Abstract
This chapter reviews human neuroimaging studies that investigate the neurobiology of reward processing in eating disorders associated with binge eating. Across the relatively small research literature on binge-eating disorder (BED) and bulimia nervosa (BN) using food and nonfood stimuli, neuroimaging studies consistently suggest alterations in brain reward circuit response. Studies tend to identify heightened brain response to visual presentation of reward cues, while reward receipt, including unexpected receipt, is associated with lower brain activation. Those results point toward specific neurotransmitter alterations associated with binge eating pathophysiology. However, there is still extensive heterogeneity across studies due to different study designs and analytic approaches, and research that systematically translates and studies basic science models in humans will have the best chance of identifying neurocircuitry that is specific to this pathology.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning ObjectivesIn this chapter, you will learn:
-
To understand the current state of reward-focused neuroimaging research in disorders associated with binge eating.
-
To identify the gaps and limitations of the current research.
-
To discuss the potential future directions of neuroimaging research on binge eating.
1 Introduction
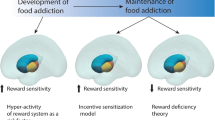
The motivation to seek and consume food is mediated by the brain’s reward circuitry. A form of dysregulated food consumption is binge eating, which has been associated with abnormalities of the reward system in both animal models as well as human research on eating disorders (Avena 2013; Wierenga et al. 2014; Berridge 2009b). Binge eating is a cross-cutting behavior that is characterized by recurrent episodes of eating very large amounts of food in a short period of time with a sense of lack of control (American Psychiatric Association 2013). Binge eating can be found most characteristically in binge-eating disorder (BED), and it is also a diagnostic criterion for bulimia nervosa (BN) where those episodes are followed by compensatory behaviors to avoid weight gain. Anorexia nervosa can also present with binge eating, but there it only defines a subtype. Notably, an overweight or obese body mass index (BMI) can often be found in BED but it is not a diagnostic prerequisite, while individuals with BN are commonly in the high normal weight range.
Several reviews have surveyed the reward-focused neuroimaging literature on BED, obesity, and other eating disorders characterized by binge eating behavior (Michaelides et al. 2012; Schag et al. 2013; Wu et al. 2016; Boswell and Kober 2016). The research studies reviewed in this chapter (Table 1) will particularly focus on the emerging role of the brain’s reward processing circuitry, including the striatum, frontal cortex, and insula. Striatal structures are known to respond to salient stimuli and encode prediction errors during reward learning, contributing to impulsivity in decision-making (Flagel et al. 2011). The medial prefrontal and orbitofrontal cortex are important for reward valuation and sensory-specific satiety, and code when to stop eating a certain food, while other food might still be valued and therefore of interest (Rolls et al. 1981). The insula contains the primary taste cortex and integrates somatosensory and interoceptive processing, emotional, and cognitive regulation, implicating a central role of the insula in appetite control and hedonic food reward processing (Uddin et al. 2017; Craig 2009; Frank 2013; Rolls 2016). The hyper- and hypo-responsivity found across these regions may reflect the imbalance of reward sensitivity and inhibition/impulsivity thought to underlie binge eating pathophysiology (Kessler et al. 2016; Wierenga et al. 2014). A key question that remains to be answered is how neurotransmitter systems drive binge eating and how can they be manipulated to improve outcome of binge eating associated pathology.
2 Functional Magnetic Resonance Imaging (fMRI)
Functional magnetic resonance imaging (fMRI), which measures the blood–oxygen level-dependent (BOLD) signal, is the most common functional neuroimaging modality used to study binge eating neurobiology. This technique allows the comparison of brain activity in response to different stimuli during a brain scan. The following study designs utilized both food-specific stimuli that are directly relevant to binge eating, and nonfood stimuli that explore generalized reward processing.
2.1 Food-Specific Reward Paradigms
2.1.1 Visual Cue Studies
Two studies have used visual and auditory food cues across four groups of women: individuals with subthreshold BED with and without obesity, and individuals without binge eating with and without obesity. The first study demonstrated greater dorsal anterior cingulate cortex response to high-calorie food cues in women with binge eating compared to those without, regardless of weight status (Geliebter et al. 2006). The second study assessed the conservation of regional activation within group rather than comparing regional activation between groups (Geliebter et al. 2016). The five obese binge eaters exhibited strict conservation of right premotor area response to binge food stimuli, which was interpreted to represent motor planning of eating the food stimuli. The design of these studies is strengthened by the inclusion of visual and auditory food cues, different weight status in women with and without binge eating, and a standardized meal 3 h prior to the scan. Problematic though are, as stated above, the small group sizes in those studies. Several other studies have compared visual food reward responses across BED, BN, normal weight, and overweight/obese controls. One group tested the brain response of fasted participants viewing high-calorie foods, disgust-inducing items, and neutral items. Compared to BN, normal weight, and overweight groups, BED showed greater medial orbitofrontal cortex response to food stimuli (Schienle et al. 2009). In contrast, although the BN and BED groups scored similarly in the degree of binge eating, the BN group showed greater insula and anterior cingulate cortex response to food stimuli than the other three groups. These results implicate distinct neural mechanisms in BED, BN, and obesity, where altered orbitofrontal cortex processing of food cues may underlie binge eating in BED. However, a decoding analysis of this data set later showed that BED could be distinguished from normal weight controls, not by the orbitofrontal cortex, but by insula response to food cues and from obese controls with ventral striatum response (Weygandt et al. 2012). The same data set was further studied for brain volume across BED, BN, and controls in a voxel-based morphometry (VBM) analysis (Schafer et al. 2010). Groups showed no differences in global gray matter, white matter, or cerebrospinal fluid volume. However, regional gray matter volume differences in regions involved in food reward processing were detected: both the obese BED and BN groups showed greater orbitofrontal cortex volume compared to controls, while BED had larger anterior cingulate and BN larger ventral striatal volumes compared to controls. The BN group showed also higher orbitofrontal cortex and striatal volumes compared to BED participants. This same sample of individuals with BED displayed greater medial orbitofrontal cortex activation in response to food stimuli compared to BN, overweight and normal weight control groups (Schienle et al. 2009). The authors suggest that the structural and functional abnormalities of the orbitofrontal cortex could underlie the altered self-regulation and habit learning in BED. Brain volume could be different across groups due to developmental differences in growth and neuron pruning, and neuronal mass could explain altered brain function. While these are compelling findings, the combination of structural and functional imaging data will need to be applied in future analyses to better understand brain structure–function relationships (Frank et al. 2018b).
In a reward incentive delay task that included both visual food cues and monetary stimuli, brain response was compared between 27 individuals with BED, 28 with obesity, 29 with BN, and 27 normal weight controls (Simon et al. 2016). That task tests brain activation during expectation of rewards, while rewards vary in magnitude and how long a person has to wait for a larger or smaller reward. No group differences for brain response in the monetary task were found. In response to the notification that a food reward had been earned, both BED and BN groups exhibited heightened medial orbitofrontal cortex activity compared to their respective control groups. This hyper-responsiveness was further correlated with increased food craving and external eating scores, but not binge eating behavior, in the BED and BN groups. That study suggested that food reward circuitry was specifically hyper-responsive in the binge eating study groups and related to the drive to approach food.
Another study investigated the effects of food image interference in a Stroop-Match-to-Sample task to investigate whether potentially reward system activating food stimuli would interfere with cognitive performance (Lee et al. 2017). Compared to healthy controls, the BED group showed greater ventral striatum response to food images. Behaviorally, there was a nonsignificant trend of impaired cognitive control over food image interference in BED. These results suggest the reward salience processing function of the ventral striatum could interfere with top-down attentional control in BED, but the groups were small and the study likely underpowered.
One study investigated brain response during viewing of palatable foods in full and subthreshold BN and compared a neutral versus a stress condition (Wonderlich et al. 2018). That study, which did not include a control group, showed that brain response decreased to food cues following the stress induction in the right and left ventromedial prefrontal cortex, the right anterior cingulate cortex, and left amygdala. Interestingly, less change in brain response was associated with greater negative and less positive affect prior to binge eating. That study suggests a direct relationship between negative affect and brain response, which in turn could control the drive to binge eat.
A recent review of the use of food images and functional brain imaging in anorexia nervosa found that using this approach resulted in more consistent findings when targeting reward pathways than other cognitive or emotional processes (Lloyd and Steinglass 2018). Thus, this approach may also have value to study reward circuit activation in binge eating. Nevertheless, presentation of food images frequently leads to results that are difficult to relate to the underlying neurobiology or neurochemistry that drives pathological eating behavior and more sophisticated studies are needed to move this field forward.
2.1.2 Taste Cue Studies
Individuals with a BED diagnosis are yet to be studied with fMRI while consuming real taste stimuli. One study has investigated binge eating behavior with taste stimuli in a single group of 26 individuals with a BMI over 25 kg/m2 and a moderate binge eating score on a self-report measure (Filbey et al. 2012). Reward regions in the brain (medial orbitofrontal cortex, ventral tegmental area, insula, caudate, putamen, nucleus accumbens, and precuneus) were more responsive to high-calorie taste stimuli compared to water in this group. Higher binge eating symptoms, but not BMI, were associated with higher high-calorie brain taste responses. These findings provide some evidence of taste reward sensitivity underlying the increased motivation to eat in BED. A study that applied milkshake or control solution to women with full or subthreshold BN found that the BN group tended to have less activation when expecting milkshake in the right anterior cingulate, and in response to consumption of milkshake lower activation in the left middle frontal gyrus, posterior insula, precentral gyrus, and mid-dorsal insula (Bohon and Stice 2011). However, the results were not statistically significant, making the implications less clear. One recent study compared sweet taste (sucrose) with the aversive bitter stimulus quinine in BN (Monteleone et al. 2018). In that study, the BN group had a lower response to the bitter stimulus in insula and amygdala, but sweet taste response was normal. Sweet sucrose taste was also used in a study from our group in BN that assessed brain prediction error response, a model that has been associated with brain dopamine function and tests brain response to unexpected receipt or omission of stimuli (Frank et al. 2011). The BN group showed lower activation as well as prediction error regression in insula, ventral putamen, amygdala, and orbitofrontal cortex compared to controls, suggesting a downregulation of the sensitivity of the dopamine circuitry. Importantly, higher binge eating frequency was negatively correlated with brain prediction error response, suggesting either a direct impact from eating disorder behavior on brain function or a premorbid lower brain response that could drive binge eating episodes. Any causal relationships need further study. Brain imaging can also be used to test the direction of activation between brain regions using so-called effective connectivity analyses. We used this approach in the above-described sample of individuals with BN and controls that we studied for prediction error response and extracted data for the expected sucrose solution taste condition (Frank et al. 2016). Controls showed effective connectivity from the hypothalamus to the ventral striatum, while the BN group had the opposite result; the direction of activation was from cortical structures to ventral striatum and hypothalamus. We hypothesized that sugar as a fear-inducing stimulus may stimulate a pathway that interrupts the eating drive via the ventral striatal—hypothalamic circuitry (Frank et al. 2018a).
Umami taste has been described as a savory flavor, it is different than the other taste qualities, sweet, sour, bitter or salty, and specific tongue taste receptors exist (de Araujo et al. 2003). A study in BN using this taste stimulus found that the BN group had a stronger response to the umami taste in the right insula compared to the control group (Setsu et al. 2017). In addition, in the control group, there was a significant inverse relationship between insula response and subjective umami pleasantness ratings, while there was no significant brain–behavior response in the BN group.
In summary, studies report higher or lower brain responses to taste stimuli across study designs that vary in taste quality and method of application. The key to identifying biological targets for treatment development will be that studies use basic science models that can be tested in humans and that allow identifying neurotransmitters directly involved in specific eating disorder behaviors. The prediction error model is such a model that is based on dopamine neuronal function and that can be studied using specific dopamine receptor agonists and antagonists. In addition, studies that test neurobiology cross cutting the various eating disorder groups may help identify circuitry that drives binge eating behaviors and identify for instance circuit alterations specific to binge eating versus purging or high BMI. The NIMH Research Domain Criteria provide a framework for such studies (Cuthbert 2014).
2.2 Nonfood-Specific Reward Paradigms
The first study to explore nonfood-specific reward processing in BED compared brain activity during a monetary incentive delay task in 19 individuals with obesity and BED (OB BED), 19 with obesity and without BED (OB), and 19 healthy weight controls (Balodis et al. 2013). The BED group displayed reduced ventrostriatal activity during reward anticipation and reduced prefrontal cortex and insula activity during reward outcome. The BED group then went on to complete 4 months of treatment with sibutramine (an appetite suppressant) and/or cognitive behavioral therapy. Compared to individuals in the group who successfully responded to this treatment, individuals who did not respond to treatment (i.e. continued to binge eat) showed decreased ventral striatal and inferior frontal gyrus response to reward anticipation and decreased medial prefrontal cortex response to reward outcome pretreatment (Balodis et al. 2014). These findings implicate hypo-responsivity to nonfood reward stimuli in BED.
One study in BED-linked responses on a monetary reward learning task with brain structure (but not functional brain response) in subjects who were obese with BED and subjects who were obese without BED (Voon et al. 2015). The obese BED group displayed a greater tendency toward habit-based learning and perseveration and reduced left ventral striatal, bilateral caudate, and orbitofrontal cortex gray matter volume compared to the OB group. Interestingly, these regional volume differences were no longer significant when researchers accounted for the model-based parameter for the subjects’ habit-based learning behavior. Furthermore, higher binge eating scores were associated with a stronger bias toward using a habit-based or “model-free” (“trial and error”) strategy. These results point to model-free reward learning as a neurocomputational mechanism contributing to the maladaptive habit formation involved in binge eating behaviors. Importantly, the regional volumes were different in the OB groups depending on the presence of BED. Unfortunately, the study did not include normal weight controls, preventing comparison of its results with the previous MRI study (Schafer et al. 2010).
A more recent study found that BED compared to healthy controls exhibited reduced insula and ventrolateral prefrontal cortex activation during exploratory decisions using a monetary dynamic choice task that tested a reinforcement learning model (Reiter et al. 2017). The BED group further displayed reduced ventromedial prefrontal cortex activation associated with the prediction error learning signature that incorporated alternative choices. Although the study did not relate behavioral or brain activation data to binge eating symptoms, the findings suggest a neurocognitive phenotype of BED, where deficient prefrontal cortex activation during decision-making represents a neural correlate of maladaptive switching behavior. A study that investigated brain circuitry for both neurocognition and reward recruited adolescents with BN and controls and applied a spatial orientation task in a virtual maze where subjects could earn monetary rewards (Cyr et al. 2016). The BN group showed opposite responses compared to controls. The BN participants activated the right anterior hippocampus during the receipt of unexpected rewards (control condition), and deactivated the left superior frontal gyrus and right anterior hippocampus during expected reward receipt (learning condition). Furthermore, hippocampal activation in the BN during the unexpected rewards condition was significantly related to BN behavior scores. Anxiety and impulsivity are behavioral constructs that have been associated with BN (Chase et al. 2017; Xia et al. 2017; Vitousek and Manke 1994; Wagner et al. 2006). The hippocampus has traditionally been found to be involved in memory function but recent optogenetic research implicated hippocampal serotonin neurons in the modulation of anxiety and impulsivity (Ohmura et al. 2019). It is possible that for instance, hippocampal hyper-responsiveness during an unexpectancy task condition can be a neurobiological correlate that is related to impulsivity and tendency to binge eat in a person’s natural environment. A different approach was taken in a study that recruited adolescent girls from a community sample and compared binge eating participants with those without that behavior (Bodell et al. 2018). In that study, the severity of binge eating correlated positively with activation in ventromedial prefrontal cortex and caudate during winning money. This study further points toward reward circuit abnormalities.
Taken together, nonfood reward tasks have led to altered brain responses in groups with binge eating behaviors. BED and BN tended to show lower brain response in frontal or subcortical brain response, although the described community sample study indicated higher brain activation with more severe binge eating severity. Lower response to unexpected stimuli could point again to reduced dopamine circuit sensitivity as found in a sweet taste paradigm in BN (Frank et al. 2011).
2.2.1 Drug Challenge Studies
The reward system involves the interaction of cortical and subcortical brain regions and associated connecting pathways to process desire, action to approach and consume reward stimuli, and learning from those experiences (Haber and Knutson 2010; Kelley et al. 2005). The neurotransmitters dopamine and opioids code key aspects of neural reward processing. Dopamine neurons code motivation (“wanting”), reward approach and learning, and the opioid system codes pleasurable experience from rewards (“liking”) (Berridge 2009a; Kelley and Berridge 2002). Functional magnetic resonance brain imaging (fMRI) tests brain activation across brain regions and circuits, such as reward or anxiety pathways. Those studies usually do not test brain neurotransmitters directly, but the response during tasks that test specific behaviors might help in understanding neurotransmitters involved in the brain response (Frank 2011). Although fMRI does not allow for direct measurement of neurotransmitter levels, drugs can be administered to pharmacologically manipulate neurotransmitter systems. Several fMRI studies have used drugs to challenge specific neurotransmitter systems in BED. The first measured brain response to high- and low-calorie food images after placebo or a dopamine D3 receptor antagonist in 26 individuals who were overweight/obese and had binge eating behaviors (Dodds et al. 2012). Binge eating behavior was assessed with a self-report questionnaire and subjects fasted 15 h prior to scanning. While high-calorie food images did elicit stronger responses than low-calorie food images in reward processing regions (caudate, insula, nucleus accumbens, putamen, amygdala), this was unaffected by the dopamine D3 receptor antagonist GSK598809. These results do not support a direct role of D3 receptor function on the processing of food reward images in individuals with binge eating. However, as noted by the authors, the task only assessed reward-cue responsivity and did not require reward learning processes which would rely more on the dopamine system. The second drug challenge study also measured fasted brain response to high- and low-calorie food images, but targeted the opioid system (Cambridge et al. 2013) and included individuals with BED rather than just binge eating behavior with no prior history of eating disorders. Compared to placebo, the mu-opioid receptor antagonist, GSK1521498, reduced both behavioral motivation to view high-calorie food images as well as right pallidum and putamen response to high-calorie food images. This provides evidence of the opioid system’s involvement in food-related motivational processes in BED. If the opioid system were to be targeted for treatment purposes as suggested by the authors, future studies should measure more direct effects on binge eating behaviors. A third study used the catecholamine-depleting agent, alpha-methyl-paratyrosine (AMPT), together with the monetary incentive delay (MID) task during fMRI in healthy controls and women with BN (Mueller et al. 2018). The results suggested that the BN group was less sensitive in terms of dopamine-dependent brain response and supported the notion of a dopamine downregulation in BN (Frank et al. 2011).
3 Positron Emission Tomography (PET) Imaging
Positron emission tomography (PET) imaging allows researchers to more directly probe the involvement of neurotransmitter systems, which are central to the rewarding effects of eating and have been shown to be altered in eating disorders (Frank and Kaye 2005; Bailer et al. 2013). A caveat is that those studies can tell about neurotransmitter receptor distribution and thus about up- or downregulation in numbers, but connecting those to brain response during tasks that test illness-specific pathophysiology has been more challenging. To date, only a few studies have utilized PET imaging in individuals diagnosed with BN or BED. Earlier studies showed elevated serotonin 1A receptor binding in BN when ill and after recovery, but lower serotonin 2A receptors compared to controls when recovered, and receptor binding was frequently associated with anxiety (Frank 2015). Serotonin receptors may have a specific impact on reward processing across psychiatric disorders and further study on how this pervasive neurotransmitter system is involved in binge eating warrants further study (Hayes and Greenshaw 2011). A study that investigated dopamine receptor binding did not show significant dopamine D2 receptor group differences between BN and controls, but striatal dopamine release was lower in BN, which was inversely associated with binge eating frequency (Broft et al. 2012). One study investigated striatal dopamine changes in 10 subjects who were obese with BED (OB BED) and eight subjects who were obese without BED (OB) (Wang et al. 2011). This crossover design study included 2 days of scanning. On the first day, participants completed a neutral condition scan with placebo and then a food-stimulation scan with oral methylphenidate (MPH) to block dopamine reuptake (i.e., enhance dopamine signaling). On the second day, they completed a food-stimulation scan with a placebo and then a neutral condition scan with MPH. Subjects fasted overnight before both scan days. In the food stimulation condition, subjects viewed and smelled fresh, warm food (selected based on prior subject preference ratings), and then tasted the food indirectly via cotton swabs. Only the OB BED group displayed significant increases in caudate and putamen in response to the food stimulation condition. Across both groups, greater binge eating scores, but not BMI, were associated with caudate dopamine increases in response to food stimulation. This provides further evidence of the importance of dopamine in BED reward processing and self-reported severity of binge eating behavior. It is likely that neurotransmitters and receptors are in part trait alterations that could contribute to the development of eating disorder behaviors including binge eating, but also adapt to the effects of behaviors and hinder recovery (Frank 2016). With the same food stimulation task, another PET study explored striatal dopamine changes and attitudes toward food, such as restraint and emotionality, in a small sample of ten healthy, nonobese, and non-BED subjects (Tomasi and Volkow 2013). The group found that increased dorsal striatum DA responsivity to food stimulation correlated with higher restraint scores. No significant correlations were found between striatal DA responsivity to food stimulation and BMI. The authors’ interpretation of these findings is that the increased DA changes signal greater saliency of the food stimuli and that those subjects utilize restrained eating as a compensatory strategy.
One other study measured regional cerebral blood flow (rCBF) with single photon emission tomography (SPECT) in three groups of adult women: eight subjects who were obese with BED (OB BED), 11 who were obese without BED (OB non-BED), and 12 healthy normal weight controls (Karhunen et al. 2000). Participants were scanned after an overnight fast once while viewing a control image of a landscape and on a second day while viewing a portion of real food which they selected. In the food exposure condition, the OB BED group exhibited a significantly greater increase in rCBF in the left frontal and prefrontal cortices compared to the OB non-BED and healthy controls. Furthermore, only the OB-BED group’s increase in hunger ratings, but not desire to eat, during food exposure correlated with greater left frontal and prefrontal rCBF. The prefrontal cortex’s role in reward expectancy, specifically the orbitofrontal cortex’s response to food reward value estimation, is therefore suggested to be potentially involved in BED. The inclusion of the OB non-BED comparison group is a strength of this study, although these particular control subjects had completed an active weight reduction program before scanning. Weight stability may be an important variable to control for in such a group (Frank et al. 2018c).
4 Limitations and Future Directions
When interpreting the rather small brain imaging literature on reward processing and binge eating behaviors, it is important to take several considerations into account. First, these studies used several different self-report questionnaires and combinations of scores, while others used a structured clinical interview to identify BED. Some applied DSM-IV criteria and other DSM-5. Because the DSM-5 requires reduced frequency (1 day a week instead of 2) and duration (3 months instead of 6) of binge eating to meet BN and BED criteria, earlier studies using DSM-IV criteria may include subjects with slightly more severe symptoms. Future studies should further clarify the potential relationships between binge eating symptom severity and neurobiological measures. Moreover, BMI was not correlated with brain function in several studies reviewed here, supporting the inclusion of nonobese individuals with BED in future work. Second, menstrual cycle phase was not consistently controlled for in the studies described here. Future investigations should take sex hormones into account given the evidence of structural and functional effects in areas of the brain that mediate reward processing, appetite, emotion, and cognition (Frank et al. 2018b). Third, not all the studies reviewed here included males with BED and none included men with BN. Significant effects of sex were not reported in these studies and sample sizes were too small to compare males and females within BED groups. Nevertheless, some evidence suggests sex differences in cortical response to food images and therefore emphasizes the need for further examination (Michaelides et al. 2012).
5 Conclusion
In summary, the still sparse literature on reward system function and binge eating yield some themes that deserve further exploration. Heightened response to visual food cues may indicate hyper-arousal to those stimuli and it could be tested in the laboratory and natural environment whether for instance mindfulness techniques could normalize such a response. Lower brain activation to taste stimuli, and especially to tasks where reward cues were received unexpectedly, point toward altered dopamine brain circuit function, which could become an important target for pharmacological intervention for binge eating. PET imaging and neurotransmitter receptor-specific drugs before fMRI can be used to study neurotransmitter circuits directly. The ideal solution may be multimodal imaging approaches that combine techniques and study binge eating pathophysiology across patient populations that exhibit that behavior to be able to identify specific brain circuit function that drives this behavior.
References
American Psychiatric Association (2013) Desk reference to the diagnostic criteria from DSM-5. American Psychiatric Publishing, Washington, DC
Avena NM (2013) Animal models of eating disorders. In: Avena NM (ed) Neuromethods, vol 74. Humana Press, Totowa, NJ, pp 281–290
Bailer UF, Frank GK, Price JC, Meltzer CC, Becker C, Mathis CA, Wagner A, Barbarich-Marsteller NC, Bloss CS, Putnam K, Schork NJ, Gamst A, Kaye WH (2013) Interaction between serotonin transporter and dopamine D2/D3 receptor radioligand measures is associated with harm avoidant symptoms in anorexia and bulimia nervosa. Psychiatry Res 211(2):160–168. https://doi.org/10.1016/j.pscychresns.2012.06.010
Balodis IM, Kober H, Worhunsky PD, White MA, Stevens MC, Pearlson GD, Sinha R, Grilo CM, Potenza MN (2013) Monetary reward processing in obese individuals with and without binge eating disorder. Biol Psychiatry 73(9):877–886. https://doi.org/10.1016/j.biopsych.2013.01.014
Balodis IM, Grilo CM, Kober H, Worhunsky PD, White MA, Stevens MC, Pearlson GD, Potenza MN (2014) A pilot study linking reduced fronto-striatal recruitment during reward processing to persistent bingeing following treatment for binge-eating disorder. Int J Eat Disord 47(4):376–384. https://doi.org/10.1002/eat.22204
Berridge KC (2009a) ‘Liking’ and ‘wanting’ food rewards: brain substrates and roles in eating disorders. Physiol Behav 97(5):537–550. https://doi.org/10.1016/j.physbeh.2009.02.044
Berridge KC (2009b) Wanting and liking: observations from the neuroscience and psychology laboratory. Inquiry (Oslo) 52(4):378. https://doi.org/10.1080/00201740903087359
Bodell LP, Wildes JE, Goldschmidt AB, Lepage R, Keenan KE, Guyer AE, Hipwell AE, Stepp SD, Forbes EE (2018) Associations between neural reward processing and binge eating among adolescent girls. J Adolesc Health 62(1):107–113. https://doi.org/10.1016/j.jadohealth.2017.08.006
Bohon C, Stice E (2011) Reward abnormalities among women with full and subthreshold bulimia nervosa: a functional magnetic resonance imaging study. Int J Eat Disord 44(7):585–595. https://doi.org/10.1002/eat.20869
Boswell RG, Kober H (2016) Food cue reactivity and craving predict eating and weight gain: a meta-analytic review. Obes Rev 17(2):159–177. https://doi.org/10.1111/obr.12354
Broft A, Shingleton R, Kaufman J, Liu F, Kumar D, Slifstein M, Abi-Dargham A, Schebendach J, Van Heertum R, Attia E, Martinez D, Walsh BT (2012) Striatal dopamine in bulimia nervosa: a PET imaging study. Int J Eat Disord 45(5):648–656. https://doi.org/10.1002/eat.20984
Cambridge VC, Ziauddeen H, Nathan PJ, Subramaniam N, Dodds C, Chamberlain SR, Koch A, Maltby K, Skeggs AL, Napolitano A, Farooqi IS, Bullmore ET, Fletcher PC (2013) Neural and behavioral effects of a novel mu opioid receptor antagonist in binge-eating obese people. Biol Psychiatry 73(9):887–894. https://doi.org/10.1016/j.biopsych.2012.10.022
Chase HW, Fournier JC, Bertocci MA, Greenberg T, Aslam H, Stiffler R, Lockovich J, Graur S, Bebko G, Forbes EE, Phillips ML (2017) A pathway linking reward circuitry, impulsive sensation-seeking and risky decision-making in young adults: identifying neural markers for new interventions. Transl Psychiatry 7(4):e1096. https://doi.org/10.1038/tp.2017.60
Craig AD (2009) How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci 10(1):59–70. https://doi.org/10.1038/nrn2555
Cuthbert BN (2014) Translating intermediate phenotypes to psychopathology: the NIMH research domain criteria. Psychophysiology 51(12):1205–1206. https://doi.org/10.1111/psyp.12342
Cyr M, Wang Z, Tau GZ, Zhao G, Friedl E, Stefan M, Terranova K, Marsh R (2016) Reward-based spatial learning in teens with bulimia nervosa. J Am Acad Child Adolesc Psychiatry 55(11):962–971.e3. https://doi.org/10.1016/j.jaac.2016.07.778
de Araujo IE, Kringelbach ML, Rolls ET, Hobden P (2003) Representation of umami taste in the human brain. J Neurophysiol 90(1):313–319. https://doi.org/10.1152/jn.00669.2002
Dodds CM, O’Neill B, Beaver J, Makwana A, Bani M, Merlo-Pich E, Fletcher PC, Koch A, Bullmore ET, Nathan PJ (2012) Effect of the dopamine D3 receptor antagonist GSK598809 on brain responses to rewarding food images in overweight and obese binge eaters. Appetite 59(1):27–33. https://doi.org/10.1016/j.appet.2012.03.007
Filbey FM, Myers US, Dewitt S (2012) Reward circuit function in high BMI individuals with compulsive overeating: similarities with addiction. NeuroImage 63(4):1800–1806. https://doi.org/10.1016/j.neuroimage.2012.08.073
Flagel SB, Clark JJ, Robinson TE, Mayo L, Czuj A, Willuhn I, Akers CA, Clinton SM, Phillips PE, Akil H (2011) A selective role for dopamine in stimulus-reward learning. Nature 469(7328):53–57. https://doi.org/10.1038/nature09588
Frank GK (2011) Reward and neurocomputational processes. Curr Top Behav Neurosci 6:95–110. https://doi.org/10.1007/7854_2010_81
Frank GK (2013) Altered brain reward circuits in eating disorders: chicken or egg? Curr Psychiatry Rep 15(10):396. https://doi.org/10.1007/s11920-013-0396-x
Frank GK (2015) Advances from neuroimaging studies in eating disorders. CNS Spectr 20:1–10. https://doi.org/10.1017/S1092852915000012
Frank GK (2016) The perfect storm—a bio-psycho-social risk model for developing and maintaining eating disorders. Front Behav Neurosci 10:44. https://doi.org/10.3389/fnbeh.2016.00044
Frank GK, Kaye WH (2005) Positron emission tomography studies in eating disorders: multireceptor brain imaging, correlates with behavior and implications for pharmacotherapy. Nucl Med Biol 32(7):755–761. https://doi.org/10.1016/j.nucmedbio.2005.06.011
Frank GK, Reynolds JR, Shott ME, O’Reilly RC (2011) Altered temporal difference learning in bulimia nervosa. Biol Psychiatry 70(8):728–735. https://doi.org/10.1016/j.biopsych.2011.05.011
Frank GK, Shott ME, Riederer J, Pryor TL (2016) Altered structural and effective connectivity in anorexia and bulimia nervosa in circuits that regulate energy and reward homeostasis. Transl Psychiatry 6(11):e932. https://doi.org/10.1038/tp.2016.199
Frank GKW, DeGuzman MC, Shott ME, Laudenslager ML, Rossi B, Pryor T (2018a) Association of brain reward learning response with harm avoidance, weight gain, and hypothalamic effective connectivity in adolescent anorexia nervosa. JAMA Psychiatry 75(10):1071–1080. https://doi.org/10.1001/jamapsychiatry.2018.2151
Frank GKW, Favaro A, Marsh R, Ehrlich S, Lawson EA (2018b) Toward valid and reliable brain imaging results in eating disorders. Int J Eat Disord 51(3):250–261. https://doi.org/10.1002/eat.22829
Frank GKW, Shott ME, DeGuzman MC, Smolen A (2018c) Dopamine D2 -141C Ins/Del and Taq1A polymorphisms, body mass index, and prediction error brain response. Transl Psychiatry 8(1):102. https://doi.org/10.1038/s41398-018-0147-1
Geliebter A, Ladell T, Logan M, Schneider T, Sharafi M, Hirsch J (2006) Responsivity to food stimuli in obese and lean binge eaters using functional MRI. Appetite 46(1):31–35. https://doi.org/10.1016/j.appet.2005.09.002
Geliebter A, Benson L, Pantazatos SP, Hirsch J, Carnell S (2016) Greater anterior cingulate activation and connectivity in response to visual and auditory high-calorie food cues in binge eating: preliminary findings. Appetite 96:195–202. https://doi.org/10.1016/j.appet.2015.08.009
Haber SN, Knutson B (2010) The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology 35(1):4–26. https://doi.org/10.1038/npp.2009.129
Hayes DJ, Greenshaw AJ (2011) 5-HT receptors and reward-related behaviour: a review. Neurosci Biobehav Rev 35(6):1419–1449. https://doi.org/10.1016/j.neubiorev.2011.03.005
Karhunen LJ, Vanninen EJ, Kuikka JT, Lappalainen RI, Tiihonen J, Uusitupa MI (2000) Regional cerebral blood flow during exposure to food in obese binge eating women. Psychiatry Res 99(1):29–42
Kelley AE, Berridge KC (2002) The neuroscience of natural rewards: relevance to addictive drugs. J Neurosci 22(9):3306–3311. https://doi.org/10.1523/JNEUROSCI.22-09-03306.2002
Kelley AE, Baldo BA, Pratt WE, Will MJ (2005) Corticostriatal-hypothalamic circuitry and food motivation: integration of energy, action and reward. Physiol Behav 86(5):773–795. https://doi.org/10.1016/j.physbeh.2005.08.066
Kessler RM, Hutson PH, Herman BK, Potenza MN (2016) The neurobiological basis of binge-eating disorder. Neurosci Biobehav Rev 63:223–238. https://doi.org/10.1016/j.neubiorev.2016.01.013
Lee JE, Namkoong K, Jung YC (2017) Impaired prefrontal cognitive control over interference by food images in binge-eating disorder and bulimia nervosa. Neurosci Lett 651:95–101. https://doi.org/10.1016/j.neulet.2017.04.054
Lloyd EC, Steinglass JE (2018) What can food-image tasks teach us about anorexia nervosa? A systematic review. J Eat Disord 6:31. https://doi.org/10.1186/s40337-018-0217-z
Michaelides M, Thanos PK, Volkow ND, Wang GJ (2012) Dopamine-related frontostriatal abnormalities in obesity and binge-eating disorder: emerging evidence for developmental psychopathology. Int Rev Psychiatry 24(3):211–218. https://doi.org/10.3109/09540261.2012.679918
Monteleone AM, Castellini G, Volpe U, Ricca V, Lelli L, Monteleone P, Maj M (2018) Neuroendocrinology and brain imaging of reward in eating disorders: a possible key to the treatment of anorexia nervosa and bulimia nervosa. Prog Neuropsychopharmacol Biol Psychiatry 80(Pt B):132–142. https://doi.org/10.1016/j.pnpbp.2017.02.020. Epub 2017 Mar 1
Mueller SV, Morishima Y, Schwab S, Wiest R, Federspiel A, Hasler G (2018) Neural correlates of impaired reward-effort integration in remitted bulimia nervosa. Neuropsychopharmacology 43(4):868–876. https://doi.org/10.1038/npp.2017.277
Ohmura Y, Tsutsui-Kimura I, Sasamori H, Nebuka M, Nishitani N, Tanaka KF, Yamanaka A, Yoshioka M (2019) Different roles of distinct serotonergic pathways in anxiety-like behavior, antidepressant-like, and anti-impulsive effects. Neuropharmacology:107703. https://doi.org/10.1016/j.neuropharm.2019.107703
Reiter AM, Heinze HJ, Schlagenhauf F, Deserno L (2017) Impaired flexible reward-based decision-making in binge eating disorder: evidence from computational modeling and functional neuroimaging. Neuropsychopharmacology 42(3):628–637. https://doi.org/10.1038/npp.2016.95
Rolls ET (2016) Functions of the anterior insula in taste, autonomic, and related functions. Brain Cogn 110:4–19. https://doi.org/10.1016/j.bandc.2015.07.002
Rolls BJ, Rolls ET, Rowe EA, Sweeney K (1981) Sensory specific satiety in man. Physiol Behav 27(1):137–142
Schafer A, Vaitl D, Schienle A (2010) Regional grey matter volume abnormalities in bulimia nervosa and binge-eating disorder. NeuroImage 50(2):639–643. https://doi.org/10.1016/j.neuroimage.2009.12.063
Schag K, Schonleber J, Teufel M, Zipfel S, Giel KE (2013) Food-related impulsivity in obesity and binge eating disorder—a systematic review. Obes Rev 14(6):477–495. https://doi.org/10.1111/obr.12017
Schienle A, Schafer A, Hermann A, Vaitl D (2009) Binge-eating disorder: reward sensitivity and brain activation to images of food. Biol Psychiatry 65(8):654–661. https://doi.org/10.1016/j.biopsych.2008.09.028
Setsu R, Hirano Y, Tokunaga M, Takahashi T, Numata N, Matsumoto K, Masuda Y, Matsuzawa D, Iyo M, Shimizu E, Nakazato M (2017) Increased subjective distaste and altered insula activity to umami Tastant in patients with bulimia nervosa. Front Psychiatry 8:172. https://doi.org/10.3389/fpsyt.2017.00172
Simon JJ, Skunde M, Walther S, Bendszus M, Herzog W, Friederich HC (2016) Neural signature of food reward processing in bulimic-type eating disorders. Soc Cogn Affect Neurosci 11(9):1393–1401. https://doi.org/10.1093/scan/nsw049
Tomasi D, Volkow ND (2013) Striatocortical pathway dysfunction in addiction and obesity: differences and similarities. Crit Rev Biochem Mol Biol 48(1):1–19. https://doi.org/10.3109/10409238.2012.735642
Uddin LQ, Nomi JS, Hebert-Seropian B, Ghaziri J, Boucher O (2017) Structure and function of the human insula. J Clin Neurophysiol 34(4):300–306. https://doi.org/10.1097/WNP.0000000000000377
Vitousek K, Manke F (1994) Personality variables and disorders in anorexia nervosa and bulimia nervosa. J Abnorm Psychol 103(1):137–147
Voon V, Morris LS, Irvine MA, Ruck C, Worbe Y, Derbyshire K, Rankov V, Schreiber LR, Odlaug BL, Harrison NA, Wood J, Robbins TW, Bullmore ET, Grant JE (2015) Risk-taking in disorders of natural and drug rewards: neural correlates and effects of probability, valence, and magnitude. Neuropsychopharmacology 40(4):804–812. https://doi.org/10.1038/npp.2014.242
Wagner A, Barbarich-Marsteller NC, Frank GK, Bailer UF, Wonderlich SA, Crosby RD, Henry SE, Vogel V, Plotnicov K, McConaha C, Kaye WH (2006) Personality traits after recovery from eating disorders: do subtypes differ? Int J Eat Disord 39(4):276–284. https://doi.org/10.1002/eat.20251
Wang GJ, Geliebter A, Volkow ND, Telang FW, Logan J, Jayne MC, Galanti K, Selig PA, Han H, Zhu W, Wong CT, Fowler JS (2011) Enhanced striatal dopamine release during food stimulation in binge eating disorder. Obesity (Silver Spring) 19(8):1601–1608. https://doi.org/10.1038/oby.2011.27
Weygandt M, Schaefer A, Schienle A, Haynes JD (2012) Diagnosing different binge-eating disorders based on reward-related brain activation patterns. Hum Brain Mapp 33(9):2135–2146. https://doi.org/10.1002/hbm.21345
Wierenga CE, Ely A, Bischoff-Grethe A, Bailer UF, Simmons AN, Kaye WH (2014) Are extremes of consumption in eating disorders related to an altered balance between reward and inhibition? Front Behav Neurosci 8:410. https://doi.org/10.3389/fnbeh.2014.00410
Wonderlich JA, Breithaupt L, Thompson JC, Crosby RD, Engel SG, Fischer S (2018) The impact of neural responses to food cues following stress on trajectories of negative and positive affect and binge eating in daily life. J Psychiatr Res 102:14–22. https://doi.org/10.1016/j.jpsychires.2018.03.005. Epub 2018 Mar 14.PMID: 29558632
Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich HC (2016) Reward-related decision making in eating and weight disorders: a systematic review and meta-analysis of the evidence from neuropsychological studies. Neurosci Biobehav Rev 61:177–196. https://doi.org/10.1016/j.neubiorev.2015.11.017
Xia L, Gu R, Zhang D, Luo Y (2017) Anxious individuals are impulsive decision-makers in the delay discounting task: an ERP study. Front Behav Neurosci 11:5. https://doi.org/10.3389/fnbeh.2017.00005
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
DeGuzman, M., Frank, G.K.W. (2020). Neuroimaging to Study Brain Reward Processing and Reward-Based Learning in Binge Eating Pathology. In: Frank, G., Berner, L. (eds) Binge Eating. Springer, Cham. https://doi.org/10.1007/978-3-030-43562-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-43562-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43561-5
Online ISBN: 978-3-030-43562-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)