Abstract
Being physically active reduces the overall risk of developing at least ten different types of cancer and is associated with better outcomes in several cancers. However, in order to obtain the full benefit of physical activity and/or exercise for prevention or treatment, the mechanisms by which exercise impacts cancer development must be understood. Research on mechanistic relationships between physical activity or exercise and cancer has gained momentum in the last decades, and there is now evidence to support several different potential mechanisms. In this chapter, we review tumor cell intrinsic and extrinsic changes induced by exercise. We review tumor microenvironment changes including changes in the vasculature and immune response to cancer, as well as epigenetic changes within tumor cells. Finally, we briefly highlight emerging mechanisms that are likely to be important for the impact of physical activity on cancer development, treatment, and outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Exercise
- Physical activity
- Mechanisms
- Cancer development
- Tumor vasculature
- Immune response
- Epigenetics
- Exercise and cancer treatment
- Adjuvant therapy
- Molecular signaling
Introduction: Physical Activity and Cancer
It is well established that maintaining a healthy lifestyle which includes regular physical activity reduces the risk of developing numerous types of cancer, including breast, prostate, colon, and kidney cancers. The evidence for the relationship between higher physical activity levels and reduced risk of developing these cancers is strong, based on large datasets and meta-analyses, and has been extensively reviewed [1,2,3].
Similarly, there is strong meta-analysis-level data supporting a relationship between increased physical activity and decreased risk of death from cancer even after cancer occurs. Evidence also suggests that while exercise appears to reduce the overall risk of developing and dying from cancer, the effect of exercise within cancer types is nuanced and may have disproportionate impact on specific molecular subtypes of broader cancer diagnoses. For example, in a 26-year study of 49,160 men measuring the relationship of physical activity to prostate cancer development, men in the highest quintile of exercise intensity had a 30% lower risk of developing an advanced cancer and 25% lower risk of lethal cancer in comparison to men in the lowest quintile [4]. Interestingly, men in the top quintile of amount of vigorous exercise had a 29% lower risk of TMPRSS2:ERG fusion-positive, but no difference in the risk of fusion-negative, prostate cancer compared to men in the lowest quintile [4].
Similarly, in a study examining physical activity and the risk of colorectal (CRC) or colon cancer in 2769 Korean individuals, regular exercise significantly decreased the risk of CRC or colon cancer [5]. For CRC, the presence of a PITX1 minor allele confers higher risk. In this study, a significant interaction effect between exercise, the presence of the PITX1 minor allele, and the risk of CRC or colon cancer was identified. Individuals with the PITX1 minor allele who did not exercise regularly were at the highest risk of developing CRC and colon cancer, leading the authors to conclude that particularly for individuals with the PITX1 minor allele, physical activity is important.
Another example of a differential impact of exercise in patients with varying molecular subtypes of tumors was demonstrated in 803 Caucasian bladder cancer patients and 803 healthy controls [6]. This study evaluated both risks associated with behavior, such as low, medium, or high physical activity, and genetic polymorphisms of the mTOR pathway that increase the risk of bladder cancer. The low- or medium-activity groups had a significantly higher risk than the high-activity group of developing cancer independent of genotype. Interestingly, when stratified by genotype (based on the number of single nucleotide polymorphisms in the mTOR pathway), a low activity level correlated with a 2.74-fold increased risk for a low-risk genotype, a 3.72-fold increased risk for a medium-risk genotype, and a 3.45-fold increased risk for a high-risk genotype, indicating that physical activity may be most beneficial for persons with the medium-risk genotype [6].
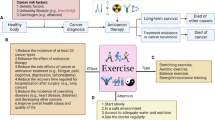
These studies and others support the need for understanding the cellular and molecular mechanisms by which exercise modulates cancer development, as the most appropriate exercise interventions are unlikely to be “one size fits all” either as a preventive or therapeutic method. The studies discussed above and several others indicate that tumors which are driven by specific genetic mutations may respond differently to exercise than those driven by others, suggesting that the mechanism of action of certain exercise interventions may be dependent on molecular pathways that are also important in cancer development. Identification of the mechanisms by which exercise impacts tumor biology and the molecular contexts in which exercise is most effective is necessary to achieve the most beneficial prescriptive exercise interventions for the prevention, treatment, and survivorship of cancer. Several of the mechanisms by which exercise impacts cancer were recently reviewed [7]. In this chapter, we add to the existing review literature on what is known about the mechanisms by which exercise modulates cancer. Mechanisms to be discussed include changes to the tumor vasculature and epigenetic regulation (Fig. 4.1) as well as changes to the immune system and circulating factors (Fig. 4.2).
Exercise and Tumor Vascular Function
One hallmark of cancer is the ability of the tumor to induce angiogenesis [8]. The formation and function of vasculature are largely regulated by the balance of pro-angiogenic factors, such as vascular endothelial growth factor (VEGF), and antiangiogenic growth factors, such as thrombospondin-1 (TSP-1). In general, tumor cells secrete more pro-angiogenic than antiangiogenic factors. Due to secretion of pro-angiogenic factors by tumor cells, tumors are able to induce endothelial cell proliferation and the rapid development of blood vessels by sprouting from existing vasculature, recruitment of local vasculature, and recruitment and proliferation of endothelial and perivascular progenitor cells. While inhibiting the ability of the tumor to form blood vessels with the aim of “starving” the tumor of nutrients and oxygen does work in some tumors such as renal cell carcinoma, clinical evidence suggests that pharmacologically targeting one pro-angiogenic factor is rarely sufficient for a sustained vascular inhibiting effect in patients [9]. Further, in recent years, tumor cells have been demonstrated to be able to survive extreme hypoxia, and evidence suggests that enhancing tumor hypoxia (starving the tumor of oxygen by eliminating blood supply) may actually increase the metastatic potential of tumor cells [9, 10]. Thus, the field of tumor angiogenesis has evolved in ways that are important to note prior to interpreting data on how exercise impacts tumor vasculature.
Tumor vasculature is inherently dysfunctional and inefficient due to the rapid proliferation of endothelial cells causing disorganized vasculature without appropriate hierarchy or perivascular cell coverage. In the last two decades, the concept of normalizing tumor vasculature to enhance delivery of therapeutic agents and reduce tumor hypoxia has emerged [11, 12]. Tumor vascular normalization refers to making tumor vessels more like “normal” organ vasculature, i.e., become more organized, have less sprouting and reduced proliferation, have better pericyte coverage, become appropriately permeable, and, importantly, have increased function. In this model, increasing blood flow to the tumor is beneficial because increased blood delivery to the tumor would reduce hypoxia and increase the delivery of therapeutic agents. As the impact of exercise is evaluated in regard to the tumor, it must be considered in context: treatment of some tumors would benefit from ablation of angiogenesis (ovarian cancer, renal cell carcinoma), which would be indicated by reduced microvessel density within the tumor, while treatment of most others would benefit more from tumor vascular normalization, indicated by changes to vessel structure and increased function, as an adjuvant to therapy.
Preclinical Evidence: Exercise and Tumor Vasculature
Overwhelmingly, current evidence in preclinical animal models suggests that exercise remodels tumor vasculature to improve vascular function and blood flow to the tumor. However, evidence is limited to less than 20 studies with wide variability in study design and analysis methods.
In contrast to more recent studies examining tumor vasculature and exercise which use moderate exercise doses, evaluation of blood vessels in one model of EL4 lymphoma growth in mice suggests that exhaustive high-intensity exercise (20–40 m/min for 3 h or until exhaustion daily) significantly decreased the vascular density of tumors compared to those in sedentary mice [13]. Exercise was begun on the day of tumor inoculation and caused a delay in time to peak tumor size but no change in final peak tumor size. Similar effects on microvessel density were found within hepatocellular carcinoma tumors in a study using a more moderate exercise intervention (treadmill, 60 minutes per day, 5 days per week). Microvessel density was decreased by moderate exercise in rats when exercise was initiated 6 weeks prior to and continued 4 weeks following tumor implantation [14]. The decrease in microvessel density did not correlate with a change in tumor size, but tumors from exercised rats had less viable and more necrotic tissue. In both of these studies, exercise caused decreased microvessel density but had little or no antitumor effect. Also in both of these studies, microvessel density was the only vessel analysis; other aspects of vascular structure and function were not evaluated.
Microvessel density is difficult to interpret in the absence of other features of the vasculature, as hyper-proliferation of dysfunctional vessels is not likely productive in terms of blood delivery. In contrast to the above studies, microvessel density within orthotopic breast tumor models has been shown to be increased by voluntary wheel running [15] and to be unchanged in melanoma or prostate tumor models by treadmill exercise [16]. These studies and others used multiple measures of tumor vascular structure and function to demonstrate increased blood vessel function within tumors, as discussed below.
A beneficial effect of exercise against tumor growth, and in improving blood delivery to tumors, has been consistently shown in murine and rat models of orthotopic breast cancer. Power Doppler imaging of in vivo blood flow within carcinogen-induced mammary tumors in rats demonstrated that 35 weeks of moderate-to-high-intensity treadmill running for 5 days per week led to a significant increase in blood perfusion within tumors [17]. Similarly, voluntary wheel running increased the number of functional, perfused vessels and the total blood perfused tumor area relative to sedentary controls in mammary MDA-MB-231 tumors in mice [18]. Further studies of breast tumor vascularity using 4 T1 and E0771 mammary tumor murine models confirmed that voluntary wheel running, begun at the time of tumor inoculation, positively impacts tumor vascular function [15]. In these studies, exercise conferred a significant decrease in tumor hypoxia and an increase in pericyte coverage of tumor endothelium, indicative of more functional blood vessels.
Consistent with a model in which exercise improves tumor vascular function allowing for better delivery of chemotherapy, 4 T1 mammary tumors in mice treated with exercise combined with cyclophosphamide were significantly smaller than tumors in mice treated with cyclophosphamide alone [15]. While the exact molecular response to exercise that induces tumor vascular remodeling is not yet clear, changes in breast cancer cell-secreted angiogenic factors in response to exercise have been demonstrated. For example, 8 weeks of endurance treadmill exercise decreased IL-6 and VEGF within MC4L2 mammary tumor in mice [19]. Thus, exercise may cause the tumor itself to change the way it crosstalks with endothelial cells, leading to changes in tumor vasculature.
In a series of elegant studies utilizing orthotopic prostate tumors (Dunning R-3327 AT-1 cells implanted into Copenhagen or nude rats), exercise was demonstrated to increase blood flow to the tumor [20, 21]. Five days per week of low-to-moderate-intensity exercise (15 m/min, 60 min per day) increased blood flow to the tumor by ~200%, significantly increased the number of patent vessels (vessels delivering Hoechst 33342), and significantly decreased hypoxia during exercise [21]. This was attributed, in part, to the lack of ability of the tumor vasculature to contract in response to exercise. For exercise to be beneficial to patients as a method to reduce tumor hypoxia and improve therapeutic delivery, there must be some sustainable change to blood delivery to the tumor that remains after exercise. Indeed, 7 weeks of exercise training afforded a twofold increase in microvascular PO2 and significantly reduced hypoxia even 48 h after exercise, suggesting that exercise caused a semipermanent improvement in blood delivery to the tumor [20].
In agreement with the studies discussed above, exercise has also been shown to improve blood vessel structure in subcutaneous melanoma and pancreatic ductal adenocarcinoma tumors. Five days per week of moderate treadmill running significantly increased the number of open vessel lumens and the average vessel length, consistent with vascular normalization. Pancreatic ductal adenocarcinoma tumors from exercised mice also had a ~25% increase in the number of functional blood vessels, which correlated with significantly better antitumor effect of gemcitabine when combined with exercise compared to gemcitabine treatment alone [16]. The unique contribution of this study to the field was that it demonstrated that the tumor vascular remodeling in response to exercise was due in part to the upregulation of antiangiogenic TSP-1. Exercise increased systemic circulating TSP-1, and in mice lacking TSP-1, the vascular remodeling effect of exercise and the increased efficacy of chemotherapy were significantly diminished. Further, the authors hypothesized with some supporting evidence that exercise increases TSP-1 by increasing the shear stress experienced by endothelial cells. The model presented indicates that increased shear stress led to the activation of nuclear factor of activated T cells (NFAT), a master transcriptional regulator of endothelial cell function, which induced TSP-1 transcription. Identification of the molecular pathways governing the tumor vascular response to exercise is critical if biomarkers representing the best intensity and duration of exercise to improve drug delivery are to be developed.
Clinical Evidence: Exercise and Tumor Vasculature
Evidence supporting the ability of exercise to impact vascular structure in tumors in patients (as opposed to animal models) is still sparse. However, one prospective study evaluated the relationship between pre-diagnosis physical activity and vascular morphology in prostate tumors by utilizing data from the Health Professionals Follow-Up Study, which included 571 men who developed prostate cancer [22]. Prostate tumors from men who reported their usual walking pace as brisk (3–3.9 miles per hour) prior to diagnosis (median time of assessment 14 months prior to diagnosis) had significantly more regularly shaped (perimeter2/4 × (3.14) × area) and longer blood vessels compared to those who walked at a less brisk pace, but with no difference in microvessel density. This is consistent with what was predicted by mouse models, where vascular normalization characterized by remodeling of the structure and functional capacity of blood vessels was shown. Perhaps surprisingly, there was no association between the self-reported number of hours per week of vigorous or non-vigorous activity and the vessel parameters that were measured, which included microvessel density, vessel shape, and lumen regularity.
The impact of exercise during chemotherapy on angiogenic factors and vascular function has also been studied in women with breast cancer receiving neoadjuvant doxorubicin and cyclophosphamide [23]. Twenty women participated in a study comparing the combination of an exercise intervention consisting of three supervised cycle ergometry sessions/week at 60–100% of VO2 peak, 30–45 min/session, for 12 weeks with chemotherapy to chemotherapy alone. In patients who were in the exercise intervention, the number of CD133+VEGFR2+ circulating endothelial progenitor cells increased over time, while it decreased in control patients. There was also an increase from baseline to the end of the 12-week intervention in circulating placental growth factor (Plgf), a pro-angiogenic factor, and a decrease in IL-2 in patients who exercised. For both of these, patients in the control groups had changes in Plgf and IL-2 expression in the opposite direction of patients who exercised.
Physical Activity and the Immune Response
The immune response to cancer cells, and the necessity of cancer cells to evade this response, is appreciated as a critical component of disease etiology. Infiltration of T lymphocytes, NK cells, and other immune cells correlates with outcome for numerous tumor types. In addition to the endogenous immune response to the tumor, manipulation of the immune system to promote an antitumor response is now being developed as a therapy. For example, checkpoint inhibition by blockage of CTLA-4 or PD-1 allows T cells to “see” tumor cells, and CTLA-4 inhibition is FDA approved to treat metastatic melanoma, while PD-1 inhibitors are in clinical trials for multiple tumor types [24, 25]. Finally, cell therapy, such as delivery of chimeric antigen receptor T cells (CAR-T) or NK cells, is also a growing field of immunotherapy [26, 27]. As immunotherapy grows to be a central component of the arsenal of cancer-targeting tools, the impact of exercise on the immune system cannot be ignored.
Exercise has long been known to regulate immune cell proliferation, migration, and function. Over the last two decades, the impact of exercise on the immune system in the context of cancer has been explored. A number of well-written reviews on the topic exist [28,29,30,31]. There is wide variability in study outcomes depending on the duration, intensity, and type of exercise and depending on whether acute or chronic exercise was evaluated. Common themes are that exercise activates natural killer (NK) cells and T lymphocytes, increases the number of circulating immune cells acutely, may promote polarization of macrophages, and regulates the level of numerous circulating cytokines.
In healthy individuals, exercise is well known to promote lymphocytosis, an increase in the number of circulating lymphocytes. Exercise intensity is correlated to both the magnitude of lymphocytosis and to changes in the function of circulating immune cells [32]. Also in healthy individuals, there is substantial evidence for an inverse relationship between physical activity and natural killer (NK) cell function. For example, in a study of 12,014 healthy participants, physical inactivity correlated with a significantly decreased interferon gamma (IFN-γ) production by NK cells in response to stimulation relative to minimally active or active individuals [33]. In another study, serum from participants who exercised for 1 hour was shown to increase NK cell cytolytic activity in vitro, and this was correlated with low cortisol and high IFN-γ [34]. Due to the clear role of exercise in modulating the immune system in healthy people, exercise is generally expected to promote an anticancer immune response. Below we discuss evidence in support of this possibility.
Preclinical Evidence: Exercise and Immune Response to Cancer
Preclinical mouse and rat cancer models have begun to define the role of exercise as an immune modulator for cancer prevention and therapy. One of the first preclinical studies examining the impact of exercise on immune cell infiltration into tumors utilized EL4 lymphomas in BALB/c mice and exhaustive daily exercise (described previously). This study demonstrated that exhaustive exercise reduces the number of neutrophils and macrophages that infiltrate a developing tumor while increasing the number of lymphocytes in the tumor [13]. This study should be interpreted with caution, as exhaustive daily exercise is unlikely to be clinically relevant. Further, there was no characterization of lymphocyte subtypes and the increased lymphocyte infiltration by exercise was only seen at the time of peak tumor size. The current understanding of immune influences on tumor growth suggests that immune cells often play opposing roles, tumor-promoting or tumor-inhibiting, depending on their activation and/or polarization status. Thus, due to the lack of analysis of macrophage polarization (tumor-promoting or tumor-inhibiting) or lymphocyte subtype, it’s not clear whether the immune cell infiltration that correlated with exercise in this study was responsible for the observed delay in time to peak tumor size.
In a work that did attempt to evaluate changes in immune cell function, rats underwent an anaerobic exercise intervention of weighted swimming intervals 4 days per week for 6 weeks prior to inoculation of Walker 256 tumor cells, continuing until the end of the experiment [35]. Exercise significantly reduced final tumor volumes, and gut-associated lymphocytes from exercised mice proliferated significantly more in response to stimulus than lymphocytes from non-exercised mice. Further, the phagocytic capacity of gut-associated macrophages from exercised tumor-bearing rats was significantly higher than the phagocytic capacity of macrophages from non-exercised rats. This study is noteworthy in that it uses a relatively unique exercise intervention of weighted swimming and evaluates macrophage function [35].
In addition to changes in ex vivo function, as evaluated in the study of rats discussed above, changes in the phenotype (which implies changes in function) of tumor-infiltrating immune cells in response to exercise are also important to evaluate. The impact of 6 days per week, 1 h per day at 15 m/min treadmill running over a 12-week period on colon polyp development was recently examined using the ApcMin/+ mouse model [36]. This model lends itself to the study of the impact of exercise on the immune system in the context of tumor development because the autochthonous tumors occur over time due to the genetic background of the mice and because the mice are fully immunocompetent. Mice that exercised had fewer large polyps, and mRNA analysis of mucosal tissue of the colon demonstrated fewer macrophages, both M1 and M2 phenotypes, within polyps of exercised mice. Further, tissue from exercised mice had significantly more CD8+ and fewer Foxp3+ T cells as determined by mRNA. As Foxp3 is an indicator of Treg cells, which are immunosuppressive, a reduction in this cell population may contribute to the antitumor effect of exercise.
In agreement with the above study noting fewer tumor-infiltrating macrophages, fewer CD68+ macrophages and fewer CD209+ dendritic cells were found in circulation of exercised mice after exposure to N-nitroso-diethylamine (DEN), which causes liver cancer development, compared to control [37]. In this study, mice performed 6 weeks of wheel running prior to DEN inoculation. Interestingly, the protective effects of exercise against inflammation were sex specific, as the reduced circulating innate immune cells were only observed in female mice. Female exercised mice also had a significantly smaller spike in TLR9, which activates the innate immune system, compared to female non-exercised mice. This is important as TLR9 promotes an inflammatory response, and inflammation is believed to be an early initiating step of HCC.
The NK cell response to exercise in the context of cancer has also been evaluated. In a thorough and elegant investigation of the role of NK cells in exercise-mediated tumor growth inhibition, Pedersen et al. used five different tumor types (B16F10 melanoma subcutaneous and tail vein-induced lung tumors, diethylnitrosamine-induced liver tumors, Lewis lung carcinoma, and Tg(Grm1)EPv spontaneous melanoma) to demonstrate that wheel running, particularly when initiated prior to tumor inoculation, reduces the incidence and growth rate of tumors [38]. Microarray analysis of B16F10 melanoma tumors from control or exercised mice demonstrated that 52% of upregulated genes were related to immune function and inflammation. Surprisingly, within the tumor, there was upregulation of cytokines and immune cell markers considered to be tumor promoting (i.e., IL-10 and FoxP3) and tumor suppressing (i.e., TNF-α and NKp46), further supporting the concept of a complex immune response to exercise in the context of cancer. Despite this, the authors demonstrated significant upregulation within the tumor of several NK cell-recruiting or NK cell-activating factors (NKG2D, MULT1, H60a, Clr-b) and were able to show a clear role for NK cells in the antitumor effect of exercise. The number of tumor-infiltrating NK cells in the B16F10 melanoma model inversely correlated with tumor burden, and depletion of NK cells completely abolished the protective effect of exercise. In addition, this study provides convincing evidence that epinephrine and IL-6 upregulation by exercise promoted recruitment of IL-6-responsive NK cells to the tumor [38].
In addition to evaluation of changes in numbers of circulating or immune cells, several studies have evaluated changes of cytokines in circulation or in tumor tissue in response to exercise. Exercise is well known to change the secretion of cytokines by muscles, known as myokines, and has been shown to change cytokines such as IL-6, IFN-γ, and IL-10 [39,40,41]. In general, it appears that Th1-type cytokines such as IL-6 increase immediately following exercise and in some cases persist, while other cytokines, such as MCP-1, spike temporarily followed by a decrease to lower than pre-exercise levels. Unfortunately, it is difficult to identify a clear pattern of cytokine response to exercise largely due to disparate findings following widely variable exercise protocols and cytokine measurement protocols.
Notwithstanding the caveats expressed above, preclinical models utilizing tumor-bearing mice indicate that exercise likely changes the cytokine milieu systemically and within the tumor microenvironment and that these changes likely support an immune response against the tumor. An interval treadmill training intervention initiated 6 weeks prior to tumor inoculation and maintained for 6 weeks after demonstrated significant changes both within 4 T1 mammary tumors and in the spleens of mice. Tumors from exercised mice had significantly increased oncostatin M and TNF-α, but significantly decreased IL-4, relative to tumors from non-exercised mice [42]. Similarly, splenocytes from exercised mice had significantly higher IFN-γ and lower IL-4 than splenocytes from control mice. Oncostatin M has been demonstrated to be secreted by muscles and to induce apoptosis of breast cancer cells in vitro, and IFN-γ and TNF-α both promote antitumor responses. Of note, there was no difference in tumor growth between exercised and control mice in this study [42], suggesting that modulation of these cytokines alone is not sufficient to confer suppression of tumor growth.
Clinical Evidence: Exercise and the Immune Response
As predicted by animal models, exercise appears to increase the immune response in cancer patients, though the data is sparse compared to studies in healthy persons. In one recent study of breast cancer survivors, the impact of an acute bout of exercise on circulating NK cells was examined. The study included 18 women, 9 breast cancer survivors within 3–6 months posttreatment and 9 healthy controls. Cancer survivors had lower numbers of NK cells at baseline. Thirty minutes of moderate aerobic exercise significantly increased the number of circulating NK cells in both survivors and control subjects, although the increase was not as substantial in breast cancer survivors as in control subjects [43]. In this study, the number of circulating NK cells returned to baseline in both groups within 24 h of the exercise bout. In a separate study, chronic resistance exercise in breast cancer survivors (n = 20 resistance training, 19 control) was examined over a 16-week training period and was not found to increase the number of NK or NKT cells. However, resistance training did reduce the expression of pro-inflammatory TNF-alpha by both NK and NKT cell populations compared to baseline and relative to breast cancer survivors in the control group [44]. While together this data suggests that exercise can have beneficial effects for NK cell number and function in cancer survivors, the low number of study participants and few total number of studies indicate that conclusions should be drawn with caution and further study is warranted.
It is unclear whether these findings in long-term survivors can be extrapolated to breast cancer patients still undergoing treatment, as one study found that a chronic, albeit very moderate, exercise intervention did not increase circulating immune cells. The impact of a walking exercise program on immune cell numbers in 20 women actively undergoing chemotherapy treatment demonstrated that a 12-week walking intervention caused no significant increase in the number of lymphocytes, T-helper cells, cytotoxic T cells, natural killer cells, or natural killer T cells [45].
Similar to other potential mechanisms of the impact of exercise on cancer, modification of the immune response is an exciting but as of yet not fully supported potential mechanism. Further study into how exercise regulates the immune system, and how this impacts cancer development and growth, is needed and likely to be fruitful.
Epigenetic Gene Regulation by Exercise
“Epigenetics” refers to a change in gene expression without direct alteration in the DNA sequence. Epigenetic modifications can change the frequency or magnitude of transcription of the DNA without changing the genetic code. Epigenetic modification of DNA is a key regulator of gene expression during development and in the natural processes of aging. There is also a clear role for epigenetic gene regulation in cancer development. Epigenetic modifications have been shown to alter the characteristics of tumor cells that are necessary for cancer growth [8] including proliferative signaling, evasion of cell death, induction of angiogenesis, and more [46]. Epigenetic elements including DNA methylation , histone modifications, and noncoding RNAs have been implicated in cancer and have been shown to be modified by exercise [47, 48]. However, the relationship between physical activity and epigenetic elements, and how this relationship influences cancer progression, is not fully understood. The following section will summarize important findings and current knowledge describing the role of exercise in epigenetic changes and gene regulation including alterations in DNA methylation , histone modification, and microRNA (miRNA) in cancer.
Exercise and DNA Methylation in Healthy Tissue
DNA methylation is a common epigenetic element that regulates gene expression. In mammals, methylation occurs on cytosine nucleotides in areas of the DNA called CpG sites or islands. CpG methylation in a gene promoter is associated with decreased gene expression by altering chromosome structure and preventing binding of transcription factors or recruiting gene-repressive proteins [49]. Thus, methylation can silence or reduce expression of a specific gene, altering cellular function. DNA methylation also occurs in transposable elements, including long interspersed nuclear elements (LINEs) [50]. Methylation status of LINE-1, which comprises about 17% of the human genome [51], predicts cancer risk [52,53,54] and is associated with health status [55].
Exercise may alter global DNA methylation patterns of LINEs or at CpG sites. Zhang et al. found that individuals aged 45–75 who were physically active 26–30 min per day (measured by an accelerometer) had significantly higher levels of global DNA methylation based on peripheral blood analysis in comparison to individuals that were active only 10 minutes or less per day [56]. This study suggested that physical activity influences global DNA methylation ; however, after data was adjusted for factors including gender, age, race, and other lifestyle factors, the differences became statistically insignificant. Weak associations were still reported in certain populations, including trends of physical inactivity associating with elevated risk of global hypo-methylation in non-Hispanics, supporting further investigation of exercise effects on global DNA methylation [56]. This study also demonstrates the relationship between factors like gender or race and global DNA methylation and the need for these to be considered when studying exercise in heterogeneous populations.
In another study, healthy individuals were evaluated pre-exercise, post-acute exercise, and post-4-week chronic exercise intervention to investigate the effect of exercise on methylation of promoter CpG sites of a natural killer (NK) cell-activating gene (KIR2DS4) and an NK cell-inhibiting gene (KIR3DL1) [57]. Interestingly, after acute exercise, a decrease in methylation was observed in the activating gene (KIR2DS4 gene) which correlated with increased gene expression, suggesting activation of NK cells by acute exercise. In contrast, chronic exercise resulted in non-significant decreases in DNA methylation and no changes in gene expression of either genes. No changes in NK cell numbers were found after acute or chronic exercise. This data suggests that acute exercise affects the NK cell population more strongly than chronic exercise, likely through modifications in promoter methylation [57]. As NK cells are an important component of the antitumor immune response and since exercise is known to mobilize NK cells, changes in NK cell activation status by exercise are likely to impact tumor growth. Studies like these demonstrate a clear role for physical activity in regulation of DNA methylation.
Exercise, DNA Methylation, and Cancer
Due to the growing amount of literature describing the dynamic regulation of epigenetic markers in response to exercise, understanding the implications of such regulation in cancer development and progression is key. There have been increasing efforts to understand the role of exercise in cancer-related DNA methylation .
Decreased levels of genome-wide methylation are often seen in cancer cells compared to normal tissue [58]. Studies defining global DNA methylation changes in cancer have revealed that exercise can change gene expression through changes in global methylation phenotype or pattern. In a study investigating changes in genome-wide methylation, levels of methylation of LINE-1, a repetitive genome element, were used as a surrogate for global methylation levels. Six hundred women at various ages with a family history of breast cancer participated in the study. Women who reported higher physical activity than the median in each age group had higher LINE-1 methylation than women below the median [59], demonstrating that exercise may reduce cancer development in part by increasing global methylation levels.
In contrast to hypo-methylation globally as represented by LINE-1 methylation , increased CpG methylation at specific sites can result in abnormal gene expression in cancer cells. In many cancers, including colorectal cancer, gliomas, breast cancer, and more, increased levels of CpG site methylation are seen in comparison to normal tissue [60]. Global CpG site methylation status has been demonstrated to be predictive in many cancer types. Specifically, CpG island methylator phenotype (CIMP) is a term used to describe tumor types with hyper-methylation at CpG sites of tumor suppressor genes or pathways, which suppresses tumor suppressor gene expression and promotes tumor development and progression [60]. It is not yet clear whether exercise influences CIMP status or reduces risk in a CIMP status-dependent way.
Apart from studies aimed at understanding broad methylation of CpG islands such as in CIMP, more focused approaches to determine mechanisms by which exercise influences specific cancer-related gene methylation have also been done. In one study, DNA methylation in prostate patient tumor samples was measured and correlated to exercise in patients with prostate cancer [61]. Self-reported levels of physical activity were used. Individuals who engaged in vigorous exercise at least once per week had a reduced chance of progression to late-stage metastatic prostate cancer in comparison to inactive individuals. Using the analysis of DNA methylation profiles, the authors demonstrated that patients who exercised at least one time per week had lower methylation in nine CpG sites of CRACR2A gene, an important gene involved in the innate immune system, in comparison to individuals who exercised less than once per week. Decreased methylation inversely correlated with CRACR2A gene expression [61], revealing a possible mechanism by which exercise reduces the risk of prostate cancer progression through alteration of the methylation status of CRACR2A gene. In a similar study using gastric carcinoma tumor samples, tumor-related gene methylation levels were measured to determine whether lifestyle factors prior to cancer diagnosis, including physical exercise, obtained through patient questionnaires, influenced methylation status. Interestingly, although not significant, increasing physical activity hours per week correlated with decreased methylation levels of CACNA2D3, a gene in which low expression due to hyper-methylation correlates with poor prognosis [62].
In another study, salivary samples were collected pre- and post-12-week exercise intervention in healthy adults to determine DNA methylation status in cancer-related genes [63]. Forty-five CpG sites in over 20 genes associated with breast cancer development and progression were analyzed. Baseline methylation levels significantly correlated with reported pre-study physical activity levels. Further, an increase in physical activity correlated with a significant decrease in DNA methylation in post-exercise intervention samples. This study demonstrates that exercise over a relatively short period of time (12 weeks) can change DNA methylation levels using 45 novel CpG sites related to breast cancer [63]. A clear correlation between physical activity levels and methylation of genes important in breast cancer has been further supported by two independent studies which identified APC, L3MBTL1, and 42 other genes as differentially methylated in patients who perform different levels of physical activity [64, 65].
These studies uncover exercise as an epigenetic regulator, which could be one mechanism by which exercise prevents cancer development. Future studies are necessary to understand and identify epigenetic markers modulated by exercise. Epigenetic modifications, therefore, represent exciting potential biomarkers for exercise and a possible mechanistic link between exercise and cancer risk reduction.
Exercise and Histone Acetylation in Healthy Tissue and Cancer
Histone modifications are posttranslational modifications including methylation, acetylation, and more which impact gene expression by altering the histones, leading to changes in chromatin configuration [66]. Histone-modifying proteins are divided into three types: “writers,” which add posttranslational modifications; “erasers,” which remove posttranslational modifications; and “readers,” which recognize certain histone marks and contribute to the posttranslational modification of histones.
While studies are limited, exercise has been demonstrated to regulate gene expression via histone modifications. In a rat model, in which stress and behavioral depression were induced using a chronic restraint model, 1 hour per day of voluntary wheel running exercise reversed depressive behaviors caused by upregulation of oxytocin and arginine vasopressin expression in the brain [67]. In the study, the exercise intervention correlated with histone modifications. Specifically, after chronic restraint, H3K9 methyltransferases, which facilitate H3K9 methylation causing reduced gene transcription, were significantly reduced, resulting in decreased methylation at oxytocin and arginine vasopressin promoters and increased expression. When an exercise intervention was used in combination with the chronic stress model, H3K9 methyltransferase G9a was significantly increased, which restored H3K9 methylation and reduced oxytocin and arginine vasopressin, protecting against depressive behaviors [67]. Exercise also had a protective effect in an acute stress restraint animal model where decreases in global DNA methylation in areas of the brain were observed after stress; however, animals exposed to stress restraint with an exercise intervention had no change in global DNA methylation status [68].
Exercise also activates cellular stress pathways like AMP-activated protein kinase (AMPK), promoting various downstream signaling including the NAD-dependent histone and protein deacetylase, SIRT1 [69, 70]. Histone deacetylation is usually associated with tighter association of chromatin and histones, creating a “closed” formation, which is associated with reduced gene expression. Interestingly, in animal models, exercise was recently shown to increase SIRT1 protein in muscles, suggesting a role of exercise-induced histone modification through increased SIRT1 expression [71]. However, studies are needed to elucidate the epigenetic role of SIRT1 in response to exercise.
The impact of exercise on histone modifications specifically within tumors is understudied. However, there is evidence demonstrating a relationship between exercise and histone modifications in immune cell populations in cancer patients, revealing that exercise may induce epigenetic changes altering the tumor microenvironment. Intense endurance exercise consisting of running a half marathon increased histone acetylation and expression of NK functional marker, NKG2D, demonstrating that exercise activates NK cells in cancer patients and healthy individuals [72]. Interestingly, moderate 30-minute bicycle exercise increased CD8+ T lymphocyte histone 4, lysine 5 (H4K5) acetylation in non-Hodgkin’s patients and healthy controls; therefore, exercise also impacts T cell epigenetic regulation which may have implications in antitumor immune cell functioning in cancer patients [73]. Further studies are needed to confirm the full extent to which exercise influences histone modifications in cancer and the cancer microenvironment.
Although exercise has a robust effect on epigenetic regulation and links to cancer development and progression, it is important to note that several studies discussed reported non-significant trends which may be due to a small sample size or to a variation in the physiological response to exercise between individuals. In other studies, no epigenetic changes were observed after exercise intervention [74]. However, the large variation in study design, including tumor types and physical activities analyzed, likely accounts for the disagreement in results. Further research to elucidate the effects of exercise on DNA methylation and histone modification is essential to form a comprehensive understanding of exercise’s implications in cancer development and prognosis.
MicroRNAs, Exercise, and Cancer
MicroRNAs (miRNAs) are a family of small noncoding RNAs that modulate gene expression [75]. There are over 2000 currently known miRNAs in the human genome which participate in vital processes including development, metabolism, signaling, and more [76]. In cancer, miRNAs that promote tumorigenesis are termed oncomiRs. OncomiRs promote cancer development and progression by reducing expression of tumor suppressors or increasing expression of oncogenes [77]. While a clear relationship between exercise and miRNA levels has been established and a relationship between miRNAs and cancer development is well described, data directly linking exercise-induced changes in miRNA levels to cancer development is sparse. This section will highlight known links between exercise and miRNAs and one published report linking these to tumor growth.
As discussed in previous sections, wide variability in the type and duration of exercise, as well as in the specific miRNAs studied, makes it difficult to draw broad conclusions about the relationship between exercise and miRNA or circulating miRNA expression [78, 79]. This section aims to give a sampling of studies in order to leave the reader with the understanding that exercise can impact cellular and circulating miRNA levels. However, the direction and magnitude of change are likely different based on which miRNA (just as expression of different genes would be) and what physical activity are being considered.
In healthy human subjects, changes in particular circulating miRNAs varied with different exercise interventions including a brief maximum exercise test, moderate-level 4 hour bicycle exercise, endurance exercise (running a marathon), or a single bout of resistance training [48]. With the goal of understanding endothelial cell or muscle damage in response to exercise, the authors chose to measure plasma levels of miR-126, a highly expressed endothelial cell miRNA , as a marker for endothelial cell damage and miR-133 as a marker for muscle damage. Interestingly, brief maximum exercise and 4 hour moderate bicycling increased miR-126 levels with no change in miR-133, while resistance training increased levels of miR-133 but did not change miR-126. Differently, running a marathon resulted in increased levels of both miR-126 and miR-133 [48]. These results clearly demonstrate the range of effects various types of exercise can have on circulating miRNA , likely due to the differing levels of muscle and respiratory involvement. In summary, authors suggest less strenuous or brief bouts of exercise which do not reach an individual’s maximum threshold cause damage to mainly endothelium, therefore causing upregulation of miR-126, while resistance training targets muscle, resulting in upregulation of miR-133. Intense endurance exercise, in contrast, was suggested to upregulate both miR-126 and miR-133 due to the overall strenuous nature and long bout of activity [48].
In another study, Nielsen et al. investigated the impact of a single acute bout versus a 12-week chronic exercise regimen on circulating miRNA plasma signatures [80]. Seven hundred forty-two circulating miRNAs were measured at 0 hours, 1 hour, and 3 hours after acute exercise. At 0 hours (immediately post-exercise), the eight miRNAs that significantly changed were downregulated, while 1 hour and 3 hours after acute exercise, all miRNAs that significantly changed (5 and 1 miRNAs, respectively) were upregulated. In contrast, after a chronic exercise regimen, seven miRNAs were significantly downregulated, and two miRNAs were significantly upregulated [80]. Interestingly, there were few overlapping circulating miRNAs altered by acute versus chronic exercise, demonstrating that acute and chronic exercise likely cause miRNA alterations through differing mechanisms. However, likewise a portion of circulating miRNAs that changed in response to both acute and chronic exercise was cardiac or skeletal muscle specific [80].
Changes in cellular miRNA levels in immune cell populations have also been demonstrated in response to exercise. In NK cells, isolated from blood of healthy men, before and after intense exercise, 23 miRNAs and 986 mRNAs were significantly changed. Interestingly, analysis identified pathways related to cancer signaling, adhesion molecules, and p53 signaling. Thus, exercise likely influences NK cell gene expression and miRNA levels, causing modulation of pathways known to regulate cancer development and progression [81]. A similar study identified 34 miRNAs that were significantly altered in PBMCs of healthy young men by an acute bout of intense exercise. Pathway analysis revealed that these miRNAs play roles in inflammation, demonstrating a novel concept of exercise-induced inflammation through miRNA regulation [82]. Neutrophils were also found to have changes in miRNAs associated with inflammatory pathways in response to exercise [83].
While exercise or physical activity clearly changes miRNA expression, which is likely to impact tumor growth, direct linkage of the two is currently unclear. Using mouse models, Isanejad et al. found in a breast cancer mouse model that interval exercise training alone and in combination with hormone therapy significantly reduced tumor volume [84]. Levels of angiogenic factors in the tumor tissue were also reduced in comparison to sedentary controls. Reduction in tumor growth and angiogenesis correlated with increased miR-206 and let-7a and decreased miR-21 in exercise and hormone-treated samples, demonstrating that exercise may influence tumor growth through miRNAs related to angiogenesis [84].
There are current reviews discussing exercise and miRNAs in cancer; however, they summarize miRNAs regulated by exercise and implicated in cancer progression [79, 85]. Interestingly, Dufrense et al. focuses on evidence reporting circulating levels of miR-133, miR-222, miR-221, miR-126, and let-7, all important miRNAs in various cancer types, to be altered in response to acute or physical exercise [79]. While enthusiasm for understanding the link between exercise, miRNAs, and cancer is present, as yet, an in-depth understanding of this link is lacking and not supported by data.
Other Emerging Mechanisms
Myokines
In recent decades, skeletal muscle has been recognized as an endocrine organ that secretes and responds to numerous growth factors, cytokines (known as myokines when secreted by contracting myocytes), hormones, and other signals. Some of the most well described include interleukins (IL-6, IL-8, IL-15), myostatin, irisin, secreted protein acidic and rich in cysteine (SPARC), and fibroblast growth factor (FGF) family members [41, 86]. In addition to being secreted by muscles in response to contraction, these factors have been implicated in tumor development, growth, or therapeutic response in various tumor models. Thus, muscle is highly likely to crosstalk with tumor cells and impact tumor development. Emerging evidence supports the likelihood of exercise impacting the crosstalk between muscles/myocytes and tumors/tumor cells [39, 87, 88] and has been well reviewed [86, 89].
Activation of p53 by Exercise
The master regulator of apoptosis, p53, is a critical tumor suppressor that is mutated or deleted in many cancer types. Appropriate activation of p53 in response to stress induces cell death and is therefore protective against cancer. Exercise induces p53 activation in muscle, and p53 is important for mitochondrial biogenesis and exercise capacity [90]. Thus, it is not surprising that p53 may play an important role in the protective effects of exercise against cancer. Exercise training of female rats during puberty correlated with significant upregulation of p53 mRNA, as well as BRCA1 and ERΒ mRNA, in mammary glands when rats reached 100 days old [91]. Similarly, voluntary wheel running caused significant upregulation of p53 in A549 lung carcinoma tumors in mice [92]. In addition to directly activating p53 in precancerous lesions, exercise appears to cause upregulation of systemic factors that cause p53 stabilization in LNCaP prostate cancer cells [93]. These studies demonstrate that exercise can impact p53 activation, at least within certain contexts. Given the critical role of p53 in numerous cancers, this potential mechanism is likely to become a major area of focus in the field.
Summary
In healthy humans and animals, physical activity or exercise causes changes to many systems of the body, including the cardiovascular, musculoskeletal, immune, and others. The molecular mechanisms by which these changes occur in the absence of disease are becoming clearly understood. In recent decades, the impact of these exercise-induced changes on tumor development, progression, treatment, and survivorship has gained focus in the cancer biology and exercise physiology communities. As our mechanistic understanding of exactly what exercise does and how in the context of cancer grows, so will the ability to utilize exercise in a preventive or therapeutic setting.
References
Al-Bayati O, et al. Systematic review of modifiable risk factors for kidney cancer. Urologic Oncology: Seminars and Original Investigations; 2019.
de Souza-Teixeira F, et al. PGC-1α as a biomarker of physical activity-protective effect on colorectal Cancer. Cancer Prev Res. 2018;11(9):523–34.
Moore SC, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults leisure-time physical activity and risk of 26 types of cancer leisure-time physical activity and risk of 26 types of cancer. JAMA Intern Med. 2016;176(6):816–25.
Pernar CH, et al. A prospective study of the association between physical activity and risk of prostate cancer defined by clinical features and TMPRSS2:ERG. Eur Urol. 2018;76(1):33–40.
Madhawa Neranjan Gunathilake JL, Cho YA, Jae Hwan O, Chang HJ, Sohn DK, Shin A, Kim J. Interaction between physical activity, PITX1 rs647161 genetic polymorphism and colorectal cancer risk in a Korean population: a case-control study. Oncotarget. 2018;9:7590–603.
Lin J, et al. Energy balance, the PI3K-AKT-mTOR pathway genes, and the risk of bladder cancer. Cancer Prev Res. 2010;3(4):505–17.
McTiernan A. Mechanisms linking physical activity with cancer. Nat Rev Cancer. 2008;8:205.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Jayson GC, et al. Antiangiogenic therapy in oncology: current status and future directions. Lancet. 2016;388(10043):518–29.
Gilkes DM, Semenza GL, Wirtz D. Hypoxia and the extracellular matrix: drivers of tumour metastasis. Nat Rev Cancer. 2014;14:430.
Goel S, et al. Normalization of the vasculature for treatment of cancer and other diseases. Physiol Rev. 2011;91:1071–121.
Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307(5706):58–62.
Zielinski MR, et al. Exercise delays allogeneic tumor growth and reduces intratumoral inflammation and vascularization. J Appl Physiol. 2004;96(6):2249–56.
Saran U, et al. Anti-tumoral effects of exercise on hepatocellular carcinoma growth. Hepatol Commun. 2018;2(5):607–20.
Betof AS, et al. Modulation of murine breast tumor vascularity, hypoxia, and chemotherapeutic response by exercise. J Natl Cancer Inst. 2015;107(5):pii: djv040.
Schadler KL, et al. Tumor vessel normalization after aerobic exercise enhances chemotherapeutic efficacy. Oncotarget. 2016;7(40):65429–40.
Faustino-Rocha AI, et al. Long-term exercise training as a modulator of mammary cancer vascularization. Biomed Pharmacother. 2016;81:273–80.
Jones LW, et al. Effect of aerobic exercise on tumor physiology in an animal model of human breast cancer. J Appl Physiol. 2010;108(2):343–8.
Shalamzari SA, et al. The effect of exercise training on the level of tissue IL-6 and vascular endothelial growth factor in breast cancer bearing mice. Iran J Basic Med Sci. 2014;17(4):231–58.
McCullough DJ, et al. Effects of exercise training on tumor hypoxia and vascular function in the rodent preclinical orthotopic prostate cancer model. J Appl Physiol. 2013;115(12):1846–54.
Behnke BJ, et al. Modulation of blood flow, hypoxia, and vascular function in orthotopic prostate tumors during exercise. J Natl Cancer Inst. 2014;106(4):dju036.
Van Blarigan EL, et al. Physical activity and prostate tumor vessel morphology: data from the health professionals follow-up study. Cancer Prev Res. 2015;8(10):962–7.
Jones LW, et al. Modulation of circulating Angiogenic factors and tumor biology by aerobic training in breast Cancer patients receiving neoadjuvant chemotherapy. Cancer Prev Res. 2013;6(9):925–37.
Yun S, et al. Targeting immune checkpoints in unresectable metastatic cutaneous melanoma: a systematic review and meta-analysis of anti-CTLA-4 and anti-PD-1 agents trials. Cancer Med. 2016;5(7):1481–91.
Balar AV, Weber JS. PD-1 and PD-L1 antibodies in cancer: current status and future directions. Cancer Immunol Immunother. 2017;66(5):551–64.
Brudno JN, Kochenderfer JN. Chimeric antigen receptor T-cell therapies for lymphoma. Nat Rev Clin Oncol. 2017;15:31.
Ghosh A, et al. CAR T cell therapy for multiple myeloma: where are we now and where are we headed? Leuk Lymphoma. 2018;59(9):2056–67.
Kruijsen-Jaarsma M, Révész D, Bierings MB, Buffart LM, Takken T. Effects of exercise on immune function in patients with cancer: a systematic review. Exerc Immunol Rev. 2013;19:120–43.
Idorn M, Hojman P. Exercise-dependent regulation of NK cells in cancer protection. Trends Mol Med. 2016;22(7):565–77.
de Jesus Leite MAF, et al. Effects of combined and resistance training on the inflammatory profile in breast cancer survivors: a systematic review. Complement Ther Med. 2018;36:73–81.
Hojman P. Exercise protects from cancer through regulation of immune function and inflammation. Biochem Soc Trans. 2017;45(4):905–11.
LaVoy EC, et al. T-cell redeployment and intracellular cytokine expression following exercise: effects of exercise intensity and cytomegalovirus infection. Physiol Rep. 2017;5(1):e13070.
Jung YS, et al. Physical inactivity and unhealthy metabolic status are associated with decreased natural killer cell activity. Yonsei Med J. 2018;59(4):554–62.
Gupta P, et al. Autologous serum collected 1 h post-exercise enhances natural killer cell cytotoxicity. Brain Behav Immun. 2018;71:81–92.
de Lima C, et al. Anaerobic exercise reduces tumor growth, cancer cachexia and increases macrophage and lymphocyte response in Walker 256 tumor-bearing rats. Eur J Appl Physiol. 2008;104(6):957.
McClellan JL, Steiner JL, Day SD, Enos RT, Davis MJ, Singh UP, Murphy EA. Exercise effects on polyp burden and immune markers in the ApcMin/+ mouse model of intestinal tumorigenesis. Int J Oncol. 2014;45(2):861–8.
Bay ML, et al. Voluntary wheel running reduces the acute inflammatory response to liver carcinogen in a sex-specific manner. Cancer Prev Res. 2017;10(12):719–28.
Pedersen L, et al. Voluntary running suppresses tumor growth through epinephrine- and IL-6-dependent NK cell mobilization and redistribution. Cell Metab. 2016;23(3):554–62.
Hojman P, et al. Exercise-induced muscle-derived cytokines inhibit mammary cancer cell growth. Am J Physiol Endocrinol Metab. 2011;301(3):E504–10.
Goh J, Niksirat N, Campbell KL. Exercise training and immune crosstalk in breast cancer microenvironment: exploring the paradigms of exercise-induced immune modulation and exercise-induced myokines. Am J Transl Res. 2014;6(5):422–38.
Manole E, et al. Myokines as possible therapeutic targets in cancer cachexia. J Immunol Res. 2018;2018:9.
Molanouri Shamsi M, et al. Effects of exercise training and supplementation with selenium nanoparticle on T-helper 1 and 2 and cytokine levels in tumor tissue of mice bearing the 4 T1 mammary carcinoma. Nutrition. 2019;57:141–7.
Evans ES, et al. Impact of acute intermittent exercise on natural killer cells in breast cancer survivors. Integr Cancer Ther. 2015;14(5):436–45.
Hagstrom AD, et al. The effect of resistance training on markers of immune function and inflammation in previously sedentary women recovering from breast cancer: a randomized controlled trial. Breast Cancer Res Treat. 2016;155(3):471–82.
Kim JJ, Shin YA, Suk MH. Effect of a 12-week walking exercise program on body composition and immune cell count in patients with breast cancer who are undergoing chemotherapy. J Exerc Nutr Biochem. 2015;19(3):255–62.
Flavahan WA, Gaskell E, Bernstein BE. Epigenetic plasticity and the hallmarks of cancer. Science. 2017;357:eaal2380.
Chuang JC, Jones PA. Epigenetics and MicroRNAs. Pediatr Res. 2007;61:24R–9R.
Uhlemann M, et al. Circulating microRNA-126 increases after different forms of endurance exercise in healthy adults. Eur J Prev Cardiol. 2014;21(4):484–91.
Deaton AM, Bird A. CpG islands and the regulation of transcription. Genes Dev. 2011;25(10):1010–22.
Schulz WA, Steinhoff C, Florl AR. Methylation of endogenous human retroelements in health and disease. Curr Top Microbiol Immunol. 2006;310:211–50.
Consortium IHGS. Initial sequencing and analysis of the human genome. Nature. 2001;409:860–921.
Baba Y, et al. Long interspersed element-1 methylation level as a prognostic biomarker in gastrointestinal cancers. Digestion. 2018;97:26–30.
Swets M, et al. Tumor LINE-1 methylation level in association with survival of patients with stage II colon cancer. Int J Mol Sci. 2016;18:pii: E36.
Woo HD, Kim J. Global DNA Hypomethylation in peripheral blood leukocytes as a biomarker for cancer risk: a meta-analysis. PLoS One. 2012;7:e34615.
Luiz Marques-Rocha J, et al. LINE-1 methylation is positively associated with healthier lifestyle but inversely related to body fat mass in healthy young individuals. Epigenetics. 2016;11(1):49–60.
Zhang FF, et al. Physical activity and global genomic DNA methylation in a cancer-free population. Epigenetics. 2011;6:293–9.
Schenk A, et al. Acute exercise increases the expression of KIR2DS4 by promoter demethylation in NK cells. Int J Sports Med. 2019;40(1):62–70.
Gaudet F, et al. Induction of tumors in mice by genomic hypomethylation. Science. 2003;300(5618):489–92.
White AJ, et al. Recreational and household physical activity at different time points and DNA global methylation. Europ J Cancer (Oxford, England: 1990). 2013;49:2199–206.
Hughes LAE, et al. The CpG Island Methylator phenotype: what’s in a name? Cancer Res. 2013;73(19):5858–68.
Dai JY, et al. Vigorous physical activity is associated with lower risk of metastatic–lethal progression in prostate cancer and Hypomethylation in the CRACR2A gene. Cancer Epidemiol Biomark Prev. 2019;28:258–64.
Yuasa Y, et al. DNA methylation status is inversely correlated with green tea intake and physical activity in gastric cancer patients. Int J Cancer. 2009;124:2677–82.
Bryan AD, et al. Physical activity and differential methylation of breast cancer genes assayed from saliva: a preliminary investigation. Ann Behav Med. 2013;45:89–98.
Coyle YM, et al. Role of physical activity in modulating breast cancer risk as defined by APC and RASSF1A promoter Hypermethylation in nonmalignant breast tissue. Cancer Epidemiol Biomark Prev. 2007;16:192–6.
Zeng H, et al. Physical activity and breast cancer survival: an epigenetic link through reduced methylation of a tumor suppressor gene L3MBTL1. Breast Cancer Res Treat. 2012;133:127–35.
Bannister AJ, Kouzarides T. Regulation of chromatin by histone modifications. Cell Res. 2011;21(3):381–95.
Kim TK, et al. G9a-mediated regulation of OXT and AVP expression in the basolateral amygdala mediates stress-induced lasting behavioral depression and its reversal by exercise. Mol Neurobiol. 2016;53(5):2843–56.
Rodrigues GM Jr, et al. Acute stress affects the global DNA methylation profile in rat brain: modulation by physical exercise. Behav Brain Res. 2015;279:123–8.
Lai C-H, et al. Exercise training enhanced SIRT1 longevity signaling replaces the IGF1 survival pathway to attenuate aging-induced rat heart apoptosis. Age (Dordrecht, Netherlands). 2014;36:9706.
Suchankova G, et al. Concurrent regulation of AMP-activated protein kinase and SIRT1 in mammalian cells. Biochem Biophys Res Commun. 2009;378:836–41.
Huang C-C, et al. Effect of exercise training on skeletal muscle SIRT1 and PGC-1α expression levels in rats of different age. Int J Med Sci. 2016;13:260–70.
Zimmer P, et al. Exercise-induced natural killer cell activation is driven by epigenetic modifications. Int J Sports Med. 2015;36:510–5.
Zimmer P, et al. Impact of exercise on pro inflammatory cytokine levels and epigenetic modulations of tumor-competitive lymphocytes in non-Hodgkin-lymphoma patients-randomized controlled trial. Eur J Haematol. 2014;93:527–32.
Boyne DJ, et al. Aerobic exercise and DNA methylation in postmenopausal women: an ancillary analysis of the Alberta Physical Activity and Breast Cancer Prevention (ALPHA) trial. PLoS One. 2018;13:e0198641.
Treiber T, Treiber N, Meister G. Regulation of microRNA biogenesis and its crosstalk with other cellular pathways. Nat Rev Mol Cell Biol. 2019;20:5–20.
Hammond SM. An overview of microRNAs. Adv Drug Deliv Rev. 2015;87:3–14.
Zhang B, et al. microRNAs as oncogenes and tumor suppressors. Dev Biol. 2007;302:1–12.
Denham J, et al. Exercise: putting action into our epigenome. Sports Med. 2014;44:189–209.
Dufresne S, et al. A review of physical activity and circulating miRNA expression: implications in cancer risk and progression. Cancer Epidemiol Biomarkers Prev. 2018;27:11–24.
Nielsen S, et al. The miRNA plasma signature in response to acute aerobic exercise and endurance training. PLoS One. 2014;9:e87308.
Radom-Aizik S, et al. Impact of brief exercise on peripheral blood NK cell gene and microRNA expression in young adults. J Appl Physiol (Bethesda, MD: 1985). 2013;114:628–36.
Radom-Aizik S, et al. Effects of exercise on microRNA expression in young males peripheral blood mononuclear cells. Clin Transl Sci. 2012;5:32–8.
Radom-Aizik S, et al. Evidence for microRNA involvement in exercise-associated neutrophil gene expression changes. J Appl Physiol (1985). 2010;109(1):252–61.
Isanejad A, et al. MicroRNA-206, let-7a and microRNA-21 pathways involved in the anti-angiogenesis effects of the interval exercise training and hormone therapy in breast cancer. Life Sci. 2016;151:30–40.
Ferioli M, et al. Role of physical exercise in the regulation of epigenetic mechanisms in inflammation, cancer, neurodegenerative diseases, and aging process. J Cell Physiol. 2019; https://doi.org/10.1002/jcp.28304.
Whitham M, Febbraio MA. The ever-expanding myokinome: discovery challenges and therapeutic implications. Nat Rev Drug Discov. 2016;15:719.
Gannon NP, et al. Effects of the exercise-inducible myokine irisin on malignant and non-malignant breast epithelial cell behavior in vitro. Int J Cancer. 2015;136(4):E197–202.
Aoi W, et al. A novel myokine, secreted protein acidic and rich in cysteine (SPARC), suppresses colon tumorigenesis via regular exercise. Gut. 2013;62(6):882–9.
Roy P, Chowdhury S, Roy HK. Exercise-induced myokines as emerging therapeutic agents in colorectal cancer prevention and treatment. Future Oncol. 2018;14(4):309–12.
Wang P-Y, Zhuang J, Hwang PM. p53: exercise capacity and metabolism. Curr Opin Oncol. 2012;24(1):76–82.
Wang M, et al. Prepubertal physical activity up-regulates estrogen receptor β, BRCA1 and p53 mRNA expression in the rat mammary gland. Breast Cancer Res Treat. 2009;115(1):213–20.
Higgins KA, et al. Exercise-induced lung cancer regression: mechanistic findings from a mouse model. Cancer. 2014;120(21):3302–10.
Barnard RJ, et al. A mechanism to explain how regular exercise might reduce the risk for clinical prostate cancer. Eur J Cancer Prev. 2007;16(5):415–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Savage, H., Schadler, K.L. (2020). Mechanisms of Exercise in Cancer Prevention, Treatment, and Survivorship. In: Schmitz, K. (eds) Exercise Oncology. Springer, Cham. https://doi.org/10.1007/978-3-030-42011-6_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-42011-6_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-42010-9
Online ISBN: 978-3-030-42011-6
eBook Packages: MedicineMedicine (R0)