Abstract
Immune therapeutics are revolutionizing cancer treatments. In tandem, new and confounding imaging characteristics have appeared that are distinct from those typically seen with conventional cytotoxic therapies. In fact, only 10% of patients on immunotherapy may show tumor shrinkage, typical of positive responses on conventional therapy. Conversely, those on immune therapies may initially demonstrate a delayed response, transient enlargement followed by tumor shrinkage, stable size, or the appearance of new lesions. New imaging response criteria, such as the immune-related Response Evaluation Criteria in Solid Tumors (irRECIST) and immune-related Response Criteria (irRC), are being implemented in many trials. However, FDA approval of emerging therapies, including immunotherapies, still relies on the current RECIST criteria. In this chapter, we review the traditional and new imaging response criteria for evaluation of solid tumors and briefly touch on some of the more commonly associated immunotherapy-induced adverse events.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
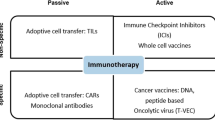
Cancer immunotherapy has caused a plethora of new and important radiographic features that are imperative to understand when assessing tumor response and immune-related adverse events [1,2,3]. Immunotherapy, which is an approach to treat cancer by augmenting or generating an immune response against cancer cells, causes radiographic responses distinct from conventional cytotoxic chemotherapies [2, 3].
Objective imaging response criteria as measured by the World Health Organization (WHO) and Response Evaluation Criteria in Solid Tumors (RECIST) criteria were originally created to assess the effects of cytotoxic chemotherapy and are dependent on tumor shrinkage and absence of new lesions; however, these criteria do not perform well in assessing the effects of drugs with other mechanisms of action, such as antiangiogenic therapies or immune therapies [1,2,3,4]. Evaluation of tumor response to cytotoxic chemotherapy depends on tumor shrinkage within a few weeks of initiating treatment. In fact, in addition to the appearance of new lesions and increased tumor size, stable disease was at one point considered a treatment failure [4]. On the other hand, new tumor therapies with recombinant cytokines, cancer vaccines, and immunomodulatory monoclonal antibodies may demonstrate a delayed response, transient enlargement (transit flair-up phase) followed by tumor shrinkage, stable size, or the appearance of new lesions [4] . Unique challenges associated with immunotherapy reflect delays in response and therapy-induced inflammation. Cancers after immunotherapy demonstrate confounding radiographic appearances with only 10% showing regression [4]. Typically, these tumors initially demonstrate a delay in response, including none or slow decrease in tumor size, increase in tumor size, and/or the appearance of new lesions, which over time become stable, decrease, or resolve without further treatment (Fig. 18.1). Over the years, there have been many modifications to the different assessment criteria by combining changes in size and inclusion of metabolic features of specific tumors to overcome the limitations of the traditional criteria [5]. However, these modifications have caused difficulties in assessing treatment efficacy since standardization of response assessments among those clinical trials lacks. It is critical to distinguish as early as possible between patients who are responding to a particular treatment and those who are not in order to maximize the effectiveness of patient care [5]. In addition, it is important to understand immunotherapy-induced side effects as in some cases treatment might be changed or halted. In this chapter, we discuss the use of a variety of traditional and new immunotherapy criteria for the evaluation of tumor response in patients who are undergoing immunotherapy. We also briefly discuss some of the immunotherapyinduced adverse events.
Conventional Imaging Response Criteria (Table 18.1)
The WHO and the RECIST criteria were the first criteria developed to assess tumor responses to traditional cancer treatment, which included cytotoxic chemotherapy, radiation therapy, or surgical resection. These criteria depend on changes in tumor size and do not take into consideration appearance of new lesions when evaluating responses that may be related to treatment [4].
WHO Criteria
In 1981, the WHO published the first tumor response criteria, thus establishing a standard assessment metric and nomenclature to evaluate treatment response [6]. The WHO criteria introduced the concept of assessing tumor burden using the sum of the products of diameters (SPD) (i.e., longest overall tumor diameter and longest diameter perpendicular to the longest overall diameter) and determining response to therapy by evaluating the changes from baseline during treatment [6]. These criteria were categorized into four tumor response groups: complete response (tumor not detected for at least 4 weeks), partial response (≥50% reduction in the SPD from baseline, also confirmed at 4 weeks), progressive disease (≥25% increase in tumor size in one or more lesions), and no change (stable) in disease (neither partial response, complete response, nor progressive disease) (Table 18.1) [7] . However, the WHO has a few major pitfalls (discussed below), in particular, because tumor measurements are based on SPD, small increases in tumor size may result in a sufficiently overall increase in tumor size (≥25% increase) to consider it as progressive disease [5].
RECIST 1.0, 1.1, and mRECIST Criteria
RECIST 1.0
In 2000, the RECIST 1.0 criteria was established and addressed some of the pitfalls of the WHO criteria. Of these, the key features of RECIST 1.0 included a clear definition of measurable disease, number of lesions to be assessed, and the use of unidimensional (i.e., longest dimension) rather than bidimensional tumor measurements (Table 18.1) [6].
RECIST 1.1
In 2009, RECIST 1.1 was developed. RECIST 1.1 addressed multiple questions regarding the assessment of lymph nodes, number of lesions to be assessed, and use of new imaging modalities, such as multidetector computed tomography (MDCT) and magnetic resonance imaging (MRI) [8]. In RECIST 1.1, the number of target lesions is reduced; target lesions can reach a maximum of five lesions (up to two lesions in any one organ) and must be measured in their longest dimension (should be at least 10 mm in the longest diameter to be considered measurable), except for lymph nodes, which use the shortest diameter (must be at least 15 mm in the short axis to be considered pathological). In coalescing lesions (nonnodal lesions), its portions should be added together (as lesions coalesce) and its longest dimensions measured [8]. Furthermore, if a lesion cannot be reliably measured, the next largest lesion that can be reproducibly measured should be selected. In addition, if any target lesions (including lymph nodes) become too small to be measured, these should also be recorded and taken in assessment of response and reassessed in the follow-up examination to determine if they represent a new lesion [5] (Table 18.1).
Modified RECIST (mRECIST)
Modified RECIST (mRECIST) was created to measure the response rate in hepatocellular carcinoma (HCC). Similar to RECIST 1.0 and 1.1, mRECIST uses tumor size as an index of tumor response; however, in contrast, mRECIST takes into account treatment-induced tumor necrosis, and changes in size are determined by assessing for viable tumor, referred to an uptake of contrast agent in the arterial phase on CT or MRI [9, 10]. For example, a complete tumor response is defined as the disappearance of arterial phase enhancement in all target lesions which should be classified as a measurable lesion according to the RECIST criteria [5]. Tumors in malignant portal vein thrombosis are considered as nonmeasurable disease since the bland thrombus formed during the course of treatment can obscure the tumor.
Choi Response Criteria
The Choi criteria was initially proposed for assessment of gastrointestinal stromal tumors (GIST) on imatinib, a tyrosine kinase receptor inhibitor. This study found that GISTs on treatment may initially increase in size due to internal hemorrhage, necrosis, or myxoid degeneration. Some may show a minimal decrease in tumor size but not sufficient enough to be classified as having a positive response to therapy according to RECIST criteria [11]. The Choi criteria focuses on changes in density (Hounsfield units on CT) rather than tumor shrinkage to assess response. A decrease in tumor density on CT is often seen in these tumors responding to imatinib and is related to tumor necrosis or myxoid degeneration. There are two main limitations of the Choi criteria: it cannot be applied to MRI and there is lack of sufficient validation in other tumors.
EORTC
The European Organization for Research and Treatment of Cancer (EORTC) criteria has formalized the concept of assessing tumor response via quantifying the changes in fluorodeoxyglucose (FDG) uptake. Criteria standardization and rules were proposed on patient preparation, timing of [18F]-FDG positron emission tomography (PET) scans, attenuation correction and dose of [18F]-FDG, methods to measure [18F]-FDG uptake, tumor sampling, reproducibility, and definition of [18F]-FDG tumor response [12, 13].
The criteria follows the model of RECIST in terms of defining four response categories with similar names as RECIST. Complete metabolic response (CMR) would be the complete resolution of [18F]-FDG uptake within the tumor volume so that it is indistinguishable from surrounding normal tissue. Partial metabolic response (PMR) would be classified as a reduction of a minimum of 15–25% in tumor [18F]-FDG SUV after one cycle of chemotherapy, and greater than 25% after more than one treatment cycle. Stable metabolic disease (SMD) would be classified as an increase in tumor [18F]-FDG SUV of less than 25% or a decrease of less than 15% and no visible increase in extent of [18F]-FDG tumor uptake (20% in the longest dimension). Progressive metabolic disease (PMD) would be classified as an increase in [18F]-FDG tumor SUV of greater than 25% within the tumor region defined on the baseline scan, visible increase in the extent of [18F]-FDG tumor uptake (20% in the longest dimension) or the appearance of new [18F]-FDG uptake in metastatic lesions [12, 13].
PERCIST Criteria
Based on the premise that newer cancer therapies are more cytostatic than cytocidal, tumor response can manifest with a decrease in metabolism without a notable tumor size reduction [14]. In 2009, the PET response criteria for solid tumors (PERCIST) was proposed and is based mainly on FDG uptake to evaluate tumor response [15]. PERCIST focuses on the percentage of change in metabolic activity from baseline and the number of weeks from initiation therapy. The standardized uptake value (SUV) corrected for lean body mass (SUL) is used for the assessment of tumor response. The SUL peak is measured within a spherical region of interest of 1.2 cm in diameter (or 1 cm3 for volume) within the area of highest uptake in the tumor [5]. PERCIST defines four metabolic response categories. In brief, according to these criteria, complete response means disappearance of all metabolically active tumors while partial metabolic response is defined as a 0.8-unit (>30%) decline in SUL peak between the most intense lesion before treatment and the most intense lesion after treatment. Of note, the lesion at follow-up may be a different lesion than previously measured since the most active lesion needs to be followed. Progressive disease is defined as an increase (>30%) in SUL peak or the appearance of a new metabolically active lesion [5]. It is likely that PERCIST will replace the EORTC criteria in the same way that RECIST has replaced the WHO criteria [12].
RANO Criteria
The Revised Assessment in Neuro-Oncology (RANO) criteria was proposed to overcome the significant limitations in the Macdonald criteria for response assessment in high-grade gliomas. The Macdonald criteria didn’t take into account, for example, pseudoprogression, pseudoresponse observed with antiangiogenic agents, and the inability to capture recurrence in the nonenhancing component of the lesion, due to using only the contrast-enhancing component of the tumor in it [13].
Similar to the Macdonald criteria, the RANO criteria uses two-dimensional tumor measurements; however, the RANO criteria also accounts for changes in the nonenhancing T2/FLAIR signal abnormality. Measurable disease is defined as two perpendicular diameters of at least 10 mm (visible on two or more axial slices being preferably not more than 5 mm apart with 0 mm skip) and allows selection of a total of five target lesions (Fig. 18.2). RANO criteria addressed pseudoprogression and pseudoresponse. The RANO criteria for high-grade glioma are summarized in Table 18.2 [16, 17].
Algorithm for identifying measurable and target lesions [16]
In RANO, the postradiation examination as the baseline for response assessment instead of the postsurgical MRI scan can be used. Progressive disease is defined by at least two sequential scans separated by at least 4 weeks, both showing >25% increase in the sum of products of perpendicular diameters or > 40% increase in total volume of enhancing lesions. If the follow-up scan exhibits SD or PR/CR, then the first scan that showed “preliminary PD” is noted at pseudoprogression. Pseudoprogression is also considered if imaging showed PD and the follow-up scan >4 weeks apart showed SD, CR, PR or the lesions became nonmeasurable; if the latter, the scan that showed “preliminary PD” is noted as “pseudoprogression” [16]. On the other hand, if imaging demonstrated preliminary PR/CR and the follow-up scans exhibited PD with respect to the “preliminary CR/PR” scan, then the response isn’t sustained and is noted as pseudoresponse. Pseudoresponse can also be noted in tumors that show regression in size of their enhancing component whilst their nonenhancing component show progression [16].
RANO-BM
The Response Assessment in Neuro-Oncology Brain Metastases working group initially convened in 2011 and proposed response assessment on the basis of literature review and consensus opinion [18]. RANO-BM adopted features from RECIST and RANO-HGG to be able to meet the specific needs of patients with brain metastases, where response assessment in RANO-BM is being based on the sum diameter of one-dimensional measurements, corticosteroid dosing and clinical status (Table 18.3) [17].
Cheson Response Criteria for Malignant Lymphomas
Tumor assessment criteria have been developed specifically for lymphoma. In lymphoma, masses often don’t regress in size completely after therapy because of the presence of residual fibrosis and necrotic debris; thus, reporting whether the tumor is viable or not viable does not depend solely on the stability of the tumor’s size. The Cheson response criteria analyzes the size and the metabolic activity of the tumor during the course of treatment. The revised version of the Cheson criteria in 2007 replaced gallium scintigraphy with PET and included the evaluation of flow cytometry and immunohistochemistry as mentioned in Tirkes et al. (Table 18.4) [5].
Immunotherapy Imaging Response Criteria
Evaluating tumor responses during immune therapy in solid cancers remains a challenge [5, 20]. The mechanism of action in immunotherapy differs substantially from cytotoxic agents; thus a well-tailored set of criteria to capture accurate and exact response to this new line of therapeutic agents is needed [4, 5, 20]. To this end, Wolchok et al. presented a set of criteria to evaluate immune-related responses, adopting a bidimensional approach similar to the WHO criteria and measuring a maximum number of five lesions per organ (Table 18.5) [4]. Although these criteria were widely accepted, it still harbors some challenges. For instance, assessing a relatively large number of lesions per organ could be relatively time-consuming in cases of extreme tumor burdens [2, 21]. Furthermore, evaluation of excessive number of lesions impacts the reproducibility of the results [2, 21]. As such, Nishino et al. proposed a modification to the immune-related response criteria (irRC) in the light of RECIST 1.1 guidelines [2, 8, 21]. With regard to brain tumors, the Immunotherapy Response Assessment in Neuro-Oncology (iRANO) criteria is a set to tumor metrics to assess brain tumors in patients undergoing immune therapies.
Immune-Related Response Criteria
Arising from the heightened awareness by national and international communities as to the unique radiographic response patterns seen with vaccines and immunotherapeutics, modifications were made to the WHO and RECIST criteria in 2004 and 2005. In 2009, the immune-related Response Criteria (irRC) was published by Wolchok et al., based on the observed patterns in treatment response from phase II clinical trials in advanced melanoma patients who were receiving ipilimumab, a human monoclonal antibody that blocks cytotoxic T lymphocyte antigen–4 (CTLA-4). In this study [4], four patterns of treatment responses were recognized: (1) a decrease in the size of the lesion and without new tumors, similar to what is seen after conventional cytotoxic therapy; (2) stable disease after completion of treatment; (3) a delay in tumor response to therapy after an initial increase in total tumor burden; (4) the appearance of new lesions that precede tumor shrinkage.
In contrast to the WHO and RECIST criteria, irRC takes into account both the index and new measurable lesions to assess the “total tumor burden,” a new concept from prior criteria, and compare to the baseline scan [4]. The irRC was derived from the WHO criteria and, therefore, the thresholds of response remain the similar. However, the irRC response categories have been modified from those of the WHO criteria [4]. According to the irRC, the sum of the products of the two largest perpendicular diameters (SPD) of all index lesions (five lesions per organ, up to 10 visceral lesions and five cutaneous index lesions) is calculated at the baseline. At every time point, the index lesions and any new measurable lesions are added together to accurately measure the total tumor burden (TTB) [(TTB = SPDindex lesions + SPDnew, measurable lesions)]. This is a major difference from the WHO criteria, which considers all new measurable lesions as progressive disease [5]. Further, a confirmatory examination at least 4 weeks from the initial scan documenting progression is required by the irRC prior to declaring progressive disease, as there can be a delay in response in patients on immunotherapy. In addition, decreases in tumor burden must be assessed relative to baseline measurements (i.e., the SPD of all index lesions at screening). The overall response according to the irRC is derived from time-point response assessments based on tumor burden, as described in Table 18.5.
The irRC does not mention the use of specific imaging modalities in the assessment of tumor response, although CT and MRI are typically used. However, research on novel PET radiotracers that incorporate amino acids, nucleotides, choline, and s-receptor to detect cell proliferation or cell death is being carried out [22]. Further, immune-related adverse effect can be sometimes identified with FDG-PET/CT and metabolic changes can be noted before the clinical symptoms to allow early change of the immunotherapy [1].
Immune-Related RECIST Criteria
The newly proposed irRECIST (Table 18.6) and adopted irRC [4] set thresholds for determining different possible responses, including complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD) [2, 21]. Nishino et al. demonstrated that such changes did not result in any statistically significant variation of the response evaluation in melanoma patients receiving immunotherapy [2, 21]. They also demonstrated that irRECIST measurements were relatively more reproducible than the more involved bidimensional irRC measurements [2, 21]. In 2017, the RECIST working group published the immune-RECIST (iRECIST) based on RECIST 1.1, where the definition of pseudoprogression was introduced. It is noteworthy, iRECIST criteria was used for response assessment to immunotherapy in trials for patients with brain metastases, by discerning between intra- and extracranial responses [24]. The criteria are summarized in Table 18.7 [25].
Immunotherapy Response Assessment for Neuro-oncology Criteria
The iRANO criteria is used to assess brain lesions in patients undergoing immunotherapy [3]. In order that misclassification of patients with stable or increasing tumor size and new lesions as progressive disease does not occur when the therapy is actually effective and the patient is receiving clinical benefit, the iRANO criteria was published. In brief, the iRANO follow the same guidelines as the RANO criteria. However, in those cases of appearance of disease in the absence of clinical deterioration within 6 months of immunotherapy, continuation of immunotherapy and repeat assessment in 3 months is recommended (Table 18.8). As with all current imaging assessment criteria, the iRANO guidelines will require future amendments, including the possible incorporation of volumetrics, advanced imaging sequences, and other types of imaging analytics. A recent study by our group demonstrated that radiomics can discriminate between patients who have pseudoprogression versus true tumor progression with high sensitivity (97%), specificity (79%), and accuracy (95%) in patients with glioblastoma [26]. The iRANO criteria also added specific guidance for the determination of progressive disease in patients with brain metastases undergoing immunotherapy. The criteria for iRANO-BM is summarized in Table 18.9 [3].
It’s crucial for clinicians to indicate and conclude an underlying tumor progression during the course of immunotherapy. It has been shown that early radiographic progression in patients who ultimately derive clinical benefit actually stabilize or even improve within 3 months. The iRANO working group has come up with an algorithm to guide assessment of progressive disease in neuro-oncology patients undergoing immunotherapy to decrease the likelihood of prematurely stating progressive disease in patients with PsP or delayed response (Fig. 18.3) [3].
iRANO treatment algorithm for the assessment of progressive imaging findings in neuro-oncological malignancies [3]
Future Directions for Immune Therapy Imaging Assessment
Although irRECIST and irRC represent an improvement over the conventional WHO criteria and RECIST to evaluate tumor response in immunotherapy, there remains limitations and challenges and further refinements are warranted [4]. Plans for improving imaging response criteria include volumetric (3D) imaging, dynamic contrast imaging, and functional (molecular) imaging. Radiomics is a more recent developing field within imaging that can help in more precise tumor assessments that are unrelated to tumor size or burden. Radiomics has the potential to be a noninvasive digital biopsy technique that is spatially guided and that can quantify T-cell infiltration of tumors and reflect the entire tumor burden by providing information on each cancer lesion, in contrast to the traditional biopsy that represents only a sample of the tumor. Quantitative imaging biomarkers can support personalized design of immunotherapy interventions and longitudinally monitor and assess immune checkpoint blockade response [27, 28]. Radiomics can be the key to help discriminate between pseudoprogression and true progression, which are significantly difficult to differentiate radiographically. Multiple studies conducted by our group demonstrated 5 texture features were able to robustly predict whether a GBM patient had pseudoprogression or true progression [29,30,31,32]. Roger Sun et al. reported on an eight-feature radiomics-based signature of CD8 cell expression, which they developed by use of CT images. The radiomics signature was also shown to be associated with clinical outcomes in patients treated with anti-PD-1 or anti-PD-L1 immunotherapy in an independent cohort [28]. Further, radiogenomics, the linkage between imaging phenotypes and tumor genomics, might help develop more robust stratification and end-point imaging biomarkers for immunotherapy and molecular targeted clinical trials.
Imaging in Immune-Related Adverse Events
Immune-related adverse events (irAE) can represent a serious complication and can be challenging for any imager. Thus, it is important to be aware and take into consideration the possibility of its occurrence so that early management is undertaken [33]. Treatment of adverse events is typically based on published guidelines and includes delaying treatment dosing, administering corticosteroids, or terminating therapy depending on the severity of the event. However, success in outcome lies heavily on correctly identifying and interpreting these complications.
Severe colitis has the highest mortality and worst outcome associated with irAE [33]. Because of the possibility of misdiagnosis of autoimmune colitis, the patient can take antibiotic therapy instead of corticosteroid therapy, which can result in a delayed diagnosis and complication by colonic bowel perforation [33]. Other common immune adverse events are sarcoid-like adenopathy and pancreatitis. It is important to recognize and accurately diagnose these events in order to avoid misdiagnosis for metastatic disease [1]. There are also many other events which can occur as a result of immunotherapy, for example, autoimmune hepatitis, pneumonitis, thyroiditis, myocarditis, pericarditis, temporal arteritis, conjunctivitis, sarcoid-like reaction such as lymphocytic vasculitis, organizing pneumonia, and fasciitis [34, 35]. Autoimmune hepatitis may be seen as periportal edema and hypoattenuation of the edematous liver parenchyma in CT. However, these finding are not specific to autoimmune hepatitis and can be seen in the setting of cancer immunotherapy [1].
Immunotherapy-induced pneumonitis is an uncommon yet potentially fatal irAE that requires clinical suspicion and early detection. A recent study by our group demonstrated that specific radiomic imaging features (extracted from baseline CT scans) were able to predict those patients that will subsequently develop pneumonitis prior to the initiation of immune therapy (Fig. 18.4). This study highlights the ability of imaging to identify those patients that might be most susceptible to irAE before the irAE even occurs [36].
(a) An illustration of the outlined regions of interest (ROIs) in the lungs. An ROI containing three consecutive slices, taken in each lobe in the right lung and ROIs outlined in the left lung correspond to the same level as the right lung ROIs. Postcontrast lung CT images depicting the segmented ROIs in upper (b), middle (c), and lower, (d) sections of the right and left lungs. Each ROI is outlined with a different label. Contrast-enhancing vessels from the ROIs were subtracted. Radius of the ROI ranged between 14 and 15 mm
References
Kwak JJ, Tirumani SH, Van den Abbeele AD, Koo PJ, Jacene HA. Cancer immunotherapy: imaging assessment of novel treatment response patterns and immune-related adverse events. Radiographics. 2015;35(2):424–37.
Nishino M, Tirumani SH, Ramaiya NH, Hodi FS. Cancer immunotherapy and immune-related response assessment: the role of radiologists in the new arena of cancer treatment. Eur J Radiol. 2015;84(7):1259–68.
Okada H, Weller M, Huang R, Finocchiaro G, Gilbert MR, Wick W, et al. Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol. 2015;16(15):e534–e42.
Wolchok JD, Hoos A, Day S, Weber JS, Hamid O, Lebbé C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15(23):7412.
Tirkes T, Hollar MA, Tann M, Kohli MD, Akisik F, Sandrasegaran K. Response criteria in oncologic imaging: review of traditional and new criteria. Radiographics. 2013;33(5):1323–41.
Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981;47:207.
Organization. W.H. WHO handbook for reporting results of cancer treatment: offset publication no. 481979.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol. 2001;35(3):421–30.
for the Panel of Experts in HCCDCT, Di Bisceglie AM, Zhu AX, Kramer BS, Gores GJ, Talwalkar J, et al. Design and endpoints of clinical trials in hepatocellular carcinoma. J Nat Cancer Inst. 2008;100(10):698–711.
Van den Abbeele AD, Badawi RD. Use of positron emission tomography in oncology and its potential role to assess response to imatinib mesylate therapy in gastrointestinal stromal tumors (GISTs). Eur J Cancer. 2002;38:S60–S5.
Pinker K, Riedl C, Weber WA. Evaluating tumor response with FDG PET: updates on PERCIST, comparison with EORTC criteria and clues to future developments. Eur J Nucl Med Mol Imaging. 2017;44(1):55–66.
Subbiah V, Chuang HH, Kairemo K, Gambhire D. Defining clinical response criteria and early response criteria for precision oncology: current state-of-the-art and future perspectives. Diagnostics (2075–4418). 2017;7(1):10.
Vossen JA, Buijs M, Kamel IR. Assessment of tumor response on MR imaging after locoregional therapy. Tech Vasc Interv Radiol. 2006;9(3):125–32.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S.
Ellingson BM, Wen PY, Cloughesy TF. Modified criteria for radiographic response assessment in glioblastoma clinical trials. Neurotherapeutics: J Am Soc Exp NeuroTherap. 2017;14(2):307–20.
Wen PY, Chang S, Van den Bent MJ, Vogelbaum MA, Macdonald DR, Lee EQ. Response assessment in neuro-oncology clinical trials. J Clin Oncol. 2017;35:2439.
Alexander BM, Brown PD, Ahluwalia MS, Aoyama H, Baumert BG, Chang SM, et al. Clinical trial design for local therapies for brain metastases: a guideline by the response assessment in neuro-oncology brain metastases working group. Lancet Oncol. 2018;19(1):e33–42.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25(5):579–86.
Ribas A, Chmielowski B, Glaspy JA. Do we need a different set of response assessment criteria for tumor immunotherapy? Clin Cancer Res. 2009;15(23):7116.
Nishino M, Gargano M, Suda M, Ramaiya NH, Hodi FS. Optimizing immune-related tumor response assessment: does reducing the number of lesions impact response assessment in melanoma patients treated with ipilimumab? J Immunother Cancer. 2014;2(1):17.
Aarntzen EHJG, Srinivas M, Radu CG, Punt CJA, Boerman OC, Figdor CG, et al. In vivo imaging of therapy-induced anti-cancer immune responses in humans. Cell Mol Life Sci. 2013;70(13):2237–57.
Somarouthu B, Lee SI, Urban T, Sadow CA, Harris GJ, Kambadakone A. Immune-related tumour response assessment criteria: a comprehensive review. Br J Radiol. 2018;91(1084):20170457.
Porcu M, Solinas C, Garofalo P, de Azambuja E, Scartozzi M, Willard-Gallo K, et al. Radiological evaluation of response to immunotherapy in brain tumors: where are we now and where are we going? Crit Rev Oncol Hematol. 2018;126:135–44.
Seymour L, Bogaerts J, Perrone A, Ford R, Schwartz LH, Mandrekar S, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18(3):e143–e52.
Srishti Abrol GT HA, Kotrotsou A, Alfaro-Munoz KD, de Groot JF, Zinn P, Colen RR. Radiomics differentiate between true progression and pseudo-progression in GBM patients: annual meeting of the American society of neuroradiology—ASNR. 2016.
Lambregts DMJ, Lalezari F, Kurilova I, RGH B-T, Trebeschi S, HJWL A, et al. Predicting response to cancer immunotherapy using non-invasive radiomic biomarkers. Ann Oncol. 2019;30(6):998.
El Naqa I, Ten Haken RK. Can radiomics personalise immunotherapy? Lancet Oncol. 2018;19(9):1138–9.
Abrol S, Kotrotsou A, Hassan A, Elshafeey N, Hassan I, Idris T, et al. Radiomic analysis of pseudo-progression compared to true progression in glioblastoma patients: a large-scale multi-institutional study. J Clin Oncol. 2017;35(15_suppl):2015.
Elshafeey N, Kotrotsou A, Giniebra Camejo D, Abrol S, Hassan I, El Salek K, et al. Multicenter study to demonstrate radiomic texture features derived from MR perfusion images of pseudoprogression compared to true progression in glioblastoma patients. J Clin Oncol. 2017;35(15_suppl):2016.
Abrol S, Kotrotsou A, Hassan A, Elshafeey N, Idris T, Manohar N, et al. Abstract 3040: radiomics discriminates pseudo-progression from true progression in glioblastoma patients: a large-scale multi-institutional study. Cancer Res. 2018;78(13 Supplement):3040.
Elakkad A, Hassan A, Kotrotsou A, Kumar AM, McDonald C, Kogias E, et al. 213 radiomic machine learning algorithms discriminate pseudo-progression from true progression in glioblastoma patients: a multi-institutional study. Neurosurgery. 2018;65(CN_suppl_1):119–20.
Weber JS, Dummer R, de Pril V, Lebbé C, Hodi FS, for the MDXI. Patterns of onset and resolution of immune-related adverse events of special interest with ipilimumab. Cancer. 2013;119(9):1675–82.
Barjaktarevic IZ, Qadir N, Suri A, Santamauro JT, Stover D. Organizing pneumonia as a side effect of ipilimumab treatment of melanoma. Chest. 2013;143(3):858–61.
Bronstein Y, Ng CS, Hwu P, Hwu W-J. Radiologic manifestations of immune-related adverse events in patients with metastatic melanoma undergoing anti–CTLA-4 antibody therapy. Am J Roentgenol. 2011;197(6):W992–W1000.
Colen RR, Fujii T, Bilen MA, Kotrotsou A, Abrol S, Hess KR, et al. Radiomics to predict immunotherapy-induced pneumonitis: proof of concept. Investig New Drugs. 2018;36(4):601–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ayoub, M., Eleneen, Y., Colen, R.R. (2020). Cancer Imaging in Immunotherapy. In: Naing, A., Hajjar, J. (eds) Immunotherapy. Advances in Experimental Medicine and Biology, vol 1244. Springer, Cham. https://doi.org/10.1007/978-3-030-41008-7_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-41008-7_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-41007-0
Online ISBN: 978-3-030-41008-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)