal record created during the provision of care to the patient.
Electronic Health Records (EHRs)
An EHR is a computerized health record used to capture, store, access, and share summary information for a patient between health care organizations and providers. Examples of information include demographics, medical history, medication and allergies, immunizations, discharge summaries, and other summary information. Typically, EHRs are developed to support the provision of care across health sector or geographical boundaries. They may also be used by individuals and their caregivers to take a more active role in the management of their own health.
Personal Health Records (PHRs)
A PHR is a computerized health record created and maintained by an individual who is proactive in the management of her or his own health. The record can be private or made available to health-care providers. PHRs can store a diverse range of information such as an individual’s allergies, adverse drug reactions, chronic diseases, family history, illnesses and hospitalizations, medications, diet and exercise plans, and test results.
Telemedicine (telehealth)
Telemedicine supports the provision of health-care services at a distance; that is, the individual and health-care providers need not be in the same location. Telemedicine enables the delivery of safe and quality care to individuals living in areas with limited access to services. Examples of telemedicine services are provided below.
-
Store-and-forward services involve acquiring medical data (e.g., images) and transmission to a health-care provider (e.g., doctor or medical specialist) for offline assessment and treatment recommendation. Examples include teleradiology and telepathology.
-
Remote monitoring services enable health-care providers to monitor an individual’s condition remotely, using technologies such as implanted devices and sensors with wireless or wired connections.
-
Interactive services enable real-time interaction between an individual and her or his health-care provider through means such as telephone, web conference, video conference, and other forms of online and remote communication. Psychiatry and mental health services are classic examples.
-
Telecare services enable care and support to older individuals and those with special needs. This helps them to remain independent in their homes and increases their sense of connectivity with the broader community. Services include alerts (e.g., domestic accidents such as falls) and monitoring (e.g., vital signs, blood glucose, and weight).
Mobile Health (mHealth)
mHealth describes services and information provided through mobile technology, such as mobile phones and handheld computers. mHealth has emerged rapidly in developing countries as a result of the large penetration of mobile phones and the lack of other, modern health infrastructure.
Examples include the use of mobile devices for:
-
Data collection for surveillance and public health (e.g., outbreak investigation)
-
Real-time monitoring of an individual’s health
-
Treatment support, health advice, and medication compliance
-
Health information to practitioners, researchers, and patients
-
Health education and awareness programs
-
Diagnostic and treatment support, communication for health-care workers.
Decision Support Systems
Decision support systems assist health-care providers in making diagnosis and treatment decisions. These systems combine an individual’s current and historical health information with the health-care provider’s knowledge, to provide advice intended to result in better quality care and outcomes for the individual.
For example, in the area of medication management, decision support tools draw on electronic knowledge sources, such as clinical practice guidelines and knowledge bases, and apply this knowledge to local patient and clinical data through expert rules to guide medications decision-making.
Decision support systems, when coupled with a comprehensive and accurate base of patient information, are able to identify potential drug interactions, dosing inaccuracies, and prescribing errors that could lead to serious adverse events.
Chronic Disease Management Services
Chronic disease management services are designed to improve coordination and management of care for individuals with chronic conditions. Better tracking of health status, test results, and other parameters enables closer management and prevention of episodes of acute illness or decline in status. Information tracked over time supports individual care planning as well as program design, resource allocation, and research on disease states, benefiting clinicians, administrators, managers, and researchers.
Practice, Patient, and Clinical Management Systems
Practice, patient, and clinical management systems refer to the computer systems that health-care organizations use to manage the delivery of care to individuals. These systems provide the ability to capture, store, access, and share health information for patients during their care episode. These systems can also provide a broad range of health-care management and delivery functions for a health-care entity, such as diagnostics management, scheduling and resourcing management, clinical care management, and reporting. Practice, patient, and clinical management systems form one of the foundations required for collecting, recording, and sharing electronic information across a country’s health sector.
Electronic Medication Services
Electronic medication services benefit health-care professionals and the general public. Services such as electronic prescribing allow the electronic transmission of prescription information from the health professional to the pharmacy, reducing medication errors and replacing paper-based systems. Online (Internet) medication purchase from certified pharmacies can reduce cost and improve convenience and access to medications.
Health Knowledge Resources
Health knowledge resources encompass those services that manage and provide access to trusted information to support health-care providers and individuals. Resources include international electronic journals and resource collections, national electronic journals, and national open archives.
Distance Learning for Health Professionals (eLearning)
eLearning services comprise education and training in electronic form for health professionals. eLearning can improve the quality of education, increase access where learning resources are unavailable, or use new forms of learning. Examples of use include continuing medical education for doctors and nurses, and training on preventive services at the household level for community health workers. eLearning tools vary widely, and may allow interaction between the learner and instructor, access to digital libraries and online courses, networks to share experiences, or the use of mobile devices to access information to support delivery of care.
Health Information Systems
Health information systems facilitate gathering, aggregating, analyzing, and synthesizing data from multiple sources to report on health situation and trends (disease burden, patterns of risk behavior, health service coverage, and health system metrics). Countries may have in place one or more health information systems supporting reporting on diseases or programs. They may also have HIS strategies aimed at improving decision-making, policy development, health services management, response to emerging threats and better allocation of health resources.
The Diffusion of eHealth Solutions: A Global and African Regional Perspective
The utilization of eHealth solutions since the late 2000s has been increasing (WHO 2016). This trend has been fostered by increased global leadership of the WHO, strengthened donor commitments (Spider 2020), formulation of international digital development principles (Digital Impact Alliance 2020), national commitments, ubiquity of ICT person held devices, and an increasing coverage of broadband. However, significant challenges have hampered this progress relating to a number of factors including adoption costs, siloed implementation, interoperability (technical, semantic, and syntactic), health workforce readiness, workflow configuration, long-term sustainability, fragmentation, and verticalization. (Granja et al. 2018; WHO 2016). The draft WHO global strategy on digital health (WHO 2020h), aims at actualizing the WHO resolution of digital health (WHO 2020j), has been positioned to mitigate these challenges, and to further strengthen the value proposition of health in the digital health, and the acceleration of global public health visionary goals and targets.
Since the 2005 WHO resolution on eHealth (WHO 2020k), the global landscape on eHealth has seen remarkable progress at both policy and eHealth solutions level (WHO 2020i). At the policy level, the national WHO – ITU toolkit has been a critical instrument in the promotion and elaboration of national digital health strategies (ITU 2020b). At the eHealth solutions level, various tools have been used to manage the production of eHealth solutions, from conception, initiation, streamlining, development, implementation, review to end user engagement.
The WHO – ITU national eHealth toolkit is a how to guide and methodic tool that enables governments, development partners, implementers, and various actors in the eHealth echo system, providing guidance in the formulation of a national eHealth vision, action plan, and method for evaluation of the impact of the strategy (ITU 2020b; WHO – ITU 2013; WHO 2020h). While the eHealth vision statement is an aspirational statement of how eHealth contributes to global and national development public health goals, the action plan enables the realization of the eHealth vision. The toolkit articulates seven building blocks aimed at fostering a conducive enabling environment, including strategy and investment, services and applications, standards and interoperability, infrastructure, legislation, policy and compliance, and workforce. Though not prescriptive, these pillars have been used to measure the maturity of the eHealth enabling environment. Tools, such as the Global Digital Health Index, have been used to demonstrate maturity modeling based on the toolkit (HealthEnabled 2020).
According to the third WHO global observatory on eHealth (WHO 2016), which focused on the use of eHealth for universal health coverage, the results of the survey show progressive policy arrangements for eHealth with more than half of the 125 WHO Member States (from here on referred to simply as countries) reporting having an eHealth strategy, with 90% of these eHealth strategies having a reference to the objectives of UHC components (ibid.). Further, given the critical need of addressing security considerations in eHealth for both data in transit and data at rest, 78% of participating countries reported having legislation for protecting the privacy of personal information. Further, 54% of the participating countries reported having legislative provisions to protect the privacy of electronically held patient data (WHO 2020l). These arrangements provide an enabling environment for eHealth solutions to be used safely and effectively, enabling eHealth solutions to be governed and directed toward health system challenges, enabling interoperability, and the provision of patient centric health services for better health outcomes. The strategies also provide a platform to enable holistic, horizontal eHealth solution implementations meeting country needs while mitigating silos and unscalable pilots, as well as costly fragmentation (Fei Huang 2017; McCann 2020; Björn Schreiweis 2019).
Beyond policy arrangements for eHealth solutions, the third WHO eHealth observatory survey reported significant uptake of eHealth solutions at the global level. (WHO 2016). This update shows a consistent rate of eHealth penetration from earlier surveys, with remarkable progress seen in mHealth, telehealth, eLearning, EHRs, and social media (ibid.). Of the 125 reporting countries, several reported implementing at least one mHealth eHealth solution (83%). Several countries reported growth in the use of telehealth services, with teleradiology being the most popular (77%), while other telehealth services such as telepathology, remote patient monitoring, and teledermatology were reported in almost half of the reporting countries (ibid.). eLearning was reported in 84% of the reporting countries, while EHRs eHealth solutions were reported in 47% of the reporting countries. About 80% of the reporting countries reported using social media tools for health promotion (ibid.).
The above global picture resonates with the trends in the African region. eHealth policies and solutions are backed by a resolution passed by Ministers of health in the African region in 2013 (WHO AFRO 2020a; WHO AFRO 2020b; WHO 2020m). By the end of 2019, 33 countries in the African region had developed their eHealth strategies (WHO AFRO 2020c). Consistent with the global trends, mHealth solutions are the leading trend in the African region, with 24 countries reporting at least one or more mHealth solutions according to the 2016 global observatory on eHealth (WHO 2020i; WHO AFRO 2018). At least 22 countries reported using social media for health promotion while at least 20 countries reported using telehealth for increasing access to care (ibid.). At least 13 countries reported using eLearning systems to broaden the reach of continuous professional development, while at least 16 countries reported implementing electronic health record systems (ibid.). At least 18 countries reported having a human resource information system while at least 18 countries reported implementing a supply chain information system (ibid.). Several countries in the African region reported linking eHealth solutions with medical devices to further enhance the integration between the solutions and medical devices, especially for care in remote areas (WHO 2013).
Success Factors for eHealth Solutions
In order for eHealth solutions to deliver value in health care, countries need to continue to tackle the key issues identified at the onset of the first WHO resolution on eHealth relating country led eHealth roadmaps and key enabling environment issues of connectivity, eHealth literacy for the health workforce, interoperability, and legislation, among others (Joses and Kirigia 2005; WHO 2020g). Overlaying these enabling environmental issues are issues related to systematic application of implementation methods, using such tools as the WHO Digital implementation investment guide (DIIG) and the principles of digital development, in order to accelerate the adaption and sustainability of eHealth solutions (WHO 2020b; Digital Impact Alliance 2020). The principals of digital development are critical in streamlining current efforts of introduction of eHealth solutions in such a way as to foster holistic approaches. They emphasize nine living approaches to automation, related to designing electronic solutions with the end user (co-creation); understanding the existing health ecosystem; designing solutions for scale; building solutions for sustainability; using data as a driving force; using open standards, open data, open source, and open Innovation as much as possible; reusability and improvements based of what has worked; addressing privacy and security aspects of solution introduction; and fostering a collaborative spirit among actors in the eHealth echo system (Digital Impact Alliance 2020).
Inventory Tools for eHealth Solutions
A proliferation of eHealth solutions exists today. This has largely been due to the simplification in the creation of these solutions over time, as a result of the advancement in the technology arena. Countries need to ensure that they have a method to document these solutions, the standards they use as well as the areas where they are deployed. One such instrument of eHealth solutions inventory management is the WHO digital health atlas (WHO 2020n; Measure Evaluation 2020).
The digital health Atlas is a technology platform aimed at strengthening the value and impact of eHealth investments, coordination of eHealth efforts, and enabling eHealth solutions to scale (ibid.). Among the challenges of scaling eHealth solutions has been their visibility at the global and national levels. In addition, the Atlas provides a mechanism to add meta-data about the eHealth solutions, such as the implemented standards and the addressed health system challenges.
Moving Toward Scale for Better Health Outcomes
As awareness has been on the increase with regard to the availability of eHealth solutions, a paradigm shift is needed in the health sector with regard to the introduction of eHealth solutions. While the African region has seen rapid introduction of eHealth solutions post the 2005 eHealth resolution, the solutions were largely characterized by pilots or program-based solutions (McCann 2020; Fei Huang 2017). One aspect of the paradigm shift relates to transitioning toward a systems approach from a solutions approach. Many countries in the African region are still struggling with legacy eHealth systems that were not built for interoperability, but nevertheless have legacy patient data that cannot be discarded. Another dimension of the paradigm shift relates to seeing eHealth solutions as a means to an end and not the end in itself. This requires strategic thinking on eHealth literacy at secondary education and preservice health education. This paradigm shift ensures wider adoption of eHealth solutions for the long term, so as to ensure sustained better health outcomes enabled by eHealth, and that no one is left behind.
Conclusion
eHealth solutions have the potential to accelerate internationally agreed health targets and goals, such as the sustainable development goals (SDGs), especially SDG3, and in particular UHC. This was underscored in 2018, when several government leaders around the world met in Astana to mark 40 years post the Alma Ata declaration that made primary health care a corner stone of public health interventions (Rifkin 2018; WHO 2018). At the international level, coordination is needed to ensure that the public health proposition that eHealth solutions offer are aligned with global targets. This includes alignment of investments and approaches. At the country level, a multisectoral approach is needed to ensure a whole of government approach and enhance health in all policies, enabled by eHealth (CDC 2020; WHO 2020o).
The WHO, as a global leader in public health, has produced various instruments to support the creation of an eHealth ecosystem (WHO – ITU 2013). These are backed by various resolutions on eHealth and recently also on digital health. These instruments require initialization among various actors in the eHealth ecosystem, to enable systematic, coherent, and replicable implementation at the national level. It is critical to think ahead by building foundations for long-term sustainability, including the creation of an adaptable, eHealth ready health workforce, investing in data standards, establishing interoperability frameworks and system-based eHealth solutions, updating legal frameworks, providing sustainable financing models for eHealth solutions, connectivity, and governance arrangements.
The draft WHO global strategy (WHO 2020h) forms a new foundation to advance eHealth. However, for this to be realized, continued dialogue with all actors in the eHealth space will be critical, to avoid past mistakes of fragmentation, silos, and pilotitis (Fei Huang 2017; McCann 2020). In the past 20 years, the international community has seen a number of global health threats that have compromised global health security. At the end of 2019, a new health emergency threat called COVID19 emerged that underscored the acceleration of ICTs in health. eHealth stands to accelerate health emergency preparedness and the building of resilient and responsive health systems. This aspiration requires seamless integration of eHealth solution in health-care service provision.
References
Björn Schreiweis MP (2019) Barriers and Facilitators to the Implementation of eHealth Services: Systematic Literature Analysis. Journal of Medical Internet Research. https://doi.org/10.2196/14197
CDC (2020, November 2) Office of the Associate Director for Policy and Strategy: Health in All Policies. Retrieved from Health in All Policies: https://www.cdc.gov/policy/hiap/index.html#:~:text=Health%20in%20All%20Policies%20(HiAP,of%20all%20communities%20and%20people
Digital Impact Alliance (2020, October 31) Principles: Principles for digital development. Retrieved from Principles for digital development: https://digitalprinciples.org/
FDA (2020, 10 11) Digital Health Center of Excellence: What is Digital Health? Retrieved from What is Digital Health?: https://www.fda.gov/medical-devices/digital-health-center-excellence/what-digital-health
Fei Huang SB (2017) Beyond pilotitis: taking digital health interventions to the national level in China and Uganda. BMC, https://doi.org/10.1186/s12992-017-0275-z.
Giedrius Vanagas RE (2018) eHealth Solutions for the Integrated Healthcare. Journal of Healthcare Engineering. https://doi.org/10.1155/2018/3846892
Granja C, Janssen W, Johansen MA (2018) Factors Determining the Success and Failure of eHealth Interventions: Systematic Review of the Literature. Journal of Medical Internet Research. https://www.jmir.org/2018/5/e10235/
HealthEnabled (2020, October 31) Global Digital Health Index. Retrieved from https://www.digitalhealthindex.org/
HHS (2020, 10 11) COVID-19: About COVID-19. Retrieved from About COVID-19: https://www.gov.nt.ca/covid-19/en/services/about-covid-19
ITU (2020a, September 13) Development: eHealth. Retrieved from eHealth: https://www.itu.int/en/ITU-D/ICT-Applications/eHEALTH/Pages/EHEALTH.aspx
ITU (2020b, October 31) National eHealth Strategy Toolkit. Retrieved from https://www.itu.int/pub/D-STR-E_HEALTH.05-2012#:~:text=The%20National%20eHealth%20Strategy%20Toolkit,action%20plan%20and%20monitoring%20framework
Joses M, Kirigia AS (2005) E-health: Determinants, opportunities, challenges and the way forward for countries in the WHO African Region. BMC Public Health. https://doi.org/10.1186/1471-2458-5-137
L Velez-Lapaõ MM (2019) eHealth solutions to regional shortages in the health workforce (Supplement 4). European Journal of Public Health. 1101–1262
Mark H, Siska DA (2011) Opportunities and challenges related to technology in supporting optimal pharmacy practice models in hospitals and health systems. American Journal of Health-System Pharmacy. 1116–1126
McCann D (2020, October 31) ICT Works : A Ugandan mHealth Moratorium Is a Good Thing. Retrieved from A Ugandan mHealth Moratorium Is a Good Thing: https://www.ictworks.org/ugandan-mhealth-moratorium-good-thing/#.X57IBIhKjIU
Mea VD (2001) What is e-Health (2): The death of telemedicine? Journal of Medical Internet Research, https://doi.org/10.2196/jmir.3.2.e22
Measure Evaluation (2020, November 1) HIS Assessment Tools: Digital Health Atlas. Retrieved from Digital Health Atlas: https://www.measureevaluation.org/his-strengthening-resource-center/his-tools/tool?ToolId=76
Rashid L, Bashshur GW (2009) National Telemedicine Initiatives: Essential to Healthcare Reform. Mary Ann Liberty, inc publichers. https://doi.org/10.1089/tmj.2009.9960
Rifkin SB (2018) Alma Ata after 40 years: Primary Health Care and Health for All–from consensus to complexity. BMJ Glob Health. https://doi.org/10.1136/bmjgh-2018-001188
Spider (2020, October 31) Digital Investment Principles: The Principles of Donor Alignment for Digital Health. Retrieved from The Principles of Donor Alignment for Digital Health: https://digitalinvestmentprinciples.org/
The World Bank (2020, October 18) Health: Universal Health Coverage for Inclusive and Sustainable Development. Retrieved from Universal Health Coverage for Inclusive and Sustainable Development: https://www.worldbank.org/en/topic/health/publication/universal-health-coverage-for-inclusive-sustainable-development
UN (2020, October 18) Sustainable Development Goals : Goal 3: Ensure healthy lives and promote well-being for all at all ages. Retrieved from Goal 3: Ensure healthy lives and promote well-being for all at all ages: https://www.un.org/sustainabledevelopment/health/
WHO – ITU (2013) National eHealth Toolkit. Geneva: WHO
WHO (2010) Monitoring The Building Blocks Of Health Systems:A Handbook Of Indicators And Their Measurement Strategies. Geneva: WHO
WHO (2013) Medical devices and eHealth solutions: Compendium of innovative health technologies for low-resource settings. Geneva: WHO
WHO (2016) Global diffusion of eHeath : Making universal health coverage achievable. Geneva: WHO
WHO (2018) Declaration of Astana : Global Conference on Primary Health Care. Geneva: WHO
WHO (2020a, September 13) eHealth : eHealth at WHO. Retrieved from eHealth at WHO: https://www.who.int/ehealth/en/
WHO (2020b) Digital implementation investment guide. Geneva: WHO
WHO (2020c, October 11) Overview: Ebola virus disease. Retrieved from Ebola virus disease: https://www.who.int/health-topics/ebola/#tab=tab_1
WHO (2020d, September 13) History of WHO. Retrieved from Who we are: History of WHO: https://www.who.int/about/who-we-are/history
WHO (2020e, September 13) Our Values: Our Values, our DNA. Retrieved from Our Values, our DNA: https://www.who.int/about/who-we-are/our-values
WHO (2020f, September 13) What we do: Thirteenth General Programme of Work 2019–2023. Retrieved from Thirteenth General Programme of Work 2019–2023: https://www.who.int/about/what-we-do/thirteenth-general-programme-of-work-2019–2023
WHO (2020g, 10 11) Health Academy: WHO eHealth Resolution. Retrieved from WHO eHealth Resolution: https://www.who.int/healthacademy/news/en/
WHO (2020h, October 31) Draft global strategy on digital health 2020–2025. Retrieved from https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf
WHO (2020i, October 25) Global Observatory for eHealth. Retrieved from https://www.who.int/goe/en/
WHO (2020j, October 31) Seventy-First World Health Assembly: Digital health. Retrieved from Digital health: https://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_R7-en.pdf?ua=1
WHO (2020k, October 31) Resolutions And Decisions: eHealth. Retrieved from eHealth: https://www.who.int/healthacademy/media/WHA58-28-en.pdf?ua=1
WHO (2020l, October 31) eHealth. Retrieved from https://www.who.int/ehealth/en/#:~:text=The%20Strategy%20aims%20to%20accelerate,consultation%20until%2030%20April%202019
WHO (2020m, November 1) World Health Organisation Regional Office for Africa. Retrieved from https://www.afro.who.int/
WHO (2020n, November 1) Digital Health Atlas. Retrieved from https://digitalhealthatlas.org/fr/-/
WHO (2020o, November 2) Health promotion: Health in All Policies: Framework for Country Action. Retrieved from Health in All Policies: Framework for Country Action: https://www.who.int/healthpromotion/frameworkforcountryaction/en/
WHO AFRO (2018, August 30) Progress Report On Utilizing Ehealth Solutions To Improve National Health Systems In The African Region. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/275914/AFR-RC68-INF-DOC-2-eng.pdf?sequence=1&isAllowed=y
WHO AFRO (2020a, November 1) Regional Committee for Africa: Utilizing Ehealth Solutions To Improve National Health Systems In The African Region. Retrieved from Utilizing Ehealth Solutions To Improve National Health Systems In The African Region: https://www.afro.who.int/sites/default/files/sessions/resolutions/afr-rc63-r5-utilizing-ehealth-solutions-to-improve-national-health-systems.pdf
WHO AFRO (2020b, November 1) Health Topics: E-Health. Retrieved from E-Health: https://www.afro.who.int/health-topics/e-health
WHO AFRO (2020c, November 1) Utilizing Ehealth Solutions to Improve National Health Systems In The African Region: Information Document. Retrieved from Utilizing Ehealth Solutions to Improve National Health Systems In The African Region: https://apps.who.int/iris/bitstream/handle/10665/334099/AFR-RC70-INF-DOC-4-eng.pdf?sequence=3&isAllowed=y
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 World Health Organization under and exclusive license to Springer Nature Switzerland AG, part of Springer Nature
About this entry
Cite this entry
Muneene, D. (2021). eHealth Solutions in Global Health. In: Kickbusch, I., Ganten, D., Moeti, M. (eds) Handbook of Global Health. Springer, Cham. https://doi.org/10.1007/978-3-030-45009-0_72
Download citation
DOI: https://doi.org/10.1007/978-3-030-45009-0_72
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45008-3
Online ISBN: 978-3-030-45009-0
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences