Abstract
Regional anesthetic and analgesic techniques represent the cornerstones of orthopedic anesthesia; their development and advancement have established new possibilities and have allowed orthopedic surgery to become more available to more patients with comorbidities. While widely used at the Hospital for Special Surgery, variations of regional anesthetic approaches have to be tailored to individual patient comorbidities, preferences, anatomic variations, as well as surgical cofactors. In this chapter we discuss how regional anesthesia can provide focused and sustained pain relief for patients undergoing orthopedic surgery. We further elaborate on how the choice of specific anesthetics and techniques plays a key role in the successful conduct of regional anesthesia. Despite its benefits, the possibility of complications and contraindications must be kept in mind in order to minimize potential harm.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anesthetic techniques
- Analgesic techniques
- Regional anesthesia
- Techniques
- Complications
- Contraindications
-
To introduce the rationale for the choice of specific anesthetics and techniques.
-
To discuss frequently encountered contraindications and complications of regional anesthesia.
-
To describe techniques used to perform various regional anesthetics.
-
To provide an overview of the use of anesthetics for specific orthopedic procedures.
-
Many different local anesthetics with various effect profiles are available for the practice of regional anesthesia, as well as a number of additives. Main considerations in choosing the appropriate agent are dosage/volume, speed of onset, duration, and side effects.
-
Absolute or relative contraindications include infection, coagulation disorders, and preexisting neurologic deficits. Among the potential hazards of regional anesthesia are local anesthetic systemic toxicity and neuropathy.
-
Four methods to determine the right injection sites have been developed over time: anatomic landmarks, the paresthesia technique, electric nerve stimulation, and ultrasound guidance. The insertion of catheters allows for a prolonged period of regional anesthesia or analgesia.
-
Numerous block techniques can be carried out to provide anesthesia to different body parts. For the upper extremity, several approaches to anesthetize the brachial plexus have been described, including interscalene, supraclavicular, infraclavicular, and axillary blocks. Apart from neuraxial anesthesia, lumbar plexus block, femoral nerve block, saphenous nerve block, popliteal nerve block, and ankle block are among the techniques available for the lower extremity.
Introduction
The practice of anesthesia at the Hospital for Special Surgery is primarily one of regional anesthesia (RA) techniques. Regional anesthesia—whether neuraxial (spinal, epidural) or peripheral nerve blocks—can decrease the stress response to surgery and, as such, is considered beneficial in the perioperative period. Neuraxial anesthesia is associated with decreases in (early) mortality, deep vein thrombosis/pulmonary embolism, myocardial infarctions, respiratory morbidity, and postoperative confusion. Peripheral nerve blocks (PNB) are associated with improved rehabilitation and reduced length of hospital stay. The safe and successful practice of regional anesthesia relies on anesthetizing nerves without damaging their structure. Disruption of the nerve structure or the surrounding tissue architecture with the needle can cause undesirable neurological consequences. Anesthesiologists trained in regional anesthesia achieve this goal by relying on anatomical landmarks, the patient’s feedback, and the use of nerve stimulators or ultrasonography to locate the targeted nerves. This chapter introduces the reader to the practice of regional anesthesia at a single institution—it is neither meant to be all inclusive or to provide a detailed “cookbook” approach to regional anesthesia—rather it is meant to provide an overview of its use at the Hospital for Special Surgery. Specific attention will be paid to the presentation of various techniques used for a variety of orthopedic procedures while discussing (1) the choice of local anesthetic, (2) the contraindications for the use of regional anesthesia, (3) the complications and side effects associated with regional anesthetics, (4) the performance and indications for various peripheral nerve blocks and neuraxial techniques, and (5) the utilization of techniques in the setting of specific orthopedic surgeries as practiced at the Hospital for Special Surgery.
Local Anesthetics
Choice of Local Anesthetic
Medium- and long-acting amide local anesthetics (LAs) are most frequently used to achieve peripheral nerve blockade, whether for surgical anesthesia or for postoperative analgesia. The choice of LA is dependent upon a number of factors, including speed of onset, duration of surgery, toxicity profile, and patient comorbidities. In general, at our institution, medium-acting LAs, such as mepivacaine, are used for cases of relatively short duration (<2 h) and long-acting LAs, such as bupivacaine, are used for cases of longer duration (>2 h). In the case of peripheral nerve blockade, the choice to use longer-acting LAs depends on the desired prolonged length of postoperative analgesia. Please refer to Table 8.1 for a summary on characteristics of different local anesthetics in peripheral nerve blocks and epidural and spinal anesthesia.
Drug Dosage
Depending on age and comorbidities, in general, a volume of 30–50 ml of a number of commercially available LAs can be used to anesthetize peripheral nerves close to the trunk in an average-sized adult. The doses of different types of anesthetics are shown in Table 8.1 [1].
Latency
The latency to block onset can be decreased by (1) carbonization of the local anesthetic, (2) alkalinization of the LA, and (3) warming of the LA. A fourth option to hasten block onset of shorter-acting LA includes the use of higher volumes and has become common practice at the Hospital for Special Surgery, where anesthetic blocks are performed in the operating room with surgery following in short order, allowing limited time for block onset.
Adjuvants
Different medications have been used as adjuvants to LA in peripheral nerve blocks with the goal to either enhance or prolong the effect of a block. Possible adjuvants include epinephrine, dexamethasone, ketamine, neostigmine, opioids, and clonidine. In general, the practice at HSS includes the use of epinephrine, clonidine, or dexamethasone to increase the duration of peripheral nerve blocks.
Contraindications for the Use of Regional Anesthesia
Infection
Infection at the needle puncture site is an absolute contraindication to the use of any type of regional anesthetic [2]. Bacteremia or infection in the region to be blocked is not absolute, but rather relative contraindications to the use of regional anesthesia or peripheral nerve blocks—after weighing the overall risks and benefits of the use of either neuraxial or peripheral nerve block. Conservative practice dictates that indwelling catheters should be avoided in the setting of infection, unless the patient has begun a course of antibiotics. It should be noted that, in the case of neuraxial anesthesia without indwelling catheter, where infection without signs of systemic involvement is present, the risk of bacterial spread to the neuraxial space is probably low [3]. Indeed, in a series of almost 500 patients presenting for surgical treatment of an infected joint and in whom a neuraxial anesthetic was performed, no cases of meningitis or epidural abscess were encountered at our institution [4].
Coagulation Disorders
Problems with coagulation, whether iatrogenic or pathologic, remain a relative contraindication to the use of regional anesthesia or peripheral nerve blockade. The American Society of Regional Anesthesia and Pain Medicine (ASRA) provides recommendations and practice guidelines on this topic [5]. This is especially important in the setting of newer anticoagulants which carry broad indications for use (atrial fibrillation, DVT, etc.). Details on regional anesthesia in the setting of anticoagulant are frequently updated and should be followed closely [6].
Preexisting Neurological Deficits
Previous neurological disease or peripheral nerve injuries of either acute or chronic nature are not absolute contraindications to the use of regional anesthesia or peripheral nerve blockade. Some evidence suggests, however, that preexisting neurologic abnormalities may increase the risk of anesthesia-related neuropathies after neuraxial anesthesia [7]. Therefore, given the obvious advantages of regional anesthesia, the risks and benefits should be carefully weighed, and thorough documentation should be performed before an anesthetic is performed. In general, due to the conservative nature of the practice of regional anesthesia at HSS, we do not perform peripheral nerve blocks in the setting of preexisting neurological deficits.
Complications and Side Effects Associated with Regional Anesthesia
Local Anesthetic Systemic Toxicity
Local anesthetic systemic toxicity (LAST) is a relatively rare but a potentially life-threatening complication of regional anesthesia. It can range from neurological symptoms to cardiovascular collapse. While the pathophysiology of LAST is not fully clear, there is evidence that some of its mechanisms relate to the drugs’ sodium channel blocking activity. Local anesthetic agents readily bind to voltage-gated sodium channels and decrease transmembrane sodium flux, thus impairing depolarization and producing the desired anesthetic action when applied to peripheral nerves. Depending on concentration they also interact with a multitude of other ion channels, drug receptors, and enzymes. In the central nervous and cardiac tissues, where the local anesthetic is redistributed to in a dose-dependent manner after adsorption, a number of unfavorable side effects can occur. In the brain, disruptions of inhibitory and excitatory circuits evoke either seizure activity or cerebral depression and coma. Cardiac toxicity comprises mainly impairment of contractility and generation of arrhythmias, for which different mechanisms are thought to play a role [8]. In general, LA agents have variable side effect profiles. Longer-acting LAs like bupivacaine and ropivacaine are reportedly more prone to produce cardiac toxicity even at low doses; further, they rather affect conductance than myocyte contractility, resulting in sustained arrhythmias. On the contrary, shorter-acting LAs like lidocaine and prilocaine have a higher central nervous system to cardiac toxicity ratio and in the latter organ predominantly affect cardiac contractility. The optimal treatment for LAST might therefore not only depend on the predominant site of toxicity but also on the type of LA involved [9]. According to the ASRA practice advisory, airway management and prevention of hypoxia and acidosis are among the most crucial first steps to treatment [10]. Both cardiac and central nervous system toxicities have been successfully treated with the use of Intralipid® (Fresenius Kabi AB, Uppsala, Sweden) [11]. It is the currently recommended treatment for all cases of LAST except minor central nervous system toxicity [12]. It is thought that Intralipid will extract lipophilic LA from the plasma, thus reducing concentrations and its effect on neurons and cardiac cells. Other treatment options include benzodiazepines to terminate seizures; positive inotropic support with epinephrine, which is believed to be particularly beneficial where LAs are causing myocardial depression; or, as a last resort, intermittent maintenance on cardiac bypass. At the Hospital for Special Surgery, Intralipid® (and an algorithm for its use) is easily accessible at all anesthetizing locations where regional anesthesia is performed.
Neuropathy/Neurological Injury
Prevention and education are the keys to management of neurologic injury. Nerve injury from anesthetic sources is very rare and often multifactorial [13]. A careful and considered discussion of the risks and benefits relating to neurological injury and their incidence should involve every patient to be anesthetized [14]. There are often situations (i.e., professional athletes and dancers) in which even the potential for risk of injury makes regional anesthesia an unacceptable choice.
Regional Anesthesia Techniques
Anatomical Landmarks
Anatomic landmarks were the original means of guiding the location of injections for regional anesthesia. They are still used with marked success in certain situations (placement of spinals and epidurals, axillary nerve blocks, etc.). Increasingly, they are an adjunct to newer technologies for identification of neural structures (i.e., femoral artery palpation to guide placement of ultrasound probe), especially in situations involving the teaching of residents and fellows.
Paresthesia Techniques
Eliciting a paresthesia from probing of the needle is a time-tested technique—hence the dictum “no paresthesia, no anesthesia.” It is thought that the paresthesia develops when the tip of the needle comes in contact with the nerve. Theoretically, there is an increased risk of nerve damage (decreased margin of safety) when attempting to elicit paresthesias, and, as a result, its use has somewhat fallen out of favor. Further, utilizing a paresthesia technique requires the patient’s cooperation, which limits the level of sedation provided during block performance.
Nerve Stimulator
The nerve stimulator works on the principles of electrostimulation. A nerve stimulator discharges an electrical current that is transmitted through tissue structures via a needle. When the needle tip approaches the nerve, the electrical current causes a twitch of the muscle that is innervated by a particular nerve, providing localizing information to the anesthesiologist. Using this technique, the anesthesiologist can target specific nerves and deliver a dose of local anesthetic to anesthetize the surgical site. Nerve stimulation has been used to locate nerves for many years and is currently the most commonly utilized technique [15]. However, there are drawbacks to this technique, one of which is the inability to directly visualize the path of the needle as it passes through tissue.
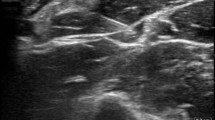
Ultrasound Guidance
Ultrasound-guided techniques were historically used to either diagnose side effects or avoid vascular puncture. They have more recently become the technique of choice for identifying nerves and their surrounding anatomy [16]. Ultrasonography helps visualize the targeted nerves and the needle as it moves through tissues and associated vital structures. It can also help determine the adequacy of spread of the local anesthetics around the nerves. Ultrasound imaging relies on the ability of tissue to reflect sound waves. Sound waves are emitted from the ultrasound probe into the tissue over which it is applied. These sound waves then reflect back toward the probe as they cross different areas of the body. The probe receives the reflected waves and an image is created on the screen of the ultrasound machine. The angle and intensity of the reflected sound waves transmitted through tissues determine the clarity of the picture. When using this technique, the anesthesiologist can visualize, in real time, the structures that he/she is looking for, pass the needle toward the targeted nerves, and avoid vital structures that may be in the way and avoid, for example, vascular puncture [17]. This ensures success of the block by confirming an adequate spread of the local anesthetic solution around the nerve. However, it must be noted that no data are available to suggest that using ultrasound decreases the risk of neuropraxias [18].
Catheter Techniques
Continuous nerve catheter techniques can be used for either intraoperative management (depending on surgical duration and postoperative pain plan) or postoperative pain management (severe postoperative pain, posttraumatic pain states, sympathetic blockade, amputation/stump pain, etc.). Different types of administration are available—intermittent bolus administration, continuous administration, or patient-controlled administration [19]. The method of choice for a given institution most often depends on organizational factors. Continuous peripheral catheters are frequently used at our institution for patients who cannot receive epidural analgesia when undergoing lower extremity arthroplasty. Further, patients with extensive foot reconstructions benefit from this approach, as the location of pain is difficult to control with neuraxial techniques.
Upper Extremity Nerve Blocks
The Brachial Plexus
There are four commonly used primary approaches to regional anesthesia of the brachial plexus: interscalene, supraclavicular, infraclavicular/coracoid, and axillary. Nerve stimulator and/or ultrasound approaches can be used for each of these blocks; however, at the Hospital for Special Surgery, ultrasound techniques are used primarily for interscalene, supraclavicular, and infraclavicular approaches, while nerve stimulator techniques are most commonly reserved as adjuncts and for teaching purposes.
Review of Anatomy
The brachial plexus is formed by the anterior rami of the C5–C8 and T1 spinal nerves. It contains a contribution from C4 in 60% and from T2 in nearly 30% of individuals. The roots of the spinal nerves exit from the spinal canal behind the vertebral artery and cross the transverse process of the corresponding vertebrae. They join to form three trunks and run together toward the first rib. The upper trunk arises from the union of the roots of C5/6, while the middle is comprised of the root of C7 and the lower of the roots of C8/T1. The trunks (which lie on top of each other) pass between the scalenus anterior and scalenus medius muscles in the interscalene groove. Just above the clavicle, the trunks divide into an anterior and posterior division. The three posterior divisions join to form the posterior cord, the anterior divisions of the upper and middle trunks form the lateral cord, and the medial cord is the continuation of the anterior division of the lower trunk. The cords lie close together in the infraclavicular region, surrounding the subclavian artery [20].
Interscalene Nerve Block
The interscalene nerve block (ISB) was first introduced by Winnie as a puncture site in the interscalene groove at the level of the cricoid cartilage and the sixth cervical vertebra, with the needle directed perpendicular to the skin [21]. It has been modified and revised multiple times since then. The block provides anesthesia and analgesia for both arthroscopic and open procedures of the shoulder and proximal upper arm. Its use can also be indicated for closed reduction of shoulder dislocations, physical therapy, or as a diagnostic tool in the evaluation or therapy of certain chronic pain syndromes (e.g., complex regional pain syndrome (CRPS)). Interscalene nerve blocks are contraindicated in certain situations, including contralateral phrenic nerve paresis, contralateral recurrent laryngeal nerve paresis, and severe chronic pulmonary obstructive disease. The reason for this is a high rate of temporary paralysis of the phrenic and/or recurrent nerve on the side of the block, thus exposing the patient to respiratory failure and upper airway obstruction [22,23,24]. Interscalene nerve blocks can also be associated with a number of complications, including vertebral artery injection (resulting in immediate seizure), local anesthetic toxicity, direct intrathecal or epidural injection (with subsequent high or total epidural or spinal), and even permanent quadriplegia [25]. Interscalene nerve blockade is achieved by injecting 15–40 ml of LA solution into the interscalene groove at the level of a line drawn laterally from the transverse process of C6 (the external jugular vein often overlies the intersection site). The site of injection can be localized via paresthesia, nerve stimulator, and/or ultrasound technique. If a paresthesia approach is used, sensory signs should be elicited before injection of LA solutions. The site can be superficial in many people. One should aim for a paresthesia of the hand or forearm, although a paresthesia of the shoulder—which does not necessarily reflect direct stimulation of the brachial plexus—may be sufficient for anesthesia needed for shoulder surgery. If a nerve stimulator technique is used, the brachial plexus in the interscalene groove should ideally contract the biceps (flexion at the elbow) before local anesthesia is deposited. If the brachial plexus is localized by using an ultrasound technique, one is classically looking for the “stop light” configuration of the C4, C5, and C6 nerve roots. Deposition of local anesthesia around these roots will achieve the desired surgical anesthesia. Smaller amounts (5 ml) of local anesthesia deposited around each nerve root have been found equally efficacious in achieving surgical anesthesia [26]. Regardless of the technique used, when the interscalene block is achieved, a catheter may be placed for those situations in which a prolonged block of the brachial plexus is desired (i.e., re-anastomosis of digits). The interscalene block of the brachial plexus can be performed with the arm at the patient’s side, and the risk of pneumothorax is remote. However, a pneumothorax should be considered if cough or chest pain is produced while exploring for the location of the brachial plexus. Phrenic nerve and/or recurrent laryngeal nerve block with associated ipsilateral hemiparesis of the diaphragm and laryngeal musculature are common side effects of the interscalene approach to the brachial plexus, but remain clinically irrelevant in the majority of cases [27]. Accidental epidural anesthesia and spinal anesthesia are also possible using this approach, and if local anesthesia is accidentally injected into the vertebral artery, convulsions are likely to follow. At HSS, the interscalene nerve block is used in conjunction with sedation for most arthroscopic and open procedures of the shoulder.
Supraclavicular Nerve Block
The supraclavicular nerve block (SNB) is used to provide anesthesia for surgery on the shoulder, arm, and even forearm. It is approached by paresthesia, nerve stimulator, or ultrasound techniques. This block’s popularity has increased with the recent introduction of ultrasound. Classically, a SNB is achieved by injecting 15–40 ml of LA at a point just behind the midpoint of the clavicle where the nerves cross the first rib. The midpoint of the clavicle can be confirmed by palpating the subclavian artery in thin individuals or by extending an imaginary straight line from the end of the external jugular vein. Paresthesias of the forearm or hand should be elicited before the injection of LA. Pneumothorax is the most common complication of SNB (about 1% incidence) [28], initially manifesting as cough, dyspnea, and pleuritic chest pain. Block of the phrenic nerve occurs frequently but generally does not cause clinically significant symptoms. Advantages of SNB are rapid onset and ability to perform the block with the arm in any position. Historically, the high risk of pneumothorax limited the use of SNB. The use of ultrasound has theoretically reduced the incidence of pneumothorax by allowing visualization of the supraclavicular artery and nerve and, just as importantly, visualization of the first rib, clavicle, and apex of the lung [29]. This permits localization of the nerves while avoiding needle puncture of the lung. Ultrasound approaches either use hydrodissection (advancement of the needle while injecting) of the classic “cluster of grapes” lying next to the artery or deposition of all local anesthesia at a “12 o’clock” position above and adjacent to the neural structures [30]. Nerve stimulation can be used as an adjunct to ultrasonography to confirm needle position by eliciting an appropriate contraction of the muscles supplied by the brachial plexus. SNB is used for most closed procedures of the shoulder in conjunction with sedation.
Infraclavicular Nerve (Coracoid) Block
Coracoid blocks are often used to provide anesthesia for surgery involving the arm, elbow, wrist, and hand. The introduction of ultrasonography has made blocking of the brachial plexus in this location relatively risk-free in comparison to earlier approaches [31]. Using the ultrasound probe, the subclavian artery is visualized medially to the coracoid process, and 5–7 ml of LA is deposited next to the medial, lateral, and posterior cords of the brachial plexus, which lie circumferential to the artery. Alternatively, a single injection of 20–30 ml LA posterior to the artery may be equally effective [32]. Appropriate visualization of surrounding tissues and control to where the needle is directed are keys to the success of this block.
Axillary Nerve Block
Use of the axillary nerve block for upper extremity surgery has decreased at the Hospital for Special Surgery concomitant with the increased use of ultrasound-guided infraclavicular nerve blocks. Both nerve blocks remain useful for operations involving the hand, wrist, forearm, and/or elbow; however, the newer ultrasonographic technology allows direct visualization of the nerve structures while avoiding the theoretical complications associated with the axillary nerve block. There remain two primary techniques—the perivascular “single-injection” technique and the transarterial technique [33]. The axillary block of the brachial plexus is achieved by injecting 25–40 ml of LA in the axillary sheath of the axilla. The nerves are anesthetized around the axillary artery. The primary “problem” with the axillary block is that significant anatomic variation exists. Individual septa may surround different nerves, necessitating multiple injections when compared to single injection approaches. In order to perform the block, the upper extremity is abducted to 90° and externally rotated, the axillary artery is palpated and traced back toward the axilla, and the needle is inserted just anterior to the vessel. Entrance of the needle into the axillary sheath transmits a “popping” sensation to the anesthesiologist’s fingers, and the needle transmits the pulsation of the artery. Paresthesias are useful but not mandatory for confirming correct placement of the needle. Digital pressure applied distal to the needle during and after injection should promote proximal flow of LA solutions, within the sheath toward the side, where the musculocutaneous nerve exits. Alternatively, one can transfix the axillary artery (aspirating on both sides of the artery before placement of local anesthesia) with the needle and deposit 10–15 ml of local anesthesia on either side of the vessel, theoretically within the confines of the axillary sheath.
Typically, a small cuff of LA is deposited in the subcutaneous tissues over the proximal medial aspect of the axilla during withdrawal of the needle to block the intercostobrachial nerve. The musculocutaneous nerve is sometimes not blocked because it leaves the sheath proximal to the point of injection. This nerve is important because it provides sensory innervations from the radial side of the forearm to the thenar eminence. It should be blocked as it emerges from between the elbow crease with 5–10 ml of LA. The axillary approach carries the lowest risk of pneumothorax, making it useful for outpatients undergoing surgery on the forearm and hand.
Extremity Nerve Blocks
The Lumbosacral Plexus
The lumbosacral plexus (lumbar, sacral, and pudendal plexus) is formed by a set of conjoining nerve roots that arise from the lower lumbar and sacral spinal nerves (T12–S5), passing communicating branches between each other. Together, they account for the sensory and motor support of the lower extremity.
Unlike in the upper extremity, it is not easily possible to provide anesthesia to the entirety of the lower extremity via one single injection or block. Combinations of various peripheral nerve blocks with or with neuraxial anesthesia are therefore frequently utilized.
Review of Anatomy
After assembling lateral to the intervertebral foramina, the lumbar plexus proceeds downward in the psoas compartment between the psoas major and quadratus lumborum muscles. Aside from short, direct muscular branches, six major nerves branch off: the iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, obturator, and femoral nerves. While the former three pierce the abdominal wall or psoas muscle, the latter exit the pelvis through the obturator foramen (obturator nerve) and the muscular lacuna underneath the inguinal ligament (femoral nerve), respectively. The lumbar plexus provides innervations to the anterior portions of the hip joint, groin, most regions of the anterior and medial thigh, as well as parts of the knee joint and medial lower leg.
The adjacent sacral plexus innervates posterior and lower portions of the leg through nerves and direct branches. Two branches are most relevant for blockade, the posterior cutaneous femoral and sciatic (containing common fibular and tibial) nerves, which leave the pelvis together through the greater sciatic foramen.
Lumbar Plexus Block
Different ways to anesthetize parts of the lumbar plexus have been described, including the psoas compartment and perivascular (3-in-1) blocks. For the psoas compartment block, a nerve stimulator needle is inserted 3 cm inferior and 5 cm lateral to the fourth lumbar spine, which is commonly located at the height of an imaginary line between the iliac crests. After contact with the fifth lumbar transverse process, the needle should be advanced in cephalad direction, sliding off the transverse process, until a quadriceps motor response can be seen. Complications of this technique include risk of intravascular, epidural, or subarachnoid injection and nerve damage [34]. The 3-in-1 block, in contrast, is based on the assumption that a large volume of local anesthetic injected into the femoral perineural sheath will migrate in lateral and cephalad directions, toward the lumbar plexus, or at least toward its terminal branches femoral, obturator, and lateral femoral cutaneous nerve, providing anesthesia to three peripheral nerves with only one injection (hence, 3-in-1 block). The reliability of this block is subject to controversy [35].
However, the nerves of the lumbar plexus do not fully cover the posterior hip, so neither of these blocks will provide full anesthesia for hip surgery; rather, they are often used in conjunction with either a spinal or epidural approach. A lumbar plexus block is sometimes performed at the Hospital for Special Surgery to help alleviate hip pain. It can be used alone or in combination with epidural anesthesia for postoperative pain control in patients after hip replacement surgery, open reduction and fixation of the femur, and closed reduction of the hip joint.
Saphenous Nerve Block
At the Hospital for Special Surgery, the saphenous nerve block is the nerve block most commonly used for surgeries of the knee and medial foot. It is most often anesthetized at the level of the adductor canal. The saphenous nerve is a sensory branch of the femoral nerve, responsible for sensation from the inner aspect of the knee to the inner aspect of the lower leg and foot. As a purely sensory nerve, its blockade is not associated with motor blockade. As such, it is often used in the outpatient setting when early rehabilitation/motor control of the knee (i.e., knee ligamentoplasty) is requested. The saphenous nerve can be localized in the subsartorial region with the ultrasound probe 7–10 cm above the medial epicondyle of the femur. It is located between the vastus medialis and the gracilis muscles, on the inner aspect of the thigh [36]. Ten to fifteen milliliters of LA is deposited in this space to achieve blockade.
IPACK Block
At the Hospital for Special Surgery, local infiltration between the popliteal artery and capsule of the knee (IPACK) block is often used to provide analgesia for knee operations with a component of posterior knee surgical pain. Using ultrasound, the IPACK block targets the articular branches of the tibial, common peroneal, and obturator nerves in the popliteal region, allowing for analgesia by controlling posterior knee pain following knee surgery. Because the block is done under ultrasound visualization, it is associated with a very low incidence of nerve injury, arterial injury, and foot drop.
Femoral Nerve Block
At the Hospital for Special Surgery, the femoral nerve block is also used for surgeries of the knee and medial foot. However, concerns relating to its potential for prolonged motor blockade and subsequent delayed rehabilitation have seen the femoral nerve block fall out of favor. The femoral nerve is blocked by the injection of 20–30 ml of LA immediately laterally to the femoral artery, just below the midpoint of the inguinal ligament. A line drawn from the anterior superior iliac spine to the symphysis pubis will approximate the ligament. The block itself can be performed by using anatomic landmarks with either nerve stimulator or ultrasonography. With a nerve stimulator, electrical stimulation resulting in contraction of the quadriceps in the prepatellar groove at 0.5 mA is considered sufficient to block the femoral nerve. As with other nerve blocks, the concentration of LA determines the clinical effect. A lower concentration is associated with analgesia of the surgical site, while a higher concentration is associated with both surgical anesthesia and motor blockade in the femoral distribution [37].
Popliteal Nerve Block
Sciatic nerve blocks in the popliteal fossa are used at the Hospital for Special Surgery to help alleviate pain after foot and ankle surgery, whether reconstructive or arthroscopic. Occasionally, they are used as the primary surgical anesthetic. Patients who have a popliteal block will usually have analgesia to approximately 85% of surface area of the foot. Because the sciatic nerve does not supply sensation to the entire foot, this block is often used in combination with a saphenous nerve block for postoperative pain control. The popliteal nerve is blocked in the popliteal fossa, an anatomical site that is bordered laterally by the biceps femoris muscle and medially by the semimembranosus muscle. This is also where the sciatic nerve splits into its two major components, the tibial and common peroneal nerves. Needle entry for the popliteal nerve block should be proximal to the splitting of these two nerves to avoid a partial block. With a nerve stimulator, electrical stimulation resulting in dorsiflexion of the foot at 0.5 mA is considered sufficient to block the popliteal nerve. When this is achieved, 30–40 ml of LA is injected—a large volume is required to ensure adequate anesthesia of both branches of the sciatic nerve. As with other nerve blocks, the concentration of LA determines the clinical effect. A lower concentration is associated primarily with analgesia of the surgical site, while a higher concentration is associated with both surgical anesthesia and motor blockade in the popliteal distribution.
Ankle Block
The ankle block is often used at the Hospital for Special Surgery to either provide surgical anesthesia and/or postoperative analgesia for surgeries of the forefoot. It is a combination of multiple injections around the foot and ankle area. All five nerves of the foot can be blocked at the level of a line connecting the medial and lateral malleoli. The posterior tibial nerve is the major contributor of sensation to the sole of the foot. To block this nerve, the needle is introduced just behind the posterior tibial artery and advanced until a paresthesia to the sole of the foot is elicited or bone is encountered, at which point the needle is slightly withdrawn and 5 ml of LA is injected. The sural nerve is blocked by injecting 5 ml of LA between the lateral malleolus and calcaneus. Infiltration of 5 ml of LA anterior to the medial malleolus blocks the saphenous nerve. The deep peroneal nerve is the major nerve to the dorsum of the foot and is blocked by injecting 5 ml of local anesthesia just lateral to the anterior tibial artery. Superficial branches of the peroneal nerve are blocked by a subcutaneous ridge of local anesthesia injected between the anterior tibial artery and lateral malleolus.
Neuraxial Anesthesia
Spinals, epidurals, and continuous spinal epidurals (CSE) are the mainstay of anesthesia for surgery of the lower limb at the Hospital for Special Surgery. Their techniques are well described elsewhere. As with peripheral nerve blocks, the choice of LA depends upon many factors, including availability, practitioner comfort, duration of surgery, positioning, and patient comorbidities. At our institution, epidurals facilitate the practice of controlled hypotension and are sometimes used to ensure patient comfort in settings where the use of a tourniquet is required. As a generalization, combined spinal/epidural techniques allow for continuous infusions of opioids and LAs for postoperative pain in the postoperative period.
Regional Anesthesia for Specific Procedures
As mentioned previously, regional anesthesia is used for most procedures performed at the Hospital for Special Surgery except spine surgical interventions, which require general anesthetics and are not discussed here.
Following is a brief description of the anesthetic techniques routinely used for various procedures commonly performed. Variations of the techniques described will depend on details of the surgery and patient comorbidities. A summary of anesthetic techniques used by procedure type is presented in Table 8.2.
Anesthetic Techniques: Upper Extremity
Total Shoulder Arthroplasty
As regional techniques, interscalene or supraclavicular nerve blocks are possible approaches for total shoulder arthroplasty, both for surgical anesthesia and postoperative pain control. Additionally, deep sedation or general anesthesia and airway management by laryngeal mask should be considered, given that the patient position and proximity of the surgical intervention to the airway can be very discomforting. An arterial line attached to a continuous blood pressure monitoring device is commonly utilized to duly detect and counteract blood pressure variations, which commonly appear in the sitting (beach chair) position.
Shoulder Arthroscopy
Similar to total shoulder arthroplasty, an interscalene or supraclavicular block in conjunction with sedation is used for diagnostic or interventional shoulder arthroscopy, providing adequate surgical anesthesia and postoperative analgesia to the shoulder region. Longer procedures or those requiring relaxation of the shoulder musculature, including shoulder stabilizations, may require the addition of a general anesthetic.
Elbow, Forearm, and Hand Surgery
Depending on the exact location of surgical intervention, a supraclavicular, infraclavicular, or axillary block can be taken into consideration. At HSS, the supraclavicular block is predominantly used for proximal, and an infraclavicular block for distal procedures, while the axillary block decreases in importance.
Anesthetic Techniques: Lower Extremity
Total Hip Arthroplasty
For total hip arthroplasty, combined spinal and epidural anesthesia has proven beneficial. On the one hand, given the complex nerve supply to the hip joint, surrounding tissue, and muscles, neuraxial anesthesia provides advantages compared to peripheral nerve blocks in practicality and ease of use. On the other hand, controlled hypotensive epidural anesthesia can reduce bleeding. Further, a lumbar plexus block can contribute to excellent postoperative analgesia, especially in cases where anticoagulation requires removal of the epidural catheter shortly after the procedure. Arterial blood pressure monitoring is obligatory with the use of controlled hypotension and with regard to invasiveness of the surgery and potential blood loss.
Total Knee Arthroplasty
The knee joint is supplied by both the femoral and sciatic nerves. Pain often extends to the thigh, for instance, when a tourniquet is used to reduce bleeding. Complete surgical anesthesia and postoperative pain control are most easily achieved by combination of neuraxial anesthesia (spinal and epidural) and peripheral (femoral or saphenous) nerve block. Catheters make prolonged postoperative application of local anesthetic possible. Arterial blood pressure monitoring is applied in patients classified as American Society of Anesthesiologists Class 3 or above.
Knee Arthroscopy
Outpatient knee arthroscopy can, as a minor painful procedure, most frequently be managed by spinal anesthesia alone at the Hospital for Special Surgery. Advantages are fast recovery and low incidence of complications. However, depending on patient preference or comorbidity profile, general anesthetics with a laryngeal mask airway may be used.
Foot and Ankle Surgery
Nerve supply to the lower leg, ankle, and foot is provided by the saphenous nerve (medial side), the sciatic nerve, and its branches, respectively. Blockade of one or more of these nerves is sufficient for complete surgical anesthesia, as long as no thigh tourniquet is applied. Depending on the location of the surgery, a popliteal block, an ankle block, or a saphenous block is chosen. For more extensive procedures, a spinal or combined spinal and epidural is added.
Spine Surgery
The transversus abdominis plane (TAP) block is a peripheral nerve block designed to anesthetize the nerves supplying the anterior abdominal wall (T6 to L1). It is often used in spinal surgical procedures that incorporate an anterior surgical approach to the spine. The anterior rami of spinal nerves T6–L1 innervate the anterolateral abdominal wall. The anterior divisions of the intercostal nerves (T7-11) enter the abdominal wall between the internal oblique and transversus abdominis muscles. The goal of the TAP block is to inject local anesthetic in the plane between the internal oblique and transversus abdominis muscles, targeting the spinal nerves in this plane. The injection interrupts innervation to the abdominal skin, muscles, and parietal peritoneum; however, it will not block visceral pain. The TAP block can be performed using a blind approach or with ultrasound guidance. Using an anatomic approach, a single point of entry is at the lumbar triangle of Petit. The triangle is bounded inferiorly by the iliac crest (IC), anteriorly by the external oblique muscle, and posteriorly by the latissimus dorsi. The costal margin (CM) is just superior to the triangle of Petit. The classic description is the feel of a “double pop” as the needle traverses the fascia extensions of the external oblique and the internal oblique muscles. However, the ultrasound approach, in which the probe is placed in a transverse plane to the lateral abdominal wall in the midaxillary line, between the lower costal margin and iliac crest, allows for a more accurate deposition of local anesthesia.
Summary
Orthopedic surgery is undoubtedly one of the specialties where regional anesthesia is used most frequently and most successfully. Not only does the practice of selectively anesthetizing specific regions of the body mitigate the systemic stress associated with surgery, but it also allows for more focused and sustained postoperative analgesia. Especially the elderly and people suffering from comorbidities like cardiovascular or respiratory disease benefit most. Furthermore, many studies demonstrated reductions in demand for analgesics and other systemically administered drugs, exerting a positive influence on perioperative well-being and diminishing associated side effects like nausea, vomiting, or constipation [38]. However, in order to achieve optimal acuity, duration, and minimal side effects, it is essential for the anesthesiologist to gain knowledge about a number of influencing factors: selection of appropriate block technique; choice of the right local anesthetic agent, concentration, and dosage; locating injection sites by use of anatomical landmarks, paresthesia technique, ultrasound, or a combination of these methods; determining block success and, if in doubt, resorting to another method of regional or even general anesthesia; ensuring sustained analgesia; and, last but not least, awareness of side effects associated with injection and/or drugs. The most cumbersome immediate complication of regional anesthesia is LAST. LAST can rapidly lead to catastrophic situations, only manageable by means of the full-scale application of intensive care services. The mainstay of treatment is Intralipid, and its availability is mandatory in areas where regional anesthesia is administered. Moreover, although infrequently occurring, permanent nerve damage is a matter of concern and potentially disqualifies some patients from receiving regional anesthesia.
Comprehensive unilateral anesthesia to the whole limb can more easily be achieved in the upper extremity. Possible approaches include the interscalene, supraclavicular, infraclavicular, and axillary plexus block and should be chosen according to type of surgery and desired distribution of anesthesia. In the lower limb, several techniques are available for the lumbosacral plexus as well as for peripheral nerves. However, a multimodal approach combining one or more of these peripheral blocks with neuraxial anesthesia is applied frequently.
In conclusion, regional techniques are cornerstones of orthopedic anesthesia; their development and advancement establish new possibilities and make orthopedic surgery available to more patients. While widely used at the Hospital for Special Surgery, variations of these approaches have to be tailored to individual patient comorbidities, preferences, anatomic variations, as well as surgical cofactors like patient positioning.
Summary Bullet Points
-
Regional anesthesia provides focused and sustained pain relief for patients undergoing orthopedic surgery.
-
Choice of specific anesthetics and techniques is the key to successful regional anesthesia.
-
Complications and contraindications must be kept in mind in order to minimize potential harm.
Case Study
A 27-year-old woman (68 kg, 165 cm) with a history of shoulder pain over several months presented for ambulatory diagnostic shoulder arthroscopy. Her preoperative vital signs, clinical examination, and routine laboratory workup were unremarkable.
The patient was monitored as per routine and a 20-gauge intravenous cannula was placed. The injection site for an interscalene block was determined using a 30 mm insulated needle attached to a nerve stimulator. After biceps response was evoked at 1.8 mA and intravascular needle position was ruled out by negative aspiration, 30 mL of 0.375% bupivacaine was injected, with aspiration occurring at 5 mL intervals.
The patient immediately began to complain about acoustic sensations as well as feelings of dry and itchy mouth and eyes. The injection was interrupted and the needle withdrawn; within 20 s, generalized convulsions resembling a grand mal seizure developed, and the patient was found to be apneic. Mask ventilation with 100% oxygen was initiated, midazolam 5 mg was administered, and the anesthesia technician was instructed to get a lipid rescue kit from the cardiac arrest cart located outside the room. The convulsions stopped and the anesthesiologist noticed broad complex tachycardia with a heart rate of 140 bpm on the ECG; a pulse was difficult to palpate at the carotid artery. Intralipid® 20% 500 mL intravenously was started. Attempts to place a radial arterial catheter failed at that point. An attempt of cardioversion was unsuccessful. After 50 mL of Intralipid® was infused, a brief period of ventricular fibrillation was immediately followed by asystole. After commencement of cardiac compressions, administration of epinephrine 1 mg, and successful tracheal intubation, another 150 mL of Intralipid® was infused rapidly. Return of spontaneous circulation occurred approximately 45 s after initial appearance of ventricular fibrillation. A narrow complex tachycardia was present on the ECG; a radial arterial catheter was successfully placed. The initial blood pressure obtained was 140/90 mmHg, but rapidly declined to 80/40 mmHg. Circulation was supported with repetitive boluses of phenylephrine and epinephrine, until a central line and continuous epinephrine infusion was established. Analysis of arterial blood samples revealed the following values: pH 6.8, PaCO2 116 mmHg, PaO2 144 mmHg, and lactate exceeding 15 mmol/L. Intermittent positive pressure ventilation was maintained to counteract hypercapnia and acidosis. To facilitate ventilation and prevent reoccurrence of convulsions, another 7.5 mg bolus of midazolam was administered. The remaining 300 mL of Intralipid was infused over 20 min (0.22 mL/kg/min). The patient was transferred to the intensive care unit. A repeated arterial blood sample after 2 h revealed a pH of 7.33, PaCO2 of 48 mmHg, PaO2 of 222 mmHg, lactate of 9.2 mmol/L, potassium of 2.7 mmol/L, and glucose of 90 mg/dL. The ECG showed a sinus tachycardia at a rate of 110 bpm with occasional ventricular ectopy. An amiodarone loading dose (300 mg) and potassium were subsequently administered, and the patient was maintained on continuous inotropic support (epinephrine 0.02 μg/kg/min) and sedation (propofol 50 μg/kg/min). Epinephrine and propofol were gradually decreased and eventually discontinued 4 h after admission to the intensive care unit. The patient was extubated shortly thereafter. The patient was transferred to a cardiac ward on day 3 and discharged 7 days after the initial event. The surgical procedure was carried out 4 weeks later using general anesthesia without any incident.
References
Rosenberg PH, Veering BT, Urmey WF. Maximum recommended doses of local anesthetics: a multifactorial concept. Reg Anesth Pain Med. 2004;29:564–75. discussion 524
Wedel DJ, Horlocker TT. Regional anesthesia in the febrile or infected patient. Reg Anesth Pain Med. 2006;31:324–33.
Hebl JR, Niesen AD. Infectious complications of regional anesthesia. Curr Opin Anaesthesiol. 2011;24:573–80.
Gritsenko K, Marcello D, Liguori GA, Jules-Elysee K, Memtsoudis SG. Meningitis or epidural abscesses after neuraxial block for removal of infected hip or knee prostheses. Br J Anaesth. 2011;108:485–90.
Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp SL, Benzon HT, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American society of regional anesthesia and pain medicine evidence-based guidelines (third edition). Reg Anesth Pain Med. 2010;35:64–101.
Horlocker TT. Regional anaesthesia in the patient receiving antithrombotic and antiplatelet therapy. Br J Anaesth. 2011;107(Suppl 1):96–106.
Hebl JR, Horlocker TT, Kopp SL, Schroeder DR. Neuraxial blockade in patients with preexisting spinal stenosis, lumbar disk disease, or prior spine surgery: efficacy and neurologic complications. Anesth Analg. 2010;111:1511–9.
Wolfe JW, Butterworth JF. Local anesthetic systemic toxicity: update on mechanisms and treatment. Curr Opin Anaesthesiol. 2011;24:561–6.
Weinberg GL. Treatment of local anesthetic systemic toxicity (LAST). Reg Anesth Pain Med. 2010;35:188–93.
Neal JM, Bernards CM, Butterworth JF 4th, Di Gregorio G, Drasner K, Hejtmanek MR, et al. ASRA practice advisory on local anesthetic systemic toxicity. Reg Anesth Pain Med. 2010;35:152–61.
Corman SL, Skledar SJ. Use of lipid emulsion to reverse local anesthetic-induced toxicity. Ann Pharmacother. 2007;41:1873–7.
Picard J, Ward SC, Zumpe R, Meek T, Barlow J, Harrop-Griffiths W. Guidelines and the adoption of ‘lipid rescue’ therapy for local anaesthetic toxicity. Anaesthesia. 2009;64:122–5.
Jacob AK, Mantilla CB, Sviggum HP, Schroeder DR, Pagnano MW, Hebl JR. Perioperative nerve injury after total hip arthroplasty: regional anesthesia risk during a 20-year cohort study. Anesthesiology. 2011;115:1172–8.
Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104:965–74.
Urmey WF. Using the nerve stimulator for peripheral or plexus nerve blocks. Minerva Anestesiol. 2006;72:467–71.
Antonakakis JG, Ting PH, Sites B. Ultrasound-guided regional anesthesia for peripheral nerve blocks: an evidence-based outcome review. Anesthesiol Clin. 2011;29:179–91.
Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound guided infraclavicular block. Br J Anaesth. 2006;96:502–7.
Barrington MJ, Snyder GL. Neurologic complications of regional anesthesia. Curr Opin Anaesthesiol. 2011;24:554–60.
Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113:904–25.
Partridge BL, Katz J, Benirschke K. Functional anatomy of the brachial plexus sheath: implications for anesthesia. Anesthesiology. 1987;66:743–7.
Winnie AP. Interscalene brachial plexus block. Anesth Analg. 1970;49:455–66.
Urmey WF, Gloeggler PJ. Pulmonary function changes during interscalene brachial plexus block: effects of decreasing local anesthetic injection volume. Reg Anesth. 1993;18:244–9.
Plit ML, Chhajed PN, Macdonald P, Cole IE, Harrison GA. Bilateral vocal cord palsy following interscalene brachial plexus nerve block. Anaesth Intensive Care. 2002;30:499–501.
Sinha SK, Abrams JH, Barnett JT, Muller JG, Lahiri B, Bernstein BA, et al. Decreasing the local anesthetic volume from 20 to 10 ml for ultrasound-guided interscalene block at the cricoid level does not reduce the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2011;36:17–20.
Benumof JL. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia. Anesthesiology. 2000;93:1541–4.
Gautier P, Vandepitte C, Ramquet C, DeCoopman M, Xu D, Hadzic A. The minimum effective anesthetic volume of 0.75% ropivacaine in ultrasound-guided interscalene brachial plexus block. Anesth Analg. 2011;113:951–5.
Liu SS, Gordon MA, Shaw PM, Wilfred S, Shetty T, Yadeau JT. A prospective clinical registry of ultrasound-guided regional anesthesia for ambulatory shoulder surgery. Anesth Analg. 2010;111:617–23.
Guzeldemir ME. Pneumothorax and supraclavicular block. Anesth Analg. 1993;76:685.
Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009;34:171–6.
Chan VW, Perlas A, Rawson R, Odukoya O. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97:1514–7.
Chin KJ, Singh M, Velayutham V, Chee V. Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Anesth Analg. 2010;111:1072.
Fredrickson MJ, Wolstencroft P, Kejriwal R, Yoon A, Boland MR, Chinchanwala S. Single versus triple injection ultrasound-guided infraclavicular block: confirmation of the effectiveness of the single injection technique. Anesth Analg. 2010;111:1325–7.
Chin KJ, Handoll HH. Single, double or multiple-injection techniques for axillary brachial plexus block for hand, wrist or forearm surgery in adults. Cochrane Database Syst Rev. 2011;(7):CD003842.
De Tran QH, Clemente A, Finlayson RJ. A review of approaches and techniques for lower extremity nerve blocks. Can J Anaesth. 2007;54:922–34.
Atanassoff PG, Weiss BM, Brull SJ, Horst A, Kulling D, Stein R, et al. Electromyographic comparison of obturator nerve block to three-in-one block. Anesth Analg. 1995;81:529–33.
Saranteas T, Anagnostis G, Paraskeuopoulos T, Koulalis D, Kokkalis Z, Nakou M, et al. Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Reg Anesth Pain Med. 2011;36:399–402.
Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A, et al. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113:1144–62.
Richman JM, Liu SS, Courpas G, Wong R, Rowlingson AJ, McGready J, et al. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg. 2006;102:248–57.
Heavner JE. Local anesthetics. Curr Opin Anaesthesiol. 2007;20:336–42.
Berde C, Strichartz G. Local anesthetics. In: Miller R, editor. Miller’s anesthesia. 7th ed. Philadelphia: Churchill Livingstone; 2009. p. 913–39.
Forster JG, Rosenberg PH. Revival of old local anesthetics for spinal anesthesia in ambulatory surgery. Curr Opin Anaesthesiol. 2011;24:633–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stundner, O., Swamidoss, C.P. (2020). Anesthetic Techniques and Their Clinical Application for Specific Orthopedic Procedures. In: MacKenzie, C., Cornell, C., Memtsoudis, S. (eds) Perioperative Care of the Orthopedic Patient. Springer, Cham. https://doi.org/10.1007/978-3-030-35570-8_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-35570-8_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-35569-2
Online ISBN: 978-3-030-35570-8
eBook Packages: MedicineMedicine (R0)