Abstract
Ethanol is the most widely detected drug in both postmortem and human performance forensic toxicology. After ingestion, ethanol is absorbed into the body primarily by passive diffusion in the small intestine. It is distributed throughout the body according to the water content of the fluid or tissue and is eliminated mainly by metabolism in the liver by oxidation. The pharmacokinetics of ethanol is best described by Michaelis-Menten kinetics. The primary effect of ethanol is central nervous system depression, and the extent of the depression is roughly correlated with the blood ethanol concentration. Tolerance, both dispositional and cellular, plays a key role in the individual differences to the effects of alcohol. Ethanol is quantitated in blood specimens by enzymatic or gas chromatographic methods; ethanol is measured in breath specimens by infrared spectrophotometric or electrochemical methods. Testing for ethanol in postmortem specimens may be affected by postmortem production of ethanol in blood specimens. Mandatory testing of ethanol in suspected drunk driving cases and in the workplace at established limits has been accepted as an important component of public safety.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Alcohol, which is better known to chemists and toxicologists as ethanol (CH3CH2OH), is the psychoactive substance most commonly encountered in forensic toxicology casework when blood or other body fluids from living and deceased persons are analyzed. Ethanol tops the list of drugs identified in medical examiner or coroner cases, impaired drivers (traffic cases), drug-facilitated sexual assaults, as well as workplace accident investigations. Between 20 and 50% of all drivers killed in road-traffic crashes, according to various epidemiological surveys, had been drinking alcohol before the crash, and their blood alcohol concentration (BAC) at autopsy exceeded the statutory alcohol limit for driving.
Ethanol is probably man’s oldest psychoactive drug and is produced in nature by microbial fermentation of sugars contained in fruits, honey, or other vegetable matter. Alcohol is a legal drug and is available for purchase by adults almost without any restrictions. Moderate drinking, such as 10–20 g ethanol daily (1–2 drinks), has no detrimental effects on a person’s health or well-being, and there is growing evidence that this amount, especially in the form of red wine, has a protective effect against cardiovascular diseases, such as stroke. Unfortunately, for about 10% of the population, especially among men, initial moderate drinking escalates into overconsumption and abuse of alcohol, with serious consequences for the individual, the family, and society as a whole.
Efforts to prevent alcohol-related problems have a long history, and one example is the enactment of prohibition during the first decades of the twentieth century in the USA. Examples of medical complications caused by excessive drinking are disease of the liver (hepatitis, cirrhosis), acute and chronic pancreatitis, gout, various cancers, and cardiomyopathy. The prevalence and deaths from these medical conditions are highly correlated with total alcohol consumption in society.
Classification of Alcohols
Textbooks devoted to organic chemistry classify alcohols according to their chemical structure, such as carbon chain length, the degree of branching, or the number of hydroxyl groups (-OH) contained in each molecule. Alcohols with one hydroxyl group are referred to as monohydroxy (e.g., ethanol and methanol), and two hydroxyl groups are dihydroxy (e.g., ethylene glycol), whereas glycerol is a trihydroxy alcohol and mannitol and sorbitol are polyhydroxy alcohols. The various aliphatic alcohols are also denoted as primary (ethanol), secondary (isopropanol), or tertiary (t-butanol), depending on whether one, two, or three alkyl groups are bonded to the saturated carbon atom containing the hydroxyl (-OH) radical.
Examples of the alcohols commonly encountered in clinical and forensic toxicology are shown in Table 19.1 along with their main physicochemical properties and toxic metabolites formed in the body during metabolism in the liver.
In general, the narcotic effects of aliphatic alcohols on cell membranes increase with the number of carbon atoms in the molecule, with the notable exception of methanol (CH3OH). Methanol is commonly referred to as wood alcohol because it was originally made from the distillation of wood under vacuum. Although methanol is comparable with ethanol in terms of its acute intoxicating effects, wood alcohol is much more dangerous, owing to toxicity of its metabolites, namely, formaldehyde and formic acid (Table 19.1). Another common alcohol is isopropanol, or rubbing alcohol , widely used in clinics as an antiseptic to clean the skin before taking blood samples. The additional carbon atom in isopropanol makes it more lipid-soluble and easier to penetrate cell membranes giving a greater depression of the central nervous system. Occasionally, chronic alcoholics resort to drinking industrial alcohol products that contain more toxic alcohols, such as methanol or isopropanol, in addition to varying amounts of ethanol.
Another toxic alcohol encountered in clinical and forensic toxicology is the sweet-tasting solvent ethylene glycol, which is a major component of antifreeze. The two hydroxyl groups in ethylene glycol are oxidized successively by hepatic enzymes, first to aldehydes (-CHO) and then carboxylic acids (-COOH), and the end product of metabolism is oxalic acid (Table 19.1). Oxalic acid can react with intracellular calcium ions to produce insoluble calcium oxalate crystals, which get trapped in the kidney tubuli eventually causing renal failure and death. In a poisoned patient, the analysis of ethylene glycol and/or its metabolites in body fluids and extent of metabolic acidosis furnish proof of toxic alcohol ingestion. In medical examiner cases, ethylene glycol fatalities are often recognized from presence of calcium oxalate crystals in sections of the kidney or from presence of these crystals in the urine when examined under polarized light.
Because the boiling point of ethylene glycol (197 oC) is much higher than that of ethanol (78 oC), methanol (65 oC), and isopropanol (82 oC), this aliphatic diol is not identified in biological specimens during routine gas chromatography (GC) analysis of volatiles. Ethylene glycol is usually determined by an enzymatic method (e.g., with glycerol dehydrogenase) or after protein precipitation and direct injection into a GC instrument fitted with a flame ionization detector (FID) or by GC-FID after making a suitable chemical derivative, such as the phenyl boronate ester.
On entering the bloodstream, primary alcohols are oxidized in the liver to aldehydes, whereas secondary alcohols, such as isopropanol, are converted into ketones, such as acetone. Tertiary alcohols are resistant to oxidation and usually undergo phase II conjugation reactions forming glucuronides, which are excreted in the urine. The method used to determine ethanol in blood and other body fluids must be able to distinguish acetone, isopropanol, and methanol, which are commonly encountered together with ethanol in forensic casework.
Production of Alcoholic Beverages
The initial step in the production of alcoholic beverages is fermentation, which is one of the oldest known organic reactions dating back ~3000 years. Fermentation requires adding yeast to an aqueous solution of some carbohydrate substrate, and one molecule of a six-carbon sugar, such as glucose, is converted into two molecules of ethanol and two molecules of carbon dioxide.
Any natural product with sufficient amounts of starch or sugar can undergo fermentation by the enzymes contained in yeast or by other microorganism depending on appropriate conditions of temperature and time. Brewer’s yeast (Saccharomyces cerevisae) has been around for a long time and is a type of fungus. During the fermentation process, ethanol concentrations up to 12–14 vol% are produced, whereas on reaching higher concentrations, the yeast is inactivated and the fermentation stops. Beverages with higher concentrations of ethanol are produced by distillation or by spiking fermented drinks with extra ethanol.
In addition to ethanol and water, alcoholic beverages contain small amounts of other substances broadly classified as congeners, which according to the Oxford English Dictionary means one of the same kind, allied in nature or origin. Accordingly, congeners are other types of alcohols (e.g., methyl, pentyl, or amyl), aldehydes, and ketones as well as other low-molecular-weight substances that might be produced during the fermentation process, depending on source and type of raw materials used. Other congeners are imparted when fermented or distilled beverages are stored in oak casks during the aging process prior to bottling.
The congeners contribute to the smell and taste and give color to certain types of alcoholic beverage, such as whisky or cognac. The “cleanest” alcoholic drink in terms of low congener content is vodka, which after distillation is filtered through activated charcoal to remove any trace impurities. Distilled alcoholic beverages usually contain 40–60 vol% ethanol (80–120 proof), and in some nations this alcohol content is regulated by statute. Beers might contain from 4 to 12 vol% alcohol depending on the manufacturing process, whereas table wines are 8–14 vol%, and fortified wines 14–24 vol% ethanol. The so-called alcohol-free beers, which are widely available, are usually about 1 vol% or less, which makes these drinks safe to consume by drivers and others engaged in safety-sensitive work.
Fate of Alcohol in the Body
Absorption
Absorption describes the process by which a drug or poison (e.g., alcohol) passes from outside the body into the bloodstream. The oral route of administration (by mouth or drinking) is how drinks are consumed in real-life situations. However, in emergency medicine sterile solutions of ethanol in saline (8–10 vol%) might be administered intravenously to treat patients admitted to hospital poisoned from drinking methanol or ethylene glycol. High blood alcohol concentrations can also be reached after rectal administration.
The absorption of alcohol into the portal venous blood starts already in the stomach, but the rate of uptake is much faster when the stomach contents empty into the duodenum and jejunum, owing to the much larger surface area provided by the villi and microvilli that project from the surface of the mucosa of the small intestines. Accordingly, factors influencing gastric emptying have a major influence on the rate of absorption of ethanol into the bloodstream. A more rapid rate of absorption is associated with a higher and earlier occurring peak blood concentration (Cmax) and thus a greater impairment of the central nervous system.
Small amounts of ethanol might be absorbed into the blood via the dermal route (intact skin) or by inhalation through the lungs, although these methods are ineffective in elevating the BAC above 0.01 g/100 mL. The slow absorption through the skin is balanced by simultaneous metabolism in the liver at a rate of 7–8 g/hour. If the skin is damaged with cuts or abrasions and there are open blood vessels, this might enhance uptake, but this is still not an effective way to increase the BAC. The absorption of ethanol into the bloodstream by inhalation via the lungs depends on the concentration in the ambient air breathed and the degree of lung ventilation. However, even under extreme conditions when concentrations in the inhaled air are high, this is not a practical way to increase a person’s BAC owing to ongoing metabolism of any absorbed ethanol.
Because absorption is a passive diffusion process, one can expect that ethanol contained in distilled liquors (40 vol%) is absorbed faster than ethanol in wine (10 vol%) or beer (5 vol%), as predicted by Fick’s principle. However, this simple rule is offset by the fact that beers and wines, as well as fruit brandies, contain sugars and other constituents that delay gastric emptying. The type of mixer used with spirit drinks also impacts on speed of absorption by delaying gastric emptying. The ethanol in carbonated (CO2) beverages, such as champagne, seems to be absorbed faster than decarbonated drinks with the same alcohol content, such as white wine. When neat spirits are consumed on an empty stomach, this often irritates the gastric mucosa and results in a pyloric spasm, which leads to a delayed gastric emptying and a slower rate of absorption of ethanol into the blood.
The results from hundreds of controlled drinking studies show that peak BAC occurs at between 10–120 min after end of drinking and on average after about 60 min. However, in social drinking situation, when multiple drinks are consumed over longer time periods, the absorption takes place progressively as more and more alcohol is consumed and the peak concentration in blood is reached earlier, usually within 30 min after cessation of drinking. Figure 19.1 gives examples of blood alcohol curves obtained from experiments with N = 16 healthy men after they drank a standard dose of alcohol (0.85 g/kg) as neat whisky on an empty stomach in 25 min. These BAC curves show the magnitude of intersubject variation, which is greatest during the absorption phase as reflected in variations in Cmax and tmax before the post-absorptive phase starts at about 60–90 min post-drinking.
Some absorption of alcohol occurs through the mucous surfaces of the stomach, but the bulk of the dose administered is absorbed via the upper part of the small intestine. Estimates of the relative amounts of ethanol absorbed from the stomach (20%) and intestines (80%) are only approximate because much depends on stomach emptying, such as presence of food in the stomach before drinking, the type of beverage consumed, and use of certain prescription drugs. Absorption of ethanol from different parts of the gastrointestinal (GI) tract depends on the concentration present in the individual structures, the blood flow (vascularity), and the absorption surface area.
Factors that increase GI motility will increase the rate of ethanol absorption into the blood, and a delayed gastric emptying (gastroparesis) decreases the absorption of ethanol. Inflammation of the GI tract, for example, increases blood flow to that region resulting in a more rapid absorption of alcohol. Prokinetic drugs increase gastric motility (e.g., cisapride or metaclopramide) and lead to a faster rate of absorption of ethanol into the portal blood. Heavy cigarette smoking delays gastric emptying and slows rate of ethanol absorption. However, the single most important factor delaying the absorption of ethanol is the presence of food in the stomach such as when alcohol is consumed immediately after eating a large meal. The amount of food eaten seems more important than its composition in terms of protein, fat, or carbohydrate content. Figure 19.2 shows blood alcohol curves obtained when the same dose of ethanol (0.8 g/kg) was consumed on an empty stomach (overnight fast) or immediately after eating a standardized breakfast.
The peak concentration of ethanol in blood was higher and occurred earlier when ethanol was consumed on an empty stomach compared with the same dose after eating a meal. Food mixes with and dilutes the concentration of ethanol in the stomach so that it remains unabsorbed for a much longer time. The BAC curve obtained in the fed state gives the impression that a smaller dose of ethanol had been administered, but this was not the case (Fig. 19.2). It seems that food not only lowers the bioavailability of ethanol but also increases the rate of metabolism as reflected in a smaller area under the curve and a shorter time to reach zero BAC. For the most part, the rate of ethanol metabolism is independent of the concentration in blood provided the oxidative enzymes are saturated with substrate (BAC > 0.02–0.03 g/100 mL).
Eating a meal increases hepatic blood flow, and consequently there is a more effective clearance of ethanol, which is one mechanism that helps to explain the food effect. This was demonstrated when subjects eat a meal when the alcohol was given by intravenous infusion, thus sidestepping any influence of gastric emptying. Some investigators suggested that when alcohol is retained in the stomach for longer, such as when drinking and eating occurs, a larger amount undergoes pre-systemic metabolism owing to alcohol dehydrogenase located in the gastric mucosa.
Distribution
After absorption into the portal venous blood, ethanol is transported first to the liver, then the right side of the heart, and to the lungs, before oxygenated blood returns to the left side of the heart and transported throughout the whole body. When blood enters the pulmonary circulation, some of the ethanol in solution diffuses across the alveolar-capillary membrane and is exhaled in the breath. This forms the basis of the widely used breath alcohol test, which will be covered in more detail later in this chapter. During the absorption phase, the concentration of ethanol in alveolar air and hence in the expired air runs closer to the arterial blood concentration rather than the venous blood concentration. Tissues that are initially free of alcohol extract alcohol from the arterial blood so that the venous blood returning to the heart with deoxygenated blood has a lower concentration of alcohol.
The magnitude of the arterial-venous (A-V) difference in alcohol content is greatest when a bolus dose is consumed on an empty stomach. After the end of drinking, the magnitude of the A-V difference progressively decreases and eventually becomes zero (A = V), which marks the point when ethanol is fully absorbed and distributed in all body fluids and tissues. Studies have shown that venous blood contains a slightly higher concentration of ethanol than arterial blood during the post-absorptive elimination phase of the BAC curve.
The speed of equilibration of ethanol between blood and other body fluids and tissues depends on the ratio of blood flow to tissue mass, which means that organs with a rich blood supply, such as the brain and kidneys, rapidly equilibrate with the concentration of ethanol in arterial blood, whereas bulky skeletal muscles, with lower ratio of blood flow to tissue mass, require a longer time to equilibrate. Body fluids containing more water than blood (e.g., saliva, vitreous humor, and urine) will also have higher concentration of ethanol when equilibration is reached.
An important concept in pharmacokinetics is how a drug distributes between the blood or plasma and the other tissues of the body. Known as volume of distribution (Vd), this important pharmacokinetic parameter relates the concentration of a drug in the blood or plasma to the total amount of drug in the body. A drug’s Vd depends on lipid solubility and the degree of binding to plasma proteins. From a knowledge of Vd, it is easy to calculate the amount of drug absorbed and distributed in all body fluids and tissues from the concentration determined in a sample of blood. The Vd for a water-soluble drug like ethanol depends on the person’s age and gender and the proportion of fat to lean tissue in the body.
Total body water (TBW) comprises about 60% of body weight in men and 50% in women as determined by isotope dilution experiments. The Vd for ethanol varies twofold between individuals from a low of 0.4–0.5 L/kg in obese females to a high of 0.7–0.8 L/kg in lean male subjects. Results from drinking experiments show in average values of Vd of 0.7 L/kg in healthy adult men and 0.6 L/kg in healthy adult women. The water content of blood is easy to determine by desiccation or freeze-drying and is ~80% w/w with a small but statistically significant gender difference, owing to lower hematocrit (less red cells and more plasma) in female blood.
Because ethanol distributes into the water fraction of all body fluids, the distribution ratio of ethanol between the blood and the body as a whole should be similar to distribution of water, namely, 60/80 or 0.75 for men and 50/80 or 0.62 for women. In practice, much depends on body composition, especially the amount of adipose tissue in relation to fat-free mass. A clinical measure of obesity is given by body mass index (BMI) calculated as ratio of body weight in kg to height in meters squared (kg/m2). A person with BMI 30 kg/m2 can be expected to have a lower ethanol Vd than a person with normal BMI of 20–25 kg/m2.
Blood consists of the straw-colored plasma (92 % w/w water) and red cells (erythrocytes) which are 68% w/w water. This suggests a plasma/blood distribution ratio of ethanol of 1.15:1 (92/80 = 1.15) and a red cell/blood ratio of 0.85 (68/80 = 0.85) depending in part on hematocrit and lipid content of the blood specimen. Most people can be expected to have plasma/blood distribution ratio of ethanol ranging from 1.1:1 to 1.2:1 depending on state of health. In people suffering from anemia (low hematocrit) with more plasma (and water) per unit volume of blood, the plasma/blood distribution of ethanol should be closer to 1.10:1 or lower. Plasma and serum contain the same amount of water, and therefore the same amount of ethanol and ethanol distribution ratios are the same.
If a clinical laboratory reports a serum ethanol concentration of 0.1 g%, then for forensic purposes, the expected concentration in whole blood is 0.087 g/100 mL (0.1/1.15 = 0.086) and might range from 0.083 g/100 ml (0.1/1.2) to 0.091 g/100 mL (0.1/1.1). The results from analysis of ethanol in plasma and serum done at hospital clinical chemistry laboratories cannot be used for legal purposes without making this conversion to the expected concentration in whole blood.
The distribution of ethanol between blood and other biological fluids and tissues has been extensively studied, and the values depend on water content of specimens and the time after drinking when samples are taken. Results from many such studies are summarized in Table 19.2 if samples are taken after absorption and distribution is complete. The concentrations in vitreous humor, saliva, spinal fluid, and urine are 15–20% higher than in an equal volume of blood as expected from differences in water content. However, in practice the distribution ratios of ethanol between CSF and blood and urine and blood are higher (1.3:1), because of a lag time in the formation of these alternative body fluids. Concentrations of ethanol in the liver, kidney, and brain are less than in blood in part because of lower water content in these tissues and the fact some are metabolically active after death, leading to a decrease in the concentrations of ethanol.
Metabolism
More than 90% of the dose of ethanol consumed undergoes oxidative metabolism in the liver by various enzymatic reactions as shown in Fig. 19.3. The first step involves oxidation of ethanol to acetaldehyde, and this reaction is catalyzed by a cytosolic enzyme alcohol dehydrogenase (ADH). ADH is polymorphic, and various isozymes exist with slightly different amino acid sequences and kinetic properties (Vmax and km), which might account for individual differences in rates of ethanol metabolism. Zinc is a necessary element for enzyme activity of alcohol dehydrogenase. During oxidative metabolism of ethanol, the cofactor nicotinamide adenine dinucleotide (NAD+) is simultaneously reduced to NADH and the reoxidation of NADH to NAD+ is the rate-limiting step in the overall redox reaction.
Acetaldehyde is a toxic and highly reactive substance, but luckily the primary metabolite of ethanol is rapidly oxidized to acetic acid by the action of low km aldehyde dehydrogenase (ALDH) located in the mitochondria. The acetate becomes transported with blood away from the liver and enters the aerobic respiration process (citric acid cycle) eventually being breakdown to end products carbon dioxide and water. The oxidative metabolism of ethanol via the ADH and ALDH pathway is the primary route of alcohol elimination from the body. However, in the early 1960s it was discovered that the smooth endoplasmic reticulum of liver cells contained an enzyme that oxidized ethanol denoted microsomal ethanol oxidizing system (MEOS). MEOS formed part of the cytochrome P450 family of enzymes, and CYP2E1 was the variant mainly responsible for oxidation of ethanol. The same P450 enzyme is responsible for metabolism of certain drugs such as acetaminophen and chlorinated and aromatic hydrocarbons. The P450 system is inducible after chronic exposure to substrate, which accounts for the finding that some alcoholics during detoxification have higher rates of metabolism of ethanol compared with occasional drinkers.
Non-oxidative Metabolism
Considerable research has focused on non-oxidative metabolites of ethanol (Fig. 19.4). A small fraction of the dose of ethanol ingested (0.1–0.2%) undergoes phase II conjugation reactions to give ethyl glucuronide (EtG) and ethyl sulfate (EtS) as metabolites via glucuronosyltransferase and sulfotransferase enzymes, respectively. EtG and EtS are detectable in blood and urine for considerably longer than ethanol itself and can serve as biomarkers to disclose recent drinking after ethanol has been eliminated from the body. However, care is needed when results of EtG are interpreted because ethanol is a constituent of many household products, such as mouthwash, cosmetics, cough medication, hand sanitizers, etc. This requires use of conservative and reasonable cutoff concentration when urinary EtG is analyzed and reported, such as 100–500 ng/mL (0.1–0.5 mg/L). Lower cutoffs are acceptable for EtS, such as 25–100 ng/mL (0.025–0.1 mg/L), before a person is accused of drinking alcoholic beverages.
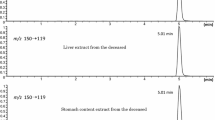
Analysis of EtG and EtS finds applications in postmortem toxicology to distinguish ethanol produced during decomposition from antemortem ingestion of alcoholic beverages. If EtG and/or EtS conjugates are verified present in postmortem blood or urine, this speaks toward consumption of alcoholic beverages during life. Ethanol must undergo metabolism to produce these conjugates and must therefore have passed through the liver as opposed to being produced after death by action of bacteria or yeasts.
Another non-oxidative metabolite of ethanol is phosphatidylethanol (PEth), which is formed in a reaction between ethanol and phosphatidylcholine and the enzyme phospholipase D. PEth also remains elevated after ethanol has been cleared from the bloodstream. However a heavier drinking period is needed to produce elevated levels of PEth compared with EtG and EtS.
Ethanol undergoes an enzymatic reaction with both saturated and unsaturated fatty acids (e.g., palmitic, linoleic, stearic, etc.) to give fatty acid ethyl esters (FAEE). The incorporation of FAEE into various body organs (the heart, brain, and pancreas) has been suggested as a possible mechanism for alcohol-related tissue damage, which is often seen in chronic alcoholics. FAEE can also be determined in hair strands and used to monitor abstinence in people required to refrain from drinking for various reasons.
Excretion
Excretion refers to the removal of ethanol from the body in an unchanged form and this occurs via the lungs (in breath), the kidney (in urine), and through the skin (in sweat). However, all three routes of excretion combined account for at most 5–10% of the dose of ethanol administered. Ethanol can also be detected in the saliva, which however is usually swallowed and then reabsorbed into the blood.
Urine has a long history as a biological specimen for forensic analysis of alcohol because large volumes are available. In the past, the urine alcohol concentration (UAC) was used to estimate the BAC, but this conversion is not advisable owing to large variations in the UAC/BAC ratio depending on sampling time after end of drinking. Concentration-time profiles of ethanol in blood and bladder urine are shown in Fig. 19.5 when 0.85 g ethanol/kg body weight was consumed as neat whisky on an empty stomach. Note that after a bolus dose the concentration in urine is less than in blood during the absorption phase and higher than in blood after about 100 min and remains higher for the duration of the post-absorptive period. The insert graph shows the ethanol-induced dieresis, which is greatest (6 mL per min) during the absorption phase of the blood alcohol curve returning to normal (~1 mL per min) during the post-absorptive period.
The physiological principles of ethanol excretion in urine are well known, and as renal artery blood enters the kidney, about 20% is filtered at the glomerulus. Most of this filtrate is reabsorbed, with <1% of the filtrate being excreted as urine in the bladder. Analysis of near simultaneous samples of blood and bladder urine shows that UAC/BAC concentration ratios range from 1.2 to 1.3 after absorption of alcohol is complete. However, individual ratios vary widely depending on status of absorptive and the time of storage of urine in the bladder before voiding. Blood ethanol decrease by metabolism as urine is produced, whereas there is no metabolism in urine after it collects in the bladder. During the absorptive phase of the BAC curve, UAC/BAC ratio is <1.0, and during the post-absorptive phase, the concentration in urine is 25–30% higher than in blood. The variations in urine to blood concentration ratios for an individual in the post-absorptive phase can be so large that it is generally considered unacceptable to estimate a blood ethanol concentration from the ethanol concentration of a randomly collected urine specimen. Better correlations are obtained for ethanol in urine and blood when two consecutive urine specimens are collected. The second voided specimen, collected 30–60 min after the first, shows a closer correlation with BAC and the average UAC/BAC is about 1.3:1.
Pharmacokinetics
Pharmacokinetics is concerned with absorption, distribution, metabolism, and excretion (ADME) of drugs and how these processes can be described in quantitative terms. The Swedish scientist Erik MP Widmark (1889–1945) made extensive studies of ADME of ethanol in the 1930s when he plotted BAC time profiles and used these to derive a set of alcohol parameters for controlled drinking conditions. A Widmark-type BAC curve is shown in Fig. 19.6 along with the pharmacokinetic parameters of ethanol C0, Cmax, tmax, β, min0, and rho.
A male subject drank a moderate dose of ethanol (0.8 g/kg) on an empty stomach in 30 min. The peak concentration in (Cmax) and time of reaching the peak tmax are read directly from the graph. At about 80 min post-dosing after Cmax is reached, the BAC decreases at a constant rate per unit time in accordance with zero-order saturation kinetics. The slope of this rectilinear elimination part of the BAC profile is determined from the dashed diagonal line in Fig. 19.6 denoted β-slope with y-intercept C0 (g/100 mL) and x-intercept min0 (min or h), where C0/min0 = β (g/100 mL per h). In the example shown, the rate of ethanol elimination from blood (β-slope) was 0.014 g/100 mL per h. The other important pharmacokinetic parameter is distribution volume of ethanol derived from the ratio of alcohol in the entire body (g/kg) to concentration in the blood at time zero given by C0 (g/L). This latter parameter is the concentration of ethanol in blood that would be obtained if the entire dose was absorbed and distributed in the body before any metabolism occurred. In Fig. 19.6 the volume of distribution (Vd) was calculated to be 0.70 L/kg and represents a good average for male subjects.
On reaching low concentrations of ethanol in blood (< 0.01–0.02 g/100 mL), the ADH metabolizing enzyme is no longer saturated with substrate and zero-order kinetics change to first-order kinetics. The entire post-absorptive elimination phase from high to low concentrations is best described by saturation kinetics described mathematically by the Michaelis-Menten equation. Table 19.3 compares the properties of zero-order, first-order, and Michaelis-Menten kinetics when applied to BAC profiles.
The Michaelis constant (km) for human class I ADH is about 0.005–0.01 g/100 mL. Table 19.3 shows that if the Michaelis constant is much greater than the substrate concentration (BAC), the equation collapses into first-order kinetics. In contrast, if the substrate concentration (BAC) is much greater than the Michaelis constant (e.g., > 0.02 g/100 mL), elimination kinetics of ethanol are adequately described by zero-order kinetics.
The results from many alcohol dosing studies show that the average elimination rate of ethanol from blood is 0.015 g/100 mL per hour for men and 0.018 g/100 mL per hour for women. Several factors can affect this elimination rate. Enhanced rates of ethanol elimination from blood are likely in alcoholics during detoxification owing to a process of enzyme induction involving CYP2E1. Genetic factors may also be involved in controlling rates of metabolism, as seen in some ethnic groups such as Asians with slightly faster elimination rates of ethanol from blood compared with Caucasians. Because most of the ethanol consumed is eliminated in the liver, any disease state in that tissue can potentially impair the clearance of ethanol. Administration of fructose, glycine, or alanine may enhance ethanol elimination. Recent work has suggested that food, as well as affecting the absorption of ethanol, might slightly enhance the elimination of ethanol.
There is some evidence that metabolism of ethanol occurs in the gastric mucosa before the blood reaches the liver, which would contribute to the observed first-pass metabolism (FPM) of ethanol when drinking occurs after a meal. The relative importance of FPM and whether this occurs in the liver or stomach or both organs is still an open question although most investigators seem to consider it more important in part because of the greater amount of oxidative enzyme present. The area under the BAC curve is smaller when the same dose is administered orally compared with intravenously which indicates a lower systemic availability. Gastric ADH would facilitate metabolism of some of ethanol the longer it remains unabsorbed in the stomach. This implies that any drug that affects the activity of gastric ADH impacts on the FPM of ethanol. Drugs such as cimetidine and ranitidine, which inhibit the activity of gastric ADH, are therefore expected to allow more of the dose of ethanol to become absorbed into the blood, thus increasing the bioavailability. Activity of gastric ADH also varies as a function of age and gender and also between different racial groups. With all these factors to consider, it is not surprising that the absorption phase of the BAC curve shows large intersubject variations and speaks against making predictions of BAC expected after a given dose.
The Widmark Equation
Blood alcohol curves are characterized by a rising phase mainly reflecting the absorption process which initially occurs faster than elimination through metabolism and excretion. As time passes and amount of alcohol that is still unabsorbed decreases, the BAC eventually reaches a peak or maximum concentration usually at 30–90 min post-drinking. At this time the rates of absorption and metabolism are now about equal. During the post-absorptive declining portion of the BAC curve, absorption has already ended and elimination is the dominant process.
The relationship between a person’s blood alcohol concentration and the amount of alcohol in the body has been thoroughly investigated and is expressed by the well-known Widmark equation :
A(g) = BAC(g/L) × body weight (kg) × Vd or rho (L/kg)
In the above equation, A is amount of alcohol (g) absorbed and distributed in all body fluids and tissues at the time of sampling blood, BAC is the blood alcohol concentration in g/L (g/100 mL × 10), and Vd is the apparent volume of distribution (rho factor = L/kg), which expresses the ratio of ethanol concentration in the whole body (g/kg) to that in the blood (g/L).
Blood alcohol calculations are commonly requested when alcohol-related crimes are investigated, such as driving under the influence of alcohol. For example, if a male person (Vd = 0.7 L/kg) with a body weight of 80 kg has a BAC of 0.1 g/100 mL, then 56 g ethanol is absorbed and distributed in all body fluids and tissues. If drinking began 6 h before the blood was taken, the total amount of ethanol consumed is easy to calculate by adding on the amount lost through metabolism. Ethanol is eliminated from the whole body in moderate drinkers at a rate of 0.1 g/kg per h, so over 6 h a person has disposed of 48 g ethanol (0.1 × 80 × 6). The total amount consumed is easy to calculate from the equation below, and this comes to 104 g (56 + 48 = 104), which if necessary, can be converted to the number of standard drinks consumed.
The main sources of variation are uncertainty in the distribution factor Vd or rho and the elimination rate of alcohol from the body (g/kg/h). The results from many controlled drinking studies show that average Vd for ethanol is 0.70 for men and 0.60 for women and the interindividual variation of about ± 20%. The lower average Vd of ethanol in females leads to a higher BAC for a given dose of ethanol ingested, and this gender difference needs to be considered when blood alcohol calculations are made. The ± 20% variability in Vd stems from differences in body composition, especially the proportion of fat to lean tissue in the body. There is scant evidence that menstrual cycle and female sex hormones impact on the disposition and fate of ethanol in the body.
Other Alcohols
Forensic toxicologists are often required to analyze and interpret the concentrations of other aliphatic alcohols in blood samples, such as methanol (wood alcohol), isopropanol (rubbing alcohol), and ethylene glycol (antifreeze). These alcohols are widely available in household and commercial products and are sometimes consumed as ethanol substitutes for intoxication purposes by problem drinkers and alcoholics. The acute intoxication effects of ethanol are similar to these more toxic alcohols, which means that people are initially unaware they are in danger of poisoning and therefore don’t seek emergency hospital treatment.
The metabolism of methanol is blocked as long as blood ethanol concentration exceeds 0.02 g/100 mL. Below this concentration methanol is converted in the liver first to formaldehyde and then formic acid, and the elimination half-life is about 2–4 h. Formic acid is a strong organic acid (pKa = 3.77), which causes a disordered acid-base balance and a dangerous state of metabolic acidosis. Patients complain of nausea, and they might vomit and suffer from abdominal pains after drinking methanol. A well-recognized clinical observation in methanol poisoning is blurred vision and blindness, owing to the interaction of formaldehyde with the retina or the eye. Methanol poisoning is associated with high mortality because people seek emergency treatment too late when life-threatening acidosis has already developed. Clinical diagnosis of methanol poisoning might include measuring osmolal gap and anion gap metabolic acidosis, although specificity is improved if blood methanol and serum formate are determined. When methanol poisoning deaths are investigated, fatalities often depend on whether this alcohol was consumed alone or mixed with ethanol. The presence of ethanol prevents conversion into toxic metabolites, and during this time methanol is eliminated in urine and breath.
Ethylene glycol is metabolized in the liver by the same enzymes involved in the metabolism of ethanol and methanol, and the elimination half-life of the diol is 2.5–3.5 h in the absence of antidote treatment. The first product of metabolism is glycolaldehyde, which is further oxidized to glycolic acid. Oxidation of the second hydroxyl group produces glyoxylic acid and finally oxalic acid. Glycolic, glyoxylic, and oxalic acids contribute to the metabolic acidosis seen in patients poisoned with ethylene glycol. The clinical presentation of glycol toxicity is usually considered in three stages depending on time elapsed after ingestion. The first stage occurs after 0.5–2 h when concentrations of the diol in blood are fairly leading to acute intoxication and depression of the central nervous and also a raised osmolal gap. The second stage is seen after 12–24 h when anion gap metabolic acidosis increases and osmolal gap decreases. Patients might experience difficulties breathing with hyperventilation with hypoxia. The third stage is after 24–72 h when concentration of the diol in blood is low or zero, but there is a high anion gap and patients complain of pain in the lower back. Many cannot urinate (oliguria), and victims eventually die from renal failure and metabolic acidosis.
The traditional first-aid treatment for patients poisoned with methanol or ethylene glycol was to administer ethanol (8–10 % v/v) to reach and maintain a BAC of 0.1–0.15 g% for several hours. The higher affinity of liver ADH for ethanol meant that methanol and ethylene glycol were not converted into toxic metabolites. The unchanged alcohols as well as any metabolites formed could be removed from the blood by hemodialysis. Because dialysis also removes ethanol from the bloodstream, the infusion must be continued even during treatment.
A more modern alternative to ethanol as antidote for methanol and ethylene glycol poisoning is the drug fomepizole (Antizol®), which chemically is 4-methylpyrazole. This heterocyclic molecule is a potent competitive inhibitor of liver ADH and like ethanol blocks conversion of the toxic alcohols into their more dangerous metabolites. Fomepizole also undergoes metabolism and needs to be administered as a series of i.v. injections to be an effective treatment for the poisoned patient. Unlike ethanol, fomepizole does not depress the central nervous system and is the preferred antidote for treatment of children or skid-row alcoholics, who might suffer from hepatic dysfunction (cirrhosis or other liver diseases). The disadvantage of fomepizole is the high costs of the medication compared with ethanol.
Treatment of patients poisoned with isopropanol is less complicated and requires only a general supervision to ensure they don’t vomit and thus keep the airways clear and wait for the alcohol to become metabolized. The secondary alcohol is converted in the liver into acetone as the principal metabolite so patients have a sweetish smell of this ketone on the breath. The elimination half-life of isopropanol (3–5 h) is much shorter than that of acetone (15–20 h), which means that acetone can be measured in blood and breath for a lot longer than isopropanol.
Effects of Ethanol
Ethanol exerts a wide spectrum of biochemical and physiological effects on the body depending on the amounts consumed on each occasion (the dose) as well as duration (years) of exposure to this drug. The acute intoxicating effect of ethanol depends on the dose, the speed of drinking, and gastric emptying.
Metabolic Effects
A variety of metabolic disturbances occur during hepatic oxidation of ethanol as a direct result of an altered redox state of the liver, which is shifted to a more reduced potential. Acetaldehyde, the first product of oxidation, is a highly reactive chemical species which binds to proteins and other endogenous molecules, and toxicity of acetaldehyde has been incriminated in alcohol-related diseases, including development of various cancers. When ethanol is oxidized to acetaldehyde, one atom of hydrogen is transferred to the cofactor nicotinamide adenine dinucleotide (NAD), which is converted to its reduced form (NADH). Further reduction of NAD to NADH occurs when acetaldehyde is oxidized to acetate in the second stage of ethanol biotransformation. The acetate generated from ethanol metabolism is transported with the blood away from the liver and is oxidized in the citric acid cycle into end products carbon dioxide and water (see Fig. 19.3). When people were given ethanol labeled with 14C, this radioactive tracer was immediately afterward detected in the expired air as 14CO2 verifying a rapid oxidative metabolism.
The markedly raised NADH/NAD+ ratio and excess of reducing equivalents associated with the hepatic metabolism of ethanol have important consequences for other NAD-dependent biochemical reactions in the liver. The lactate/pyruvate ratio increases, which leads to hyperlactacidemia and a metabolic acidosis; this diminishes the capacity of the kidney to excrete uric acid which eventually leads to hyperuricemia and attacks of gout. Furthermore, an elevated NADH/NAD ratio favors triglyceride accumulation and also promotes fatty acid synthesis and lipogenesis, hence the clinical syndrome of fatty liver. Another metabolic consequence of elevated NADH/NAD is inhibition of hepatic gluconeogenesis, which explains why heavy drinkers and alcohols often suffer from hypoglycemia. This condition is worsened by an inadequate diet in alcoholics, who obtain most of their calories from the combustion of ethanol (7.1 kcal per gram). However, these are referred to as “empty calories” because the body cannot store alcohol for later use and alcoholic drinks lack essential proteins, vitamins, and minerals contained in normal foods so many alcoholics are also malnourished.
Cardiovascular System
Moderate ethanol consumption has no significant effect on blood pressure, cardiac output, and cardiac contractile force. Moderate doses increase high-density lipoprotein, which has been associated with reduced cardiovascular disease. Ethanol does cause vasodilatation of the cutaneous vessels, which creates a feeling of warmth often associated with the consumption of alcoholic beverages. This vasodilatation does not occur uniformly over the vasculature. In fact, moderate doses of ethanol can cause vasoconstriction in the heart and the brain.
Central Nervous System
Ethanol easily crosses the blood-brain barrier to interact with nerve cell membranes and receptor proteins with the overall effect of depressing the central nervous system. At fairly low BAC (0.03–0.05 g/100 mL), people feel less inhibited; they become more talkative and social, which is often incorrectly conceived as stimulation. After higher doses and increasing BAC, depression of simpler and more basic functions occurs. At very high blood ethanol concentration (> 0.4 g/100 mL), the respiratory center in the brain is depressed and coma and death ensue. Scientific studies performed over many years have established general relationships between BAC and effects on the brain as reflected in clinical signs and symptoms of drunkenness, and one widely cited and recently updated compilation is shown in Table 19.4.
The table shows a broad overlap in the signs and symptoms of alcohol influence for different ranges of BAC. The mild euphoria at low BAC (< 0.05 g/100 mL) is actually caused by disinhibition. As the blood ethanol concentration increases (0.03–0.12 g/100 mL), judgment and decision-making abilities are influenced, and perception and reaction to events are impaired. This impairment develops prior to the onset of more overt symptoms of ethanol intoxication, such as difficulties in walking, speaking, and maintaining balance (0.09–0.25 g/100 mL). The signs and symptoms described in Table 19.4 are what might be expected for an adult person with moderate drinking habits. Habituation to alcohol alters the relationship, and some people are able to function at high BAC, especially when relatively simple tasks are performed. The pattern of drinking is also important in relation to ethanol-induced impairment, which is more pronounced after rapid drinking and when the BAC is in the rising phase. When the BAC curve enters the post-absorptive phase, several hours post-dosing , one observes a marked recovery in the intoxication/impairment effects of alcohol, which does not necessarily mean that a person is a safe driver, owing to anxiety and fatigue.
Gastrointestinal Tract
Consumption of ethanol preceding or in combination with meals stimulates the production of gastric juices rich in acid and poor in pepsin. Concentrated ethanol, i.e., at concentrations above 40%, can irritate mucosal membranes, which may lead to hyperemia or gastritis. Many chronic alcoholics have chronic GI problems due to the irritating effects of ethanol on the stomach. In general, gastric motility is not directly affected by ethanol.
Kidney
The ingestion of ethanol produces a diuretic effect in part because of an increase in volume of liquid consumed, especially in beer drinkers who frequently need to urinate. However, the main diuretic action of ethanol is by inhibition of the secretion of antidiuretic hormone (vasopressin). Antidiuretic hormone is produced by the pituitary gland and is responsible for the renal tubular reabsorption of water. In general, about 99% of the water filtered by the kidney is reabsorbed, with the remaining water (1%) entering the bladder as urine. The increased production of urine after drinking ethanol is only evident during the absorption part of the BAC curve as shown in Fig. 19.5. In the post-absorptive elimination phase of the BAC curve, the production of urine returns to normal at about 1 mL per minute.
Liver
The acute ingestion of ethanol has little effect on hepatic function. Damage to the liver will develop as a result of long-term, regular consumption of ethanol. Injury first occurs from the accumulation of fat in the liver. The amount of ethanol presented to the liver after drinking is large in comparison to the concentration of other substances. For the liver to process the ethanol, it reduces the activity of other biochemical processes. One of the processes reduced is the oxidation of fat, causing excess fat to remain in the liver. Furthermore, ethanol ingestion leads to increased acetaldehyde formation, which can also have a toxic effect on the liver by increasing lipid peroxidation. Initially, these fatty changes are reversible; however, over time, continued heavy drinking requires repair of liver damage through the deposition of collagen. This leads to fibrotic changes in the liver that eventually become irreversible, developing into liver cirrhosis, liver failure, and death.
Miscellaneous Effects
Ethanol may cause either an increase or a decrease in a variety of secretions. For example, ethanol increases the production of hydrocortisone but decreases plasma testosterone concentrations. Plasma catecholamines also increase following the consumption of ethanol.
Ethanol is also associated with teratogenic effects. These effects have been defined collectively as the “fetal alcohol syndrome” and are described by lower intelligence, slower growth, and facial abnormalities. As a result, drinking alcoholic beverages during pregnancy is not recommended.
While the vasodilatation of ethanol gives the feeling of warmth, it in fact causes increased sweating which leads to heat loss. Therefore, ethanol may cause a slight lowering of body temperature.
Tolerance
It is common knowledge that people differ in their response to the same dose of a drug and the legal drug ethanol is no exception. Ethanol’s effects are biphasic with stimulation being more pronounced during the rising part of the BAC curve and sedative and depression on the declining part of the BAC curve
Tolerance is defined as a decrease in response to a given dose of a drug after repeated intake, and in pharmacology this is reflected in a shift in the dose-response curve to the right. Two main types of tolerance are recognized for ethanol, known as dispositional and cellular tolerance. Dispositional tolerance has to do with altered absorption, distribution, or elimination after repeated exposure to the drug, whereas cellular tolerance is reflected in an altered pharmacological response. Another name for dispositional tolerance is metabolic tolerance, reflected in an increased rate of metabolism owing to induction of the microsomal CYP2E1 enzyme after a period of chronic heavy drinking. The slope of the post-absorptive elimination phase in alcoholics might range from 0.02 to 0.035 g/100 mL per hour compared with 0.01–0.02 g/100 mL per hour in moderate drinkers. The dose of alcohol and frequency of drinking necessary to cause an induction of the microsomal enzyme have not been established in humans.
The cellular tolerance to alcohol has two components. One is acute tolerance, which refers to diminished effects of the drug on performance and behavior during a single exposure. Acute tolerance is sometimes referred to as the “Mellanby effect” named after a British pharmacologist, who first observed the phenomenon in dogs receiving alcohol by stomach tube. Acute tolerance is a robust finding and has been confirmed by many investigators using various behavioral measures of alcohol influence. Impairment is more pronounced on the ascending limb of the blood alcohol curve compared with the descending phase. A steeper slope on the ascending limb of the BAC curve produces greater degree of intoxication and can be reinforcing for some drinkers but aversive for others causing nausea and vomiting, especially in novice drinkers. Gulping drinks and drinking on an empty stomach are associated with a steeper rise in BAC and a greater effect on the brain. The mechanism behind the development of acute tolerance is however not completely understood.
The other aspect of tolerance is chronic or functional tolerance, reflected in diminished effects of alcohol after the same dose or the need to drink greater amounts (higher dose) to achieve the same effects before development of tolerance. Many people are capable of functioning despite an elevated BAC as exemplified by drunk drivers many of whom when examined by physicians were judged not under the influence of alcohol despite a high BAC. Apart from the smell of alcohol on the breath, when people arrested for public intoxication were admitted to emergency hospital departments for treatment they were coherent and could be interviewed despite some having a BAC of 0.3 g/100 ml or more. Whether caused by learning or previous experience, these individuals were able to compensate for the behavioral impairment effects of ethanol and in this way conceal the more overt symptoms of intoxication.
The phenomenon of cross-tolerance occurs between ethanol and other classes of drugs, such as barbiturates and benzodiazepines, which act as agonists at the GABAA receptor complex. Larger doses of these drugs might be necessary to achieve a desired effect in individuals who are tolerant to alcohol. This calls for caution when drugs such as benzodiazepines are prescribed to alcoholics and other people susceptible to abuse and dependence.
Blood Alcohol Analysis
Sampling
The proper sampling of blood for determination of ethanol and other drugs requires assistance from a registered nurse, a physician, or a phlebotomist, legally entitled to draw blood. In some jurisdictions medical laboratory technicians might also be trained and permitted to take blood samples for forensic analysis. Obviously, when ethanol is the substance analyzed in blood, an alcohol swab should not be used to disinfect the skin where the needle puncture is made. This would raise a suspicion that the blood might have been contaminated with alcohol from the swab, even through the risk of this happening is minimal when blood is drawn by venipuncture. To avoid unnecessary discussion and debate in legal cases, a non-alcohol skin disinfectant should be used, such as povidone-iodine or chlorhexidine. Simply washing the skin with soap and water would suffice, because the needle used to penetrate the skin is sterile. Many alcohol-type antiseptics contain isopropanol and not ethanol; these alcohols are easily separated when using gas chromatography for analysis. Evacuated tubes used for sampling blood intended for ethanol analysis should contain an anticoagulant (potassium oxalate or heparin) as well as sodium fluoride (1% w/v) as an enzyme inhibitor. The latter is necessary to quash any notion that ethanol was produced by the action of yeasts or bacteria on blood glucose, which is not very likely anyway because the tubes and needle are sterile.
Three principal methods are available for analysis of ethanol in biological specimens: (i) chemical oxidation and titrimetric or photometric analysis, (ii) enzymatic oxidation and measuring reduced coenzyme NADH by UV absorption at 340 nm, and (iii) gas chromatography either by liquid injection or headspace analysis after equilibration of blood at a fixed temperature.
Chemical Oxidation
Methods of alcohol analysis based on chemical oxidation methods have been used for over 100 years and the most common oxidizing agent is a mixture of potassium dichromate and sulfuric acid. Before starting the chemical reaction, it was necessary to remove ethanol from the sample by distillation, aeration, diffusion, or protein precipitation. The aqueous solution of ethanol produced was then reacted with the dichromate-acid mixture and the endpoint determined by titrimetric analysis or photometric analysis.
Wet-chemical oxidation methods of analysis were not specific for ethanol, and other volatiles, such as acetone, methanol, or ether, if also present in blood were oxidized leading to false high concentrations of ethanol. This was a particular problem in postmortem toxicology when alcohol poisonings were investigated and the deceased had consumed denatured industrial alcohol. Special preliminary tests were necessary to identify the presence of these interfering substances.
One of the most successful wet-chemical oxidation methods was described by Widmark in 1922 and was used in several countries for legal purposes. This micro-diffusion method required only 80–100 mg of capillary blood for each analysis. Widmark flasks resemble the Conway diffusion cells, which is a dish containing two concentric wells. The blood or other biological specimen (~100 mg) enters the outer well, and an excess of the dichromate oxidizing agent is added to the inner well. The flask was sealed and allowed to stand at room temperature or heated until the reaction was completed. Ethanol and any other volatile substances in the blood diffuse into the center well where the chemical reaction occurs. The amount of oxidizing agent that remained after the reaction was over was determined by iodometric titration. Crystals of potassium iodide were added to react with dichromate and liberate iodine, which was determined by volumetric analysis using standard sodium thiosulfate and starch indicator to detect the endpoint.
The dichromate ion (Cr+6) is converted to the chromic ion (Cr+3), which causes a change in color from yellow to green, which was observed visually providing a simple screening test of alcohol. Semiquantitative results were possible by making a series of ethanol standards and allowing them to react with dichromate in exactly the same way as case specimens. However, methods based on chemical oxidation are labor intensive and nonspecific making them more or less obsolete in modern clinical and forensic laboratories.
Enzymatic Oxidation
Enzymatic methods were first applied to blood alcohol analysis in the 1950s and coincided with the isolation of the liver enzyme alcohol dehydrogenase (ADH) in a pure crystalline form. The enzymes contained in yeast were found to be more selective for oxidation of ethanol than mammalian ADH, which was an important consideration for specificity of the method. Because the ADH-NAD+ oxidative is reversible, the acetaldehyde formed must be trapped so that the reaction is driven to completion. The buffer solution of coenzyme NAD+ also had semicarbazide present, which reacted with acetaldehyde to produce a stable semicarbazone. The NADH produced from NAD+ is measured spectrophotometrically at 340 nm and used for quantitative analysis. Although this assay was designed for serum, it works equally well with urine and also whole blood after precipitation of proteins with perchloric acid.
Enzymatic methods had the advantage in that they were easier to automate, and several procedures became available including use of a Technicon AutoAnalyzer or an Abbott X series analyzers. In the latter method, NADH produced by the ADH-catalyzed reaction of ethanol reacts with a thiazolyl blue dye, forming a chromagen. This technique is called radiative energy attenuation (REA) and is based on the principle that the measured fluorescence intensity of a solution containing a fluorophore and a chromagen is related to the absorbance of the solution. In this assay, fluorescein is the fluorophore and has been used successfully to measure ethanol in serum, urine, as well as blood from living and deceased persons.
Gas-Liquid Chromatography
The “gold standard” method for qualitative and quantitative determination of ethanol in biological specimens in both clinical and forensic laboratories is gas-liquid chromatography (GLC) equipped with a flame ionization detector (FID). GLC is a highly sensitivity and specific and provides accurate and precision results in a minimum of time. Moreover, other volatiles that might be present in blood together with ethanol, such as other alcohols, aldehydes, and ketones, can be determined simultaneously and can be distinguished by their retention times, that is, the time after injection until the appearance of the apex of the peak on the gas chromatogram. Quantitative analysis by FID gives a linear response over a wide range of ethanol concentrations in blood from 0.01 to 0.5 g/100 mL, and the limit of quantitation in routine casework is usually 0.01 g/100 mL. The FID detector has the advantage that it is insensitive to water vapor but sensitive to substances containing carbon, hydrogen, and oxygen atoms. The analytical sensitivity can be increased by saturating the blood sample with an inorganic salt, such as sodium chloride or potassium carbonate, which might be necessary if endogenous concentrations of ethanol are of interest.
The two most widely used GLC methods are direct injection of a liquid sample (1–2 μL) and analysis of the headspace vapor in equilibrium with the blood sample in a closed glass vial. Biological specimen should first be diluted (1:10) with an aqueous solution of internal standard (IS), such as n-propanol or t-butanol before GLC analysis. Diluting with an internal standard reduces the amount of biological substance that enters the GC instrument, which prolongs the life of the analytical column, and measuring peak area ratios helps to compensate for any variations in operating conditions. A calibration plot is constructed by plotting peak area ratio (ethanol/IS) for known strength aqueous standards and using this to deduce the ethanol concentration in blood samples.
The problem posed by making repeated injections of the biological matrix into the GC instrument is avoided when headspace GC analysis is done. The diluted blood sample is transferred to a glass vial, which is then fitted with a rubber septum and a crimped on aluminum cap. The vial is allowed to equilibrate at 50 or 60 oC, and then headspace vapor samples are removed with a gas-tight syringe and injected into the GC instrument for analysis. At a fixed temperature, the amount of any volatile in the air space is proportional to the concentration of the volatile liquid in the solution. Therefore, sampling the headspace of heated specimens and similarly treated ethanol calibrators allows calculation of the ethanol concentration in the specimen. Furthermore, aqueous calibrators can be used if the specimen is diluted ten times, which eliminates matrix effects.
The traditional gas chromatographs used packed columns measuring about 2 m long and 3 mm inside diameter containing polar stationary phases such as polyethylene glycol (Carbowax) or porous polymer materials (Porapak) which separated the volatile substances. Today capillary columns are the norm for GLC analysis of ethanol and other substances, and specialist columns are available for blood alcohol and related volatiles. These substances are separated according to the size of the molecules and their volatility. A thermal conductivity detector can be used but is not advisable because of the large response to water vapor in the sample. The flame ionization detector is the most appropriate for carbon-hydrogen molecules and has high sensitivity and good linearity. The effluent from the GC column could also be analyzed by mass spectrometry, and the electron impact spectrum contains mass fragments at m/z 31 (base peak), m/z 45, and m/z 46 (molecular ion), which are characteristic of ethanol and “fingerprint” the molecule. The theory behind each of these detectors is explained in Chap. 11. An example of a gas chromatogram from a calibrator containing multiple volatiles is shown in Fig. 19.7.
Analysis of Alcohol in Breath
A maximum of 10% of the total amount of alcohol consumed leaves the body unchanged by excretion via the lungs (exhaled air), the kidney (urine), and the skin (sweat). The small amount eliminated via the lungs forms the basis of the use of breath analyzers in traffic law enforcement as evidence of driving under the influence of alcohol. Roadside breath alcohol tests are routinely done by police authorities worldwide to test people suspected of driving under the influence of alcohol. There are several advantages of breath alcohol analysis over sampling blood for laboratory analysis including noninvasive sampling and obtaining results immediately afterward so that decisions can be made to arrest the driver or repeat the test.
Three special characteristics of ethanol facilitate use of breath analysis: (1) ethanol is volatile; (2) the concentrations in blood and breath are highly correlated; and (3) after drinking alcohol the concentration of ethanol exhaled in breath far exceeds that of other endogenous volatile substances. However, acetone is a potential interfering substance, and high concentrations are exhaled in breath in poorly treated diabetics or after a prolonged fast or eating low-carbohydrate diets.
Two types of breath alcohol analyzer are currently available: (1) handheld electronic devices mainly intended for screening purposes and (2) highly sophisticated stationary units used at police station for evidential purposes. The handheld units are denoted PBTs (preliminary breath testers), and they capture a sample of breath as the suspect exhales through a disposable plastic mouthpiece. Ethanol content in the breath is determined by electrochemical oxidation (fuel cell). Breath alcohol analyzers intended for evidential purposes determine ethanol content of breath by infrared spectrometry and by measuring the stretching frequency of C-H bonds (3.5 microns) or the C-O bond (9.5 microns) in ethanol molecules. Some modern breath alcohol analyzers incorporate both infrared and electrochemical methods of analysis, which is highly desirable in forensic toxicology because this furnishes two independent methods of analysis. Test subjects are required to make a prolonged end exhalation into the instrument for at least 6 seconds, and the concentration profile of exhaled ethanol is monitored as a function of time.
The physiological principles of breath alcohol testing are well founded scientifically. The distribution of ethanol between blood and alveolar air obeys Henry’s law, which states that at a given temperature, a direct relationship exists between the amount of a volatile substance (ethanol) dissolved in a liquid (blood) and the amount of the substance in the vapor (alveolar air) above the solution. Commercially available evidential breath-testing devices are based on the relationship that the amount of ethanol in 2100 mL of breath equals the amount of ethanol in 1 mL of blood at 34 °C, the temperature of expired air. This 2100:1 ratio was based on early scientific studies; more recent work indicates that 2300:1 is a better representation of the actual breath-to-blood ratio. This means that breath-testing devices based on a 2100:1 ratio will underestimate the actual blood ethanol concentration for the overwhelming majority of individuals.
Several scientific safeguards are necessary when breath alcohol analyzers are used for legal purposes; the most important of which is to observe the subject for at least 15–20 min prior to taking a sample and to ensure that nothing enters the mouth. Belching or vomiting could return ethanol from the stomach, possibly leading to an erroneous result. Evidentiary tests are confirmation tests that require a 15 min deprivation period and are preceded by a blank reading. At least two breath samples should be collected and analyzed, with the replicate analyses agreeing within 0.02 g/210L for approval. Breath ethanol results should be reported in terms of a mass of ethanol per volume of breath, which avoids any assumptions about a particular blood/breath ratio. Instrument performance should be validated with the testing of each subject using either a wet bath simulator or a calibrated dry gas standard as an ethanol control sample.
Many analytical methods have been developed for forensic breath alcohol analysis including the classic Breathalyzer® instrument developed by Robert F Borkenstein in the 1950s. The sampling of breath was done in a stainless steel cylinder and piston device with a vent that allowed discarding the initially top-lung exhaled breath. The last part of the exhalation that was considered to reflect alveolar air is trapped and saved for analysis. The sample chamber was heated to 50 °C to prevent condensation of water vapor and ethanol in the breath sample. The breath sample was analyzed by mixing with a mixture of potassium dichromate and sulfuric acid and a small amount of silver nitrate catalysis, which was contained in a glass ampoule. The oxidation reaction was allowed to proceed for 90 s which was the optimal time to prevent interference from any acetone that might be present in the breaths’ ample. The actual photometric measurement of ethanol was done at an absorbance of 440 nm.
Infrared (IR) Spectrophotometry
The absorption of infrared (IR) radiation is a characteristic property of a molecule depending on its structure and the types of chemical bonding. Absorption at IR light at certain wavelengths is characteristic of certain bonds, such as C-H, O-H, or C-O. Molecules can undergo stretching and bending vibrations when exposed to IR radiation, and the usual range of wavelengths span from 2.5 to 25 μM corresponding to wavenumbers 4000-400 cm-1.
The use of IR technology for the analysis of ethanol in breath has become a mainstay in evidential breath-testing devices. Ethanol has several types of bonds: C-H, C-C, C-O, and O-H. Selecting a wavelength where these bonds specifically absorb IR energy allows partial identification and quantification of ethanol in breath. Because many other compounds have the same chemical bonding and absorb IR energy at the same wavelength, there is a risk for interference with analysis of ethanol in breath. This potential interference problem is mitigated by the fact that an interfering substance must be volatile enough to appear in significant concentration in human expired air. Specificity can be enhanced by using multiple wavelengths simultaneously using a series of filters 3.3–3.5 μM.
IR breath analyzers differ in certain respects, such as volume of breath sampled, wavelength monitored, number of wavelengths used, and manner in which the exhalation is controlled for time and pressure characteristics. However, the basic principle is the same, and an end-expired sample of breath enters a heated chamber cell where it is irradiated with IR energy. If ethanol is present in the sample, it will absorb some of the IR energy in relation to the amount of ethanol that is in the sample. Absorption of IR energy by ethanol means that less energy reaches the detector in comparison to an air sample not containing ethanol. By calibrating the instrument with simulator solutions of known ethanol concentration, the ethanol concentration in the subject’s breath can be determined.
Electrochemical Oxidation
Electrochemical detectors oxidize ethanol in the vapor phase to acetaldehyde and further to acetic acid, and such detectors have been incorporated in a range of instruments intended for forensic breath alcohol analysis. This detector is constructed as a fuel cell, which consists of two platinum-coated conduction electrodes separated by an ion-conducting electrolyte layer, such as phosphoric acid. The conversion of ethanol present in breath to acetic acid produces a current. The flow generated is directly proportional to the amount of ethanol present in the sample. The fuel cell may react minimally with other alcohols like methanol and isopropanol but does not respond to any great extent to acetone.
Fuel cell technology has been used since the 1970s in handheld instruments for breath alcohol analysis. These devices are intended as roadside screening tests to furnish police officer with probable cause to arrest a driver for further testing. Fuel cells might also be used in evidential breath analyzers, especially in combination with an IR detector. Because the IR detector is nondestructive of ethanol, a fuel cell can be placed in series after an IR detector. The fuel cell does not oxidize acetone, which the major endogenous volatile in the breath under some circumstances. However acetaldehyde is oxidized, but the concentrations in breath, even after drinking alcoholic beverages, are so low that this ethanol metabolite is not a serious problem as an interfering substance.
Gas chromatography has also been adapted for breath alcohol analysis, because ethanol is already in the gaseous state when exhaled in the breath. Small and compact GC instruments incorporated a pressurized cylinder containing a mixture of hydrogen and nitrogen as combustible gas for the flame detector and a sampling loop to capture a portion of the exhaled air. One such instrument was the GC Intoximeter (FID detector) and another AlcoAnalyzer (thermal conductivity detector). However, the complexity of GC analysis, the need for more intensive training of operators, and the need for more frequent recalibrations meant that GC methods, although more specific, were abandoned in favor of infrared breath alcohol analyzers.
Examples of handheld PBT instruments include Alcolmeter, Alcotest, Lifeloc, and Alco-Sensor, all of which incorporate fuel cell sensors for determination of ethanol. Electrochemistry is not completely specific for ethanol because methanol and other alcohols (but not acetone) are oxidized but at different reaction rates. The instruments used for evidential breath alcohol testing are mostly based on multiple wavelength infrared (IR) detectors at 3.4 μM and/or 9.5 μM ranges, e.g. Intoxilyzer, DataMaster, and Evidenzer. One evidential breath analyzer (Intoximeter EC/IR) uses electrochemical oxidation as the primary means of detection, whereas others use a combination of IR and electrochemistry (Alcotest).
Stability of Ethanol in Blood and Urine
Compared with many other drugs and toxicants encountered in forensic toxicology, the concentrations of ethanol in blood are remarkably stable during short- and long-term storage of specimens. A small decrease in concentration of ethanol in blood of about 0.003 g/100 mL per month occurs when specimens are stored refrigerated (4 oC) in evacuated tubes until analyzed. The loss of ethanol is higher if the tubes are opened periodically to remove aliquots for analysis. Besides a diffusion of ethanol from the liquid into the air space, exposure to room air replenishes the oxygen content in the air space above the blood, and one mechanism suggested to loss of ethanol is nonenzymatic oxidation via oxyhemoglobin. Hence ethanol concentrations might be more stable in blood samples from smokers with higher concentrations of carboxyhemoglobin compared with nonsmokers. Stability is improved if specimens are stored frozen.
The evacuated tubes used to collect blood samples for ethanol analysis should contain chemical preservatives in powder form. Use of potassium oxalate, EDTA, or heparin is suitable as an anticoagulant, and sodium fluoride (~1% w/v) is included as an enzyme inhibitor. A widely used 10 mL gray stopper evacuated tube used for collecting blood samples for ethanol analysis has potassium oxalate (25 mg) as an anticoagulant and sodium fluoride (100 mg) as an enzyme inhibitor.
Ethanol concentrations in blood from living persons are rarely found to increase during long-term storage. But the situation is different in autopsy work because the specimens might already be contaminated with bacteria when the autopsy was performed. Ethanol can be produced by fermentation of substrates such as glucose and various fatty acids or amino acids in the presence of bacteria or yeasts. It is always a challenge in postmortem toxicology to establish whether a measured BAC resulted from antemortem ingestion or postmortem synthesis (neoformation). This can be investigated in a number of ways, although knowledge of the circumstances surrounding the death, especially witness statements and police reports about possible drinking by the deceased, is important information.
In postmortem toxicology, the concentrations of ethanol in different biological specimens should be compared and contrasted because this furnishes useful information to rule out postmortem synthesis having occurred. Finding acceptable agreement in results based on known water content of the materials analyzed speaks toward antemortem ingestion of ethanol and not postmortem synthesis. If the body emits a bad smell at autopsy, this is a strong indication that decomposition has already commenced and care is needed when toxicological results are interpreted. Finding an elevated concentration of ethanol in blood but negligible concentrations in vitreous humor or urine, which are both resistant to the putrefaction process, speaks toward postmortem production of ethanol.
Low concentrations of ethanol in blood, such as 0.01 g/100 mL, are easily produced after death even when there are no obvious signs of decomposition or putrefaction. This suggests that in postmortem toxicology a blood ethanol cutoff concentration of 0.02 g/100 mL would be more appropriate when positive results are reported. Low BACs of 0.01–0.03 g/100 mL need to be verified by analysis of ethanol in alternative specimens, such as vitreous humor or urine. Occasionally, blood ethanol concentrations exceeding 0.10 g/100 mL are seen with zero concentrations in alternative specimens. On the other hand, a measurable concentration found in vitreous humor or urine specimens speaks toward antemortem ingestion of alcohol, especially if the concentration ratios VH/blood or urine/blood are in the expected range of 1.2–1.3 based on relative water content of the specimens analyzed.
Other evidence that ethanol was produced in the body after death comes from fining other volatile substances besides ethanol (e.g., acetaldehyde, acetone, n-propanol, or n-butanol). Although ethanol is the main product of bacterial activity, it is not the exclusive product. However, because acetaldehyde is a normal metabolic product of ethanol metabolism and acetone might be elevated in blood of diabetics or malnourished individuals, the presence of these substances can occur by other mechanisms than fermentation.
Recent research demonstrates the possibility to determine non-oxidative metabolites of ethanol in body fluids as evidence that ethanol has undergone metabolism in the body during life. Methods involving GC-MS or LC-MS with deuterium-labeled internal standards are widely used to determine ethyl glucuronide or ethyl sulfate in postmortem specimens, including hair strands. The analysis of EtG and EtS verifies that ethanol has undergone a phase II conjugation reaction, which points toward antemortem consumption rather than postmortem synthesis. Use of realistic cutoff concentrations for positive EtG and EtS is necessary to avoid extraneous sources of ethanol in foodstuffs, medication, and various household products.
Numerous studies show a good stability of ethanol in antemortem blood specimens when they are properly stored in evacuated tubes and contain a chemical preservative. Potassium oxalate is commonly used as an anticoagulant to prevent clotting and is used in conjunction with sodium fluoride as an enzyme inhibitor. Under these conditions, in properly sealed tubes, the blood ethanol concentration will remain stable for at least a month, even if kept at room temperature.
As alluded to earlier, ethanol is rarely produced after voiding if the urine specimens are obtained from healthy subjects. The situation is different in diabetics, who might secrete glucose in the urine and also suffer from a urinary tract or Candida infection. Under these circumstances after 24–48 h storage at room temperature, high urinary concentrations are produced. However, all three components sugar, microorganism or yeast, and time are necessary for the in vitro production of ethanol after sampling. Storage of samples in the cold at +4oC or better still frozen (−20oC) prevents microbial synthesis of ethanol even when there is no NaF in the tubes. However, because urinary tract infections and candidiasis are common in diabetics, the inclusion of a fluoride preservative should be mandatory if ethanol is the substance to be analyzed.
Legal and Regulatory Aspects
Driving Under the Influence
Epidemiological surveys verify that overconsumption of alcohol and drunkenness play a major role in many types of accidents in the home, at work, and on the roads. Therefore, the analysis of alcohol in blood and other body fluids forms a critical component in any criminal or civil investigation of alcohol-related accidents. To address this problem, state legislatures have set limits on the concentration of ethanol permitted in blood or breath when an individual operates a motor vehicle.
Most countries have enacted blood alcohol limits ranging from 0.02 to 0.08 g/100 mL depending on activity, such as driving on the highway or engaging in safety-sensitive work (Table 19.5). The blood alcohol concentrations are expressed in different concentration units, such as mg/100 mL (UK and Canada), g/L (France and Spain), and g/kg (Nordic countries and Germany). SI concentration units (mmol/L) are also given for comparison because these units are increasingly used in hospital clinical chemistry laboratories when alcohol is analyzed and reported.
As early as 1971, the US National Safety Council Committee on Alcohol and Other Drugs stated that any driver with a blood alcohol concentration of 0.08 g/100 mL or more was impaired in terms of driving performance. Subsequent statements by the Committee have emphasized that driving impairment occurs at lower concentrations in some individuals. Almost all states have moved away from “presumption” statutes where the issue of an individual’s intoxication is rebuttable by other evidence, regardless of the ethanol concentration. Instead, “per se” laws have been adopted that make it a violation of the law to have above a fixed ethanol concentration in blood or breath at time of driving.
The National Committee on Uniform Traffic Laws and Ordinances (NCUTLO) developed the Uniform Vehicle Code to be adopted by the various states and the District of Columbia. The document consists of two parts: (1) the Uniform Vehicle Code, a set of motor vehicle laws designed and advanced as a comprehensive guide or standard for the state motor vehicle traffic laws, and (2) the Model Traffic Ordinance. Within the Uniform Vehicle Code, several recommendations are important to alcohol testing:
-
Revocation of license for refusal to submit to a chemical test or having a BAC of 0.08 g/100 mL or g/210 L or more, generally referred to as the “implied consent law.” Any person who drives a motor vehicle on public highways shall be deemed to have given his/her consent to have a chemical test of breath, blood, or urine to determine the alcohol concentration or the presence of other drugs.
-
Revocation of license for refusal to submit to a chemical test or having a BAC of any measurable and detectable amount (0.02 g/100 mL or g/210 L or more) for persons under 21 years of age.
-
The administration of a preliminary breath test when a law enforcement officer has probable cause to believe the person may be impaired by alcohol.
-
A driver may be compelled to submit to a chemical test if involved in a serious personal injury or fatal crash.
-
The State Department of Health is authorized to approve techniques or methods for the analysis of alcohol in blood, breath, and urine and to promulgate guidelines to determine competence of individuals to conduct such analysis.
-
The sample for analysis of blood may only be drawn by a physician, registered nurse, or other person qualified to withdraw blood acting at the direction of a police officer.
-
The defendant may have an additional test administered in addition to the test administered at the direction of the officer.
-
Alcohol concentration shall mean either grams of alcohol per 100 mL of blood or grams of alcohol per 210 L of breath.
-
If alcohol concentration measured 0.08 g/100 mL or g/210 L or more, it shall be presumed that the person was under the influence of alcohol.
The Uniform Vehicle Code serves as a basis for standardizing laws and practices among the states.
As part of an ongoing effort to decrease alcohol-related injuries and fatalities, in 2013 the National Transportation Safety Board (NTSB) recommended lowering the per se limit to 0.05 g/dL. The American Medical Association and the World Health Organization have also endorsed this position. Efforts to lower the legal alcohol limit for motor vehicle operators in the USA were also supported by the National Safety Council in 2016. Utah became the first state to decrease the per se limit to 0.05 g/dL in January 2019.
Figure 19.8 shows relative frequency distributions of blood alcohol concentrations in men and women apprehended in Sweden (statutory BAC limit 0.02 g/100 mL) for drunken driving. Mean blood alcohol concentration, regardless of gender, was 0.16–0.17 g/100 mL which signifies a period of heavy drinking and suggests that many drunk drivers are problem drinkers or alcoholics. Males dominated over females among traffic delinquents by 88% to 12%, although BAC did not seem to vary much in relation to the person’s age.
Alcohol in the Workplace
Some workplace activities obviously entail greater hazards than others, including significant risks to the worker, the workplace, and other individuals. In particular, the transportation workplace in all modalities presents a variety of basic safety hazards, which are increased by the effects of alcohol use by workers performing various safety-sensitive functions. Many non-transportation industries and workplaces also involve transport of persons, goods, and materials. In others, activities and operations occur that are inherently hazardous or associated with potential risks. The risk of error or adverse events is increased when tasks are performed by alcohol-impaired workers. Fundamentally, workers should be free of alcoholic influence at all times while at work. It is, therefore, recommended that:
-
Employees abstain from alcohol intake for 12 to 24 hours prior to undertaking critical and safety-sensitive tasks.
-
An appropriate program of on-site and off-site alcohol testing be implemented.
-
Breath alcohol concentrations <0.01 g/210 L and blood and saliva alcohol concentrations <0.01 g/100 mL should be deemed alcohol-free.
The universe of alcohol testing in the workplace is readily divided into governmentally regulated and nonregulated testing (testing for alcohol that is not required by law). In addition to testing performed under federal mandates, increasing numbers of states have enacted laws that control testing for alcohol and other drugs in workers. Further, such groups as the National Football League and the National Basketball Association require testing for alcohol and other abused drugs in professional athletes.
There are several important differences between alcohol and other abused drugs. Principally, alcohol is a licit drug and consumption of alcoholic beverages by adults is lawful, with limited exceptions, such as while driving motor vehicles. The mere presence of alcohol in the body and in body fluids (breath or saliva) does not imply a violation of law. Alcohol in the body has a short half-life, meaning that its elimination from the body is significantly faster than that of other commonly abused drugs (hours rather than days or weeks). Thus the timing of specimen collection for alcohol testing is more critical and demanding.
The National Safety Council’s Committee on Alcohol and Other Drugs (now the Alcohol, Drugs, and Impairment Division) in 1995 developed “A Model Program for the Control of Alcohol in the Workplace.” The program was designed primarily to assist employers and other required to establish testing programs in response to the Omnibus Transportation Employee Testing Act of 1991. It suggests that the purpose of alcohol testing programs is to help prevent accidents and injuries resulting from the misuse of alcohol by employees who perform safety-sensitive functions.
Workplace alcohol testing regulated by the US Department of Transportation (DOT) is mandated by the Omnibus Transportation Employee Testing Act of 1991 (Public Law 102-143, 1991) for certain transportation modalities. Performance of safety-sensitive functions by a covered employee in a DOT-regulated entity is prohibited:
-
1.
When such a person has an alcohol concentration of 0.04 g/210 L or greater, as indicated by a breath alcohol test, or temporarily when such person has an alcohol concentration of 0.02 g/210 L or greater but less than 0.04 g/210 L
-
2.
While such person is using alcohol
-
3.
Within 4–8 h after using alcohol
In addition, an employee involved in an accident may not refuse alcohol testing or consume alcoholic beverages until tested or until 8 h after an accident.
The categories for alcohol testing in the workplace are largely self-explanatory and include:
-
Applicant testing
-
Reasonable suspicion and reasonable cause testing
-
Fitness-for-duty testing
-
Post-accident testing
-
Return-to-duty and follow-up testing
-
Random testing
Testing for alcohol under the DOT regulations has the following features:
-
Alcohol is defined as “the intoxicating agent in beverage alcohol, ethyl alcohol, or other low molecular weight alcohols including methyl or isopropyl alcohol.”
-
Alcohol concentration is defined as “the alcohol in a volume of breath expressed in terms of grams of alcohol per 210 liters of breath as indicated by a breath test.”
-
All alcohol testing is to be carried out on-site at the workplace, except in some post-accident situations.
-
Breath and saliva are the only acceptable specimens for initial “screening” tests.
-
“Screening” and “confirmation” tests are required in specific situations. Breath is the only acceptable specimen for “confirmation” tests, with some exceptions for post-accident testing.
Testing is categorized into two varieties:
-
Initial tests, sometimes referred to as screening or preliminary tests, are intended to establish whether the tested person is alcohol-free or not. Alcohol-free individuals do not require any further testing. To be most practical, screening tests must be simple and rapidly performed with minimal training.
-
Confirmatory tests are performed with evidential-grade testing devices after an initial test has indicated the presence of alcohol in the tested person. The results of the confirmatory test are relied upon for personnel actions such as removal from current safety-sensitive duties.
All testing for alcohol in breath or saliva must be carried out with testing and associated devices appearing on NHTSA Conforming Products Lists. Screening tests on breath or saliva must use approved breath or saliva-alcohol screening test devices or be performed on breath with approved evidential breath testers (EBTs). Confirmation tests must be carried out on breath and must use EBTs that:
-
1.
Are capable of providing a printed result in triplicate
-
2.
Are capable of assigning a unique and sequential number to each completed test and displaying same before test
-
3.
Are capable of printing on each copy of the result the manufacturer’s name for the device, the device serial number, the time of the test, the test number, and the test result
-
4.
Are able to distinguish alcohol from acetone at an alcohol concentration of 0.02 g/210 L
-
5.
Are capable of testing an air blank prior to each collection of breath and of performing an “external calibration check”
Confirmation tests must be carried out within 30 minutes of the completion of a screening test that reports an alcohol concentration of 0.02 g/210 L or greater. A deprivation period of not less than 15 minutes and an air blank yielding a 0.00 g/210 L result must precede the breath collection for a confirmation test. (Air blanks are not required before or after a breath screening test.) Testing must be performed by a breath alcohol technician (BAT) who has successfully completed a course of instruction equivalent to the DOT model course and who has “demonstrated competence in the operation of the specific EBT(s)” that the BAT will use. Law enforcement officers who have been certified by state or local governments to conduct breath alcohol testing with the EBT concerned are deemed by DOT to be qualified as BATs.
The following documents define the criteria for evaluation and provide notice of acceptable products that meet the established criteria:
-
1.
Model Specifications for Evidential Breath-Testing Devices (58 FR 48705–10, September 17, 1993)
-
2.
Conforming Products List of Evidential Breath Alcohol Measurement Devices (82 FR 50940-50944, November 2, 2017)
-
3.
Model Specifications for Screening Devices to Measure Alcohol in Bodily Fluids (73 FR 16956-16960, March 31, 2008).
-
4.
Conforming Products List of Screening Devices to Measure Alcohol in Bodily Fluids (77 FR 35745-35747, June 4, 2012)
-
5.
Model Specifications for Calibrating Unit for Breath Alcohol Testers (72 FR 34742-34748, June 25, 2007)
-
6.
Conforming Products List of Calibrating Unit for Breath Alcohol Testers (77FR 64588-64590, October 22, 2012)
Updated notices of conforming products appear periodically in the Federal Register.
Suggested Reading
Caplan YH, Zettl JR (2002) The determination of alcohol in blood and breath. In: Saferstein R (ed) Forensic science handbook, 2nd edn. Prentice-Hall, Englewood Cliffs, pp 635–695
Caplan YH, Goldberger BA (eds) (2015) Garriott’s medicolegal aspects of alcohol, 6th edn. Lawyers and Judges, Tuscon
Dubowski KM (1985) Absorption, distribution, and elimination of alcohol: Highway safety aspects. J Stud Alcohol (Suppl 10):98–108
Dubowski KM (1992) The technology of breath-alcohol analysis. National Institute on Alcohol Abuse and Alcoholism, DHHS publication (ADM)92-1728
Jones AW (1990) Physiological aspects of breath-alcohol measurement. Alcohol, Drugs, and Driving 6:1–25
Jones AW (1996) Measuring alcohol in blood and breath for forensic purposes—a historical review. Forensic Sci Rev 8:14–43
Jones AW (2006) Urine as a biological specimen for forensic alcohol analysis and variability in the urine-to-blood relationship. Toxicol Rev 25:15–35
Jones AW (2010) Evidence based survey of the elimination rates of ethanol from blood with applications in forensic casework. Forensic Sci Int 200:1–20
Jones AW (2011) Pharmacokinetics of ethanol – issues of forensic importance. Forensic Sci Rev 23:91–136
Kugelberg FC, Jones AW (2007) Interpreting results of ethanol analysis in postmortem specimens: A review of the literature. Forensic Sci Int 165:10–29
O’Neal CL, Poklis A (1996) Postmortem production of ethanol and factors that influence interpretation. A critical review. Am J Forensic Med Path 17:8–20
Porter WH (2012) Ethylene glycol poisoning. Quintessential clinical toxicology, analytical conundrum. Clin Chim Acta 413:365–377
Walsham NE, Sherwood RA (2012) Ethyl glucuronide. Ann Clin Biochem 49:110–117
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Levine, B.S., Caplan, Y.H., Jones, A.W. (2020). Alcohol. In: Levine, B.S., KERRIGAN, S. (eds) Principles of Forensic Toxicology. Springer, Cham. https://doi.org/10.1007/978-3-030-42917-1_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-42917-1_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-42916-4
Online ISBN: 978-3-030-42917-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)