Abstract
In previous chapters of this book analyze the antiarrhythmic drugs (AADs) classified in groups I-IV according to the Vaughan-Williams classification. However, some old (adenosine, digoxin) and new AADs (ivabradine, ranolazine, vernakalant) were not listed in any of the original four classes. Therefore, in this chapter, we shall review the electrophysiological effects of these drugs (Table 6.1). Their electrophysiological and pharmacokinetic properties, adverse effects and clinical indications are summarized in Tables 6.2, 6.3, 6.4, 6.5, 6.6, and 6.7.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
In previous chapters of this book several authors analyze in detail the antiarrhythmic drugs (AADs) classified in groups I-IV according to the Vaughan-Williams classification. However, some old (adenosine, digoxin) and new AADs (ivabradine, ranolazine, vernakalant) were not listed in any of the original four classes. Therefore, in this chapter, I shall review the electrophysiological effects of these drugs (Table 6.1). Their electrophysiological and pharmacokinetic properties, adverse effects, doses drug interactions, cautions, contraindications and clinical indications are summarized in Tables 6.2, 6.3, 6.4, 6.5, 6.6, and 6.7.
Adenosine
Adenosine is a ubiquitous endogenous purine nucleoside. Activation of Gi/o protein–bound cardiac adenosine A1 receptors present in atrial muscle, sino-atrial (SAN) and atrio-ventricular nodal (AVN) cells [1,2,3]: (a) activates the acetylcholine-gated inward rectifying K+ current (IKACh/IKAdo) that hyperpolarizes the membrane potential, slows SAN pacemaker rate and shortens atrial action potential duration (APD) and refractoriness. (b) Inhibits the mixed Na+-K+ inward pacemaker current (If) generated via non-selective hyperpolarization-activated cyclic nucleotide-gated cation (HCN) channels, which regulates the rate of the spontaneous depolarization of the SAN cells. (c) Reduces adenyl cyclase activity and intracellular cAMP levels, which indirectly inhibits the L-type calcium current (ICa) during sympathetic stimulation. As a consequence, adenosine decreases SAN pacemaker activity and in the AVN slows conduction velocity and increases refractoriness. (d) Activates presynaptic purinergic receptors located on sympathetic nerve terminals decreasing the release of norepinephrine. These two later effects explain why adenosine terminates some atrial and ventricular arrhythmias and abolishes both early (EADs) and delayed (DADs) afterdepolarizations induced by catecholamines.
Activation of the Gs protein–bound A2 receptors increases adenyl cyclase activity and cAMP levels, inhibits Ca2+ entry and myosin light chain kinase and stimulates ATP-sensitive potassium (KATP) channels which hyperpolarizes vascular smooth muscle cells [1,2,3]. As a result, adenosine decreases coronary and peripheral vascular resistances, vasodilates coronary microvessels (<150 mm in diameter), adequates coronary blood flow to cardiac metabolic demands playing a key role in ischemic pre-conditioning and attenuates ischemia-reperfusion injury. Because of its coronary vasodilator properties, adenosine is indicated for stress radionuclide myocardial perfusion imaging in patients unable to undergo adequate exercise stress. Adenosine has also been used to produce controlled hypotension.
Pharmacodynamics
An intravenous (IV) bolus of adenosine, preferable through a large venous or central line, rapidly (within 10–30 s) and transiently slows AV conduction velocity [due to effects on the atrial-His (AH) interval, but not on the H-V interval] and increases AV refractoriness (prolongs the PR and A-H intervals) leading to a transient AV block that is then responsible for tachycardia termination [4, 5]. Thus, adenosine the drug of choice to terminate supraventricular tachycardias (SVT) using the AVN as a portion of the reentrant circuit, such as AV nodal re-entry tachycardias (AVNRT) and AV reentrant tachycardias (AVRT). Success rates range from 78% to 96% (similar to verapamil) in acute episodes of SVT [3,4,5,6,7,8,9,10,11]. Adenosine also slows sinus rate, may cause sinus exit block and can terminate SAN reentry. The effects of adenosine on the SAN and AVN are of greater and longer in patients with recent heart transplantation (<1 year). Adenosine is effective in terminating some focal atrial tachycardias (AT) due to a triggered mechanism in adult congenital heart disease patients, but does not interrupt macro-re-entrant ATs unless the reentrant circuit involves the AVN [7, 12]. Adenosine is unlikely to terminate atrial fibrillation (AF) or atrial flutter (AFl) [13], but it can produce a transient AV block, which unmask atrial activity and helps to diagnosis. Adenosine does not affect conduction velocity through the His-Purkinje or normal accessory pathways, but conduction can be blocked in accessory pathways with long conduction times or decremental conduction. Ventricular tachycardias (VT) do not respond to adenosine, but it can terminate idiopathic right outflow tract VT caused by a cAMP-mediated triggered activity caused by delayed afterdepolarizations; idiopathic left septal VT rarely responds.
Adenosine terminates AVNRT, SVT using an accessory pathway, and some forms of focal AT which account for <25% of SVT in adults with repaired congenital disease. However, evwn when it is unlikely to terminate atrial reentry tachycardia or atrial flutter, which represents >70% of SVT episodes in this population, adenosine may help to the diagnosis by producing transient AV block, which would make the atrial activity visible [1, 4, 7, 10,11,12].
Adenosine can help to the diagnosis of narrow-complex tachyarrhythmias [1, 4, 5, 8,9,10,11,12]. The appearance of transient AVN block with persistent AT can help to differentiate focal AT from AVNRT and AVRT [7]. In wide-QRS tachycardias of uncertain origin, adenosine can help to differentiate SVT (with aberrant conduction) from VT; adenosine is likely to terminate SVT with aberrancy or reveals the underlying atrial mechanism, while the VT continues. When an accessory by-pass tract is present, adenosine may increase conduction down the anomalous pathway revealing latent pre-excitation in patients with suspected Wolff-Parkinson-White (WPW) syndrome. A normal response occurs if transient high-grade AV block is observed; the presence of an anterograde conduction accessory pathway is inferred if adenosine produces a PR shortening-QRS widening without interruption of AV conduction. Adenosine can also differentiate conduction over the AVN from that over an accessory pathway during ablative procedures of the accessory pathway, and can provide a diagnosis in VT with retrograde conduction by blocking the P wave.
Adenosine may also promote arrhythmogenesis [2, 14]. It often produces bradycardia, sinus arrest and several degrees of AVN block, and even when prolonged bradycardia is unusual, caution is recommended in patients with known sinus node disease [2, 5, 15]. The risk of bradycardia increases in recipients of denervated orthotropic heart transplants, in whom SVT is common [5, 16]. Adenosine may induce AF with fast ventricular conduction and even VT by several mechanisms as it heterogeneously shortens atrial APD and refractoriness, produces transient sympathetic stimulation (tachycardia) through baroreflex activation in response to hypotension and it can hyperpolarize dormant pulmonary vein myocytes increasing their excitability and automaticity [17, 18]; the risk of AF appears more commonly associated with AVRT than AVNRT [8]. Patients with orthodromic AVRT often present atrial or ventricular premature complexes immediately after conversion that ocassionally may induce further episodes of AVRT. In this situation, an antiarrhythmic drug may be required to prevent acute reinitiation of tachycardia [1, 9,10,11]. Adenosine may also occasionally cause or accelerate pre-excited atrial arrhythmias [5, 19]. Because of the risk of proarrhythmia, adenosine should be used only in-hospital and with full resuscitative equipment available.
Pharmacokinetics
After IV administration adenosine is rapidly cleared from circulation via cellular uptake by erythrocytes and vascular endothelial cells, where it is metabolized by the adenosine deaminase to inosine and adenosine monophosphate which are excreted by the kidneys. Its half-life (t1/2) is <20 s, which explains why adverse effects even when frequent, they rapidly disappear and the repeated administration is safe within 1 min of the last dose.
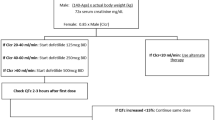
The starting dose required for efficient rhythm correction is ~6 mg, given as a rapid bolus (1–2 sec) followed by a rapid saline flush. Large, centrally located (e.g. antecubital) veins are likely to deliver more effective drug concentrations to the heart than smaller distal veins [10, 11]. Another bolus of 12 mg can be administered after 1–2 min; this 12 mg bolus can be repeated in 1–2 min if SVT persist (Table 6.3).
Adverse Effects (Table 6.4)
The most common include flushing, dyspnea (most likely secondary to stimulation of vagal C fibers in the lungs), chest discomfort, headache, dizziness, numbness or nausea, AV block and arrhythmias, but serious adverse adverse effects are rare because of the drug’s very short half-life [2, 20]. Chest discomfort begins at approximately the same time as the delay in AV conduction and is immediately preceded by a marked increase in coronary-sinus flow, suggesting that the pain has a myocardial origin [5, 11]. Adenosine may precipitate or aggravate bronchospasm; thus, it may be reasonable to replace adenosine by verapamil in asthmatic patients.
Indications
Adenosine is the drug of choice to rapidly terminate regular narrow-QRS-complex PSVT using the AVN as part of the reentry circuit when vagal manoeuvres fail, except for patients with severe asthma or angina pectoris [10, 11]. Because of its rapid onset and short duration of action, adenosine is preferable to verapamil or diltiazem, particularly in patients treated with IV β-adrenergic blockers or with history of heart failure (HF) or severe hypotension, and in neonates. Adenosine is the drug of choice for termination of SVT in pregnant patients when vagal manoeuvres fail; adverse effects to the fetus would not be expected and maternal side effects are transient given its short half-life [10, 11, 21]. Adenosine can also terminate AT, sinus node reentry and idiopathic right outflow tract VT commonly triggered by sympathetic stimulation.
Selective A1R Agonists (Table 6.1)
They slow conduction velocity and prolong refractoriness in the AVN without affecting intraventricular conduction or reducing blood pressure or causing bronchospasm, two common side effects of adenosine [22]. They are effective for the conversion of PSVT to sinus rhythm (SR) and for ventricular rate control in AF without the negative inotropic and vasodilator effects of β-blockers, verapamil or diltiazem. Tecadenoson dose-dependently prolongs the AH interval (peak effect within 1 min, but returned to baseline after 10 min) without an effect on the HV interval, presents a longer t1/2 than adenosine (20–30 min) and converts PSVT to SR in 90% of patients even after the first bolus, coincident with anterograde AV conduction block. Patients with a history of asthma or chronic obstructive pulmonary disease tolerated tecadenoson without bronchospasm. Other A1 adenosine receptor-selective full agonists and partial agonists are under development for multiple clinical indications.
Cardiac Glycosides
Cardiac glycosides (digoxin and digitoxin) increase cardiac contractility and slow AVN conduction and have been used for decades to treat patients with symptomatic heart failure (HF) or impaired left ventricular (LV) function and for ventricular rate control in patients with supraventricular arrhythmias, mainly permanent and persistent AF, respectively. However, their use have declined over the past years because of its narrow therapeutic window and multiple interactions (Table 6.7), the increasing number of evidence-based therapies for HF and the results of the DIG trial [23], where digoxin therapy was shown to reduce all-cause and HF-specific hospitalizations but had no effect on survival.
Mechanism of Action
Digoxin inhibits the Na+/K+-ATPase (3 Na+ out − 2 K+ in) [24, 25]. This inhibition increases the intracellular Na+ concentration ([Na+]i), which in turn, activates the reverse mode of the Ca2+-Na+ exchanger (NCX, Na+ efflux/Ca2+ influx) leading to an increase in intracellular Ca2+ concentration ([Ca2+]i). This increase in [Ca2+]i at the level of contractile proteins might account for the positive inotropic effect and the proarrhythmic effects during digitalis intoxication. Furthermore, digitalis form calcium-conductance pathways and cation-selective Ca2+ channels which may play a role in Ca2+-dependent cardiotoxicity [26].
At therapeutic concentrations the electrophysiologic effects of digoxin are mediated indirectly by enhancing both central and peripheral vagal and inhibiting sympathetic tone, and to a lesser extent through a direct cardiac effect [24, 25]. The increase in vagal tone: (a) inhibits If and accelerates the inactivation of the ICa due to the higher [Ca2+]i, producing a mild resting bradycardia that may increase LV performance; (b) activates the IKACh leading to a nonuniform shortening of atrial APD and refractoriness; and (c) slows conduction and prolongs refractoriness in the AVN (prolongs the PR interval). This latter effect is the basis to use digoxin to control ventricular rate in patients with AF, particularly in unstabilized HF patients in whom β-blockers and calcium antagonists are contraindicated and to terminate reentrant tachyarrhythmias involving the AVN. However, digoxin exerts minimal effects on the His-Purkinje and ventricular muscle and the QRS and QT intervals are unaffected. Inhibition of Na+/K+-ATPase in the vagal afferent fibers restores cardiac baroreceptor sensitivity, leading to a decrease in peripheral sympathetic nerve activity; digoxin also reduces renin and angiotensin II plasma levels. This neurohumoral inactivation may play a key role at these therapeutic concentrations.
At toxic concentrations , digoxin directly causes sinus bradycardia and different degrees of AVN block, shortens atrial and ventricular APD and refractoriness, but increases [Ca2+]i and sympathetic cardiac activity; these later effects increase the automaticity of cardiac pacemakers (AVN, His-Purkinje system) [24, 25]. Additionally, the inhibition of the Na+/K+-ATPase depolarizes the resting membrane potential, partially inactivates Na+ channels and decreases intracardiac conduction velocity. Additionally, digoxin increases [Ca2+]i and induces the spontaneous release of Ca2+ from the sarcoplasmic reticulum during the diastole, which, in turn, activates the forward mode of the NCX (Na+ influx/Ca2+ efflux) leading to a net inward transient depolarizing current (ITi) that can generate EADs and DADs. All these effects predispose to both bradyarrhythmias and supraventricular and ventricular tachyarrhythmias that may degenerate in VT and ventricular fibrillation (VF). The increase in [Ca2+]i in vascular smooth muscle cells can cause a direct vasoconstriction that may cause mesenteric artery occlusion or ischemia.
Electrophysiological Effects
Digoxin effectively slows ventricular rate at rest when vagal tone predominates and in sedentary elderly patients with persistent/permanent AF [24, 25]. However, when sympathetic activity increases (i.e., during exercise, serious illness, fever, HF, hyperthyroidism, chronic lung disease, postoperative) its beneficial effects on AV conduction are reduced. Thus, digoxin is rarely used as a single agent for ventricular rate control in AF, but a satisfactory rate control can be achieved both at rest and during exercise when combined with β-blockers, verapamil or diltiazem. The ongoing RATE-AF trial is the first randomised clinical trial comparing digoxin and beta-blockers in AF.
Digoxin produces a nonuniform shortening of atrial APD and refractoriness that may explain why digoxin may increase the duration of AF, predisposes to early relapses of AF after restoration of SR and can convert the AFl to AF [24, 25]. Digoxin is no more effective than placebo to terminate AF or facilitate direct current cardioversion and may even induce episodes of AF in patients with so-called vagal AF [27]. Digoxin is contraindicated in patients with pre-excited AF because it slows AVN conduction but can accelerate anterograde conduction via the bypass tract increasing the ventricular rate during AF and the risk of provoking a life-threatening ventricular arrhythmia [13, 27,28,29].
In the ACC/AHA/HRS Guideline for the management of adult patients with supraventricular tachycardia oral digoxin is recommended for ongoing management in patients with symptomatic SVT without pre-excitation or with AVNRT who are not candidates for, or prefer not to undergo, catheter ablation [10]. However, digoxin should be reserved for patients who are unresponsive to, or are not candidates for β-blockers, diltiazem, or verapamil or a class IC agents (flecainide or propafenone) and it be used with caution in the presence of renal dysfunction. Interestingly, in the 2019 ESC Guidelines for the management of patients with SVT digoxin is not mentioned [11].
Because of its positive inotropic agent, digoxin is recommended for heart rate control in patients with AF and LVEF <40%, particularly in unstabilized patients in whom both β-blockers, diltiazem or verapamil are contraindicated. The combination of digoxin and carvedilol leads to better ventricular rate control than either agent, reduces symptoms, improves exercise tolerance and LV function [30]. In patients with AF (25% of the patients in NYHA class III) the IV administration of digoxin and esmolol produces a rapid rate control and conversion to SR occurs in 25% of patients [31]. In the AF-CHF trial [32], including patients with AF and LVEF ≤35%, adequate rate control was achieved in 82–88% of patients using adjusted doses of β-blockers with digoxin and in the CHF-STAT trial [33], amiodarone improved ventricular rate control when added to background therapy with digoxin in patients with AF and HF.
Several observational studies and meta-analysis associated digoxin therapy with excess mortality in patients with AF, but this finding was not confirmed in other studies [34,35,36]. The association is hampered by selection and prescription biases, because digoxin is commonly prescribed in sicker patients, with more comorbidities (HF, diabetes) and a higher baseline risk of mortality. A recent meta-analysis of 52 studies including over 600,000 patients with AF and concomitant HF, concluded that digoxin had a neutral effect on mortality but reduced hospital admission [36]. Thus, until proper randomized controlled trials are available, digoxin remains a suitable treatment option for rate control in patients with AF and HF.
Digoxin Plasma Levels
Digoxin presents a narrow therapeutic window. Routine monitoring of serum digoxin concentrations (SDC) is not warranted in AF patients with controlled ventricular rate and without symptoms of toxicity, but is justified in patients with suspected digoxin intoxication, impaired renal excretion, variable cardiac responses, altered volume of distribution (Vd), hyperthyroidism, or suspected drug interactions, and to monitor compliance with therapy (Table 6.7). A retrospective analysis of the DIG trial found that low SDC (0.6–0.9 ng/mL) provided hemodynamic benefit and a small decrease in all-cause mortality, while at higher SDC (≥1.2 ng/mL) digoxin increased mortality (12%) [37]. Thus, SDC should be maintained between 0.6 and 1 ng/mL.
Doses should be based on age, gender, lean body mass, serum creatinine, serum electrolytes and presence of other drugs as digoxin presents multiple pharmacodynamic/pharmacokinetic interactions (Table 6.6). In elderly patients digoxin presents a lower Vd due to a loss of lean muscle mass and decline in renal function. Renal impairment decreases digoxin clearance and prolongs its t1/2. Thus, doses, clinical response and SDC should be carefully titrated in elderly and in patients with chronic kidney disease. No dosage adjustments are recommended for patients with hepatic impairment. Digoxin is a substrate of P-glycoprotein (P-gp) and P-gp inhibitors can enhance digoxin absorption and/or reduce its renal clearance.
Adverse Effects
Digoxin presents a narrow therapeutic index and SDC should be maintained between 0.5 and 0.9 ng/mL (Table 6.7). Cardiac glycosides can produce any type of arrhythmia, including bradyarrhythmias related to an increase in vagal tone (sinus bradycardia or arrest, AV block) and supraventricular (paroxysmal AT with variable AV block, AVN tachycardias) and ventricular tachyarrhythmias (ventricular bideminy, VT, VF), particularly when electrolyte disorders are present.
If there is suspicion of toxicity, digoxin should be discontinued and ECG and SDC monitored. Electrolyte disorders, thyroid dysfunction and drugs/factor increasing SDC should be corrected (Table 6.7). Potassium salts should be avoided in the presence of bradycardia or conduction disturbances. Bradyarrhythmias or AV block respond to atropine but a temporary cardiac pacing may be required if symptomatic; ventricular arrhythmias may respond to lidocaine. Life-threatening arrhythmias can be treated with antidigoxin Fab fragments. Direct-current cardioversion should only be used if necessary using the lowest effective energy because life-threatening VT/VF can result. For elective electrical cardioversion of AF of a patient who is taking digoxin, the drug should be withheld for 1–2 days before cardioversion is performed.
Indications
Digoxin is no longer a first-line drug for acute or long-term rate control during permanent/persistent AF or AFl, but because of its low cost and accumulated knowledge in prescription during decades, digoxin would remain for rate control AF, especially for elderly-sedentary or patients with HF or LV dysfunction [13, 27].
For acute heart rate control in patients without evidence of reduced LVEF, digoxin can be added to β-blockers, verapamil or diltiazem where required [13, 27]. However, β-blockers and diltiazem/verapamil are preferred over digoxin because of their rapid onset of action and effectiveness at rest and/or during exercise. In patients with signs of HF or evidence of reduced LVEF, β-blockers and/or digoxin should be considered as first-line therapy to improve LV function; digoxin is indicated in unstabilized HF patients in whom β-blockers and calcium channel blockers are contraindicated. For long-term rate control digoxin, alone or in combination with other AV blocking drugs (beta-blockers, diltiazem, or verapamil) is recommended for long-term rate control in patients with persistent/permanent AF with LVEF ≥40%, with dosage appropriate to avoid bradycardia, and in AF patients with LVEF <40% [13, 27]. In SVT, digoxin has been replaced by adenosine, β-blockers and verapamil, drugs with faster onset of action and better safety profile. However, in the absence of pre-excitation, digoxin may be reasonable in patients with symptomatic SVT (including pregnant patients), orthodromic AVRT who are not candidates for, or prefer not to undergo, catheter ablation, and in AVNRT in patients with SBP <110 mmHg in whom β-blockers, verapamil or diltiazem may cause symptomatic hypotension or bradycardia [10, 11]. Digoxin has no role in ventricular arrhythmias.
Atrial-Selective Sodium Channel Blockers
A new strategy for suppression of AF/AFl is the development of the so-called atrial-selective Na+ channel blockers, drugs that predominantly depresses atrial versus ventricular Na+ channel-dependent parameters and suppresses AF at concentrations producing little to no effect in the ventricles, thus reducing the risk of ventricular proarrhythmia. It has been hypothesized [38] that drugs like vernakalant and ranolazine that preferentially bind to the inactivated state of the Na+ channel with fast unbinding kinetics might exhibit atrial selectivity during AF because: (a) atrial cells exhibit a more depolarized (~10 mV) resting membrane potential and a more negative half-inactivation voltage of Na+ channels. Because reactivation depends on membrane potential, fewer Na+ channels recover from the inactivated state during diastole in atrial as compared to ventricular cells and atrial refractoriness persist after the action potential is fully repolarized (postrepolarization refractoriness-PRR). (b) Atrial action potentials present a more gradual phase 3 which at rapid atrial rates results in a progressive disappearance of the diastolic interval in atria but not in ventricles and a less negative take-off potential further increasing the percentage of inactivated Na+ channels. During AF, as the atria fail to fully repolarize, the difference in resting membrane potential between the atria and ventricles increases and less atrial Na+ channels fully recover during diastole and remain in the inactivated state leading to the accumulation of Na+-channel block and PRR.
Vernakalant
Vernakalant is an atrial-selective multichannel blocker that inhibits the peak (INa) and late Na+ (INa,L) currents, resulting in slow intra-atrial conduction and prolongation of atrial refractoriness, and several outward K+ currents that control atrial repolarization: the ultra-rapid delayed rectifier current (IKur), the transient potassium current (Ito) and the inward rectifier currents IKAch and IKATP [39]. However, vernakalant has no effect on ICaL or the rapid component of the delayed rectifier (IKr). As a consequence, vernakalant blocks INa in a rate- and voltage-dependent manner, so that Na+ channel blockade increases at depolarized potentials and high heart rates, i.e. during AF, and selectively prolongs atrial APD and refractoriness with minimal effects on ventricular repolarization (QT interval) and refractoriness.
Pharmacodynamics
The efficacy and safety of IV vernakalant for cardioversion of recent-onset AF was evaluated in six clinical trials [40, 41]. Vernakalant selectively prolongs atrial APD and refractoriness without affecting ventricular repolarization (QT interval) or refractoriness, heart rate or blood pressure. Vernakalant was significantly more effective than placebo for the conversion of AF to SR; the mean time to conversion was 8–14 min and 75–82% of patients converted after the first dose. The highest efficacy of vernakalant was observed for AF lasting for up to 72 h (51–79%), but decreased with the duration of the arrhythmia, being ineffective for the conversion of AF lasting >7 days or AFl. Interestingly, pre-treatment with vernakalant can improve the efficacy of electrical cardioversion. In the AVRO trial [42], vernakalant was more effective than IV amiodarone but the responder rates were lower, probably because of the higher proportion of patients with HF were enrolled in this trial. The probability of conversion to SR is independent of age, sex, LVEF, left atrial size, prior use of AADs, history of coronary artery disease or renal impairment, but there was a trend towards decreased efficacy in elderly patients (aged ≥75 years), those with a history of HF and in patients receiving digoxin or class I AADs. However, vernakalant is ineffective in patients with AFl [13, 40, 41].
Drug exposure is not influenced by age, gender, race, coronary artery disease, HF, renal or hepatic impairment, CP2D6 genotype or coadministration of CYP2D6 inhibitors, AVN blockers or warfarin.
Indications
Intravenous vernakalant is recommended for the rapid termination of recent-onset AF (≤7 days for non-surgery patients; ≤3 days for post-cardiac surgery patients) to SR in adults without structural heart disease or with hypertension, CAD, abnormal LV hypertrophy or moderate HF (NYHA class I–II) and for cardioversion of postoperative AF, provided they do not present severe HF, hypotension, or severe aortic stenosis [13]. Vernakalant represents a fast and effective alternative to class IC antiarrhythmics and amiodarone, presents few proarrhythmic and extracardiac effects, eliminates the need for conscious sedation or anesthesia and when pharmacological cardioversion has failed it does not modify the efficacy of subsequent electric cardioversion. However, there are no head-to-head comparison with DC cardioversion or class IC AADs.
Ranolazine
Ranolazine is approved for the treatment of chronic stable angina for patients inadequately controlled or intolerant to β-blockers and/or calcium channel blockers.
Mechanism of Action
In atrial and ventricular muscle and Purkinje fibres, the rapid upstroke of the action potential is due to the activation of the INa. Most cardiac Na+ channels open transiently (1–3 ms) during membrane depolarization, but rapidly inactivate-close and remain closed during the plateau phase of the action potential. However, some Na+ channels do not inactivate or inactivate but reopen during the plateau generating the late Na+ current (INaL) [43, 44]. An enhanced INaL slows the rate of repolarization, prolongs the APD (QT interval) and increases transmural dispersion of repolarization (TDR) across the ventricular wall. These effects facilitate triggered and re-entrant arrhythmias. The INaL increases under conditions associated with a high incidence of cardiac arrhythmias, including myocardial ischemia, LV hypertrophy, HF and arrhythmias associated with mutations in the cardiac Na+ channel or their regulatory proteins (e.g. long QT and Brugada syndromes) [43, 44]. Myocardial ischemia increases the INaL and the [Na+]i which, in turn, activates the reverse mode of the NCX, leading to a Na+-mediated Ca2+ overload. This increase in Na+ and Ca2+ concentrations is a major contributor to the electrical (EADs, DADs, arrhythmias), mechanical (increases diastolic wall tension and MVO2) and metabolic disturbances (increase ATP consumption, decreases ATP formation) in the ischemic myocardium [43, 44].
Ranolazine selectively inhibits the INaL, with almost no inhibition of the peak INa. Thus, it does not widen the QRS complex or slows intracardiac conduction velocity. Ranolazine also inhibits the IKr, but the expected prolongation of the APD and QTc interval secondary to this effect is counteracted by the inhibition of INaL. Indeed, ranolazine suppresses EADs and torsades de pointes induced by selective IKr-blockers and QT-prolonging drugs. Ranolazine prolongs atrial and ventricular refractoriness, induces PRR and reduces TDR. Ranolazine, however, does not modify cardiac contractility, AVN conduction or blood pressure.
Effects on Atrial Fibrillation
In experimental models, vernakalant dose-dependently prolongs atrial APD and refractoriness, slows intra-atrial conduction, induces PRR, suppresses EADs and DADs elicited in pulmonary vein sleeves and terminates and/or prevents initiation of AF [43]. The combination of ranolazine with dronedarone or amiodarone induces potent synergistic use-dependent atrial-selective depression of Na+ channel-mediated parameters, markedly increases PRR, and prevents the induction of AF.
In small uncontrolled trials, ranolazine (500–1000 mg bid) was effective to maintain SR in patients with recurrent AF despite AF ablation and AAD therapy, facilitates electrical cardioversion in cardioversion-resistant patients, prevents post-operative AF and at high doses (2 g p.o.) produces the conversion of recent-onset AF (<48 h duration) [45, 46]. In patients with unstable angina and non-ST-segment elevation myocardial infarction, ranolazine tended to reduce the episodes of AF as compared with placebo [47].
In a meta-analysis of eight trials in patients with preserved LVEF and recent-onset AF, ranolazine significantly reduces the incidence of AF compared to the control group in various clinical settings (i.e., after cardiac surgery, acute coronary syndromes, post-electrical cardioversion of AF). In the RAFAELLO study, ranolazine (375–750 mg bid) does not prolong the time to AF recurrence as compared to placebo [48], while in the HARMONY trial the combination of ranolazine (750 mg bid) and low doses of dronedarone (225 mg bid), but not each drug in monotherapy, significantly reduces AF burden vs placebo in patients with paroxysmal AF [49].
Effects on Ventricular Arrhythmias
Ranolazine suppresses experimental ventricular arrhythmias associated with reduced repolarization reserve due to an increased INaLand/or reduced IKr. In patients with unstable angina and non-ST-segment elevation myocardial infarction, ranolazine significantly reduces the incidence of non-sustained VT, SVT, bradycardias or pauses as compared with placebo, but not sudden cardiac death [47]. In LQT3 patients with the SCN5A-ΔKPQ mutation and an increased INaL, I.V. ranolazine shortens the QTc interval without changes in PR and QRS intervals, AV conduction or blood pressure, and improves diastolic dysfunction [50]. Thus, ranolazine may be considered as add-on therapy to shorten the QT interval in LQTS3 patients with a QTc >500 ms [51].
Drug Interactions
Ranolazine is a moderate/potent inhibitor of P-gp and a mild inhibitor of CYP3A4 [20]. Avoid the administration of ranolazine with strong CYP3A inhibitors/inducers; limit the dose to 500 mg bid in patients on moderate CYP3A inhibitors (Table 6.5). Dose adjustment of CYP3A4 substrates (atorvastatin, lovastatin, simvastatin; limit the dose of simvastatin to 20 mg od), particularly of drugs with a narrow therapeutic range (e.g. cyclosporin, everolimus, sirolimus, tacrolimus), may be required when coadminstred with ranolazine. Monitor the plasma levels of the immunosuppressants when coadminstred with ranolazine. Ranolazine increases the exposure to digoxin. Exposure to CYP2D6 substrates (e.g. tricyclic antidepressants, antipsychotics) may be increased by ranolazine, and lower doses of these drugs may be required. Ranolazine also increases plasma levels of digoxin and metformin (metformin dose should not exceed 1700 mg/day when ranolazine is administered at 1000 mg bid). There is a theoretical risk that concomitant treatment of ranolazine with other drugs known to prolong the QTc interval may give rise to a pharmacodynamic interaction and increase the possible risk of ventricular arrhythmias. There is a theoretical risk that concomitant treatment of ranolazine with other drugs known to prolong the QTc interval may give rise to a pharmacodynamic interaction and increase the possible risk of ventricular arrhythmias.
Clinical Indications
Ranolazine is well tolerated, does not produce significant hemodynamic, organ toxicity or pro-arrhythmic effects and its effects are more pronounced on atrial than on ventricular myocardium. Thus, it may represent a promising new AAD in patients with paroxysmal and persistent AF and structural heart diseases associated with an increase in INaL, where most AADs are contraindicated, SVT and ventricular arrhythmias. However, long-term RCTs are needed that confirm the efficacy and safety of ranolazine for the cardioversion of AF and the maintenance of SR in these patients.
Selective If Blockers: Ivabradine
Elevated resting heart rate is an independent risk factor of cardiovascular morbidity and mortality in the general population and in patients with cardiovascular diseases. Ivabradine is an antianginal drug that selectively inhibits the cardiac pacemaker current (I) which is responsible for normal automaticity of the sinus node and reduces heart rate in a dose-dependent manner, without influencing intracardiac conduction velocity or refractoriness, myocardial contractility and blood pressure [52].
The off-label use of ivabradine in small trials recruiting patients with inappropriate sinus tachycardia (IST) in response to exercise or orthostatic challenge reduced maximum/minimum heart rate and symptoms during exercise or daily activity and improved exercise tolerance in stress tests and quality of life with an efficacy comparable with placebo or other therapies, but is better tolerated than metoprolol [52,53,54]. A persistent clinical benefit was observed in some patients even after discontinuing the drug. Thus, ivabradine is recommended for symptomatic patients with IST [10, 11]. However, this is not an FDA/EMA-approved indication of ivabradine. Potential mechanisms of the antiarrhythmic effects of ivabradine includes If inhibition, reduction of cardiomyocyte Ca2+ overload and APD prolongation induced by heart rate reduction. Ivabradine may also be effective in focal AT, but there are limited data of the efficacy of ivabradine in the treatment of postural orthostatic tachycardia syndrome, sinus tachycardia after ablation of the AVNRT and refractory junction ectopic tachycardia [10, 11, 55]. Thus, larger prospective comparative studies are needed to establish the antiarrhythmic efficacy and safety of ivabradine. However, by breaking the pressure homeostatic loop, the selective blockade of If is associated with a reflex increase in the activity of sympathetic efferent fibres [56]. Thus, ideally ivabradine should be preferably co-administered with a β-blocker when possible under close monitoring for the possibility of excess bradycardia; this combination may also be more beneficial than each drug alone for IST [10, 11].
Drug Interactions
Ivabradine is metabolized via cytochrome CYP3A4 and it should be avoided or used with caution with potent CYP44A inhibitors/inducers (Table 6.5) [20]. Increased plasma concentrations of ivabradine may be associated with excessive bradycardia. Ranolazine is partially metabolised by CYP2D6 and potent CYP2D6 may increase its plasma concentrations. Ranolazine is also a mild inhibitor of CYP2D6 and exposure to CYP2D6 substrates (e.g. cyclophosphamide, efavirenz, flecainide, metoprolol, propafenone or tricyclic antidepressants and antipsychotics) may be increased by ivabradine, so that lower doses of these drugs may be required. Ivabradine should not be taken during pregnancy or breastfeeding [21].
Gap-Junction Coupling Enhancers
Coordinated cardiac impulse conduction is a function of membrane excitability which depends on Na+ or Ca2+ channel activity, intercellular coupling of cardiomyocytes via low resistance connections (gap-junctions), and tissue architecture mainly determined by fibrosis [57]. Gap junction channels are composed of two hemichannels (connexons), formed from six connexin molecules, provided by either of the adjacent cells. The major connexins (Cx40, Cx43, and Cx45) are expressed in a chamber-specific manner. Cx43 is found in ventricles and atria, Cx40 in the atria and specific conduction system and Cx45 in the conduction system, SAN and ANV. Cellular uncoupling due to changes in Cx expression (resulting in irregular activation patterns), location (lateralization) and function occur in many forms of heart disease (i.e., ischemia, cardiac hypertrophy, HF and AF) and contribute to cardiac arrhythmias as they slow intracardiac conduction, increase repolarization heterogeneity and modulate automaticity. Cellular uncoupling together with increased fibrosis and decreased expression of Na+ channels, are implicated in conduction slowing during ischemia, increasing the risk of fatal ventricular arrhythmias [57, 58].
Small-molecules that enhance gap-junction conductance have been developed in an attempt to improve conduction, eliminate functional block and suppress reentry [59]. The hexapepide rotigaptide and its dipeptide analogue danegaptide, increase gap-junction conductance (electrical coupling) acting via Cx43 and Cx45 gap junctions and may represent a novel therapeutic strategy to improve conduction, eliminate functional block and abolish reentry. Both drugs improve conduction during acidosis, acute metabolic stress or myocardial ischemia without affecting sarcolemmal ion channels or cardiac contractility and suppress reentrant ventricular tachyarrhythmias during ischemia-reperfusion. However, rotigaptide partially reverses the loss of Cx43 and does not restore normal conduction or prevent arrhythmias in the healing infarct border zone, i.e. after a prolonged period of gap-junction remodeling, is ineffective against focal ventricular tachyarrhythmias and does not suppress triggered arrhythmias. Gap-junction enhancers can also reduce AF vulnerability in some models (chronic mitral regurgitation, acute ischemia, sterile pericarditis), but not in HF or atrial tachypacing models, and it is unclear whether they are equally effective in chronically remodelled atria. Therefore, gap-junction enhancers may be only effective when alterations in gap-junctions are responsible for conduction slowing, but not when conduction slowing is mainly due to decreased Na+ channel availability or structural remodeling (fibrosis). Furthermore, their electrophysiological effects when connexins are re-distributed but their expression and function remains unaltered is uncertain and there are concerns about their safety because theoretically, pharmacological restoration of intercellular coupling may destabilize re-entry and be proarrhythmic.
Na+/Ca2+ Exchanger (NCX) Inhibitors
The NCX is a bidirectional electrogenic transporter (Ca2+:3Na+) producing a net current in the direction of Na+ transport [60]. During the upstroke of the action potential the large influx of Na+ via the INa increases the [Na+]i and the NCX functions in the reverse mode (Na+ out/Ca2+ in), generating an outward repolarizing current. During the plateau and early diastole, there is a large influx of Ca2+ via the ICa, the [Ca2+]i raises and the NCX functions in the forward mode (Ca2+ out/Na+ in) which in conjunction with the sarcoplasmic reticulum Ca2+ uptake (via SERCA2a) facilitates cardiac relaxation and maintains intracellular Ca2+ balance.
The reverse mode is favoured by membrane depolarization and increased [Na+]i (rapid pacing, sympathetic stimulation, ischemia/reperfusion, digitalis intoxication) promoting Ca2+ influx and cellular Ca2+ overload leading to contractile failure (abnormally slow relaxation) and triggered arrhythmias. NCX is overexpressed in patients with HF or cardiac hypertrophy, which enhances Ca2+ extrusion, compensates the reduced removal of Ca2+ from the cytosol due to reduced SERCA2a activity, prolongs the APD and contributes to the spontaneous release of Ca2+ from the sarcoplasmic reticulum and to the appearance of DADs. DADs arise from uncontrolled spontaneous Ca2+ release from the sarcoplasmic reticulum under conditions of abnormal Ca2+ overload and/or dysfunction of sarcoplasmic reticulum Ca2+ release (RYR2) channels (ischemia-reperfusion, HF, LV hypertrophy, catecholamine-induced polymorphic VT) [61]. The increase of [Ca2+]i activates the forward mode of the NCX and generates a transient inward depolarizing current (ITI) that generates DADs and phase 3 EADs.
Inhibition of reverse NCX might be a novel antiarrhythmic strategy to reduce intracellular Ca2+ overload and suppress triggered activity under pathological conditions, while blockade of the forward mode at resting membrane potentials reduces Ca2+ extrusion and promotes intracellular Ca2+ overload [60, 61]. Therefore, a unique desirable property of NCX inhibitors will be the preferential inhibition of the reverse NCX based in the asymmetric nature of the cotransporter (i.e. different sensitivity for Na+ and Ca2+ at the opposite sides of the membrane), but the lack of structural information about the mammalian cardiac NCX is a major drawback to achieving this goal. Currently available NCX inhibitors present limited selectivity with additional benefit arising from off-target effects as they inhibit other cardiac channels, which may explain the contradictory results in the treatment of ischemic-reperfusion injury and triggered activity. Additionally, no proof-of-concept clinical studies are not available.
References
DiMarco JP. Adenosine and digoxin. In: Zipes DP, Jalife J, editors. Cardiac electrophysiology: from cell to bedside. 3rd ed. Philadelphia: Saunders; 2000. p. 933–8.
Layland J, Carrick D, Lee M, Oldroyd K, Berry C. Adenosine. Physiology, pharmacology, and clinical applications. JACC Cardiovasc Interv. 2014;7:581–91.
Lerman BB, Markowitz SM, Cheung JW, Liu CF, Thomas G, Ip JE. Supraventricular tachycardia. Mechanistic insights deduced from adenosine. Circ Arrhythm Electrophysiol. 2018;11:e006953.
DiMarco JP, Miles W, Akhtar M, Milstein S, Sharma AD, Platia E, et al. Adenosine for paroxysmal supraventricular tachycardia: dose ranging and comparison with verapamil. Assessment in placebo-controlled, multicenter trials. The Adenosine for PSVT Study Group. Ann Intern Med. 1990;113:104–10.
Camm AJ, Garratt CJ. Adenosine and supraventricular tachycardia. N Engl J Med. 1991;325:1621–9.
Brady WJ, DeBehnke DJ, Wickman LL, Lindbeck G. Treatment of out-of-hospital supraventricular tachycardia: adenosine vs verapamil. Acad Emerg Med. 1996;3:574–85.
Markowitz SM, Stein KM, Mittal S, Slotwtner DJ, Lerman BB. Differential effects of adenosine on focal and macroreentrant atrial tachycardia. J Cardiovasc Electrophysiol. 1999;10:489–502.
Glatter KA, Cheng J, Dorostkar P, Modin G, Talwar S, Al-Nimri M, et al. Electrophysiologic effects of adenosine in patients with supraventricular tachycardia. Circulation. 1999;99:1034–40.
Delaney B, Loy J, Kelly A-M. The relative efficacy of adenosine versus verapamil for the treatment of stable paroxysmal supraventricular tachycardia in adults: a meta-analysis. Eur J Emerg Med. 2011;18:148–52.
Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016;67:1575–623.
Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, et al.; ESC Scientific Document Group. 2019 ESC guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2019. pii: ehz467. https://doi.org/10.1093/eurheartj/ehz467.
Kall JG, Kopp D, Olshansky B, Kinder C, O’Connor M, Cadman CS, et al. Adenosine-sensitive atrial tachycardia. Pacing Clin Electrophysiol. 1995;18:300–6.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC)Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESCEndorsed by the European Stroke Organisation (ESO). Eur Heart J. 2016;37:2893–962.
Pelleg A, Pennock RS, Kutalek SP. Proarrhythmic effects of adenosine: one decade of clinical data. Am J Ther. 2002;9:141–7.
Fragakis N, Antoniadis AP, Korantzopoulos P, Kyriakou P, Koskinas KC, Geleris P. Sinus nodal response to adenosine relates to the severity of sinus node dysfunction. Europace. 2012;14:859–64.
Ellenbogen KA, Thames MD, DiMarco JP, Sheehan H, Lerman BB. Electrophysiological effects of adenosine in the transplanted human heart. Evidence of supersensitivity. Circulation. 1990;81:821–8.
Ip JE, Cheung JW, Chung JH, Liu CF, Thomas G, Markowitz SM, et al. Adenosine-induced atrial fibrillation. Insights into mechanism. Circ Arrhythm Electrophysiol. 2013;6:e34–7.
Li N, Csepe TA, Hansen BJ, Sul LV, Kalyanasundaram A, Zakharkin SO, et al. Adenosine-induced atrial fibrillation. Localized reentrant drivers in lateral right atria due to heterogeneous expression of adenosine A1 receptors and GIRK4 subunits in the human heart. Circulation. 2016;134:486–98.
Garratt CJ, Griffith MJ, O’Nunain S, Ward DE, Camm AJ. Effects of intravenous adenosine on antegrade refractoriness of accessory atrioventricular connections. Circulation. 1991;84:1962–8.
Tamargo J, Caballero R, Delpón E. Cardiovascular drugs-from A to Z. In: Kaski JC, Kjeldsen KP, editors. The ESC handbook on cardiovascular pharmacotherapy. Oxford: Oxford University Press; 2019. p. 423–808.
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cıfkova R, De Bonis M, et al. ESC Scientific Document Group. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39:3165–241.
Müller C, Jacobson KA. Recent developments in adenosine receptor ligands and their potential as novel drugs. Biochim Biophys Acta. 2011;1808:1290–308.
The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–33.
Gheorghiade M, van Veldhuisen DJ, Colucci WS. Contemporary use of digoxin in the management of cardiovascular disorders. Circulation. 2006;113:2556–64.
Tamargo J, Delpón E, Caballero R. The safety of digoxin as a pharmacological treatment of atrial fibrillation. Expert Opin Drug Saf. 2006;5:453–67.
Arispe N, Diaz JC, Simakova S, Pollard HB. Digitoxin induces calcium uptake into cells by forming transmembrane calcium channels. Proc Natl Acad Sci U S A. 2008;105:2610–5.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. ACC/AHA Task Force Members. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–4.
Sellers TD Jr, Bashore TM, Gallagher JJ. Digitalis in the pre-excitation syndrome. Analysis during atrial fibrillation. Circulation. 1977;56:260–7.
Sheinman BD, Evans T. Acceleration of ventricular rate by fibrillation associated with the Wolff-Parkinson-White syndrome. Br Med J (Clin Res Ed). 1982;285:999–1000.
Khand AU, Rankin AC, Martin W, Taylor J, Gemmell I, Cleland JG. Carvedilol alone or in combination with digoxin for the management of atrial fibrillation in patients with heart failure? J Am Coll Cardiol. 2003;42:1944–51.
Shettiggar UR, Toole JG, Appunn DO. Combined use of esmolol and digoxin in the acute treatment of atrial fibrillation or flutter. Am Heart J. 1993;126:368–74.
Roy D, Talajic M, Nattel S, Atrial Fibrillation and Congestive Heart Failure Investigators, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358:2667–77.
Deedwania PC, Singh BN, Ellenbogen K, Fisher S, Fletcher R, Singh SN. Spontaneous conversion and maintenance of sinus rhythm by amiodarone in patients with heart failure and atrial fibrillation: observations from the veterans affairs congestive heart failure survival trial of antiarrhythmic therapy (CHF-STAT). The Department of Veterans Affairs CHF-STAT Investigators. Circulation. 1998;98:2574–9.
Turakhia MP, Santangeli P, Winkelmayer WC, Xu X, Ullal AJ, Than CT, et al. Increased mortality associated with digoxin in contemporary patients with atrial fibrillation: findings from the TREAT-AF study. J Am Coll Cardiol. 2014;64:660–8.
Vamos M, Erath JW, Hohnloser SH. Digoxin-associated mortality: a systematic review and meta-analysis of the literature. Eur Heart J. 2015;36:1831–8.
Ziff OJ, Lane DA, Samra M, Griffith M, Kirchhof P, Lip GY, et al. Safety and efficacy of digoxin: systematic review and meta-analysis of observational and controlled trial data. BMJ. 2015;351:h4451.
Ahmed A, Rich MW, Love TE, Lloyd-Jones DM, Aban IB, Colucci WS, et al. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J. 2006;27:178–86.
Antzelevitch C, Burashnikov A, Sicouri S, Belardinelli L. Electrophysiological basis for the antiarrhythmic actions of ranolazine. Heart Rhythm. 2011;8:1281–90.
Fedida D. Vernakalant (RSD1235): a novel, atrial-selective antifibrillatory agent. Expert Opin Investig Drugs. 2007;16:519–32.
Guerra F, Matassini MV, Scappini L, Urbinati A, Capucci A. Intravenous vernakalant for the rapid conversion of recent onset atrial fibrillation: systematic review and meta-analysis. Expert Rev Cardiovasc Ther. 2014;12:1067–75.
Akel T, Lafferty J. Efficacy and safety of intravenous vernakalant for the rapid conversion of recent-onset atrial fibrillation: a meta-analysis. Ann Noninvasive Electrocardiol. 2018;23:e12508.
Camm AJ, Capucci A, Hohnloser SH, Torp-Pedersen C, Van Gelder IC, Mangal B, et al. A randomized active-controlled study comparing the efficacy and safety of vernakalant to amiodarone in recent-onset atrial fibrillation. J Am Coll Cardiol. 2011;57:313–21.
Tamargo J, Caballero R, Delpón E. Ranolazine: an antianginal drug with antiarrhythmic properties. Expert Rev Cardiovasc Ther. 2011;9:815–27.
Bengel P, Ahmad S, Sossalla S. Inhibition of late sodium current as an innovative antiarrhythmic strategy. Curr Heart Fail Rep. 2017;14:179–86.
Gong M, Zhang Z, Fragakis N, Korantzopoulos P, Letsas KP, Li G, et al. Role of ranolazine in the prevention and treatment of atrial fibrillation: a meta-analysis of randomized clinical trials. Heart Rhythm. 2017;14:3–1.
White CM, Nguyen E. Novel use of ranolazine as an antiarrhythmic agent in atrial fibrillation. Ann Pharmacother. 2017;51:245–52.
Morrow DA, Scirica BM, Karwatowska-Prokopczuk E, Murphy SA, Budaj A, Varshavsky S, et al. Effects of ranolazine on recurrent cardiovascular events in patients with non-ST-elevation acute coronary syndromes: the MERLIN-TIMI 36 randomized trial. JAMA. 2007;297:1775–83.
De Ferrari GM, Maier LS, Mont L, Schwartz PJ, Simonis G, Leschke M, et al. RAFFAELLO Investigators. Ranolazine in the treatment of atrial fibrillation: results of the dose-ranging RAFFAELLO (Ranolazine in Atrial Fibrillation Following An ELectricaL CardiOversion) study. Heart Rhythm. 2015;12:872–8.
Reiffel JA, Camm AJ, Belardinelli L, Zeng D, Karwatowska-Prokopczuk E, Olmsted A, et al. HARMONY Investigators. The HARMONY Trial: combined ranolazine and dronedarone in the management of paroxysmal atrial fibrillation: mechanistic and therapeutic synergism. Circ Arrhythm Electrophysiol. 2015;8:1048–56.
Moss AJ, Zareba W, Schwarz KQ, Rosero S, McNitt S, Robinson JL. Ranolazine shortens repolarization in patients with sustained inward sodium current due to type-3 long-QT syndrome. J Cardiovasc Electrophysiol. 2008;19:1289–93.
Priori S, Blomstroöm-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2015;36:2793–867.
Koruth JS, Lala A, Pinney S, Reddy VY, Dukkipati SR. The clinical use of ivabradine. J Am Coll Cardiol. 2017;70:1777–84.
Cappato R, Castelvecchio S, Ricci C, Bianco E, Vitali-Serdoz L, Gnecchi-Ruscone T, et al. Clinical efficacy of ivabradine in patients with inappropriate sinus tachycardia: a prospective, randomized, placebo-controlled, double-blind, crossover evaluation. J Am Coll Cardiol. 2012;60:1323–9.
Ptaszynski P, Kaczmarek K, Ruta J, et al. Metoprolol succinate vs. ivabradine in the treatment of inappropriate sinus tachycardia in patients unresponsive to previous pharmacological therapy. Europace. 2013;15:116–21.
Sheldon RS, Grubb BP 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, et al. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015;12:e41–63.
Dias da Silva VJ, Tobaldini E, Rocchetti M, Wu MA, Malfatto G, Montano N, et al. Modulation of sympathetic activity and heart rate variability by ivabradine. Cardiovasc Res. 2015;108:31–8.
Kleber AG, Rudy Y. Basic mechanisms of cardiac impulse propagation and associated arrhythmias. Physiol Rev. 2004;84:431–88.
Noorman M, van der Heyden MA, van Veen TA, Cox MG, Hauer RN, de Bakker JM, et al. Cardiac cell-cell junctions in health and disease: electrical versus mechanical coupling. J Mol Cell Cardiol. 2009;47:23–31.
Dhein S, Hagen A, Jozwiak J, Dietze A, Garbade J, Barten M, et al. Improving cardiac gap junction communication as a new antiarrhythmic mechanism: the action of antiarrhythmic peptides. Naunyn Schmiedeberg’s Arch Pharmacol. 2010;381:221–34.
Shattock MJ, Ottolia M, Bers M, Blaustein MP, Boguslavskyi A, Bossuyt J, et al. Na+/Ca2+ exchange and Na+/K+-ATPase in the heart. J Physiol. 2015;593:1361–82.
Antoons G, Willems R, Sipido KR. Alternative strategies in arrhythmia therapy: evaluation of Na/Ca exchange as an anti-arrhythmic target. Pharmacol Ther. 2012;134:26–42.
Acknowledgments
We thank P Vaquero for her invaluable technical assistance. This work was supported by grants from the Ministerio de Ciencia e Innovación (SAF2017-88116-P), Instituto de Salud Carlos III [PI16/00398 and CIBER-Cardiovascular (CB16/11/00303)] and Comunidad de Madrid (B2017/BMD-3738).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tamargo, J. (2020). Other Antiarrhythmic Drugs. In: Martínez-Rubio, A., Tamargo, J., Dan, G . (eds) Antiarrhythmic Drugs. Current Cardiovascular Therapy. Springer, Cham. https://doi.org/10.1007/978-3-030-34893-9_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-34893-9_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34891-5
Online ISBN: 978-3-030-34893-9
eBook Packages: MedicineMedicine (R0)