Abstract
Hepatocellular carcinoma (HCC) associated with NAFLD has been steadily increasing and non-alcoholic steatohepatitis (NASH) is the most rapidly growing risk for liver transplantation in patients with HCC in the last years. In the vast majority of cases, HCC develops in the context of hepatic cirrhosis, but recent data suggest that there is a proportion of patients with NAFLD who are at high risk for HCC in the absence of cirrhosis. Although no study clearly explains the evolution of NAFLD to HCC, researchers suggest that the most likely mechanism involves fatty acid (FA) accumulation in hepatocytes due to predisposing factors, such as MtS, increased oxidative stress, endoplasmic reticulum (ER) stress, mitochondrial dysfunction and chronic endotoxaemia. Genetic and epigenetic changes in pathogenesis and hepatic carcinogenesis potentially serve as potential diagnostic biomarkers and/or therapeutic targets. MicroRNAs (miRNAs) play a key role in the pathogenesis of HCC related to NAFLD by closely regulating lipid metabolism, glucose homeostasis, cell proliferation, apoptosis, and cell migration and differentiation. In other words, there are currently no guidelines for the screening and early detection of NAFLD-related HCC in the absence of cirrhosis. However, there is an increasing number of HCC cases without cirrhosis. Thus, there is a strong interest in identifying biomarkers to detect early detection of HCC risk related to NAFLD progression.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Hepatocellular carcinoma (HCC) is the most common primary malignant tumour of the liver and one of the most prevalent neoplasms in the world [1,2,3]. Together with hepatitis B virus (HBV), hepatitis C virus (HCV), prolonged long-term alcohol consumption, aflatoxin, and metabolic liver disease, non-alcoholic fatty liver disease (NAFLD) is a significant risk factor for HCC. Since the first reported case of HCC associated with NAFLD in 1990 [4], the number of cases has been steadily increasing [5]. In the last years, Wong et al. demonstrated in two studies that non-alcoholic steatohepatitis (NASH) is the most rapidly growing risk for liver transplantation in patients with HCC [6, 7].
In the vast majority of cases, HCC develops in the context of hepatic cirrhosis, but recent data suggest that there is a proportion of patients with NAFLD who are at high risk for HCC in the absence of cirrhosis [8,9,10,11]. In 2009, our group described seven cases of HCC in histologically confirmed NASH patients. Of these, one was non-cirrhotic (NASH stage 1), demonstrating that relevant fibrosis or cirrhosis is not mandatory for the onset of HCC [12]. Afterwards, in another study by our group with a larger number of patients (42 HCC cases secondary to NAFLD or cryptogenic cirrhosis), we identified almost 10% non-cirrhotic patients in the study [13]. Currently, some studies have demonstrated the onset of HCC in the absence of cirrhosis [13,14,15,16]. In a multicentre national Brazilian study involving nine hepatology units from six states of the country, we evaluated the clinical characteristics of 110 patients diagnosed with HCC and NAFLD. In this study, the mean age was 67 ± 11 years and 65.5% were male. Obesity was observed in 52.7% of the cases, type 2 diabetes mellitus (T2DM) in 73.6%, dyslipidaemia in 41%, arterial hypertension in 60%, and metabolic syndrome (MtS) in 57.2%. The histological diagnosis of HCC was made in 47.2% of the patients, and among these patients, NASH with cirrhosis was observed in 61.5%, NASH with fibrosis stage 1–3 in 27%, and NAFLD without fibrosis in 3.8% [17]. Evidence that HCC is part of the natural history of NASH comes from retrospective studies, case reports, and studies evaluating the late complications of NASH and cirrhosis associated with NASH [18].
Pathophysiology of NASH-Related HCC
Although no study clearly explains the evolution of NAFLD to HCC, researchers suggest that the most likely mechanism involves fatty acid (FA) accumulation in hepatocytes due to predisposing factors, such as MtS, increased oxidative stress, endoplasmic reticulum (ER) stress, mitochondrial dysfunction and chronic endotoxaemia. All these phenomena contribute to the onset of inflammation and fibrosis, leading to a chronic and progressive lesion [19, 20].
Studies show that 70% of individuals with T2DM and 90% of individuals who are obese have some form of triglyceride (TG) accumulation in the liver, such as simple steatosis (60%), NASH (25–30%) or cirrhosis (5–10%), indicating that NAFLD and NASH are common in these individuals. NAFLD and NASH may be the link between MtS (with obesity as the main factor) and HCC, that is, individuals who have the main factors of MtS [insulin resistance (IR)/T2DM and obesity] present with high chances of TG accumulation in the liver, which in turn can lead to NAFLD and progress to NASH, cirrhosis and HCC [21,22,23].
Park et al. (2010) described the development of HCC in the context of obesity as a function of increased expression of tumour necrosis factor alpha (TNF-α) and interleukin-6 (IL-6). These cytokines, in addition to causing hepatic inflammation, activate the oncogenic signal transducers and activators of transcription 3 (STAT3), which increases the proliferation and progression of hepatocytes with oncogenic mutations, leading to tumour development [24].
Deregulated cell growth in the context of hyperinsulinaemia has been described as a function of insulin-like growth factor 1 (IGF-1), mannose 6-phosphate receptor/insulin-like growth factor receptor 2 (M6P/IGF2R), and the first insulin receptor substrate (IRS-1). Hyperinsulinaemia increases the production of IGF-1, a hormonal peptide that stimulates cell growth by cell proliferation and inhibition of apoptosis in the liver. Insulin also activates IRS-1, which is involved in cytokine signalling pathways and is increased in HCC. MP6/IGF2R, a tumour suppressor gene, regulates cell growth through inhibition of cell proliferation and apoptosis via transforming growth factor beta (TGF-β) and insulin-like growth factor 2 (IGF-2), respectively. Interestingly, MP6/IGF2R mutations have been identified in HCC, even in the absence of viral hepatitis or liver cirrhosis. Adiponectin is an adipose tissue specific anti-inflammatory polypeptide that is decreased in the state of IR and has been shown to be responsible for the inhibition of angiogenesis via modulation of apoptosis in animal models [25, 26].
The development of NASH is also related to oxidative stress and the release of reactive oxygen species (ROS), which probably contribute to the development of HCC. Oxidative stress may favour tumourigenesis through steatosis, inflammation and cell proliferation or may induce mutations directly associated with cancer. It has been shown that 4-hydroxynonenal, a lipid peroxidation product, causes mutations in the p53 tumour suppressor gene that is associated with more than half of human cancers, including HCC [27]. Nuclear factor transcription factor respiratory factor 1 (Nrf1) is essential in the mediation of oxidative stress. Xu et al. (2005) demonstrated in an animal model that the lack of this factor increases the susceptibility to oxidative stress. The hepatic histology of Nrf1-deficient animals showed steatosis, apoptosis, necrosis, inflammation and fibrosis, and the development of HCC related to oxidative stress was observed in some cases [28].
Recently, the c-Jun amino-terminal kinase 1 protein (JNK1) has been related to obesity, IR, NASH and HCC. FA, TNF-α and ROS released in the hyperinsulinaemic scenario are all potent activators of JNK1, which in turn phosphorylates IRS-1. Obesity is associated with abnormal elevation of JNK1 activity. Activation of JNK1 and subsequent phosphorylation of IRS-1 are crucial components of the biochemical signalling responsible for obesity induced by IR. The activity of JNK1 has previously been associated with a variety of cancers. More recently, definitive evidence has demonstrated a significant relationship between sustained activation of JNK1 and development of HCC [25, 29].
Hepatic carcinogenesis in NASH may also be mediated by cellular mechanisms. Hepatocyte injury related to NAFLD leads to an overactivation of the Hedgehog pathway, a complex cellular pathway for repair and tissue regeneration. One of the key mechanisms activated through stimulation of this pathway involves mobilization of hepatic progenitor cell populations to replace damaged hepatocytes. Although essential for liver repair, aberrations in the activation of the hepatic progenitor cell population can lead to impaired repair and dysregulated proliferation of hepatocytes, potentiating carcinogenesis [26, 30].
The role of the adaptive immune system has been recognized through studies in animal models of NASH-related HCC. Factors that activate inflammation such as nuclear factor kappa B (NF-kB) and insulin receptor (IR) contribute to carcinogenesis in patients with NAFLD. Ma et al. (2016) demonstrated in an animal model that the deregulation of lipid metabolism in NAFLD leads to a selective loss of CD4+ T lymphocytes but not CD8+ T lymphocytes, leading to increased hepatic carcinogenesis [31]. In another study by Wolf et al. (2014), which also used an animal model, described the metabolic activation of CD8 + T lymphocytes and natural killer (NK) cells acting synergistically with inflammatory cytokines and leading to liver damage and inducing carcinogenesis [32].
Another mechanism that has been associated with the pathogenesis of HCC secondary to NAFLD is genetic predisposition. Romeo et al. (2008) described a single nucleotide polymorphism (SNP) in the Patatin-like phospholipase domain containing 3 (PNPLA3) gene, which strongly affects the accumulation of fat in the liver in the absence of IR. The PNPLA3 risk allele rs738409 [G] is found in approximately 40% of the European population and may increase the risk of progression to NASH threefold and, more importantly, the risk of developing HCC 12-fold [33].
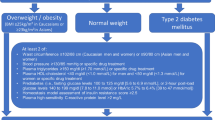
The Fig. 11.1 summarizes the possible mechanisms involved in the evolution/progression of NAFLD to HCC.
Possible mechanisms involved in the evolution/progression of non-alcoholic fatty liver disease (NAFLD) to hepatocellular carcinoma (HCC). Legend: NASH non-alcoholic steatohepatitis, HCC hepatocellular carcinoma, FFA free fatty acids, ROS reactive oxygen species, IGF-1 insulin-like growth factor 1, IRS-1 insulin receptor substrate 1, M6P/IGF2R mannose 6-phosphate receptor/insulin-like growth factor receptor 2, TNF-α tumor necrosis factor alpha, NF-kB nuclear factor kappa B, IL-6 interleukin-6, STAT signal transducers and activators of transcription
Biomarkers in NAFLD Progression and HCC
Genetic and epigenetic changes in pathogenesis and hepatic carcinogenesis potentially serve as potential diagnostic biomarkers and/or therapeutic targets. MicroRNAs (miRNAs) play a key role in the pathogenesis of HCC related to NAFLD by closely regulating lipid metabolism, glucose homeostasis, cell proliferation, apoptosis, and cell migration and differentiation [34]. Due to the effect of miRNAs on lipid metabolism and hepatic carcinogenesis, miRNAs have been considered a novel therapeutic target for metabolic disorders and HCC. Maintaining normal lipid and glucose homeostasis may prevent the development of HCC related to NAFLD. However, there is still a long way to understand the comprehensive molecular mechanisms of pathogenesis and progression of NAFLD-related HCC.
Similar to other metabolic diseases, NAFLD is a multifactorial disease in which genetic predisposition, environmental exposures, and lifestyle factors can modulate susceptibility to the disease and its progression [35]. Thus, there is a strong interest in identifying biomarkers to detect NAFLD early and monitor the progression of the disease.
Studies have shown that non-coding RNAs (ncRNAs) are implicated in the aetiology of NAFLD and are possibly the main mediators in their pathogenesis [36, 37]. ncRNAs are constitutively expressed and can regulate biological processes, genes and proteins [38]. miRNAs are the most studied ncRNAs with their well-defined biogenesis and processing [39]. miRNAs are highly conserved single-stranded short-chain ncRNAs (~18–22 nucleotides) that can regulate gene expression via specific complementary binding to target mRNA and result in degradation of mRNA (or perfect binding) or translational deletion (imperfect binding), although such silencing of mRNA expression can be reversed [40]. In addition, miRNAs are involved in post-transcriptional regulation associated with cell proliferation, differentiation and death and carcinogenesis. Circulating miRNAs are stable in body fluids, and serum levels of some miRNAs are altered under certain pathophysiological conditions, which make them excellent non-invasive biomarkers for monitoring the progression of liver disease. As a result, they can identify early and non-invasive patients at greater risk.
miR-122 is a liver-specific miRNA found in the circulation, especially in exosomes, when there is liver damage. A recent study has demonstrated that miR-122 expression is increased in NASH patients compared to patients with simple steatosis and a close correlation between miR-122 concentration and histological degree of disease severity [41]. The authors have also shown an association between serum levels of miR-122 and NAFLD Activity Score (NAS) in addition to the presence of hepatocyte balloonisation and advanced fibrosis as well as a strong correlation between miR-122 and liver enzymes [41]. miR-122 has been shown to be a better biomarker than Cytokeratin 18 (CK-18), aspartate aminotransferase (AST), or alanine aminotransferase (ALT), (biomarkers used in clinical practice to indicate presence of liver disease) to predict patients with NASH and fibrosis in this population. However, this difference in transaminases is subtle, and at NAS scores above 5, miR-122 and hepatic enzymes have the same predictive capacity [34]. On the other hand, few studies have demonstrated the role of miR-122 expression in HCC from NASH patients. Some years ago, Takaki et al. (2014) suggested experimentally and in liver tissue that silencing of miR-122 is an early event during hepatic carcinogenesis related to NASH, and miR-122 could be a novel molecular marker for evaluating the risk of HCC in patients with NASH [42]. More recently, in NAFLD patients, Akuta et al. (2016) demonstrated that HCC and/or histological components of NASH affected serum miR-122 levels independently. In longitudinal evaluations by these authors, serum miR-122 levels had already tended to decrease before the progression of the fibrosis stage [43]. However, on the contrary, our group studying 84 miRNAs expression using Liver miFinder miRNA PCR Array (QIAGEN) in all stages of NAFLD progression, including NASH/HCC (n = 5), identified higher levels of miR-122-5p in the progression of NAFLD, including NASH/HCC compared to other patients, suggesting that these miRNAs were modulated during transition from NASH to HCC. In addition, we identified in this study that miR-375 and miR-29a-3p are associated with miR-122-5p as novel molecular pathways for therapeutic intervention (unpublished data). Interestingly and similarly to our study, An et al. (2018) studying 84 cases of HCC from diverse causes identified that miR-375, miR-10a, miR-122 and miR-423 were significantly higher in HCC than in controls and suggested a novel serum microRNA panel for the diagnostic and prognostic implications of hepatocellular carcinoma [44].
Recently, miR-155, which is a direct regulator of the inflammatory cytokine TNF-α, has been associated with inflammation. miRNA-155 has important function in the early stages of choline-deficient and amino-defined (CDAA) hepatic carcinogenesis. Wang et al., 2009 demonstrated that the activation of CDAA-induced NF-κB increased the hepatic expression of miRNA-155, resulting in the induction of growth of Hep3B and HepG2 cells and the depletion of endogenous miRNA-155 inhibited cell growth SNU-182. Recently, Tessitore et al. (2016) described in animal a model of HCC-NASH, nine overexpressed miRNAs in tumours (miR-155, miR-193b, miR-27a, miR-31, miR-99b, miR-484, miR-574-3p, miR-125a-5p, and miR-182) and five downregulated miRNAs (miR-20a, miR-200c, miR-93, miR-340-5p, and miR-720) with respect to non-tumour tissues [45]. Interestingly, another miRNA, miR-375, is a key molecule for the regulation of glycaemic homeostasis and can inhibit glucose-induced insulin secretion, while elimination of miR-375 may increase insulin secretion [41]. A study by Pirola et al. (2015) demonstrated overexpression of miR-375, which was significantly associated with degree of histological severity, with degree of cellular balloonization and NAS [41].
Other miRNAs have been described in NAFLD. miR-34a is one of the most lipid-related liver miRNAs and its expression is closely related to the severity of NASH, since its overexpression results in apoptosis of hepatocytes. The main target of miR-34a is the NAD-dependent deacetylase Sirtuin-1 (SIRT1), which plays a key role in energy homeostasis by activating important transcription factors such as peroxisome proliferator-activated receptor alpha (PPARα) and liver X receptor (LXR). The silencing of miR-34a promotes the expression of SIRT1 and PPARα, resulting in the activation of AMP-activated protein kinase (AMPK) and the activation of numerous target genes of PPARα, suggesting that miR-34a functions in the deregulation of lipid metabolism associated with NAFLD [46]. Although it is not known exactly how the mechanism of action of miR-34a influences the development of NAFLD, studies have shown its dysregulation in this disease. In 2016, Xiao-Lin Liu et al. analysed the viability of miR-34a as a diagnostic marker of NASH. In this study, they identified a correlation between the serum concentrations of miR-34a, miR-122 and miR-192 and hepatic steatosis and inflammatory activity. In addition, miR-34a presented a higher correlation with lobular inflammation, and miR-122 presented a greater association with hepatocellular balloonization [47]. However, Bharali et al. (2018) demonstrated an inverse correlation between HCC expression and miR-34; nevertheless, the HCC samples were from hepatitis B [48]. Additionally, Zhou et al. (2018) demonstrated in HCC tissues and cells that miR-34a inhibits HCC progression by repressing hexokinase-1 [49]. Nevertheless, there are few studies on HCC secondary to NAFLD.
Recently, in high fat diet (HFD)-treated mice and human HepG2 cells incubated with FA, Wu et al. (2016) identified a novel mechanism by which miR-21, in part, promotes hepatic lipid accumulation and cancer progression by interacting with the Hbp1-p53-Srebp1c pathway and suggests the potential therapeutic value of miR-21 for both disorders [50].
Early Detection and Screening in NASH-Related HCC
The need for a surveillance programme in patients at risk has become imperative in current times for the early detection of HCC. The screening is based on the application of a sensitive test in a repeated way and in an at-risk population, in this case, patients with cirrhosis. HCC is a disease with curative treatments increasingly available for early lesions, such as hepatic resection, liver transplantation and percutaneous ablative treatments. In addition, it can be detected by a single exam that is effective, non-invasive and low cost: ultrasonography (US) of abdomen. The primary objective of the surveillance programme is to reduce mortality or survival analysis. In terms of scientific evidence, there are three randomized controlled trials on HCC surveillance [51,52,53], and the benefits of regular surveillance schemes with US were analysed, showing that even with a certain heterogeneity of methodology, stages and aetiologies and with verifying the results in the same way, the increase in saved lives remained [54,55,56,57,58,59,60,61,62]. Each of the recent HCC guidelines of liver cancer societies in Europe, the United States and Asia, such as EASL, AASLD 2018 and APASL 2017, shows particularities. There are recommendations for HCC surveillance with evidence scores and recommendations ranging from moderate to strong. These societies agree with each other and strongly recommend HCC surveillance in at-risk populations and a surveillance time of 6 month intervals through US [63,64,65]. The European Liver Study Society encourages vigilance and strongly recommends such issues as the importance of implementing surveillance programmes for HCC, criteria for HCC risk populations, particularities about the population with NAFLD, use of expert US, research of new biomarkers and cases of patients on transplant lists. Among the six strong recommendations, we emphasize that patients at high risk for HCC (cirrhotic) should participate in the surveillance programme, but the role of patients with NAFLD but without cirrhosis is still unknown. It is estimated that half of the cases with NASH and CHC occur in non-cirrhotic patients [66]. However, the incidence of CHC in these patients with non-advanced fibrosis is expected to be low to warrant universal vigilance, given the high prevalence of NAFLD in the general population. They point out that risky patients in the future can be identified and categorized as those that should and should not be monitored for HCC. Remember that the obesity of these patients is another challenge for US. Other radiological methods, such as CT or MRI, are available, but in this case, the surveillance programme would not be cost-effective. These European experts stress that the surveillance programme is vital and necessary as a medical intervention because it is cost-effective and promotes an increase in life expectancy of 3 months, costing less than approximately $50,000 per year of life saved [67]. In addition, the EASL demonstrates that in a scenario of CHC incidence greater than or equal to 1.5% per year, it is cost-effective regardless of the aetiology or the use of US and is sufficiently sensitive for tumour detection every 6 months [68, 69]. It is interesting to highlight some factors related to high risk of severe fibrosis or cirrhosis and occurrence of HCC, such as T2DM, advanced age and alcohol consumption. In addition, simple laboratory scores help identify patients with a higher risk of severe fibrosis and guarantee a greater depth of evaluation. Of particular note are the studies of genetic factors of PNPLA variants of rs738409 associated with the development of CHC in obese individuals [52, 53]. In addition, in the particular case of NAFLD, they recommend that patients with MtS or NASH identified with severe fibrosis or cirrhosis by histology or elastography should perform vigilance. EASL proposes an elaborate and compact investigation algorithm based on the size of the lesion detected by ultrasound from 1 (a) cm, in such a way as to minimize false positive results and additional costs. Such an algorithm design has been consistently validated.
Some years ago, our group published a series of NAFLD-related HCCs that exemplifies the importance of the discovery of new biomarkers for non-cirrhotic NAFLD in this context, because evaluating the applicability of the Barcelona Clinical Liver Cancer (BCLC) staging system in 42 cases of HCC secondary to NAFLD or cryptogenic cirrhosis (CC) only 52% of patients had real curative treatment according to BCLC. Additionally, HCC was diagnosed in a screening programme in 55% of the 42 patients (there was 1 non-cirrhotic patient), while patients with HCC diagnosed outside of a surveillance programme (n = 19) were mostly not candidates for curative therapy (73%) [18].
On the other hand, the American Society of Liver Studies (AASLD 2018) currently recommends the HCC surveillance programme in cirrhotic patients justified by the increased survival of these patients demonstrated by the same work by Zhang et al. [52]. In this new American guideline, it can be seen that the AASLD does not manifest itself on surveillance in populations with NAFLD, even with a growing incidence in that country. In addition, a surveillance method allow for the option of US with or without the concomitant use of alpha-fetoprotein (AFP). The AASLD does not comment on the existing cost-effective works of the programme, which could justify its recommendations. Regarding the last APASL 2017 guideline, this Japanese society with the world’s largest HCC surveillance programme favours all cirrhotic viral aetiologies even after treatment with antiviral drugs in cases of HCV. The recommendation of the programme is based on US examination and serum AFP, which is supported by moderate but scant evidence. Interestingly, HCC surveillance in East Asia recommends simultaneous use of US and AFP (but from a serum level above 200 IU), arguing that in these values, there is an increase in true positive results, resulting in less “recall” and greater efficiency of the programme.
In other words, there are currently no guidelines for the screening and early detection of NAFLD-related HCC in the absence of cirrhosis. However, there is an increasing number of HCC cases without cirrhosis. Thus, there is a strong interest in identifying biomarkers to detect early detection of HCC risk related to NAFLD progression.
In recent years, our group has been studying early detection of HCC in animal models. Because the early detection of focal hepatic lesions using US scanning is challenging and this challenge becomes even greater in the presence of diffuse parenchymal disease, we demonstrated the early detection of hepatocellular lesions in an experimental rat model of NASH with elastography and contrast-enhanced ultrasonography (CEUS). Both techniques allowed for the correct diagnosis of well-differentiated to moderately-differentiated HCC with good accuracy in an experimental rat model of NASH [70]. More recently, we demonstrated that 18F-FDG PET/CT was able to non-invasively evaluate the development of HCC in an experimental model of NAFLD. From the standardization of PET/CT in this model, it is possible to use this tool in future studies to monitor the progression of HCC non-invasively in vivo [71].
References
Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153–6.
Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004;127:S5–S16.
Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2016;2:16018.
Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74–80.
Duan XY, Qiao L, Fan JG. Clinical features of nonalcoholic fatty liver disease-associated hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2012;11:18–27.
Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59:2188–95.
Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148:547–55.
Cheung O, Sanyal AJ. Recent advances in nonalcoholic fatty liver disease. Curr Opin Gastroenterol. 2010;26:202–8.
Ertle J, Dechêne A, Sowa JP, Penndorf V, Herzer K, Kaiser G, et al. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int J Cancer. 2011;128:2436–43.
Simonetti RG, Cammà C, Fiorello F, Politi F, D’Amico G, Pagliaro L. Hepatocellular carcinoma. A worldwide problem and the major risk factors. Dig Dis Sci. 1991;36:962–72.
Kawada N, Imanaka K, Kawaguchi T, Tamai C, Ishihara R, Matsunaga T, et al. Hepatocellular carcinoma arising from non-cirrhotic nonalcoholic steatohepatitis. J Gastroenterol. 2009;44:1190–4.
Chagas AL, Kikuchi LO, Oliveira CP, Vezozzo DC, Mello ES, Oliveira AC, et al. Does hepatocellular carcinoma in non-alcoholic steatohepatitis exist in cirrhotic and non-cirrhotic patients? Braz J Med Biol Res. 2009;42:958–62.
Kikuchi L, Oliveira CP, Alvares-da-Silva MR, Tani CM, Diniz MA, Stefano JT, et al. Hepatocellular carcinoma management in nonalcoholic fatty liver disease patients applicability of the BCLC staging system. Am J Clin Oncol Cancer Clin Trials. 2016;39:428–32.
Mikuriya Y, Tashiro H, Kobayashi T, Kuroda S, Abe T, Hashimoto M, et al. Clinicopathological features of hepatocellular carcinoma in patients with nonalcoholic fatty liver disease. Langenbeck's Arch Surg. 2015;400:471–6.
Leung C, Yeoh SW, Patrick D, Ket S, Marion K, Gow P, et al. Characteristics of hepatocellular carcinoma in cirrhotic and non-cirrhotic non-alcoholic fatty liver disease. World J Gastroenterol. 2015;21:1189–96.
Mittal S, El-Serag HB, Sada YH, Kanwal F, Duan Z, Temple S, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States Veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14:124–131.e121.
Cotrim HP, Oliveira CP, Coelho HS, Alvares-da-Silva MR, Nabuco L, Parise ER, et al. Nonalcoholic steatohepatitis and hepatocellular carcinoma: Brazilian survey. Clinics (Sao Paulo). 2016;71:281–4.
Kikuchi L, Oliveira CP, Carrilho FJ. Nonalcoholic fatty liver disease and hepatocellular carcinoma. Biomed Res Int. 2014;2014:106247.
Caldwell SH, Crespo DM, Kang HS, Al-Osaimi AM. Obesity and hepatocellular carcinoma. Gastroenterology. 2004;127:S97–103.
Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–5.
Ascha MS, Hanouneh IA, Lopez R, Tamimi TA, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972–8.
Jimba S, Nakagami T, Takahashi M, Wakamatsu T, Hirota Y, Iwamoto Y, et al. Prevalence of non-alcoholic fatty liver disease and its association with impaired glucose metabolism in Japanese adults. Diabet Med. 2005;22:1141–5.
Hashizume H, Sato K, Takagi H, Hirokawa T, Kojima A, Sohara N, et al. Primary liver cancers with nonalcoholic steatohepatitis. Eur J Gastroenterol Hepatol. 2007;19:827–34.
Park EJ, Lee JH, Yu GY, He G, Ali SR, Holzer RG, et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell. 2010;140:197–208.
Starley BQ, Calcagno CJ, Harrison SA. Nonalcoholic fatty liver disease and hepatocellular carcinoma: a weighty connection. Hepatology. 2010;51:1820–32.
Wong CR, Nguyen MH, Lim JK. Hepatocellular carcinoma in patients with non-alcoholic fatty liver disease. World J Gastroenterol. 2016;22:8294–303.
Hu W, Feng Z, Eveleigh J, Iyer G, Pan J, Amin S, et al. The major lipid peroxidation product, trans-4-hydroxy-2-nonenal, preferentially forms DNA adducts at codon 249 of human p53 gene, a unique mutational hotspot in hepatocellular carcinoma. Carcinogenesis. 2002;23:1781–9.
Xu Z, Chen L, Leung L, Yen TS, Lee C, Chan JY. Liver-specific inactivation of the Nrf1 gene in adult mouse leads to nonalcoholic steatohepatitis and hepatic neoplasia. Proc Natl Acad Sci U S A. 2005;102:4120–5.
Hashimoto E, Tokushige K. Hepatocellular carcinoma in non-alcoholic steatohepatitis: growing evidence of an epidemic? Hepatol Res. 2012;42:1–14.
Machado MV, Diehl AM. Pathogenesis of nonalcoholic steatohepatitis. Gastroenterology. 2016;150:1769–77.
Ma C, Kesarwala AH, Eggert T, Medina-Echeverz J, Kleiner DE, Jin P, et al. NAFLD causes selective CD4(+) T lymphocyte loss and promotes hepatocarcinogenesis. Nature. 2016;531:253–7.
Wolf MJ, Adili A, Piotrowitz K, Abdullah Z, Boege Y, Stemmer K, et al. Metabolic activation of intrahepatic CD8+ T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell. 2014;26:549–64.
Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–5.
Afonso MB, Rodrigues PM, Simão AL, Castro RE. Circulating microRNAs as potential biomarkers in non-alcoholic fatty liver disease and hepatocellular carcinoma. J Clin Med. 2016;5:30.
Wruck W, Graffmann N, Kawala MA, Adjaye J. Concise review: current status and future directions on research related to nonalcoholic fatty liver disease. Stem Cells. 2017;35:89–96.
Jiang X, Zhang F. Long noncoding RNA: a new contributor and potential therapeutic target in fibrosis. Epigenomics. 2017;9:1233–41.
Turchinovich A, Baranova A, Drapkina O, Tonevitsky A. Cell-free circulating nucleic acids as early biomarkers for NAFLD and NAFLD-associated disorders. Front Physiol. 2018;9:1256.
Yamamura S, Imai-Sumida M, Tanaka Y, Dahiya R. Interaction and cross-talk between non-coding RNAs. Cell Mol Life Sci. 2018;75:467–84.
O’Brien J, Hayder H, Zayed Y, Peng C. Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne). 2018;9:402.
Vishnoi A, Rani S. MiRNA biogenesis and regulation of diseases: an overview. Methods Mol Biol. 2017;1509:1–10.
Pirola CJ, Fernández Gianotti T, Castaño GO, Mallardi P, San Martino J, Mora Gonzalez Lopez Ledesma M, et al. Circulating microRNA signature in non-alcoholic fatty liver disease: from serum non-coding RNAs to liver histology and disease pathogenesis. Gut. 2015;64:800–12.
Takaki Y, Saito Y, Takasugi A, Toshimitsu K, Yamada S, Muramatsu T, et al. Silencing of microRNA-122 is an early event during hepatocarcinogenesis from non-alcoholic steatohepatitis. Cancer Sci. 2014;105:1254–60.
Akuta N, Kawamura Y, Suzuki F, Saitoh S, Arase Y, Kunimoto H, et al. Impact of circulating miR-122 for histological features and hepatocellular carcinoma of nonalcoholic fatty liver disease in Japan. Hepatol Int. 2016;10:647–56.
An Y, Gao S, Zhao WC, Qiu BA, Xia NX, Zhang PJ, et al. Novel serum microRNAs panel on the diagnostic and prognostic implications of hepatocellular carcinoma. World J Gastroenterol. 2018;24:2596–604.
Tessitore A, Cicciarelli G, Del Vecchio F, Gaggiano A, Verzella D, Fischietti M, et al. MicroRNA expression analysis in high fat diet-induced NAFLD-NASH-HCC progression: study on C57BL/6J mice. BMC Cancer. 2016;16:3.
Baffy G. MicroRNAs in nonalcoholic fatty liver disease. J Clin Med. 2015;4:1977–88.
Liu XL, Pan Q, Zhang RN, Shen F, Yan SY, Sun C, et al. Disease-specific miR-34a as diagnostic marker of non-alcoholic steatohepatitis in a Chinese population. World J Gastroenterol. 2016;22:9844–52.
Bharali D, Jebur HB, Baishya D, Kumar S, Sarma MP, Masroor M, et al. Expression analysis of serum microRNA-34a and microRNA-183 in hepatocellular carcinoma. Asian Pac J Cancer Prev. 2018;19:2561–8.
Zhou Y, Liu K, Liu Y, Tan L. MicroRNA-34a inhibit hepatocellular carcinoma progression by repressing hexokinase-1. J Cell Biochem. 2019;120:7147–53.
Wu H, Ng R, Chen X, Steer CJ, Song G. MicroRNA-21 is a potential link between non-alcoholic fatty liver disease and hepatocellular carcinoma via modulation of the HBP1-p53-Srebp1c pathway. Gut. 2016;65:1850–60.
Chen JG, Parkin DM, Chen QG, Lu JH, Shen QJ, Zhang BC, et al. Screening for liver cancer: results of a randomised controlled trial in Qidong, China. J Med Screen. 2003;10:204–9.
Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417–22.
Yang B, Zhang B, Xu Y, Wang W, Shen Y, Zhang A, et al. Prospective study of early detection for primary liver cancer. J Cancer Res Clin Oncol. 1997;123:357–60.
Trevisani F, Santi V, Gramenzi A, Di Nolfo MA, Del Poggio P, Benvegnù L, et al. Surveillance for early diagnosis of hepatocellular carcinoma: is it effective in intermediate/advanced cirrhosis? Am J Gastroenterol. 2007;102:2448–57; quiz 2458.
Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MA, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30:37–47.
Barbara L, Benzi G, Gaiani S, Fusconi F, Zironi G, Siringo S, et al. Natural history of small untreated hepatocellular carcinoma in cirrhosis: a multivariate analysis of prognostic factors of tumor growth rate and patient survival. Hepatology. 1992;16:132–7.
Ebara M, Ohto M, Shinagawa T, Sugiura N, Kimura K, Matsutani S, et al. Natural history of minute hepatocellular carcinoma smaller than three centimeters complicating cirrhosis. A study in 22 patients. Gastroenterology. 1986;90:289–98.
Sheu JC, Sung JL, Chen DS, Yang PM, Lai MY, Lee CS, et al. Growth rate of asymptomatic hepatocellular carcinoma and its clinical implications. Gastroenterology. 1985;89:259–66.
Makuuchi M, Kokudo N, Arii S, Futagawa S, Kaneko S, Kawasaki S, et al. Development of evidence-based clinical guidelines for the diagnosis and treatment of hepatocellular carcinoma in Japan. Hepatol Res. 2008;38:37–51.
Trinchet JC, Chaffaut C, Bourcier V, Degos F, Henrion J, Fontaine H, et al. Ultrasonographic surveillance of hepatocellular carcinoma in cirrhosis: a randomized trial comparing 3- and 6-month periodicities. Hepatology. 2011;54:1987–97.
Santagostino E, Colombo M, Rivi M, Rumi MG, Rocino A, Linari S, et al. A 6-month versus a 12-month surveillance for hepatocellular carcinoma in 559 hemophiliacs infected with the hepatitis C virus. Blood. 2003;102:78–82.
Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al. Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis. Health Technol Assess. 2007;11:1–206.
easloffice@easloffice.eu EAftSotLEa, Liver EAftSot. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358–80.
Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11:317–70.
Piscaglia F, Svegliati-Baroni G, Barchetti A, Pecorelli A, Marinelli S, Tiribelli C, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: a multicenter prospective study. Hepatology. 2016;63:827–38.
Laupacis A, Feeny D, Detsky AS, Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992;146:473–81.
Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis. Am J Med. 1996;101:422–34.
Andersson KL, Salomon JA, Goldie SJ, Chung RT. Cost effectiveness of alternative surveillance strategies for hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2008;6:1418–24.
Carvalho CF, Chammas MC, Souza de Oliveira CP, Cogliati B, Carrilho FJ, Cerri GG. Elastography and contrast-enhanced ultrasonography in the early detection of hepatocellular carcinoma in an experimental model of nonalcoholic steatohepatitis. J Clin Exp Hepatol. 2013;3:96–101.
Levy CS, Costa FGB, Faria DP, Stefano JT, Cogliati B, Oliveira CP. 18F-FDG PET/CT as an assessment tool of hepatocellular carcinoma secondary to non-alcoholic fatty liver disease development in experimental model. Arq Gastroenterol. 2019;56(1):45–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stefano, J.T. et al. (2020). HCC in Patients with NAFLD/NASH. In: Romero-Gomez, M. (eds) NAFLD and NASH. Springer, Cham. https://doi.org/10.1007/978-3-030-37173-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-37173-9_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-37172-2
Online ISBN: 978-3-030-37173-9
eBook Packages: MedicineMedicine (R0)