Abstract
Nano-drug delivery carriers have fascinated researchers worldwide for the last two to three decades. The nanoformulations are preferred over conventional dosage forms as they provide improved drug solubility, bioavailability, drug stability under adverse external or physiological conditions, controlled drug release for prolonged action and target specificity using ligand binding and many more. Multiple essential aspects must be carefully studied and implemented for the development of efficient drug delivery vehicles. These aspects include rationale of nanoparticle preparation; use of polymeric or lipid nanoparticle; selection of polymer, lipid and excipients; method of preparation; screening of critical formulation or process parameters that affect the critical quality attributes; optimization of process to obtain the desired formulation characteristics; characterization of nanoparticles; strategy to improve the low entrapment efficiency and stability, etc. This chapter comprehensively summarizes all these aspects of nanoformulation development and proposes solutions for these challenges. Although a variety of nanoformulations have been described in literature, this chapter is restricted to discuss in detail the liposomes and polymeric and lipid nanoparticles.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Nanoformulation
- Polymeric nanoparticles
- Liposomes
- Lipid nanoparticles
- Characterization of nanoparticles
- Micelles
- Design of experiments
1 Introduction
Nanotechnology, a multifaceted development in science, has emerged as a breakthrough providing superiority over conventional technology due to robustness, accuracy and higher efficiency over the conventional approaches. Specifically, in medical science, researchers have explored several applications of nanotechnology including diagnostics, medical devices, imaging systems, drug delivery, etc. For the past few decades, extensive research conducted worldwide has directed us to learn the broader and multiple applications of nanotechnology in drug delivery. The delivery system, with improved pharmaceutical aspects, encapsulating the drug within the nanostructured matrix ranging from 50 to 500 nm, is generally considered as a nano-drug delivery carrier. Nano-drug delivery system commendably overcomes the limitation of conventional dosage forms (tablets, capsules, powders, gels, etc.) such as low solubility, low bioavailability, frequent dosing, high dose, low stability, toxicity, low permeation across the skin and many more (Jain et al. 2014a, b, c; Kaler et al. 2014; Uchechi et al. 2014; Agrawal et al. 2017a, b).
Mostly, the nanoparticle matrix is either polymeric or lipid-based (solid lipid nanoparticle, nanostructured lipid carrier), and the optimization process of nanoparticles involves the consideration of several critical issues. Interestingly, the rationale of nanoformulation; the selection of polymer, lipid and excipients; solvent system; and method of preparation further depend upon the drug’s physicochemical properties, application purpose and route of administration. Moreover, the optimization of nanoformulations with desired characteristics, improvement of drug encapsulation within the matrix and production of stable formulation are the most challenging tasks while preparing the nano-drug delivery system. This chapter covers all such aspects precisely and elaborates on the importance of each step during the preparation of nanoformulations.
2 Rationale of Nanoformulations
Nanoformulations possess several advantages over the conventional delivery systems and thus were found to have several applications depending upon the need. Examples of various nanoparticles developed in contemporary research with various objectives/rationales are listed in Table 3.1. A list of marketed nanoformulation has also been provided in Table 3.2.
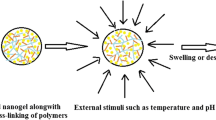
The rational of developing nanoformulations has been illustrated in Fig. 3.1 and described in the following sections.
2.1 Increase the Solubility of Poorly Soluble Drugs
Several studies based on nanotechnology approaches to improve the solubility and thus the absorption and bioavailability of drugs, which ultimately reduces the required dose, have been reported (Jain et al. 2013a, b; Rai et al. 2016). Approximately, 40% of the available drugs in the market are either weak acid or weak base and mostly suffer from low solubility in water or physiological fluids (Lipinski 2002). Even though the lipophilic drugs show higher diffusion coefficient and absorbance from the gut, the drug with low water solubility (lipophilic) possesses low bioavailability (dissolution is an essential criterion for absorption, and only solubilized or molecularly dispersed drug can diffuse across the biological membranes; thus, insoluble drugs impede the diffusion of drug across the biological membrane). The nanoparticles have proven to improve the water solubility of the entrapped drug by enhancing the surface area-to-volume ratio and thereby offer the higher surface area for dissolution in vitro or in vivo. Thus, improving the dissolution rate ultimately improves diffusion and bioavailability (Chen et al. 2011). Apart from that, a drug with low water solubility requires a higher dose to meet the therapeutic need and concentration in blood. The nanoparticle efficiently reduces the dose by improving solubility, permeation and bioavailability (Hu et al. 2004).
The dissolution phenomenon can be easily understood by Noyes-Whitney equation:
Here, C is a drug concentration in solution, Cs is equilibrium solubility of the drug (the concentration of drug in diffusion medium is equivalent to the Cs), and (Cs – C) represents the concentration gradient. So according to Eq. 3.1, the higher the surface area of the formulation, the more is the dissolution.
2.2 Improve the Half-Life and Reduce the Dosing Frequency
Nanoformulations provide controlled release over time which improves the half-life of the drug in the systemic circulation which ultimately reduces the dosing frequency (Agrawal et al. 2015a, b, 2017a, b; Aqil et al. 2017a, b, 2019). The drug release is a critical parameter that meaningfully affects the performance in vivo. The modification in release profile may bring alteration in the onset of action, duration of action, drug’s half-life in the systemic circulation and consequently therapeutic potential. The drug encapsulated within the polymeric or lipid matrix of nanoparticles releases in a controlled manner for an extended period. The nanoformulations improve the systemic half-life of the drugs by encapsulating and releasing the drug at a controlled rate for longer duration and, therefore, maintain the minimum therapeutic drug level in the systemic circulation for longer duration and thereby reduce the need of multiple dosing (Zhang et al. 2008; Wen and Park 2010; Aqil et al. 2017a, b; Gade et al. 2019).
2.3 Reduce the Toxicity
Typically, the immediate-release dosage form may elicit drug toxicity by reaching the systemic drug concentration above the maximum tolerable dose or if the drugs have inherent fatal toxicity on the vital body organ or tissues. Nanoparticle modifies the release of drug from the matrix and maintains the drug concentration below the maximum tolerable concentration or within the therapeutic window and, therefore, has the potential to reduce drug toxicity. Moreover, the cytotoxic drugs (anticancer) are highly toxic and elicit the fatal adverse events on normal human body cells also due to systemic exposure and accumulation in the organs. Targeted nanoparticles show selective accumulation at the diseased site and thus protect the normal body cell from unnecessary higher drug exposure by releasing the drug at the diseased site and reducing the occurrence of potential side effects (Jain et al. 2013a, b, 2015a, b; Kushwah et al. 2018a, b, c, d). Doxorubicin-loaded polyalkylcyanoacrylate nanoparticles have been reported to show reduced systemic toxicity due to encapsulation and less accumulation at myocardial muscle toxicity (Couvreur et al. 1982). Exosomes (biological nanoparticles), having lipid and protein as major structural components , have been reported to reduce the general toxicity (Aqil et al. 2016; Munagala et al. 2017).
2.4 Improve the Permeability and Retention
The skin has been used as a drug delivery route for several therapeutic moieties in the form of gels, ointments and lotions. But the low permeability of drugs across the skin due to stratum corneum limits the application of this route only for potent drugs (maximum dose of 20 mg per day) or for local treatments (skin disease). The advantages of the transdermal route such as avoidance of the first-pass metabolism and slow and steady release of drugs for a longer period always fascinated the researchers. A variety of inorganic and organic nanoparticles, specifically solid lipid nanoparticles and nanostructured lipid carriers, have been reported to show higher retention within the skin and permeation across the skin as compared to the conventional dosage form (gels, ointment, etc.) (Agrawal et al. 2010; Tomoda et al. 2011; Kaler et al. 2014). Similarly, the nanoparticles had a profound effect on the ocular permeability of the drugs. Nanoparticles significantly improve the corneal permeation and enhance the ocular bioavailability of drugs (Agrawal et al. 2012).
2.5 Regenerative Medicine
Nanotechnology has extended its application in the area of regenerative medicine including bone and neural tissue fabrication. The nanomaterial can be easily engineered to produce the crystal mineral human structure analogous to the bone tissue having the same strength and characteristics. Moreover, several successful attempts have been made to regenerate the human organ by growing the complex tissue within a day. Apart from that, the researchers are also working on quick healing of spinal cord injury using graphene nanoribbons, and preliminary studies performed have shown outstanding results with the growth of neurons (Engel et al. 2008; Mandoli et al. 2010).
2.6 Impart Stability at Different Environmental and Physiological Conditions
Several drugs , specifically protein-based drugs, degrade and lose their activity at various temperatures, humidity, sunlight and varying physiological conditions such as pH and presence of enzyme before it reaches the site of action (Harde et al. 2015a, b, c, d, e, f). Nanoparticles can overcome such limitations by protecting the drug within the polymeric or lipid matrix. Several studies have proved the protection from degradation following the encapsulation within the nanoparticles. Nanoparticles have demonstrated excellent insulin stability in gastric conditions and resulted in good oral bioavailability (Agrawal et al. 2013; Urimi et al. 2019).
2.7 Targeted Drug Delivery
The administered drug reaches every organ or tissue of the body by systemic circulation. So achieving the desired drug concentration selectively at the diseased site, to enhance the treatment efficacy or reduce the possible systemic toxicity, remains the foremost challenge for formulation scientists. Nanoparticles offer a larger surface area and easy surface modification for targeting the specific site using the ligands. These ligands are either adsorbed on the surface or covalently bind to specific groups present on the surface of the nanoparticles for active targeting to the pathogenic site. Some of the examples of ligands and targets are enlisted in Table 3.1. Recently, the potential use of functionalized nanoparticles is widely investigated to deliver the drug at a specific site for efficient therapy and reduced toxicity. These unconventional techniques utilize small molecules, peptides, antibodies, engineered proteins or nucleic acid aptamers as ligands (Byrne et al. 2008, Friedman et al. 2013, Agrawal et al. 2015a, b).
2.8 Diagnostic Imaging
The imaging techniques , viz. CT scan and MRI, depend on the contrast agent administered intravenously to evaluate the physiological condition and diagnosis of the disease. Apart from rapid diagnosis, the contrast agent currently in use has some limitation including the lack of specificity and potential systemic toxicity. Several investigations to explore the application of nanoparticles in the diagnosis purpose have revealed that nanoparticles are more sensitive and provide specific information without eliciting the significant systemic toxic effect (Xie et al. 2010; Rosen et al. 2011) by providing higher selectivity and accumulation to the targeted site along with the drug having therapeutic efficacy.
3 Classification of Nanoparticles
Nanoparticles can be classified in many ways:
-
1.
Classification based on origin
-
(a)
Organic – dendrimer, polymeric nanoparticles, lipid nanoparticles, etc.
-
(b)
Inorganic – gold nanoparticles, silver nanoparticles, silica nanoparticles, quantum dots, fullerene, etc.
-
(a)
-
2.
Classification based on application
-
(a)
Diagnostic
-
(b)
Imaging
-
(c)
Therapy
-
(a)
As this chapter is restricted to discuss liposomes and polymeric and lipid nanoparticles, a piece of brief information is provided here.
3.1 Micelles
Micelles are the colloidal spherical arrangement of the amphiphilic (have both hydrophilic and lipophilic end) lipids or polymers in the aqueous system (Fig. 3.2a). Micelles have a hydrophobic core and hydrophilic surface. Similarly, the reverse micelles with hydrophilic core and hydrophobic outer surface can be formed in the organic solvent. Micelles can easily accommodate the water-soluble drugs in the core and amphiphilic moiety within the structure. These are the stable arrangement with extended systemic circulation due to hydrophilic surface (Letchford and Burt 2007). Micelles have shown their potential to efficiently entrap the lipophilic drug, enhance the stability of the drug, penetrate the biological membrane and improve the therapeutic potential and targeted drug delivery.
3.2 Liposomes
Liposomes are bilayer spherical vesicles (Fig. 3.2b) made up of amphiphilic phospholipids and cholesterol. Liposomes are biocompatible and proven to be promising carriers for hydrophilic as well as hydrophobic drug moieties. The properties including surface charge and size may vary with lipid composition and the method of preparation. Moreover, the lipid constituents may also alter the rigidity and fluidity of the membrane. The phospholipids (unsaturated) with natural origin (egg and soybean phosphatidylcholine) tend to produce unstable, permeable and more fluidized bilayer; however, the saturated phospholipids, having long acyl chains like dipalmitoylphosphatidylcholine, produce comparatively more rigid and impermeable bilayer. Liposomes have fascinated researchers worldwide due to the use of physiological phospholipids which have been proven to be biocompatible, biodegradable and non-toxic for clinical applications (Jain et al. 2012). Most importantly, the liposomes can reduce the drug toxicity and target the drugs to the diseased site. The liposomes can be classified based on their application as a diagnostic and therapeutic purpose having entrapped various disease markers and bioactive molecules (Akbarzadeh et al. 2013).
3.3 Lipid Nanoparticles
Solid lipid nanoparticles (SLNs) are the most widely used nanoparticles, among the different lipid nanoparticles, which are prepared by using various physiological solid lipids. Another name under this category is nanostructured lipid carriers (NLCs) which are made up of solid as well as the liquid lipids and have shown improved encapsulation efficiency and stability. Generally, SLNs possess similar kind of molecules or crystals and on storage, temperature or relative humidity conditions trigger crystalline change from unstable state (irregular arrangement of crystal lattice) to more stable one (regular crystal) leading to the expulsion of encapsulated drug and instability of the system. However, NLCs possess two different kinds of lipids and thus are unable to rearrange in regular shape and provide the regular void for drug accommodation and thereby improve drug entrapment and stability. Lipid nanoparticles have been reported to deliver the drugs through various routes to even have liver and brain targeting (Müller et al. 2002; Schäfer-Korting et al. 2007). An in vivo study on lipid nanoparticles of flurbiprofen reported having improved transdermal permeation flux across the skin (Bhaskar et al. 2009). Similarly, the solid lipid nanoparticles of indomethacin have been reported to improve the transcorneal distribution of indomethacin in anterior and posterior lobe (Balguri et al. 2016). Several other studies have also been summarized to effectively deliver the drugs by using lipid nanoparticles (Harde et al. 2015a, b, c, d, e, f). A new class of nanoparticles, liquid crystalline nanoparticles, has also been reported to impart stability and improve the oral bioavailability of proteins (Singh et al. 2018).
3.4 Polymeric Nanoparticles
Polymeric nanoparticles , developed by using various polymers of either natural or synthetic origin, have been widely reported as drug delivery vehicles (Jain et al. 2015a, b; Kushwah et al. 2017). The polymeric nanoparticles may further be differentiated as nanospheres (Fig. 3.3a) and nanocapsules (Fig. 3.3b). In nanospheres, the drug is usually distributed uniformly in the polymeric matrix, while in nanocapsules, the drug is dispersed or dissolved within the liquid reservoir (either aqueous or oil) in the core covered by solid polymeric coating.
4 Formulation Development of Nanoformulation
4.1 Selection of Drug
The rationale of nanoparticle development as a drug delivery vehicle is dependent upon certain limitations associated with the physicochemical properties of the drug and the biological barriers and the disease’s pathophysiology.
4.1.1 Low Water Solubility
Most of the drugs are either weak acid or weak base and possess low solubility in water which results in poor dissolution rate, leading to poor absorption and thus poor bioavailability. Ultimately, it affects the pharmacokinetics and pharmacodynamics of the drug leading to low efficacy, slow onset of action and higher dose to achieve effective blood concentration. By entrapping the drug in the molecularly dispersed form inside the polymeric matrix, nanoparticles have been reported to improve dissolution, bioavailability, onset of action and therapeutic efficacy which is further helpful in reducing the dose size.
4.1.2 Short Half-Life
The systemic half-life of a drug is the time at which half of the total drug reaching the blood eliminates from the body. The basic reason for fast elimination or short half-life can be high polarity (easy renal excretion) or fast metabolism. The drugs with shorter half-life require frequent dosing to keep the effective blood concentration within the therapeutic window. Nanoparticles entrap the drug in the matrix and can overcome the fast metabolism and elimination. Simultaneously, the nanoparticles release the drug in a controlled and sustained way for longer duration which helps in maintaining the constant blood concentration and thus reducing the dosing frequency (Madan et al. 2013).
4.1.3 High Toxicity
Some drugs with high therapeutic efficacy induce severe systemic toxicity to other vital organs. Specifically, anticancer drugs along with their cytotoxic effect on cancerous cell induce lethal toxicity such as hepatotoxicity, nephrotoxicity, bone marrow depression, etc. Developing a nanoformulation for the delivery may overcome the toxicity by the restricted distribution of the nanoparticles to the diseased site (Sengupta et al. 2012).
4.1.4 High First-Pass Metabolism
The orally administered drug first undergoes the first-pass metabolism in the liver which is a pre-systemic metabolic in which fraction of absorbed drug is metabolized in the liver by microsomal enzymes after absorption from intestine before reaching to the systemic circulation. Consequently, the required concentration of drugs in blood is not attained and thus the higher dose is needed. Nanoparticles can evade the first-pass metabolism by enhancing the absorption of the drug from the lymphatic system which does not pass through the liver. Moreover, the systemically absorbed nanoparticles efficiently avoid the direct exposure of the drug to the enzyme and circumvent the metabolism. The drugs with the highest first metabolism are propranolol, raloxifene, morphine, pethidine, diazepam, lidocaine, midazolam, etc. There are several reports which indicated the bypass of the first-pass metabolism following the entrapment of drug into the nanoparticles (Yao et al. 2015).
4.1.5 Drug with Low Skin/Ophthalmic Permeation/Retention
Drugs intended to treat skin diseases or ocular ailments or drugs administered by transdermal route generally have low retention locally in the skin and low ocular and transdermal bioavailability perhaps due to low permeation across the skin, cornea and other ocular barriers. Several studies conducted on the efficiency on nanoparticles prepared for topical, transdermal and ophthalmic application proved to improve skin retention for local skin therapy, skin permeation and corneal permeation, and hence the drugs having the above-mentioned problems are good candidates to develop nanoformulations (Naik et al. 2004; Shim et al. 2004; Sahoo et al. 2008).
4.1.6 Chronic Pathophysiological Conditions
Chronic pathophysiological disease conditions such as diabetes, AIDS, tuberculosis and many others require long-term treatment regimen. Therefore, a strategy that can efficiently reduce rapid drug administration is desired for the patient’s compliance. Nanoparticles can maintain the required drug concentration in blood by extending the drug release from hours to several days, and hence developing nanoformulations for such drugs might be a good approach to improve the efficacy (El-Shabouri 2002; Sarmento et al. 2007).
4.2 Selection of Polymers and Lipids
It is mandatory to evaluate some of the parameters before starting the optimization of nanoformulation to achieve the nanoparticles with desired particle characteristics (particle size, zeta potential, polydispersity index, entrapment efficiency and in vitro release) and the desired therapeutic effect. At the same time, toxicity profiling is a regulatory mandate to assure the safety of the formulation on the human subject. Polymer or lipid (Table 3.3) used to form the nano-reservoir for the drug is selected based on numerous factors. The selection of polymers and/or lipids is again dependent upon multiple factors.
4.2.1 Physicochemical Compatibility with the Selected Drug Moiety
The polymer or lipid should not show any chemical interaction with the drug to ensure the inherent therapeutic activity and avoid the unwanted effects. Therefore, various techniques such as Fourier transform infrared spectroscopy (FTIR), differential scanning calorimetry (DSC) and X-ray diffraction are conducted to assess the possible interaction among the drug, polymer/lipid and other excipients (Patel et al. 2019a, b, c, d).
4.2.2 Biocompatibility and Toxicity
Neither polymer/lipid nor the metabolites should elicit harmful effect on human vital organs or tissues on short-term or long-term exposure. Therefore, toxicity profiling is very important before the selection of any polymer/lipid for nanoformulation development.
4.2.3 Biodegradability
The nanoformulations intended to be administered orally or systemically should be degraded in the human physiological environment to confirm its easy elimination from the body. The polymers with higher molecular weight may have slower elimination and thus may accumulate within different body tissues and induce severe toxicity (Seymour et al. 1987).
4.2.4 Desirable Particle Size
Polymeric and lipid nanoparticle size increases with an increased molecular weight of the polymer and lipid, respectively. Moreover, the lipid nanoparticles have been used to have a higher particle size range as compared to the polymeric nanoparticles. Hence, based on the desired application and route of administration, the polymer/lipid is selected.
4.2.5 Anticipated Release Profile
Nanoparticles have shown to have a controlled or sustained release profile (Yoo et al. 1999). The molecular weight of polymer/lipid is deciding property for the desired release profile. The polymer/lipid with higher molecular weight increases the release time for a longer period. Therefore, depending on the therapeutic need, the matrix component can be selected.
4.2.6 Inherent Properties of the Drug
This is a very common practice to select either the polymeric matrix or lipid matrix based on the drug solubility characteristic and its logP value. At the same time, the drug solubility in the lipids is determined to achieve the maximum possible encapsulation while optimizing the SLNs and NLCs.
4.2.7 Surface Charge and Permeability
The nature of the surface charge on the nanoparticles determines the interaction of particles with body cells and tissues.
4.2.8 Nonirritant
The formulation intended for the topical or ophthalmic purpose should be evaluated for the irritancy potential on the skin before the use. Therefore, the irritancy is one of the criteria to be considered while selecting the polymer or lipids for delivering a drug through these routes.
4.3 Selection of Solvents
The solvent system is a liquid vehicle used to prepare the solution or suspension of a particular compound for carrying out the experimentation. The solvent may be aqueous or organic. USFDA has classified the solvents into four different classes (Dixit et al. 2015) based on permissible residual limit in the formulation or drug products.
Class 1
The use of class I solvent is prohibited owing to its fatal toxicity on human or harmful effects on the environment until their use is necessary to complete the process for obtaining the product of significant therapeutic value. In that case, the residual limit should be validated according to the ICH Q3C guidelines, and the residual limits with their harmful effects are listed in Table 3.4.
Class 2
These solvents are again toxic and not allowed to use in drug unless mandatory. The permissible limit of residual solvents, of class 2, is shown in Table 3.5.
Class 3
The solvents belonging to this category are least toxic and have a lower risk to human health. None of the solvents in this class produce toxicity at its accepted limit level. The permissible quantity that can be allowed for human uptake is 5000 ppm or 50 mg/day or less without any prior clarification. The available data of toxicity is for short-term exposure and has never elicited genotoxicity. However, long-term toxicity and carcinogenic assessment on chronic exposure is needed to be performed for many of these solvents. The solvent of this class is depicted in Table 3.6.
While preparing the nanoparticles, selection of organic solvents or the combination of solvents, volume and their ratio affect the critical quality parameter of the final product and hence the selection of solvent should be done carefully to optimize the product. Moreover, solvent selection for any pharmaceutical manufacturing mainly depends on the following criteria:
4.3.1 Toxicity
As described above the solvent system used for any process or manufacturing should be less toxic, or the use of solvents with high toxicity should be justified and should be limited. Moreover, the residual limit should be maintained according to the guidelines.
4.3.2 The Solubility of Drugs/Excipients
Most of the experiments and manufacturing processes are performed in the solubilize state or by preparing the suspension, and there comes the role of solvents. Therefore, solubility is one of the critical parameters while selecting the solvent to get the product with the desired quality and high yield.
4.3.3 Volatility
Most of the drugs and excipients are solubilized in the organic solvents, and hence the use of an organic solvent is necessary for manufacturing purposes. However, organic solvent provokes human toxicity at a certain level. The solvent used should be volatile for easy removal after completion of the process.
4.4 Selection of the Excipients/Surfactants
According to the USFDA guideline, any substances intended to human use should be “generally recognized as safe (GRAS)”. Excipients are the chemicals or substances commonly used as drug carriers, bulking agents, disintegrators, binders or surfactants. Each class has a specific and important role in optimizing the product with the desired characteristic while preparing the drug product. Specifically, surfactants play a critical role in attaining stable nanoparticles with higher drug encapsulation and are reported to increase the oral bioavailability of a variety of nanoformulations (Jain et al. 2017; Shilpi et al. 2017). The surfactant may be anionic, cationic or non-ionic, and depending upon the intended use, the appropriate surfactant is selected. The regulatory authority needs assurance in terms of safety and efficacy data for approval of particular excipients. Besides several other factors, the following are the important factors that are considered before the final selection of the surfactant for formulation development.
4.4.1 Toxicity
On selecting the particular excipients, safety in clinic remains a major concern. The excipient should not be toxic. Therefore, long-term toxicity and short-term profiling need to be checked, if available, or evaluated, if not available.
4.4.2 Inertness
The compound/surfactant should be inert, i.e. should not interact chemically or physically, which may affect the efficacy of the drug product in terms of lost or diminished therapeutic activity or may exhibit toxicity.
4.4.3 Required Surface Charge
Depending upon the use and application, the surfactant can be utilized during the preparation of nanoparticles to impart specific charges (positive or negative). Charged particle stability depends on the zeta potential; however, non-ionic surfactants are long-chain polymers that provide stability by steric hindrance. Surfactant molecules adsorb on the newly formed nanoparticle surface while processing and provide stability and also prevent drug expulsion from the matrix. Therefore, the surfactant is the key factor for optimizing the formulation with the highest stability and encapsulation efficiency (Khdair et al. 2008).
4.4.4 Application
Excipients/surfactants are chosen based on the area or route of administration because the excipients used topically may have toxicity on systemic consumption. Therefore, the surfactant and excipients can also be grouped based on topical and systemic use.
4.5 Selection of Method of Preparation
There are several methods enlisted in the literature for the preparation of the drug nanoparticles. The selection of the method depends on the type of nanoparticles and physicochemical properties of polymer and drug. Factors which influence the choice of the apposite technique are enlisted below:
-
The solubility of drug and polymer
-
Thermal sensitivity of the drug
-
Type of nanoformulations
Several methodologies, commonly practised to fabricate the different kinds of nanoparticles in contemporary research, are elaborated below.
5 Method of Preparation for Polymeric/Lipid Nanoparticles
5.1 Solvent Evaporation Method
Solvent evaporation technique is the most extensively used process for nanoparticle preparation of hydrophobic drug and polymer. Briefly, there are two phases, one organic containing the dissolved drug and polymer and second aqueous phase supplemented with the desired surfactant to form the o/w emulsion (appropriate concentration). The organic phase is gradually mixed to the aqueous phase to produce the o/w type emulsion followed by high-speed homogenization or sonication to produce the desired nanoparticle size. Finally, the solvent is allowed to evaporate to initiate the polymer precipitation by reducing the pressure or by continuous stirring. The commonly used solvents are dichloromethane, chloroform or ethyl acetate. In this method, the particle size can be controlled by adjusting the polymer concentration, stabilizer, sonication time, viscosity of organic phase, homogenization speed and temperature (Lee et al. 2006).
5.2 Double-Emulsion and Evaporation Method
This is the modification of the solvent evaporation method to overcome the limitation to successfully incorporate the hydrophilic drug in the nanoparticles up to a maximum extent. Precisely, the drug-containing aqueous phase is added to an organic system containing w/o type emulsifier to form the primary w/o emulsion. Subsequently, the primary w/o emulsion is steadily mixed with a surfactant solution to produce the w/o/w emulsion at high homogenization speed. Eventually, the system is kept for the solvent removed to obtain the nanoparticles. The polymer concentration, drug quantity, organic to aqueous ratio and homogenization speed are the crucial factors that majorly affect the particle size and entrapment efficiency of the nanoparticles (Zambaux et al. 1998).
5.3 Solvent Displacement/Precipitation Method
This is one of the frequently used methods for preparing the nanoformulations of hydrophobic drugs. Moreover, this technique can be efficiently utilized to obtain the nanoparticles of thermosensitive drugs. Concisely, a water-miscible organic solvent is selected to dissolve the drug and polymer and form the organic phase. The most frequently used organic solvent is acetone; however, ethanol can also be used. Secondly, the preformed polymeric organic phase is injected slowly at a particular rate in the surfactant-rich aqueous phase. The surfactant system is kept at a magnetic stirrer at an optimized speed sufficient enough to break the drops and produce the nano-droplets. Once the organic phase comes into contact with water, it starts diffusing in water gradually due to hydrophilic affinity. The diffusion of organic solvent leads to supersaturation and nucleation of drug-polymer and induces the formation of nanoparticles. Formulation parameters such as drug/polymer ratio, polymer quantity and organic-to-aqueous phase ratio can be optimized to achieve the desired nanoparticle characteristics. Likewise, process parameters, viz. stirring rate and injection rate , also affect the quality of the particle (Lince et al. 2011).
5.4 Coacervation or Ionic Gelation Method
Nanoparticle formulation by ionic gelation method depends upon the alteration of pH of polymeric solution and formation of electrostatic bonding between the charged group of the polymer and the crosslinking agents (sodium TPP). This method is commonly employed to prepare the nanoparticles of hydrophilic polymers such as gelatin, sodium alginates and chitosan. For making the chitosan nanoparticles, the aqueous solution of chitosan in acetic acid is mixed with polyanion sodium tripolyphosphate (TPP) with continuous stirring. The anionic phosphate group of TPP is crosslinked electrostatically with an amino group of chitosan and forms the coacervates of nanosize range. The existence of strong electrostatic interaction between two aqueous phases results in the conversion of liquid into a gel-like matrix (Fan et al. 2012; Harde et al. 2014).
5.5 Supercritical Fluid Technology
Unlike all the above conventional techniques , supercritical fluid techniques do not require the use of organic solvents. Apart from that, supercritical fluid technology produces particles with a minimum size and uniform size distribution. It may be considered as the second-generation method for the preparation of nanoparticles which is not harmful to the environment and health but requires specialized equipment and supercritical fluids. These are the fluids that remain in the liquid phase and unaffected by pressure above its critical temperature. The most commonly used cheap, non-toxic supercritical fluid is CO2. This technique of nanoparticle preparation involves two major methods:
-
Supercritical fluid anti-solvent technique (SAS)
In this method drug solution in an organic solvent (anti-solvent) is mixed with supercritical CO2. The quick dissolution of supercritical CO2 into organic solvent results in the precipitation of drug molecules in the form of nanoparticles (Reverchon 1999). The nanoparticles of a hydrophilic drug such as dexamethasone phosphate have been successfully prepared using this technology.
-
The rapid expansion of supercritical solution (RESS)
In this method, drug and polymer are directly solubilized in the supercritical fluid and sprayed through the nozzles for expansion. Rapid expansion results in an abrupt decrease in pressure leading to precipitation in the form of nanoparticles (Sun et al. 2005). The nozzle size, type of supercritical fluid, spraying rate and polymer concentration affect particle size and particle size distribution significantly.
5.6 Polymerization Method
This method was firstly reported for the grafting of nanoparticles using the polymerization of butyl cyanoacrylate into polybutyl cyanoacrylate. This method involves the preparation of nanoparticles using the monomer and can be easily controlled to attain the required particle size and uniform particle distribution. Interestingly, the drug can be either incorporated in the polymerization medium before polymerization or adsorbed on the nanoparticle surface after polymerization. Particle size and other particle characteristics can be controlled by optimizing the concentration of the monomer in the reaction mixture, surfactant concentration and reaction time (Gnanakan et al. 2009).
5.7 High-Pressure Homogenization
High-pressure homogenization is an extensively employed technique to produce solid lipid nanoparticles and nanostructured lipid carriers on a laboratory scale. It can be further classified as cold homogenization and hot homogenization.
-
Hot homogenization
In this technique, the drug is dissolved or dispersed evenly in the lipid melt and homogenized at high speed in the melt state only. Finally, the preformed dispersion is homogenized at high pressure to form the nanoparticles. Unfortunately, this method cannot be applied to thermos-sensitive drugs (Jenning et al. 2002).
-
Cold homogenization
The SLNs and NLCs of highly temperature-sensitive drugs can be obtained by using cold homogenization. At the same time, hydrophilic active moiety, which might show phase separation in water, can be entrapped into the lipid nanoparticles using this technique. The drug is dissolved in the lipid matrix on short time exposure cooled down to produce solid mass and micronized. Finally, the micronized particles are dispersed in an aqueous solution containing stabilizer and homogenized at high pressure to achieve the nanoparticles.
6 Preparation of Liposomes
Liposomes can be fabricated by several methods reported in the literature (Akbarzadeh et al. 2013). The following section briefly describes such methods to prepare liposomes.
6.1 Membrane Hydration Method
The membrane hydration technique is the most commonly used method to produce large unilamellar vesicles (LUV). The organic solution (usually chloroform and ethanol combination) of lipid is placed in the round bottom flask and allowed to rotate with the simultaneous application of vacuum to form the thin lipid layer in the round bottom flask. Further addition of aqueous phase and rotation without vacuum result in the formation of LUVs. Both hydrophobic and hydrophilic drugs can be incorporated by adding in the lipid solution at the time of film formation or aqueous solution at the time of hydration, respectively. These LUVs can be converted to small unilamellar vesicles (SUVs) by using sonication or extrusion.
6.2 Mechanical Dispersion Methods
There are various methods categorized under mechanical dispersion for liposome preparation:
-
Sonication
Sonication is the most preferred method to prepare liposomal formulation. The multilamellar vesicles (MLVs ) are sonicated to produce SUVs by using sonic energy. Even being most preferred method, the sonication process is associated with some limitations in terms of polydispersity, low entrapment, low vesicular internal volume, metal contamination, phospholipid’s degradation, high energy wave generates the high temperature in the formulation that may degrade temperature-sensitive active compounds (proteins, peptides).
-
French pressure cell
This method is preferred for the temperature-sensitive (proteins and peptides) compounds that cannot be entrapped into the liposomes by sonication. It does not affect the internal structure of proteins and peptides and is therefore preferred for sensitive molecules. Precisely, preformed MLVs are passed through the fine orifices of the French press at high pressure to generate the small vesicles. Moreover, the stability of SUVs is higher concerning the expulsion of the drug from the liposome compared to those formed by sonication. Unlike the sonication, it can process only very low volume at a time.
6.2.1 Solvent Dispersion Methods
-
Ether injection (solvent vaporization)
In this method , the lipid solution prepared in the diethyl ether or in a combination of methanol is slowly injected to the buffer at a temperature above the melting point of lipid or under reduced pressure. Subsequently, the solution is kept under reduced pressure to eliminate the ether and initiate the formation of liposomal vesicles. The major drawbacks of this method are (1) formation of an azeotropic mixture of ether with water which is difficult to remove from the final formulation and (2) production of a heterogeneous population of liposomes.
-
Ethanol injection
Lipid is dissolved in the ethanol instead of ether in this process and gradually injected into the excess aqueous buffer to create the MLVs. Finally, the formulation is allowed to remove the ethanol under reduced pressure. Moreover, heterogeneous vesicle formation and the presence of residual ethanol in the final formulation are the major drawbacks associated with this method.
-
Reverse phase evaporation method
Reverse phase evaporation technique is an advanced method for achieving the liposomes with high entrapment efficiency (maximum up to 65%) for hydrophilic moiety and high aqueous space to lipid ratio. Interestingly, this method forms the inverted micelles. Concisely, the lipid dissolved in an organic solvent is dispersed in the aqueous buffer supplemented with drug and subsequently sonicated to arrange the phospholipid molecule into liposomal vesicles. Finally, the inverted micelles are generated while removing the organic phase gradually from the mixture under vacuum. The isopropyl ether, diethyl ether, chloroform and their mixture are the most commonly used organic solvents for dissolving phospholipid. Moreover, the method has already been investigated for encapsulation of several compounds including small, medium and large molecules. Major drawbacks include the residual solvent and denaturing of sensitive molecules like proteins and peptides.
6.2.2 Microencapsulation Vesicles (MCV)
The MCV is a highly reproducible preparation technique for liposome that competently creates the liposome with uniform particle size and higher entrapment efficiency. This method can encapsulate the water-soluble, lipophilic as well as amphiphilic drugs. The drugs can be dissolved either in the aqueous phase or organic phase before the preparation of liposome. The method is a two-step process; initially, w/o emulsion is prepared by dispersing the lipid dissolved in the organic phase in the aqueous phase with continuous stirring. Finally, the primary w/o emulsion is gradually added to the water to produce the w/o/w emulsion and kept at stirring to remove the organic phase using the vacuum and produce the liposome (Nii and Ishii 2005).
7 Identification of Variables
There are mainly two kinds of variables:
-
1.
Dependent variable/critical quality attributes
-
2.
Independent variables/formulation/process variables
7.1 Critical Quality Parameters or Dependent Variables
Critical quality attributes are the characteristics of the final formulation that will have a direct impact on the therapeutic performance of the developed formulation. These are also known as dependent variables because their values depend on the independent variables. So before starting the optimization of the process for fabricating the quality product, quality parameters are needed to be identified, and the desired limit should be set. Particle size, polydispersity index (PDI), zeta potential and entrapment efficiency are generally considered as major dependent variables for any kind of nanoformulation. Particle size is an important parameter as it directly affects the nanoparticle uptake, while PDI is responsible for the homogeneity of the formulation. Zeta potential plays a crucial role in nanoformulation’s stability as well as cellular uptake, while entrapment efficiency is a direct measure of the efficiency of the delivery vehicle in carrying the maximum amount of drug to the target site .
7.2 Formulation and Process Factors or Independent Variables
After setting the limits of desired quality attributes , critical formulation or process parameters, which significantly affect the critical quality attributes of the formulation, need to be identified to further optimize the process. Depending on the method, type and formulation, there are several factors (Sharma et al. 2016) that play a crucial role in achieving the quality product. The identified parameters that affect the quality of nanoparticles are as follows:
-
(i)
Organic-to-aqueous phase ratio
-
(ii)
Drug-to-polymer/lipid ratio
-
(iii)
Amount of polymer/lipid
-
(iv)
Surfactant concentration
-
(v)
Homogenization speed
-
(vi)
Working temperature
-
(vii)
Sonication time
-
(viii)
Vacuum pressure
-
(ix)
Rotation speed
-
(x)
Homogenization time
-
(xi)
Injection rate
-
(xii)
pH of the working solutions
Depending on the extent of their influence on the quality, the factors are selected for further optimization while keeping the remaining factors constant. The factors and their required levels can be designated based on the knowledge, previous studies reported in the literature and experimental approach. In an experimental approach, keeping all other factors constant, a single factor is varied to measure its influence on particle size, PDI, zeta potential and entrapment efficiency. At last, depending on the comparative analysis of data for each factor, significantly affecting factors are selected for the final process to be optimized.
8 Optimization of Process and Product
Process optimization is a step where all the critical steps are controlled to produce the product with desired quality. Similarly, in nanoformulations, the process and formulation parameters affecting the process and formulation quality are identified and controlled to obtain the product with predefined quality.
Once the critical quality attributes and the factors affecting those attributes are identified, experiments are designed with the varying combination of independent levels to obtain the nanoparticles with desired particle size, PDI, zeta potential and entrapment efficiency. The formulation with the best set of nanoparticle responses is selected as optimized and further evaluated for the respective studies. Design of experiments, a statistical tool, is now available to get the formulation with desired quality attributes (Turk et al. 2014).
9 Design of Experiments
It is a statistical method to optimize the formulation systematically. It involves the well-organized experimental approach to design the experiments and attains the optimized product by finding the optimized levels of variables from the statistical analysis of responses (for dependent variables) obtained in the experiments. Simultaneously, with optimized levels, it also explains the effect of variables on the response and their interaction. The design of experiments is an emerging tool for pharmaceutical product development that ensures the quality, safety and efficacy of the drug products. Moreover, it reduces the time consumption and resource wastage and improves process performance.
The design of experiment is completed in four basic steps:
-
1.
Based on the requirements, a number of factors and their selected levels, experiments are generated using the various DOE models.
-
2.
Experiments are performed and the responses are recorded for each experiment set.
-
3.
Statistical analysis of data to predict the optimized level of each independent variable along with the predicted response. Moreover, it also generates the polynomial equation elaborating on the effect of the variables on the responses.
-
4.
The optimized batch with predicted levels is prepared, and the responses are compared with predicted responses to determine the standard deviation (should not be more than 10% to assure the authenticity of the process).
During optimization, various models can be used from preliminary screening of factors to select their level and for the final study of their effect. It will again depend on the formulator to choose a suitable model for study and help in minimizing the experimentation time.
10 Factorial Design
Though the factorial design is ideally chosen for the screening of primary factors affecting the formulation to further design the experiments, it can be used to optimize the process also (Vandervoort and Ludwig 2002). There are several numbers of factorial designs available and selected according to suitability:
-
Two-level factorial designs
2–21 factors with two-level (−1–1) can be studied at a time by full and fractional designs each factor to only two levels. Fractional factorials are an effective method to screen out the factors having a significant effect on the process and product. At the same time, it can predict the effect of factor interaction.
-
General factorial designs
This is a special experimental design in which factors (1–12 maximum) have a different level (2 to 299) used to determine the critical factor. The method generates all possible combinations of factors with different levels.
-
Plackett-Burman designs
This is a useful technique to evaluate up to 31 factors by assuming that the factors do not possess a significant effect.
-
Taguchi designs
Not more than 63 factors can be studied simultaneously. There are number of designs available based on the number of factors to reduces the number of experiments.
11 Response Surface Design Selection
Response surface method (RSM) designs quantitatively determine the effect of various factors on the responses in terms of a polynomial equation and plot them as a surface plot to elaborate the effect. Moreover, it predicts the optimized level in the space with predicted responses from the statistical analysis of the responses generated in the experiment for a designed set of experiments. The levels are predicted by the desirability method; the desired responses selected (maximum or minimum or may be quantitatively selected) over the range of stable responses consequently predict the optimized level point. For this method, the level of the factor should be defined numerically or quantitatively. All the responses can be predicted with a combined set of factors.
12 Box-Behnken Design
When the process has three to ten factors to optimize and had three levels, the Box-Behnken is preferred. This design requires only three levels, coded as −1, 0 and + 1. The advantage of this design over the other is that very few experiments are needed to attain the designs with anticipated statistical properties. The quadratic model is the best model to explain the obtained findings and effect of a single factor or interaction of factor on the response, as the factors only have three levels and have been reported to optimize a variety of nanoformulations for oral immunization (Harde et al. 2015a, b, c, d, e, f).
13 Central Composite Design (CCD)
The CCD is a widely preferred response surface method to design the experiments and optimize the process (Hao et al. 2012). It can be divided into three groups of design points:
-
(a)
Two-level factorial or fractional factorial design points
-
(b)
Axial points
-
(c)
Centre points
14 Mixture Design Selection
This method is generally preferred over another method if:
-
1.
The components add to a fixed total. For instance, A is 10% of the mixture, B is 30% and C is the remaining 60%. If the percentage of one component is increased, then the percentage of one or more of the other components must be decreased. If the component amounts do not depend on each other, then response surface designs should be preferred over mixture designs (Choisnard et al. 2005).
-
2.
The response must be a function of the proportions of the components. For example, the flavour of ice cream depends on the relative proportions of the ingredients, not on the total amount of ice cream. If the response is not related to the ingredient proportions, then response surface designs should be used.
15 Characterization of Nanoparticles
There are various characterization methods performed to evaluate the quality of the nanoparticles. The characterization techniques are depicted in Fig. 3.4 and briefly described below.
15.1 Particle Size and Polydispersity Index
Particle size and polydispersity index are very important parameters for any nanoformulation as they may directly affect the therapeutic performance (Harde et al. 2015a, b, c, d, e, f). Particle size analysis is conducted by photon correlation spectroscopy also called dynamic light scattering. The particle size is obtained as a function of correlation of scattered intensity to the particle’s diffusion coefficient. It measures the change in the intensity of scattered light during the analysis concerning the volume of particles. The polydispersity index is a measure of particle distribution over the size range. The higher polydispersity index is the indication of heterogeneity in the particle size range.
15.2 Zeta Potential
The zeta potential has been considered as one of the very important parameters for the nanoformulation optimization as this is considered as stability of nanoformulations in suspension form (Harde et al. 2015a, b, c, d, e, f). The zeta potential measurement is based on the movement of charged nanoparticles dispersed in liquid in the direction of cathode or anode (depending on the charge on NPs) on applying the electric field in the sample. Briefly, the electric field is applied across the sample to induce mobility. Further, the electrophoretic mobility is determined in terms of the ratio of nanoparticle velocity and the electric field . Finally, the zeta potential is calculated using the Henry equation.
15.3 Entrapment Efficiency
Entrapment efficiency is calculated to find out the total drug encapsulated within the nanoparticles. The entrapment efficiency can be measured by either direct method or indirect method. The direct method measures the drug entrapped within the nanoparticles while in the indirect method the unentrapped drug is determined to calculate the drug entrapped within the nanoparticles (Harde et al. 2015a, b, c, d, e, f).
15.4 In Vitro Release
Determining the in vitro release is a very important parameter to predict the in vivo response in different physiological pH conditions (Das et al. 2014; Jain et al. 2014a, b, c). The nanoparticles or the formulation to be tested is suspended in the simulated physiological fluid or buffer of particular pH maintained at 37 °C and constant stirring. The conditions vary according to the route of administration to mimic the corresponding physiological conditions. The samples of dissolution medium are collected at various time intervals and analysed using the UV spectroscopy or HPLC depending on the suitability and sensitivity, to determine the drug concentration. Finally, the amount of drug released is calculated for each sampling period.
15.5 Scanning Electron Microscopy (SEM)
SEM has been widely reported to study the shape and surface morphology of a variety of novel formulations (Choudhary et al. 2010). This is direct visualization of prepared nanoparticles. Along with shape and morphology, actual particle size can also be measured by SEM. Before SEM analysis, properly diluted nanosuspension is dried over the copper strip and coated with gold to make it electrically conducting using the coater equipment. Then the coated nanoparticles are scanned by an electron beam over the focused area, and the secondary electron emitted from the surface is collected to attain the evidence about the surface morphology and shape of the particles.
15.6 Transmission Electron Microscopy (TEM)
In addition to the SEM, transmission electron microscopy is an excellent and widely reported tool for determining the exact shape and particle size of the nanoparticles (Jain et al. 2014a, b, c). A high potential electron beam is bombarded on the thin sample prepared in the metallic mesh (TEM grid), and once the electron beam interacts with the surface of the particles, it transmits the electrons which are captured by the detector to generate the crystal structure and shape and calculate the particle size. High-resolution TEM is an accurate technique generally applied to evaluate the quality, shape, size and density of nanoparticles. The TEM utilizes the high-potential electron for analysis rather than using the light rays. The magnification of TEM is much higher than other imaging techniques as the technique uses a low-wavelength electron beam.
15.7 Fourier Transform Infrared Spectroscopy (FTIR)
Fourier transform infrared spectroscopy is an analysis technique that determines the presence of specific functional groups in the compound in the form of transmittance peak in FTIR spectra corresponding to specific wavenumbers. During the processing, the drug may interact physically or chemically with the formulation component and can lose the activity or may elicit unwanted toxicity. FTIR is one of the widely conducted studies to assess the possible interaction (Patel et al. 2019a, b, c, d). Loss of peak corresponding to a specific functional group in the drug or appearance of some unknown peak in the spectra indicates the interaction. Moreover, the technique also qualitatively evaluates the drug entrapment in polymeric or lipid matrix.
15.8 Differential Scanning Calorimetry (DSC)
DSC is a thermal analysis usually conducted to define the melting point, glass transition temperature and melting enthalpy. This information can give us an idea about the crystalline nature qualitatively or quantitatively. Moreover, the interaction can also be evaluated with a significant shift in the melting point of the drug (Patel et al. 2019a, b, c, d). The sample equivalent to 10–20 mg is placed in the metallic pan and scanned over a certain temperature range. The endothermic peak gives the value of the melting point, while the disappearance of endothermic peak or intensity reduction signifies the loss of crystalline structure or conversion of the drug into an amorphous form. The % crystallinity can be calculated from the melting enthalpy. Melting enthalpy is directly proportional to crystallinity, and by keeping the pure drug 100% crystalline, the crystallinity of another sample can be obtained.
15.9 X-Ray Diffraction (XRD)
XRD is performed to determine the crystalline or amorphous structure of a compound and can be considered a universally accepted technique for the determination of drugs following the entrapment within the nanoformulation (Patel et al. 2019a, b, c, d). For taking the XRD spectra, the powdered sample is placed on the goniometer and thrown with the X-ray beam at a varying angle of diffraction (2θ; 10–80°). The diffracted beam of X-ray is collected by the detector to generate the X-ray diffraction pattern. The X-ray diffraction pattern of crystalline material exhibits high-intensity diffraction peaks at certain diffraction angles and has a specific arrangement for a particular compound. However, the amorphous compound does not possess a highly intense diffraction pattern. Interestingly, the nanoparticles convert the crystalline material into amorphous; thus, XRD is employed to determine the change in the crystalline structure of the drug.
16 Major Challenges
Though research in the field of nanomedicine has attained considerable success, very few nanoformulations got FDA approval in the last two to three decades of nanomedicine research. The safety, efficacy, scalability and regulatory compliance for nanoformulations are the major challenges.
17 Safety or Toxicity
Manufacturers have the responsibility to submit the appropriate and sufficient human toxicity data to regulatory agencies for approval of the drug product to assure the safety of drugs intended to be used in the clinic. The companies have to perform preclinical and clinical trials to generate sufficient toxicity data to fill the new drug application (NDA) or investigational new drug application (INDA) for FDA approval. Therefore, pharmacokinetics should be studied for any new product proposed for therapeutic use. Intensive study of the absorption, distribution, metabolism and excretion to establish complete pharmacokinetic profile to ensure safety is needed.
18 Scalability
Scalability, a process of manufacturing at an industrial level for clinical use, is a major challenge faced by the manufacturers. The optimization of the process for the efficient production of nanoformulations on a large scale is a difficult task. The unavailability of capable equipment, process controls and trained personnel and noncompliance with current good manufacturing practices pose impediments to manufacturing the nanoformulations at commercial level. Moreover, the unavailability of clear-cut regulatory guidelines is another challenge in maintaining quality standards.
19 Conclusion
Nanoformulations have been presented as a solution to overcome many of the challenges with conventional drug delivery; however, critical evaluation of different process and formulation variables, viz. selection of the right delivery system, polymer/lipid and solvent, method of preparation and exhaustive characterization, is needed to develop nanoformulations with the desired quality attributes for better therapeutic performance. Although extensive research in this field has resulted in the development of a handful of clinically approved products, finding a biocompatible material with minimal possible toxicity and scalability is the major issue that needs attention.
References
Agrawal A, Gupta P, Khanna A, Sharma R, Chandrabanshi H, Gupta N, Patil U, Yadav S (2010) Development and characterization of in situ gel system for nasal insulin delivery. Pharmazie 65(3):188–193
Agrawal AK, Das M, Jain S (2012) In situ gel systems as ‘smart’carriers for sustained ocular drug delivery. Expert Opin Drug Deliv 9(4):383–402
Agrawal AK, Harde H, Thanki K, Jain S (2013) Improved stability and antidiabetic potential of insulin containing folic acid functionalized polymer stabilized multilayered liposomes following oral administration. Biomacromolecules 15(1):350–360
Agrawal AK, Urimi D, Harde H, Kushwah V, Jain S (2015a) Folate appended chitosan nanoparticles augment the stability, bioavailability and efficacy of insulin in diabetic rats following oral administration. RSC Adv 5(127):105179–105193
Agrawal AK, Urimi D, Jain S (2015b) Multifunctional polymeric nano-carriers in targeted drug delivery. In: Targeted drug delivery: concepts and design. Springer, Cham, pp 461–500
Agrawal AK, Aqil F, Jeyabalan J, Spencer WA, Beck J, Gachuki BW, Alhakeem SS, Oben K, Munagala R, Bondada S (2017a) Milk-derived exosomes for oral delivery of paclitaxel. Nanomedicine 13(5):1627–1636
Agrawal AK, Kumar K, Swarnakar NK, Kushwah V, Jain S (2017b) “Liquid crystalline nanoparticles”: rationally designed vehicle to improve stability and therapeutic efficacy of insulin following oral administration. Mol Pharm 14(6):1874–1882
Akbarzadeh A, Rezaei-Sadabady R, Davaran S, Joo SW, Zarghami N, Hanifehpour Y, Samiei M, Kouhi M, Nejati-Koshki K (2013) Liposome: classification, preparation, and applications. Nanoscale Res Lett 8(1):102
Aqil F, Kausar H, Agrawal AK, Jeyabalan J, Kyakulaga A-H, Munagala R, Gupta R (2016) Exosomal formulation enhances therapeutic response of celastrol against lung cancer. Exp Mol Pathol 101(1):12–21
Aqil F, Jeyabalan J, Agrawal AK, Kyakulaga A-H, Munagala R, Parker L, Gupta RC (2017a) Exosomal delivery of berry anthocyanidins for the management of ovarian cancer. Food Funct 8(11):4100–4107
Aqil F, Munagala R, Jeyabalan J, Agrawal AK, Gupta R (2017b) Exosomes for the enhanced tissue bioavailability and efficacy of curcumin. AAPS J 19(6):1691–1702
Aqil F, Munagala R, Jeyabalan J, Agrawal AK, Kyakulaga A-H, Wilcher SA, Gupta RC (2019) Milk exosomes-natural nanoparticles for siRNA delivery. Cancer Lett 449:186–195
Balguri SP, Adelli GR, Majumdar S (2016) Topical ophthalmic lipid nanoparticle formulations (SLN, NLC) of indomethacin for delivery to the posterior segment ocular tissues. Eur J Pharm Biopharm 109:224–235
Bhaskar K, Anbu J, Ravichandiran V, Venkateswarlu V, Rao YM (2009) Lipid nanoparticles for transdermal delivery of flurbiprofen: formulation, in vitro, ex vivo and in vivo studies. Lipids Health Dis 8(1):6
Byrne JD, Betancourt T, Brannon-Peppas L (2008) Active targeting schemes for nanoparticle systems in cancer therapeutics. Adv Drug Deliv Rev 60(15):1615–1626
Casadó A, Sagristá ML, Mora M (2014) Formulation and in vitro characterization of thermosensitive liposomes for the delivery of irinotecan. J Pharm Sci 103(10):3127–3138
Chen H, Khemtong C, Yang X, Chang X, Gao J (2011) Nanonization strategies for poorly water-soluble drugs. Drug Discov Today 16(7–8):354–360
Cheow WS, Chang MW, Hadinoto K (2010) Antibacterial efficacy of inhalable levofloxacin-loaded polymeric nanoparticles against E. coli biofilm cells: the effect of antibiotic release profile. Pharm Res 27(8):1597–1609
Choisnard L, Géze A, Bigan M, Putaux J-L, Wouessidjewe D (2005) Efficient size control of amphiphilic cyclodextrin nanoparticles through a statistical mixture design methodology. J Pharm Sci 8(3):593–600
Choudhary H, Agrawal A, Malviya R, Yadav S, Jaliwala Y, Patil U (2010) Evaluation and optimization of preparative variables for controlled-release floating microspheres of levodopa/carbidopa. Pharmazie 65(3):194–198
Couvreur P, Kante B, Grislain L, Roland M, Speiser P (1982) Toxicity of polyalkylcyanoacrylate nanoparticles II: doxorubicin-loaded nanoparticles. J Pharm Sci 71(7):790–792
Das M, Jain R, Agrawal AK, Thanki K, Jain S (2014) Macromolecular bipill of gemcitabine and methotrexate facilitates tumor-specific dual drug therapy with higher benefit-to-risk ratio. Bioconjug Chem 25(3):501–509
Dhar S, Gu FX, Langer R, Farokhzad OC, Lippard SJ (2008) Targeted delivery of cisplatin to prostate cancer cells by aptamer functionalized Pt (IV) prodrug-PLGA–PEG nanoparticles. Proc Natl Acad Sci 105(45):17356–17361
Dixit K, Athawale RB, Singh S (2015) Quality control of residual solvent content in polymeric microparticles. J Microencapsul 32(2):107–122
El-Shabouri M (2002) Positively charged nanoparticles for improving the oral bioavailability of cyclosporin-A. Int J Pharm 249(1–2):101–108
Engel E, Michiardi A, Navarro M, Lacroix D, Planell JA (2008) Nanotechnology in regenerative medicine: the materials side. Trends Biotechnol 26(1):39–47
Fan W, Yan W, Xu Z, Ni H (2012) Formation mechanism of monodisperse, low molecular weight chitosan nanoparticles by ionic gelation technique. Colloids Surf B: Biointerfaces 90:21–27
Fazil M, Md S, Haque S, Kumar M, Baboota S, Sahni JK, Ali J (2012) Development and evaluation of rivastigmine loaded chitosan nanoparticles for brain targeting. Eur J Pharm Sci 47(1):6–15
Friedman AD, Claypool SE, Liu R (2013) The smart targeting of nanoparticles. Curr Pharm Des 19(35):6315–6329
Gade S, Patel KK, Gupta C, Anjum MM, Deepika D, Agrawal AK, Singh S (2019) An ex vivo evaluation of moxifloxacin nanostructured lipid carrier enriched in situ gel for transcorneal permeation on goat cornea. J Pharm Sci 108(9):2905–2916
Gnanakan SRP, Rajasekhar M, Subramania A (2009) Synthesis of polythiophene nanoparticles by surfactant-assisted dilute polymerization method for high performance redox supercapacitors. Int J Electrochem Sci 4(9):1289–1301
Gulyaev AE, Gelperina SE, Skidan IN, Antropov AS, Kivman GY, Kreuter J (1999) Significant transport of doxorubicin into the brain with polysorbate 80-coated nanoparticles. Pharm Res 16(10):1564–1569
Gupta H, Aqil M, Khar R, Ali A, Bhatnagar A, Mittal G (2011) Biodegradable levofloxacin nanoparticles for sustained ocular drug delivery. J Drug Target 19(6):409–417
Hafner A, Lovrić J, Pepić I, Filipović-Grčić J (2011) Lecithin/chitosan nanoparticles for transdermal delivery of melatonin. J Microencapsul 28(8):807–815
Hao J, Wang F, Wang X, Zhang D, Bi Y, Gao Y, Zhao X, Zhang Q (2012) Development and optimization of baicalin-loaded solid lipid nanoparticles prepared by coacervation method using central composite design. Eur J Pharm Sci 47(2):497–505
Harde H, Agrawal AK, Jain S (2014) Development of stabilized glucomannosylated chitosan nanoparticles using tandem crosslinking method for oral vaccine delivery. Nanomedicine 9(16):2511–2529
Harde H, Agrawal AK, Jain S (2015a) Tetanus toxoid-loaded layer-by-layer nanoassemblies for efficient systemic, mucosal, and cellular immunostimulatory response following oral administration. Drug Deliv Transl Res 5(5):498–510
Harde H, Agrawal AK, Jain S (2015b) Tetanus toxoids loaded glucomannosylated chitosan based nanohoming vaccine adjuvant with improved oral stability and immunostimulatory response. Pharm Res 32(1):122–134
Harde H, Agrawal AK, Jain S (2015c) Trilateral ‘3P’ mechanics of stabilized layersomes technology for efficient oral immunization. J Biomed Nanotechnol 11(3):363–381
Harde H, Agrawal AK, Katariya M, Kale D, Jain S (2015d) Development of a topical adapalene-solid lipid nanoparticle loaded gel with enhanced efficacy and improved skin tolerability. RSC Adv 5(55):43917–43929
Harde H, Siddhapura K, Agrawal AK, Jain S (2015e) Development of dual toxoid-loaded layersomes for complete immunostimulatory response following peroral administration. Nanomedicine 10(7):1077–1091
Harde H, Siddhapura K, Agrawal AK, Jain S (2015f) Divalent toxoids loaded stable chitosan–glucomannan nanoassemblies for efficient systemic, mucosal and cellular immunostimulatory response following oral administration. Int J Pharm 487(1–2):292–304
Hatakeyama H, Akita H, Ishida E, Hashimoto K, Kobayashi H, Aoki T, Yasuda J, Obata K, Kikuchi H, Ishida T (2007) Tumor targeting of doxorubicin by anti-MT1-MMP antibody-modified PEG liposomes. Int J Pharm 342(1–2):194–200
Hu J, Johnston KP, Williams RO III (2004) Nanoparticle engineering processes for enhancing the dissolution rates of poorly water soluble drugs. Drug Dev Ind Pharm 30(3):233–245
Hu K, Li J, Shen Y, Lu W, Gao X, Zhang Q, Jiang X (2009) Lactoferrin-conjugated PEG–PLA nanoparticles with improved brain delivery: in vitro and in vivo evaluations. J Control Release 134(1):55–61
Huang G, Zhang N, Bi X, Dou M (2008) Solid lipid nanoparticles of temozolomide: potential reduction of cardial and nephric toxicity. Int J Pharm 355(1–2):314–320
Jain S, Patil SR, Swarnakar NK, Agrawal AK (2012) Oral delivery of doxorubicin using novel polyelectrolyte-stabilized liposomes (layersomes). Mol Pharm 9(9):2626–2635
Jain S, Kumar S, Agrawal AK, Thanki K, Banerjee UC (2013a) Enhanced transfection efficiency and reduced cytotoxicity of novel lipid–polymer hybrid nanoplexes. Mol Pharm 10(6):2416–2425
Jain S, Sharma JM, Agrawal AK, Mahajan RR (2013b) Surface stabilized efavirenz nanoparticles for oral bioavailability enhancement. J Biomed Nanotechnol 9(11):1862–1874
Jain S, Harde H, Indulkar A, Agrawal AK (2014a) Improved stability and immunological potential of tetanus toxoid containing surface engineered bilosomes following oral administration. Nanomedicine 10(2):431–440
Jain S, Indulkar A, Harde H, Agrawal AK (2014b) Oral mucosal immunization using glucomannosylated bilosomes. J Biomed Nanotechnol 10(6):932–947
Jain S, Jain R, Das M, Agrawal AK, Thanki K, Kushwah V (2014c) Combinatorial bio-conjugation of gemcitabine and curcumin enables dual drug delivery with synergistic anticancer efficacy and reduced toxicity. RSC Adv 4(55):29193–29201
Jain S, Kumar S, Agrawal A, Thanki K, Banerjee U (2015a) Hyaluronic acid–PEI–cyclodextrin polyplexes: implications for in vitro and in vivo transfection efficiency and toxicity. RSC Adv 5(51):41144–41154
Jain S, Spandana G, Agrawal AK, Kushwah V, Thanki K (2015b) Enhanced antitumor efficacy and reduced toxicity of docetaxel loaded estradiol functionalized stealth polymeric nanoparticles. Mol Pharm 12(11):3871–3884
Jain S, Garg T, Kushwah V, Thanki K, Agrawal AK, Dora CP (2017) α-Tocopherol as functional excipient for resveratrol and coenzyme Q10-loaded SNEDDS for improved bioavailability and prophylaxis of breast cancer. J Drug Target 25(6):554–565
Jana S, Manna S, Nayak AK, Sen KK, Basu SK (2014) Carbopol gel containing chitosan-egg albumin nanoparticles for transdermal aceclofenac delivery. Colloids Surf B: Biointerfaces 114:36–44
Jenning V, Lippacher A, Gohla S (2002) Medium scale production of solid lipid nanoparticles (SLN) by high pressure homogenization. J Microencapsul 19(1):1–10
Kaler A, Mittal AK, Katariya M, Harde H, Agrawal AK, Jain S, Banerjee UC (2014) An investigation of in vivo wound healing activity of biologically synthesized silver nanoparticles. J Nanopart Res 16(9):2605
Katiyar S, Pandit J, Mondal RS, Mishra AK, Chuttani K, Aqil M, Ali A, Sultana Y (2014) In situ gelling dorzolamide loaded chitosan nanoparticles for the treatment of glaucoma. Carbohydr Polym 102:117–124
Ke W, Zhao Y, Huang R, Jiang C, Pei Y (2008) Enhanced oral bioavailability of doxorubicin in a dendrimer drug delivery system. J Pharm Sci 97(6):2208–2216
Khdair A, Gerard B, Handa H, Mao G, Shekhar MP, Panyam J (2008) Surfactant− polymer nanoparticles enhance the effectiveness of anticancer photodynamic therapy. Mol Pharm 5(5):795–807
Kisich K, Gelperina S, Higgins M, Wilson S, Shipulo E, Oganesyan E, Heifets L (2007) Encapsulation of moxifloxacin within poly (butyl cyanoacrylate) nanoparticles enhances efficacy against intracellular Mycobacterium tuberculosis. Int J Pharm 345(1–2):154–162
Krausz AE, Adler BL, Cabral V, Navati M, Doerner J, Charafeddine RA, Chandra D, Liang H, Gunther L, Clendaniel A (2015) Curcumin-encapsulated nanoparticles as innovative antimicrobial and wound healing agent. Nanomedicine 11(1):195–206
Kushwah V, Agrawal AK, Dora CP, Mallinson D, Lamprou DA, Gupta RC, Jain S (2017) Novel gemcitabine conjugated albumin nanoparticles: a potential strategy to enhance drug efficacy in pancreatic cancer treatment. Pharm Res 34(11):2295–2311
Kushwah V, Jain DK, Agrawal AK, Jain S (2018a) Improved antitumor efficacy and reduced toxicity of docetaxel using anacardic acid functionalized stealth liposomes. Colloids Surf B: Biointerfaces 172:213–223
Kushwah V, Katiyar SS, Agrawal AK, Gupta RC, Jain S (2018b) Co-delivery of docetaxel and gemcitabine using PEGylated self-assembled stealth nanoparticles for improved breast cancer therapy. Nanomedicine 14(5):1629–1641
Kushwah V, Katiyar SS, Agrawal AK, Saraf I, Singh IP, Lamprou DA, Gupta RC, Jain S (2018c) Implication of linker length on cell cytotoxicity, pharmacokinetic and toxicity profile of gemcitabine-docetaxel combinatorial dual drug conjugate. Int J Pharm 548(1):357–374
Kushwah V, Katiyar SS, Dora CP, Agrawal AK, Lamprou DA, Gupta RC, Jain S (2018d) Co-delivery of docetaxel and gemcitabine by anacardic acid modified self-assembled albumin nanoparticles for effective breast cancer management. Acta Biomater 73:424–436
Lee M, Cho YW, Park JH, Chung H, Jeong SY, Choi K, Moon DH, Kim SY, Kim I-S, Kwon IC (2006) Size control of self-assembled nanoparticles by an emulsion/solvent evaporation method. Colloid Polym Sci 284(5):506–512
Letchford K, Burt H (2007) A review of the formation and classification of amphiphilic block copolymer nanoparticulate structures: micelles, nanospheres, nanocapsules and polymersomes. Eur J Pharm Biopharm 65(3):259–269
Lince F, Marchisio DL, Barresi AA (2011) A comparative study for nanoparticle production with passive mixers via solvent-displacement: use of CFD models for optimization and design. Chem Eng Process Process Intensif 50(4):356–368
Ling Y, Wei K, Luo Y, Gao X, Zhong S (2011) Dual docetaxel/superparamagnetic iron oxide loaded nanoparticles for both targeting magnetic resonance imaging and cancer therapy. Biomaterials 32(29):7139–7150
Ling Y, Wei K, Zou F, Zhong S (2012) Temozolomide loaded PLGA-based superparamagnetic nanoparticles for magnetic resonance imaging and treatment of malignant glioma. Int J Pharm 430(1–2):266–275
Lipinski C (2002) Poor aqueous solubility—an industry wide problem in drug discovery. Am Pharm Rev 5(3):82–85
Liu W, Hu M, Liu W, Xue C, Xu H, Yang X (2008) Investigation of the carbopol gel of solid lipid nanoparticles for the transdermal iontophoretic delivery of triamcinolone acetonide acetate. Int J Pharm 364(1):135–141
Losi P, Briganti E, Errico C, Lisella A, Sanguinetti E, Chiellini F, Soldani G (2013) Fibrin-based scaffold incorporating VEGF-and bFGF-loaded nanoparticles stimulates wound healing in diabetic mice. Acta Biomater 9(8):7814–7821
Luo Y, Chen D, Ren L, Zhao X, Qin J (2006) Solid lipid nanoparticles for enhancing vinpocetine's oral bioavailability. J Control Release 114(1):53–59
Madan J, Pandey RS, Jain V, Katare OP, Chandra R, Katyal A (2013) Poly (ethylene)-glycol conjugated solid lipid nanoparticles of noscapine improve biological half-life, brain delivery and efficacy in glioblastoma cells. Nanomedicine 9(4):492–503
Mandoli C, Pagliari F, Pagliari S, Forte G, Di Nardo P, Licoccia S, Traversa E (2010) Stem cell aligned growth induced by CeO2 nanoparticles in PLGA scaffolds with improved bioactivity for regenerative medicine. Adv Funct Mater 20(10):1617–1624
Min KH, Park K, Kim Y-S, Bae SM, Lee S, Jo HG, Park R-W, Kim I-S, Jeong SY, Kim K (2008) Hydrophobically modified glycol chitosan nanoparticles-encapsulated camptothecin enhance the drug stability and tumor targeting in cancer therapy. J Control Release 127(3):208–218
Müller RH, Radtke M, Wissing SA (2002) Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv Drug Deliv Rev 54:S131–S155
Munagala R, Aqil F, Jeyabalan J, Agrawal AK, Mudd AM, Kyakulaga AH, Singh IP, Vadhanam MV, Gupta RC (2017) Exosomal formulation of anthocyanidins against multiple cancer types. Cancer Lett 393:94–102
Nahar M, Mishra D, Dubey V, Jain NK (2008) Development, characterization, and toxicity evaluation of amphotericin B–loaded gelatin nanoparticles. Nanomedicine 4(3):252–261
Naik A, Kalia YN, Guy RH, Fessi H (2004) Enhancement of topical delivery from biodegradable nanoparticles. Pharm Res 21(10):1818–1825
Nair A, Khunt D, Misra M (2019) Application of quality by design for optimization of spray drying process used in drying of risperidone nanosuspension. Powder Technol 342:156–165
Nasongkla N, Shuai X, Ai H, Weinberg BD, Pink J, Boothman DA, Gao J (2004) cRGD-functionalized polymer micelles for targeted doxorubicin delivery. Angew Chem Int Ed 43(46):6323–6327
Nii T, Ishii F (2005) Encapsulation efficiency of water-soluble and insoluble drugs in liposomes prepared by the microencapsulation vesicle method. Int J Pharm 298(1):198–205
Parra A, Mallandrich M, Clares B, Egea MA, Espina M, García ML, Calpena AC (2015) Design and elaboration of freeze-dried PLGA nanoparticles for the transcorneal permeation of carprofen: ocular anti-inflammatory applications. Colloids Surf B: Biointerfaces 136:935–943
Patel KK, Agrawal AK, Anjum MM, Tripathi M, Pandey N, Bhattacharya S, Tilak R, Singh S (2019a) DNase-I functionalization of ciprofloxacin-loaded chitosan nanoparticles overcomes the biofilm-mediated resistance of Pseudomonas aeruginosa. Appl Nanosci 10:563. https://doi.org/10.1007/s13204-019-01129-8
Patel KK, Gade S, Anjum MM, Singh SK, Maiti P, Agrawal AK, Singh S (2019b) Effect of penetration enhancers and amorphization on transdermal permeation flux of raloxifene-encapsulated solid lipid nanoparticles: an ex vivo study on human skin. Appl Nanosci 9(6):1383–1394
Patel KK, Surekha DB, Tripathi M, Anjum MM, Muthu M, Tilak R, Agrawal AK, Singh S (2019c) Antibiofilm potential of silver sulfadiazine-loaded nanoparticle formulations: a study on the effect of DNase-I on microbial biofilm and wound healing activity. Mol Pharm 16(9):3916–3925
Patel KK, Tripathi M, Pandey N, Agrawal AK, Gade S, Anjum MM, Tilak R, Singh S (2019d) Alginate lyase immobilized chitosan nanoparticles of ciprofloxacin for the improved antimicrobial activity against the biofilm associated mucoid P. aeruginosa infection in cystic fibrosis. Int J Pharm 563:30–42
Potta SG, Minemi S, Nukala RK, Peinado C, Lamprou DA, Urquhart A, Douroumis D (2010) Development of solid lipid nanoparticles for enhanced solubility of poorly soluble drugs. J Biomed Nanotechnol 6(6):634–640
Rai VK, Mishra N, Agrawal AK, Jain S, Yadav NP (2016) Novel drug delivery system: an immense hope for diabetics. Drug Deliv 23(7):2371–2390
Reverchon E (1999) Supercritical antisolvent precipitation of micro-and nano-particles. J Supercrit Fluids 15(1):1–21
Rosen J, Yoffe S, Meerasa A, Verma M, Gu F (2011) Nanotechnology and diagnostic imaging: new advances in contrast agent technology. J Nanomed Nanotechnol 2:115
Sahoo SK, Dilnawaz F, Krishnakumar S (2008) Nanotechnology in ocular drug delivery. Drug Discov Today 13(3–4):144–151
Sarmento B, Ribeiro A, Veiga F, Ferreira D, Neufeld R (2007) Oral bioavailability of insulin contained in polysaccharide nanoparticles. Biomacromolecules 8(10):3054–3060
Schäfer-Korting M, Mehnert W, Korting H-C (2007) Lipid nanoparticles for improved topical application of drugs for skin diseases. Adv Drug Deliv Rev 59(6):427–443
Sengupta P, Basu S, Soni S, Pandey A, Roy B, Oh MS, Chin KT, Paraskar AS, Sarangi S, Connor Y (2012) Cholesterol-tethered platinum II-based supramolecular nanoparticle increases antitumor efficacy and reduces nephrotoxicity. Proc Natl Acad Sci 109(28):11294–11299
Seymour L, Duncan R, Strohalm J, Kopeček J (1987) Effect of molecular weight (M w) of N-(2-hydroxypropyl) methacrylamide copolymers on body distribution and rate of excretion after subcutaneous, intraperitoneal, and intravenous administration to rats. J Biomed Mater Res 21(11):1341–1358
Shaikh J, Ankola D, Beniwal V, Singh D, Kumar MR (2009) Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur J Pharm Sci 37(3–4):223–230
Sharma N, Madan P, Lin S (2016) Effect of process and formulation variables on the preparation of parenteral paclitaxel-loaded biodegradable polymeric nanoparticles: a co-surfactant study. Asian J Pharm Sci 11(3):404–416
Shilpi D, Kushwah V, Agrawal AK, Jain S (2017) Improved stability and enhanced oral bioavailability of atorvastatin loaded stearic acid modified gelatin nanoparticles. Pharm Res 34(7):1505–1516
Shim J, Kang HS, Park W-S, Han S-H, Kim J, Chang I-S (2004) Transdermal delivery of mixnoxidil with block copolymer nanoparticles. J Control Release 97(3):477–484
Singh S, Kushwah V, Agrawal AK, Jain S (2018) Insulin-and quercetin-loaded liquid crystalline nanoparticles: implications on oral bioavailability, antidiabetic and antioxidant efficacy. Nanomedicine 13(5):521–537
Spataro G, Malecaze F, Turrin C-O, Soler V, Duhayon C, Elena P-P, Majoral J-P, Caminade A-M (2010) Designing dendrimers for ocular drug delivery. Eur J Med Chem 45(1):326–334
Sun YP, Meziani MJ, Pathak P, Qu L (2005) Polymeric nanoparticles from rapid expansion of supercritical fluid solution. Chem Eur J 11(5):1366–1373
Suthar AK, Solanki SS, Dhanwani RK (2011) Enhancement of dissolution of poorly water soluble raloxifene hydrochloride by preparing nanoparticles. J Adv Pharm Educ Res 2:189–194
Tomoda K, Terashima H, Suzuki K, Inagi T, Terada H, Makino K (2011) Enhanced transdermal delivery of indomethacin-loaded PLGA nanoparticles by iontophoresis. Colloids Surf B: Biointerfaces 88(2):706–710
Toti US, Guru BR, Hali M, McPharlin CM, Wykes SM, Panyam J, Whittum-Hudson JA (2011) Targeted delivery of antibiotics to intracellular chlamydial infections using PLGA nanoparticles. Biomaterials 32(27):6606–6613
Turk CTS, Oz UC, Serim TM, Hascicek C (2014) Formulation and optimization of nonionic surfactants emulsified nimesulide-loaded PLGA-based nanoparticles by design of experiments. AAPS PharmSciTech 15(1):161–176
Uchechi O, Ogbonna JD, Attama AA (2014) Nanoparticles for dermal and transdermal drug delivery. In: Application of nanotechnology in drug delivery. IntechOpen, London, UK
Urimi D, Agrawal AK, Kushwah V, Jain S (2019) Polyglutamic acid functionalization of chitosan nanoparticles enhances the therapeutic efficacy of insulin following oral administration. AAPS PharmSciTech 20(3):131
Vandervoort J, Ludwig A (2002) Biocompatible stabilizers in the preparation of PLGA nanoparticles: a factorial design study. Int J Pharm 238(1–2):77–92
Wang X, Chi N, Tang X (2008) Preparation of estradiol chitosan nanoparticles for improving nasal absorption and brain targeting. Eur J Pharm Biopharm 70(3):735–740
Wen H, Park K (2010) Oral controlled release formulation design and drug delivery. Theory to practice, pp 169–183, Wiley, USA
Woitiski CB, Neufeld RJ, Veiga F, Carvalho RA, Figueiredo IV (2010) Pharmacological effect of orally delivered insulin facilitated by multilayered stable nanoparticles. Eur J Pharm Sci 41(3–4):556–563
Xie J, Lee S, Chen X (2010) Nanoparticle-based theranostic agents. Adv Drug Deliv Rev 62(11):1064–1079
Yao M, McClements DJ, Xiao H (2015) Improving oral bioavailability of nutraceuticals by engineered nanoparticle-based delivery systems. Curr Opin Food Sci 2:14–19
Yoo HS, Oh JE, Lee KH, Park TG (1999) Biodegradable nanoparticles containing doxorubicin-PLGA conjugate for sustained release. Pharm Res 16(7):1114–1118
Zambaux M, Bonneaux F, Gref R, Maincent P, Dellacherie E, Alonso M, Labrude P, Vigneron C (1998) Influence of experimental parameters on the characteristics of poly (lactic acid) nanoparticles prepared by a double emulsion method. J Control Release 50(1–3):31–40
Zhang L, Gu F, Chan J, Wang A, Langer R, Farokhzad O (2008) Nanoparticles in medicine: therapeutic applications and developments. Clin Pharm Ther 83(5):761–769
Zhang C, Wan X, Zheng X, Shao X, Liu Q, Zhang Q, Qian Y (2014) Dual-functional nanoparticles targeting amyloid plaques in the brains of Alzheimer’s disease mice. Biomaterials 35(1):456–465
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Patel, K.K., Agrawal, A.K., Singh, S. (2020). Preformulation Challenges: The Concept Behind the Selection, Design and Preparation of Nanoformulations. In: Talegaonkar, S., Rai, M. (eds) Nanoformulations in Human Health. Springer, Cham. https://doi.org/10.1007/978-3-030-41858-8_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-41858-8_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-41857-1
Online ISBN: 978-3-030-41858-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)