Abstract
Peritalar fracture dislocations are relatively uncommon. They usually occur as a result of high-energy trauma and are frequently associated with concomitant bony injuries. If not treated appropriately, these injuries can lead to significant morbidity. Appropriate management includes a meticulous physical examination focused on the condition of the skin and soft tissues, and a thorough understanding of fracture morphology utilizing plain X-ray and computed tomography. Dislocations must be diagnosed and reduced promptly. If closed reduction is unsuccessful, then open reduction is indicated. Peritalar fractures, especially those involving the subtalar joint, can cause residual instability and lead to post-traumatic arthrosis if not accurately reduced. Common complications following subtalar fracture dislocations include hindfoot stiffness, subtalar and/or tibiotalar arthrosis, and soft tissue injuries. Accurate diagnosis, expeditious reduction, and anatomic fixation are essential tenets to lessen long-term sequelae in the management of these complex fracture patterns.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Subtalar
- Peritalar
- Fracture-dislocation
- Talus dislocation
- Calcaneus dislocation
- Talus fracture
- Calcaneus fracture
Peritalar and Subtalar Dislocations
Introduction/Background
Fractures or dislocations of the talus are uncommon injuries, accounting for approximately 1% of all fractures [1]. These injuries are most commonly seen in the setting of motor vehicle accidents or falls from height. The predominant demographic affected is young adult males aged 20–39 [1, 2]. Approximately 86% of patients with talus fractures have an additional associated fracture. The most commonly associated fracture is that of the malleoli seen in ~22% of cases. Other commonly associated fractures include those of the spine, femur, and, in 4% of cases, the calcaneus [3].
Traumatic injury to the subtalar joint may occur during subtalar dislocations, talus or calcaneus intra-articular fractures, and fracture-dislocations. In fractures and fracture-dislocations of the talus and calcaneus involving the subtalar joint, anatomic reconstruction of joint congruity is paramount for optimizing outcomes. If the subtalar joint is not reduced anatomically, the patient is at risk for chronic instability, subtalar arthritis, and hindfoot deformity. These issues can be symptomatic and cause significant morbidity to the patient [4, 5].
Operative treatment of displaced, intra-articular fractures involving the talus and calcaneus are difficult. Anatomic reduction is essential, and the soft tissues must be respected in order to minimize complications and optimize outcomes. In this chapter, we outline proper methods for diagnosis and surgical management of fractures and fracture-dislocations of the talus and calcaneus.
Diagnosis/Management
A thorough history will typically reveal an acute trauma resulting in immediate pain at the foot or ankle and the inability to bear weight. Examination of the skin is expected to reveal swelling of the hindfoot; in cases of fracture-dislocation, there can be severe deformity with tethering of the skin. Other skin issues that are possible are traumatic wounds and fracture blisters [6]. The status of the neurovascular bundle also has treatment implications and is part of the standard exam.
Initial imaging work-up includes radiographs of the foot and ankle. Computed tomography (CT) scans are also recommended for more detailed evaluation of fracture morphology, displacement, and preoperative planning [1, 7]. There are other radiographic views that have utility in evaluating the hindfoot. Broden’s view can be used to visualize the subtalar joint preoperatively and will be used in the operating room with fluoroscopic examination to evaluate the accuracy of joint reduction [8]. The Canale view aids in the visualization of the long axis of the talar neck. The Harris heel view provides an axial view of the hindfoot.
Dislocations should be immediately identified and reduced. The need for immediate reduction is especially pressing in the setting of neurovascular compromise and/or skin ischemia. Medial subtalar dislocations display a medially displaced heel, inversion, and plantarflexion of the foot. Medial dislocations more commonly have an associated fracture. In lateral subtalar dislocations, the heel is displaced laterally and the foot is in eversion and abduction. These are more frequently associated with open injuries [9]. Tongue-type calcaneus fractures can also cause skin breakdown rapidly.
In approximately 10% of peritalar dislocations , there will be a mechanical block to reduction. In medial dislocations, the talar head may buttonhole through the extensor digitorum brevis tendon. Lateral dislocations can be obstructed by interposed tibialis posterior tendon [10]. Multiple closed reduction attempts are not recommended, as this may cause further articular and soft tissue damage.
Emergency operative intervention is indicated in the setting of irreducible dislocations, associated neurovascular impingement/compromise, open fractures and dislocations, or an extruded talus.
If successful reduction of a subtalar or peritalar dislocation is obtained, then management is dictated by the stability of the joint, the involvement of the articular surface, and the condition of the soft tissue envelope. Peritalar fractures can cause residual instability and must be identified. Post-reduction CT examination is recommended as fractures of the posterior talar process or sustentaculum can be missed on plain radiographs [11,12,13]. After lateral subtalar dislocations, the lateral process of the talus must be carefully inspected for a fracture. As these fractures are articular, ORIF is indicated for displaced articular fractures for fragments of sufficient size [14].
If the joint is stable after closed reduction and there are no associated articular fractures that warrant operative management, then the patient should be immobilized and made non-weight bearing in a short leg cast for 6 weeks. After this, a protocol of progressive weight bearing and physiotherapy is begun. Good results have been obtained in patients with full weight bearing starting at 10–11 weeks from injury [15]. However, if residual instability is identified, options include external fixation and transarticular Kirschner wire fixation for 3–4 weeks [14].
In the case of open dislocations or irreducible dislocations from entrapped soft tissue necessitating open reduction, soft tissue management will dictate immobilization. These merit external fixator immobilization to facilitate wound care. Occasionally massive soft tissue swelling or traumatized skin may prohibit cast treatment after closed reduction even if it is stable. In these, external fixators have also been used with good results leading to weight bearing around 10–12 weeks [15].
Results and Complications
Peritalar injury with subtalar dislocations as a whole are relatively rare, and even more so to occur in isolation. Eighty-eight percent of these injuries are associated with at least one other foot or ankle injury. The most commonly associated injury is fracture to the talus itself, followed closely by injuries to the ankle, found in 60% and 52% of cases, respectively, in one series [16]. Calcaneus fractures were found to occur in up to 16% of cases. Interestingly, the midtarsals and metatarsals are relatively infrequently injured in association with peritalar dislocations [16]. As a result of the high rate of concomitant injuries, studies looking at outcomes are limited and frequently confounded.
Complications reported include post-traumatic arthritis of the subtalar and tibiotalar joint, avascular necrosis of the talus, tendon injuries, neurovascular injury, skin necrosis and wound breakdown, hindfoot stiffness, and with open injuries deep soft tissue and bone infections [9, 14].
Several have reviewed the rates of subtalar arthritis and subsequent subtalar fusion seen in peritalar injury patterns. Subtalar dislocations are reported with a wide range from 39% to 89% developing radiographic subtalar arthritis; however, only about one-third of these will have clinical symptoms requiring fusion [14, 16, 17]. This wide range of data is likely a reflection of the array of severity of these injuries with higher energy, leading to worse arthritis and subsequent reconstructive procedures. The lowest rates of arthritis and subsequent fusion requirement are reported from purely ligamentous dislocations of the subtalar joint [4]. In a series of 23 patients with CT-proven isolated subtalar dislocations, Jungbluth et al. found only 39% developed mild radiographic changes at 5 years, and this did not correlate with patient symptomotology [15]. They emphasize the urgency of reduction in keeping a relatively low rate of arthritis after isolated subtalar dislocations.
Avascular necrosis of the talus is most commonly associated with fractures of the talar neck, but it can also occur with subtalar dislocations. Displacement and open wounds have both been associated with the development of AVN [18, 19]. Rates have been reported from 0% to 10% AVN with closed dislocations, which rises to 50% with open dislocations [14]. However, improved rates have been shown with early reduction and stable fixation [20].
Post-traumatic arthritis most frequently involves the subtalar joint [21, 22]. Contributing factors leading to arthritis are initial chondral damage at the time of injury, altered joint mechanics secondary to malunion, and prolonged immobility. If there are peritalar fractures involving a joint, then restoration of congruity to preserve mechanics is important.
Most outcomes after subtalar dislocations have been reported in small case series. At approximately 5-year follow-up, the mean AOFAS score following the treatment of a subtalar dislocation averages 71–83, with the contralateral as a control averaging 93 [15, 16].
It is clear from the literature that peritalar fracture dislocations are difficult injuries to treat and that knowledge of techniques for precise surgical management are critical for improving outcomes.
Case 1
Clinical history
A 54-year-old female presents s/p pedestrian struck with right-ankle pain, deformity, and open wound. Intubated emergently in trauma bay due to altered mental status and airway protection.
Physical Exam
Right Lower Extremity
Gross deformity at ankle with skin tenting proximal lateral foot, 2 × 1 cm deep wound with oozing blood, palpable DP/PT pulses. Unable to assess motor/sensation due to patient condition.
Imaging
Pre-reduction injury films and select CT cuts after reduction (Figs. 10.1 and 10.2).
Closed reduction performed in trauma bay, post-reduction CT obtained.
Diagnosis
Open right medial subtalar dislocation with posterior talar body fracture.
-
1.
Setup (patient position, instruments/implants need)
-
Supine
-
Radiolucent cantilever table
-
Medium or large external fixator
-
6.5 mm threaded Schanz pin
-
Tourniquet
-
-
2.
Execution – Approach used, reduction maneuvers, how implants used and placed
Begin with a gastrocnemius recession. This is an injury that occurs secondary to forced plantarflexion. The gastrocnemius complex functions as a pathologic force in this injury pattern. Therefore, the release of the gastrocnemius is part of this procedure, taking tension off of the area of injury as well as the eventual repair.
-
The incision is ~2 cm posterior to the posteromedial border of the tibia.
-
The gastrocnemius tendon is identified and separated from the soleus.
-
It is released sharply in a medial to lateral direction.
-
While supine, apply the ankle spanning external fixator. After gastrocnemius recession performed and external fixator applied, flip prone to begin fixation of the talus fracture.
A posteromedial approach can be used, beginning 1 cm medial to the Achilles tendon. Identify the FHL and incise its tendon sheath. The FHL can be swept medial and held out of the surgical field with two 1.6 mm Kirschner wires placed into the medial aspect of the distal tibia. Distraction can then be placed through the external fixator. Provisional fixation of the talus is held with 1.25 mm Kirschner wires. Intraoperative images (Figs. 10.3 and 10.4) and immediate postoperative films (Fig. 10.5) are shown.
Key Points of This Case
-
Starting supine with gastrocnemius recession can be useful in neutralizing the deforming forces in subtalar dislocations. Apply your external fixator while still supine before flipping prone.
-
Use Kirschner wires anchored in the medial distal tibia to help retract the FHL tendon and neurovascular structures medial and away from your surgical field.
-
Distract through your external fixator to better visualize the subtalar joint and protect your fixation post-operatively.
Case 2
Clinical History
A 21-year-old male presents status post-traumatic injury to right foot by a power jack. Isolated injury with decreased sensation on plantar aspect of foot.
Physical Examination
Right Lower Extremity
Three large soft tissue lacerations are seen.
-
Medial wound extending from the level of the sustentaculum posteriorly and inferiorly around the heel cord at the level of the tuberosity. Calcaneus exposed through the medial wound.
-
10–14 cm dorsolateral laceration of foot extending from the navicular to just posterior to the fibula 4 cm proximal to the tip with exposed tendons.
-
Approximately 2 cm wound over sinus tarsi with tendon exposed.
Imaging
Pre-reduction injury films (Fig. 10.6), post-reduction radiographs (Fig. 10.7), and select CT cuts after reduction (Fig. 10.8).
Reduction performed in the Trauma Bay and post-reduction films and a CT scan obtained.
Diagnosis
Right open medial subtalar fracture dislocation with a fracture of the calcaneal sustentaculum.
-
1.
Setup (patient position, instruments/implants need).
-
Supine on a cantilever radiolucent table.
-
Saline fluid and tubing for gravity irrigation.
-
Tourniquet
-
Kirschner wires 1.0–1.6 mm.
-
Mini-fragment set.
-
Medium or large external fixator (backup).
-
-
2.
Execution – Approach used, reduction maneuvers, implants placement.
-
Reduction achieved with knee flexion, ankle plantarflexion, and traction applied with a valgus moment on the midfoot. This allowed the talar head to be manipulated back into place.
-
Thorough exploration, irrigation, and debridement of the traumatic wounds were performed.
-
The medial of the three traumatic wounds provided access to the sustentacular fracture, obviating the need for a separate surgical approach. The surgical approach to the sustentaculum involves a small incision 2 cm caudal to the medial malleolus and 2 cm proximal to the navicular [23].
-
The posterior neurovascular bundle was protected and explored to identify any areas of disruption during the time of initial debridement.
-
The FHL was retracted inferiorly to expose the fragment.
-
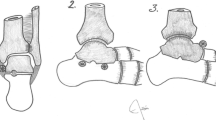
The mobile fragment of the sustentaculum was manipulated into place using Kirschner wires as joysticks and pinned in place (Fig. 10.9a,b).
-
The fragment was anatomically reduced under direct visualization, and absolute stability was obtained through compression with lag screws.
-
In this case, two 2.4 mm screws were used with lag by technique through a small 2.0 plate as a washer (Fig. 10.9d–f).
-
Fluoroscopic Broden’s views were used to confirm non-penetration into the posterior facet. In this case, the lateral wound also allowed direct visualization of the Kirschner wires that were used as drill bits as well as for provisional fixations. These wires were seen to exit the lateral cortex posterior to the sinus tarsi and plantar to the posterior facet.
-
The stability of the subtalar joint was reassessed. This patient was still able to be dislocated medially through subtalar and talonavicular joints. Therefore, after confirming the reduction of the two joints, the talonavicular joint was pinned retrograde with 1.6 k-wires (Fig. 10.10). These pins were left for 8 weeks in order to maintain the alignment of the joints. Therefore, they were cut below the level of the skin to prevent pin tract infection. Follow-up radiographs show preservation of the subtalar joint with minimal signs of arthrosis (Figs. 10.11 and 10.12).
References
Dale JD, Ha AS, Chew FS. Update on talar fracture patterns: a large level I trauma center study. AJR Am J Roentgenol. 2013;201(5):1087–92.
Vallier HA, Nork SE, Barei DP, Benirschke SK, Sangeorzan BJ. Talar neck fractures: results and outcomes. J Bone Joint Surg Am. 2004;86-A(8):1616–24.
Elgafy H, Ebraheim NA, Tile M, Stephen D, Kase J. Fractures of the talus: experience of two level 1 trauma centers. Foot Ankle Int. 2000;21(12):1023–9.
Rammelt S, Bartoníček J, Park KH. Traumatic injury to the subtalar joint. Foot Ankle Clin. 2018;23(3):353–74.
Rammelt S, Grass R, Zawadski T, Biewener A, Zwipp H. Foot function after subtalar distraction bone-block arthrodesis. A prospective study. J Bone Joint Surg Br. 2004;86(5):659–68.
Rammelt S, Biewener A, Grass R, Zwipp H. Foot injuries in the polytraumatized patient. Unfallchirurg. 2005;108(10):858–65.
Chan G, Sanders DW, Yuan X, Jenkinson RJ, Willits K. Clinical accuracy of imaging techniques for talar neck malunion. J Orthop Trauma. 2008;22(6):415–8.
Broden B. Roentgen examination of the subtaloid joint in fractures of the calcaneus. Acta Radiol. 1949;31(1):85–91.
Goldner JL, Poletti SC, Gates HS, Richardson WJ. Severe open subtalar dislocations. Long-term results. J Bone Joint Surg Am. 1995;77(7):1075–9.
LEITNER B. Obstacles to reduction in subtalar dislocations. J Bone Joint Surg Am. 1954;36(A:2):299–306.
Bibbo C, Lin SS, Abidi N, Berberian W, Grossman M, Gebauer G, et al. Missed and associated injuries after subtalar dislocation: the role of CT. Foot Ankle Int. 2001;22(4):324–8.
Dürr C, Zwipp H, Rammelt S. Fractures of the sustentaculum tali. Oper Orthop Traumatol. 2013;25(6):569–78. Epub 2013/12/06
Giuffrida AY, Lin SS, Abidi N, Berberian W, Berkman A, Behrens FF. Pseudo os trigonum sign: missed posteromedial talar facet fracture. Foot Ankle Int. 2003;24(8):642–9.
Rammelt S, Goronzy J. Subtalar dislocations. Foot Ankle Clin. 2015;20(2):253–64. Epub 2015/03/29
Jungbluth P, Wild M, Hakimi M, Gehrmann S, Djurisic M, Windolf J, et al. Isolated subtalar dislocation. J Bone Joint Surg Am. 2010;92(4):890–4.
Bibbo C, Anderson RB, Davis WH. Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases. Foot Ankle Int. 2003;24(2):158–63.
Heppenstall RB, Farahvar H, Balderston R, Lotke P. Evaluation and management of subtalar dislocations. J Trauma. 1980;20(6):494–7.
Vallier HA, Nork SE, Benirschke SK. Sangeorzan BJ. Surgical treatment of talar body fractures. J Bone Jt Surg Am. 2004;86-A(Suppl 1 (Pt 2)):180–92.
Lindvall E, Haidukewych G, DiPasquale T, Herscovici D, Sanders R. Open reduction and stable fixation of isolated, displaced talar neck and body fractures. J Bone Joint Surg Am. 2004;86-A(10):2229–34.
Milenkovic S, Mitkovic M, Bumbasirevic M. External fixation of open subtalar dislocation. Injury. 2006;37(9):909–13.
Maher MH, Chauhan A, Altman GT, Westrick ER. The acute management and associated complications of major injuries of the talus. JBJS Rev. 2017;5(7):e2.
Dodd A, Lefaivre KA. Outcomes of Talar neck fractures: a systematic review and meta-analysis. J Orthop Trauma. 2015;29(5):210–5.
Della Rocca GJ, Nork SE, Barei DP, Taitsman LA, Benirschke SK. Fractures of the sustentaculum tali: injury characteristics and surgical technique for reduction. Foot Ankle Int. 2009;30(11):1037–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jung, M., Galloway, J., Eastman, J. (2020). Fractures and Dislocations of the Talus and Calcaneus: A Case-Based Approach. In: Adams, M., Benirschke, S. (eds) Fractures and Dislocations of the Talus and Calcaneus. Springer, Cham. https://doi.org/10.1007/978-3-030-37363-4_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-37363-4_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-37362-7
Online ISBN: 978-3-030-37363-4
eBook Packages: MedicineMedicine (R0)