Abstract
Hypoglycemia in patients with diabetes is very common in the hospital and is associated with poor outcomes. While insulin is the generally accepted treatment for diabetes, it is also the primary cause of hypoglycemia. Regular point of care testing for glucose is key for preventing hypoglycemia especially since inpatients may not manifest typical symptoms. Knowledge of insulin action profiles will help mitigate risk for hypoglycemia by matching the insulin to patient needs. Guidelines and protocols should be established in the hospital to assist providers with initiating and adjusting insulin to prevent hypoglycemia. Common clinical situations can be identified which may lead to hypoglycemia and require insulin dosing changes. When hypoglycemia occurs, appropriate acute treatment and steps to prevent recurrence are necessary.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Questions to Ask When a Patient with Diabetes Has Hypoglycemia in the Hospital
-
Has the patient received insulin or sulfonylurea agent to cause hypoglycemia?
-
Does the patient have an underlying condition predisposing to hypoglycemia such as renal or hepatic failure or advanced age?
-
Was the insulin dose weight based or home dose?
-
Are eating habits different in the hospital compared to home?
-
Was prandial insulin mismatched to meal time or meal size?
-
Were continuous tube feedings or TPN held or decreased?
-
Was correctional insulin “stacked”?
-
Were glucose checks done at correct times?
-
Has there been a decrease in medications that cause hyperglycemia such as glucocorticoids or vasopressors?
-
Does the hospital have systems in place to help detect, treat, and prevent hypoglycemia?
Defining Hypoglycemia in the Inpatient Setting
Inpatient hypoglycemia has previously been defined as any glucose <70 mg/dl (3.9 mmol/l) and severe hypoglycemia as glucose <40 mg/dl (2.2 mmol/l) independent of symptoms. However, as of 2017, the American Diabetes Association has modified the definition which now applies to inpatients and outpatients. Level 1 hypoglycemia is any glucose ≤70 mg/dL which is sufficiently low to warrant acute treatment with fast-acting carbohydrate as well as to adjust therapy to prevent in the future. Level 2 hypoglycemia is any level <54 mg/dL (3.0 mmol/l) which is sufficiently low to be considered serious and clinically important. Level 3 hypoglycemia is any glucose low enough to cause severe cognitive impairment which requires external assistance.
Detecting Hypoglycemia
Frequent glucose monitoring is required to detect hypoglycemia with use of insulin. Point of care (POC) testing provides immediate actionable results. Glucose values obtained with venous blood draws sent to the lab are generally less helpful than POC because of the significant time delay for resulting as well as a tendency for glucose levels to decrease in the tube unless sodium fluoride has been added to inhibit glycolysis. However, some medical conditions such as extremes of hematocrit and peripheral ischemia may render POC testing less accurate and require venous draws. With IV insulin protocols, monitoring should be done at least every 1–2 h. With subcutaneous insulin, monitoring is usually at least four times a day: at meals and bedtime when patients are eating and every 6 h when they are NPO. In the inpatient setting, it is important to remember that patients may not manifest usual symptoms of hypoglycemia because of concomitant use of drugs that mask symptoms or diminished cognition from underlying medical conditions, so vigilance is important in detecting hypoglycemia.
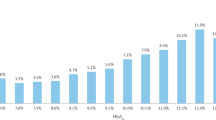
Frequency of Hypoglycemia in Patients Treated with Insulin
Rates of hypoglycemia vary by severity of underlying condition (critical or noncritical), type of glycemic treatment (intravenous insulin or basal-bolus insulin or sliding scale alone), and target glucose range. In the Normoglycemia in Intensive Care Evaluation-Survival Using Glucose Algorithm Regulation (NICE-SUGAR) study, patients in the ICU were randomized to IV insulin targeting glucose of 80–110 mg/dl or 140–180 mg/dl. Nearly 7% of the patients with the lower glucose targets had at least one episode of BG below 40 mg/dl which was significantly greater than the less than 1% rate in the patients in the higher target range. In another study on a general surgical ward, patients with diabetes were randomized to basal-bolus insulin or sliding scale alone with glucose target ranges of 100–140 mg/dl in both groups. In the basal-bolus group, the mean glucose was 145 mg/dl, and in the sliding-scale-alone group, the mean glucose was 175 mg/dl. Incidence of glucose <70 mg/dl was 23% in the basal-bolus group and 4.7% in the sliding scale group. And, a third study looking at insulin dosing found that rates of hypoglycemia are greater with total daily doses of insulin exceeding 0.6 units/kg/day compared to lower doses. The implication of these studies is not to use sliding scale alone rather than basal-bolus or IV insulin but rather to use basal-bolus therapy or IV insulin with appropriate targets and methods for dose calculation. In order to reduce potential for hypoglycemia, most professional society guidelines suggest glucose target goals should be fasting 100–140 mg/dL, premeal <140 mg/dL, and random <180 mg/dL on the general medical ward and 140–180 mg/dl in the ICU setting.
Deleterious Effects of Hypoglycemia
Hypoglycemia in the inpatient setting is strongly associated with higher mortality. In a review of general ward patients with diabetes, each day with any BG <50 mg/dl was associated with an 85% increase in inpatient death, 65% increase in 1-year mortality, and 2.5 extra days of hospitalization. In another retrospective study, inpatients on insulin with an episode of hypoglycemia (BG <50 mg/dl) had an in-hospital mortality rate of 20.3% compared to 4.5% mortality rate in insulin-treated patients without hypoglycemia. In the NICE-SUGAR study, ICU patients on the lower target insulin drip protocol who had severe hypoglycemia (BG <40) had 79% higher mortality than patients on the same insulin drip protocol who did not experience hypoglycemia. In the subset of patients with diabetes, moderate hypoglycemia was associated with 58% higher mortality and severe hypoglycemia with 85% higher mortality than patients with diabetes who did not have hypoglycemia. Whether hypoglycemia is the driver of higher mortality or a marker of poor health, it is clear that it should be avoided if possible.
Identifying Patients Most at Risk for Hypoglycemia
Patients admitted to the hospital often have multiple medical problems. The elderly and patients with renal or hepatic failure are at high risk for hypoglycemia because of decreased gluconeogenesis as well as decreased insulin metabolism. Another risk group is patients with unusually high outpatient insulin doses (over 1 unit/kg/day total daily dose) which may indicate either noncompliance or excess caloric intake, both of which will be corrected in the hospital, and therefore giving 80% of the usual outpatient dose or recalculating with standard weight-based dosing may be prudent.
Common inpatient situations that lead to an acute drop in insulin requirements are listed in Table 23.1. Change in nutrition is responsible for many episodes of hypoglycemia. Patients with insulin “on board” and who are on TPN or enteral tube feeds who have the feedings held or decreased or patients who are eating and are made NPO or do not eat a complete meal are particularly vulnerable. Other common high-risk scenarios include patients on high-dose steroids who have the steroid dose dropped, patients on high insulin infusion rates due to vasopressors who have them tapered, and patients who develop acute renal, hepatic, or adrenal failure. Patients who are actually improving such as patients with sepsis or MI and secondary acute hyperglycemia (stress hyperglycemia) will see glucose levels drop and insulin requirements decrease. Hypoglycemia should be anticipated in all these situations and insulin doses dropped preemptively to prevent hypoglycemia.
When subcutaneous insulin has already been given, short-term IV glucose infusion may be necessary to avoid hypoglycemia. For patients on continuous tube feeds, for example, that are abruptly discontinued (e.g., patient pulls out NG tube), D5W at the rate of the tube feeds or D10 at half the rate of the tube feeds will usually be adequate to avoid short-term hypoglycemia until beyond the period of active insulin action or the tube feeds can be restored. Communication between nursing and providers is essential to manage these situations that often are unpredictable.
Insulin Action
Medications that may contribute to hypoglycemia in the inpatient setting include drugs in the sulfonylurea class (glyburide, glipizide, glimepiride in the United States), meglitinides (usually repaglinide), and all insulins. In general, use of oral agents is discouraged in the hospital because of unpredictable and prolonged action, especially in the setting of hepatic or renal dysfunction or interruption of nutritional patterns.
Insulin is the most widely used medication to treat hyperglycemia in the inpatient setting because the many types of insulin offer a wide range of available action profiles to allow greater flexibility in dosing. However, insulin is also responsible for medication-induced hypoglycemia because of its narrow therapeutic window. Insulin action profiles are shown in Table 23.2. Patients are most at risk for hypoglycemia at the peak action of the insulin. When two types of insulin are used, hypoglycemic potential will be additive. Premixed insulin is not recommended in the hospital setting because the faster-acting and longer-acting components cannot be individually adjusted. When regular insulin is given IV either as a bolus or as a continuous drip, the impact is immediate and action can persist for up to an hour after the dose.
Initial Dosing of Insulin to Avoid Hypoglycemia
In patients naive to insulin who are admitted to the hospital, a framework for prescribing insulin is critical to assist in meeting glucose targets and avoid hypoglycemia. Weight; age; renal, hepatic, and pancreatic functions; and steroid use all impact insulin requirements. Generally insulin is prescribed using a combination of intermediate- or long-acting insulin (basal) with short- or rapid-acting insulin (nutritional and correctional). The schema in Fig. 23.1 is a handy way to calculate the doses. For patients on TF or glucocorticoid treatment, consider using 60% of TDD as nutritional component rather than 50%.
(a) Step 1: initiation of insulin and determination of total daily dose (TDD). Use weight or if patients on insulin as outpatient consider 80% of home dose, but not to exceed 1 unit/kg TDD (b) Step 2: Components of insulin program: basal, nutritional, correctional. (Reprinted from Hudson M.S., Palermo N.E. Diabetes in Older Adults, pp. 1–18, In: Rosenthal R., Zenilman M., Katlic M. (eds) Principles and Practice of Geriatric Surgery, © 2017, with permission from Springer Nature. See Suggested Readings)
Correctional insulin (sliding scale) can be prescribed based on the calculated total daily dose so that if TDD is less than or equal to 40 units, use a correctional scale of 1 unit rapid-acting or short-acting insulin for every 50 mg/dl above goal. For TDD over 40 units a day, consider using 1 unit for every 25 mg/dl above goal. Correctional insulin is generally given with a rapid-acting insulin analog before meals and before bed in patients who are eating and with regular human insulin every 6 h in patients who are on continuous feedings, TPN, or NPO. Outside of hyperglycemic emergencies, correctional insulin should not be given more frequently than this to avoid hypoglycemia from overlapping the actions of repeated doses, a phenomenon known as “stacking.” Some institutions give only “half” scale for bedtime correctional insulin to avoid potential for overnight hypoglycemia.
What to Do When Hypoglycemia Occurs
All hospitals should have protocols in place for managing acute hypoglycemia both on the general wards and in the ICU. Generally, treatment should be started in the hospital when glucose falls below 70 mg/dl. If possible, patients should be treated orally. A nursing protocol should be in place for treatment (Fig. 23.2).
The art of managing hypoglycemia is to determine which insulin dose may be responsible for an episode of hypoglycemia and how much it should be reduced. Knowing the insulin action profile (see Table 23.2) is helpful. Generally the early morning glucose is the best reflection of the action of basal insulin, but this may not be the case if the patient is receiving rapid-acting insulin late at night (nighttime correctional scales) or overnight (e.g., with continuous enteral nutrition). Premeal or pre-bed hypoglycemia may reflect the rapid-acting insulin given with the previous meal.
If the hypoglycemia is associated with a significant change in medical condition (stopping steroids, e.g., or acute renal failure), dose adjustments in the range of 30–50% may be necessary. However, if the patient is otherwise clinically stable, a simple calculation for adjusting insulin is to decrease the TDD of insulin by 10% for glucose values running 70–99 mg/dl and to decrease the TDD by 20% for any glucose value below 70 mg/dl.
Hospital Surveillance and Reporting: Glucometrics
Hospitals should have in place quality improvement programs to monitor glucose values generally and episodes of hypoglycemia specifically so that areas with recurrent problems can be identified and causes addressed. The Society for Hospital Medicine has developed a national Glucose Control Mentored Implementation Program that hospitals can join to report their glucose values. The hospital can then be benchmarked against other institutions for metrics such as days with any glucose below 70 mg/dl. In this way, the institution can assess performance on a national level and hopefully find ways to improve patient care. For more information, go to http://dev.hospitalmedicine.org/Web/Quality_Innovation/Implementation_Toolkits/Glycemic_Control/Web/Quality___Innovation/Implementation_Toolkit/Glycemic/Track_Performance/Introducing_Glucometrics.aspx
Beyond Basal-Bolus Insulin: Glucose Control Without Hypoglycemia
Because of concern for hypoglycemia and its potentially devastating consequences, improvements on current basal-bolus treatment recommendations are being actively studied. A trial comparing basal-bolus insulin to basal plus correctional insulin (i.e., no scheduled mealtime insulin) showed similar average glucose values but less moderate hypoglycemia (<70 mg/dl) in the basal plus correctional treatment group. Other trials have looked at using DPP-4 inhibitors or GLP-1 receptor agonist agents in the inpatient setting, but these have not received general acceptance at this time.
Suggested Reading
American Diabetes Association. Diabetes care in the hospital. Diabetes Care. 2017a;40(Suppl 1):S120–7.
American Diabetes Association. Glycemic targets. Sec 6. In Standards of medical care in diabetes–2017. Diabetes Care. 2017b;40(Suppl. 1):S48–56.
Garg R, Hurwitz S, Turchin A, Trivedi A. Hypoglycemia, with or without insulin therapy, is associated with increased mortality among hospitalized patients. Diabetes Care. 2013;36(5):1107–10.
Hudson MS, Palermo NE. Diabetes in older adults. In: Rosenthal R, Zenilman M, Katlic M, editors. Principles and practice of geriatric surgery. Cham: Springer; 2017. p. 1–18.
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY, Blair D, Foster D, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–97.
Rubin DJ, Rybin D, Doros G, McDonnell ME. Weight-based, insulin dose-related hypoglycemia in hospitalized patients with diabetes. Diabetes Care. 2011;34(8):1723–8.
Society of Hospital Medicine. Quality & innovation. External sources & benchmarking/glycemic control implementation toolkit 2017 https://www.hospitalmedicine.org/Web/Quality_Innovation/Implementation_Toolkits/Glycemic_Control/Web/Quality___Innovation/Implementation_Toolkit/Glycemic/Track_Performance/external_sources_benchmarking.aspx.
Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care. 2009;32(7):1153–7.
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, Umpierrez D, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care. 2011;34(2):256–61.
Umpierrez GE, Smiley D, Hermayer K, Khan A, Olson DE, Newton C, et al. Randomized study comparing a Basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169–74.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hudson, M. (2020). Hypoglycemia in Patients with Diabetes. In: Garg, R., Hennessey, J., Malabanan, A., Garber, J. (eds) Handbook of Inpatient Endocrinology. Springer, Cham. https://doi.org/10.1007/978-3-030-38976-5_23
Download citation
DOI: https://doi.org/10.1007/978-3-030-38976-5_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-38975-8
Online ISBN: 978-3-030-38976-5
eBook Packages: MedicineMedicine (R0)