Abstract
Hyperventilation is an effective and fast way to reduce increased intracranial pressure (ICP). However, hyperventilation reduces ICP by causing cerebral vasoconstriction and a subsequent reduction in cerebral blood flow (CBF), which can lead to cerebral ischaemia. Prophylactic hyperventilation is therefore not recommended. Hyperventilation should be avoided during the first 24 h after injury when CBF often is critically reduced. Hyperventilation is recommended as a temporary tool to reduce ICP until other measures can be effective.
If hyperventilation is used, it is recommended to monitor brain oxygen delivery by either SjO2 and PtiO2 measurements or other means of continuous brain oxygen monitoring.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara RecommendationsLevel I
There are insufficient data to support a Level I recommendation for this topic.
Level II
Prophylactic hyperventilation should be avoided.
Level III
Hyperventilation is recommended as a temporising measure for the reduction of ICP.
Hyperventilation should be avoided during the first 24 h after injury when CBF often is critically reduced. If hyperventilation is still used, it is recommended to monitor brain oxygen delivery by SjO2 or PtiO2 measurements or other means of continuous brain oxygen monitoring.
1 Overview
Aggressive hyperventilation (arterial PaCO2 ≤ 3.3 kPa) has been a cornerstone in the management of severe traumatic brain injury (TBI) for more than 20 years because it can cause a rapid reduction in ICP. Brain swelling and elevated ICP develop in 40% of patients with severe TBI (Miller et al. 1977), and high or uncontrolled ICP is one of the most common causes of death and neurologic disability after TBI (Becker et al. 1977). Therefore, the assumption has been made that hyperventilation benefits all patients with severe TBI. In a 1995 survey, Ghajar et al. found that hyperventilation was being used by 83% of US trauma centres (Ghajar et al. 1995). This number has declined over the years, but as recent as 2008, the BrainIT group made a survey in European centres showing that early prophylactic hyperventilation was used in more than 50% of cases (Neumann et al. 2008). However, hyperventilation reduces ICP by causing cerebral vasoconstriction and a subsequent reduction in CBF and cerebral blood volume and not by reducing brain oedema (Raichle and Plum 1972). Research conducted over the past 20 years clearly demonstrate that CBF during the first day after injury is less than half that of normal individuals (Bouma et al. 1992; Muizelaar et al. 1989; Robertson et al. 1988) and that there is a risk of causing or worsening cerebral ischaemia with aggressive hyperventilation, especially in the already ischaemic penumbra zone. Histologic evidence of cerebral ischaemia has been found in most victims of severe TBI who died (Graham and Adams 1971; Ross et al. 1993). A randomised study found significantly poorer outcomes at 3 and 6 months when prophylactic hyperventilation was used, as compared to when it was not (Muizelaar et al. 1991). Thus, limiting the use of hyperventilation following severe TBI may help to improve neurologic recovery following injury or at least avoid iatrogenic cerebral ischaemia.
Tips, Tricks and Pitfalls
-
If the ICP is stable and below 20 mmHg, keep the PaCO2 above 4.5 kPa.
-
If the patient is monitored with ETCO2 and the pulmonary condition is stable, compare ETCO2 with PaCO2 on a regular basis (once or twice a day). This will diminish the need for arterial blood gas monitoring since the difference between PaCO2 and ETCO2 will, for all good measures, be approximately the same if the pulmonary condition is stable.
-
If the ventilator is on pressure control and you want to decrease PaCO2, increase the frequency of ventilations rather than the tidal volume because this will not alter the difference between ETCO2 and PaCO2.
-
If the ventilator is on volume control and you increase the minute volume, keep an eye on the tidal volume to decrease the risk of overextension of the lungs.
-
It is easier to keep adequate ventilation volume if the ventilator setting is on volume control.
2 Background
2.1 CBF Following TBI
Three studies provide Class III evidence that CBF can be dangerously low soon after severe TBI (Bouma et al. 1992; Marion et al. 1991; Sioutos et al. 1995). Two CBF measurements were performed with xenon-CT/CBF method during the first 5 days following severe TBI in a total of 67 patients. CBF measurements were obtained during the first 24 h after injury in one study, and they were less than 18 mL/100 g/min in 31.4% of patients (Bouma et al. 1992). In the second study, the mean CBF during the first few hours after injury was 27 mL/100 g/min (Marion et al. 1991). The third study measured CBF with a thermodiffusion blood flow probe, again during the first 5 days post-injury, in 37 severe TBI patients (Sioutos et al. 1995). Twelve patients had a global CBF less than 18 mL/100 g/min up to 48 h post-injury.
2.2 PaCO2/CBF Reactivity and Cerebral Oxygen Utilisation
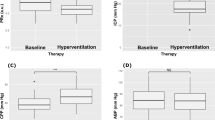
Three Class III studies provide the evidence base for this topic (Imberti et al. 2002; Oertel et al. 2002 and Sheinberg et al. 1992). Results associating hyperventilation with SjO2 and PtiO2 values in a total of 102 patients are equivocal. One study showed no consistent positive or negative change in SjO2 or PtiO2 values (Imberti et al. 2002). A second study associated hyperventilation with a reduction of PaCO2 and subsequent decrease in SjO2 from 73% to 67%, but the SjO2 values never dropped below 55% (Oertel et al. 2002). The third study reported hyperventilation to be the second most common identifiable cause of jugular venous oxygen desaturation in a sample of 33 patients (Sheinberg et al. 1992). Studies on regional CBF showed significant variation in reduction in CBF following TBI. Two studies indicated lowest flows in brain tissue surrounding contusions or underlying subdural haematomas and in patients with severe diffuse injuries (Marion et al. 1991; Salvant and Muizelaar 1993). Similarly, a third study found that CO2 vasoreactivity was most abnormal in contusions and subdural haematomas (McLaughlin and Marion 1996). Considering that CO2 vasoreactivity could range from almost absent to three times normal in these patients, there could be a dangerous reduction in CBF during hyperventilation, especially in areas surrounding contusions or underlying subdural clots. Only one of these three studies (Marion et al. 1991) had adequate design and sample to be included as evidence. Two studies associated hyperventilation-induced reduction in CBF with a significant increase in oxygen extraction fraction, but they did not find a significant relationship between hyperventilation and change in the CMRO2 (Diringer et al. 2002; Hutchinson et al. 2002).
2.3 Effect of Hyperventilation on Outcome
One Class III study involving 890 patients intubated prehospitally showed adverse outcome for both hypo- and hypercapnic patients; intubated patients arriving at the trauma centre with an PaCO2 between 4.0 and 6.5 kPa had a better survival than those who had been hypo- or hyperventilated, after adjustment for confounding factors (adjusted OR 2.17) (Davis et al. 2006).
One Class II RCT of 113 patients used a stratified, randomised design to compare outcomes of severe TBI patients provided normal ventilation (PaCO2 4.66 ± 0.25 kPa; n = 41; control group), hyperventilation (PaCO2 3.33 + 0.25 kPa; n = 36) or hyperventilation with tromethamine (n = 36) (Muizelaar et al. 1991). One benefit of hyperventilation is the minimisation of cerebrospinal fluid (CSF) acidosis. However, the effect on CSF pH may not be sustained due to a loss of HCO−3 buffer. Tromethamine (THAM) buffer treatment was introduced to test the hypothesis that it could reverse the effects of the loss of buffer. Patients were stratified based on the motor component of the Glasgow Coma Scale (GCS) score (1–3 vs 4–5). The Glasgow Outcome Scale (GOS) score was used to assess patient outcomes at 3, 6 and 12 months. For patients with a motor GCS of 4–5, the 3- and 6-month GOS scores were significantly lower in the hyperventilated patients than in the control or THAM groups. However, the effect was not sustained at 12 months. The recommendation today is that hyperventilation should be avoided.
3 Specific Paediatric Concerns
There are no specific paediatric concerns; children should be treated in accordance with the adult guidelines.
References
Becker DP, Miller JD, Ward JD, Greenberg RP, Young HF, Sakalas R. The outcome from severe head injury with early diagnosis and intensive management. J Neurosurg. 1977;47:491–502.
Bouma GJ, Muizelaar JP, Stringer WA, Choi SC, Fatouros P, Young HF. Ultra-early evaluation of regional cerebral blood flow in severely head-injured patients using xenon-enhanced computerized tomography. J Neurosurg. 1992;77:360–8.
Davis DP, Idris AH, Sise MJ, Kennedy F, Eastman AB, Velky T, Vilke GM, Hoyt DB. Early ventilation and outcome in patients with moderate to severe traumatic brain injury. Crit Care Med. 2006;34:1202–8.
Diringer MN, Videen TO, Yundt K, Zazulia AR, Aiyagari V, Dacey RG Jr, Grubb RL, Powers WJ. Regional cerebrovascular and metabolic effects of hyperventilation after severe traumatic brain injury. J Neurosurg. 2002;96:103–8.
Ghajar J, Hariri RJ, Narayan RK, Iacono LA, Firlik K, Patterson RH. Survey of critical care management of comatose, head-injured patients in the United States. Crit Care Med. 1995;23:560–7.
Graham DI, Adams JH. Ischaemic brain damage in fatal head injuries. Lancet. 1971;1:265–6.
Hutchinson PJ, Gupta AK, Fryer TF, al-Rawi PG, Chatfield DA, Coles JP, OConnell MT, Kett-White R, Minhas PS, Aigbirhio FI, Clark JC, Kirkpatrick PJ, Menon DK, Pickard JD. Correlation between cerebral blood flow, substrate delivery, and metabolism in head injury: a combined microdialysis and triple oxygen positron emission tomography study. J Cereb Blood Flow Metab. 2002;22:735–45.
Imberti R, Bellinzona G, Langer M. Cerebral tissue PO2 and SjvO2 changes during moderate hyperventilation in patients with severe traumatic brain injury. J Neurosurg. 2002;96:97–102.
Marion DW, Darby J, Yonas H. Acute regional cerebral blood flow changes caused by severe head injuries. J Neurosurg. 1991;74:407–14.
McLaughlin MR, Marion DW. Cerebral blood flow and vasoresponsivity within and around cerebral contusions. J Neurosurg. 1996;85:871–6.
Miller JD, Becker DP, Ward JD, Sullivan HG, Adams WE, Rosner MJ. Significance of intracranial hypertension in severe head injury. J Neurosurg. 1977;47:503–10.
Muizelaar JP, Marmarou A, DeSalles AA, Ward JD, Zimmerman RS, Li Z, Choi SC, Young HF. Cerebral blood flow and metabolism in severely head-injured children. Part 1: relationship with GCS score, outcome, ICP, and PVI. J Neurosurg. 1989;71:63–71.
Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruermer H, Young HF. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731–9.
Neumann JO, Chambers IR, Citerio G, Enblad P, Gregson BA, Howells T, Mattern J, Nilsson P, Piper I, Ragauskas A, Dahuquillo J, Yau YH, Kiening K, BrainT Group. The use of hyperventilation therapy after traumatic brain injury in Europe: an analysis of the BrainIT Group. Intensive Care Med. 2008;34:1676–82.
Oertel M, Kelly DF, Lee JH, McArthur DL, Glenn TC, Vespa P, Boscardin WJ, Hovda DA, Martin NA. Efficacy of hyperventilation, blood pressure elevation, and metabolic suppression therapy in controlling intracranial pressure after head injury. J Neurosurg. 2002;97:1045–53.
Raichle ME, Plum F. Hyperventilation and cerebral blood flow. Stroke. 1972;3:566–75.
Robertson CS, Clifton GL, Grossman RG, Ou CN, Goodman JC, Borum P, Bejot S, Barrodale P. Alterations in cerebral availability of metabolic substrates after severe head injury. J Trauma. 1988;28:1523–32.
Ross DT, Graham DI, Adams JH. Selective loss of neurons from the thalamic reticular nucleus following severe human head injury. J Neurotrauma. 1993;10:151–65.
Salvant JB Jr, Muizelaar JP. Changes in cerebral blood flow and metabolism related to the presence of subdural hematoma. Neurosurgery. 1993;33:387–93.
Sheinberg M, Kanter MJ, Robertson CS, Contant CF, Narayan RK, Grossman RG. Continuous monitoring of jugular venous oxygen saturation in head-injured patients. J Neurosurg. 1992;76:212–7.
Sioutos PJ, Orozco JA, Carter LP, Weinand ME, Hamilton AJ, Williams FC. Continuous regional cerebral cortical blood flow monitoring in head-injured patients. Neurosurgery. 1995;36:943–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Juul, N. (2020). Hyperventilation. In: Sundstrøm, T., Grände, PO., Luoto, T., Rosenlund, C., Undén, J., Wester, K. (eds) Management of Severe Traumatic Brain Injury. Springer, Cham. https://doi.org/10.1007/978-3-030-39383-0_60
Download citation
DOI: https://doi.org/10.1007/978-3-030-39383-0_60
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-39382-3
Online ISBN: 978-3-030-39383-0
eBook Packages: MedicineMedicine (R0)