Abstract
Control of calcium (Ca2+) homeostasis is central to all living cells, since significant deviations from physiological Ca2+ fluctuations may have deleterious consequences on the cell fate. The Na+/Ca2+ exchanger (NCX) is a master modulator of Ca2+ cycling both in physiological and pathological settings. Our research group has been working for several years on the role of NCX in physiological and pathological conditions, with special regard to the ischemic settings, where derangements in Ca2+ homeostasis dictate the transition from reversible to irreversible cell damage. In this chapter, we present a detailed description of the role played by NCX during hypoxia/reoxygenation (H/R) injury, with a focus on the different contribution of this exchanger in driving cells towards cell survival or death pathways, depending on the context within which it is operating. In this scenario, the major innovation that we describe with a special emphasis is the relationship between NCX and the Na+-dependent glutamate transporters, a physical and functional coupling impacting on critical cell functions, such as the stimulation of the oxidative metabolism. During the last few years we further explored this finding and focused on the potential of such metabolic interplay to counteract H/R-induced cell injury in cardiac and neuronal models.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Intracellular Calcium Homeostasis: Role of the Na+/Ca2+ Exchanger 1 (NCX1)
Calcium (Ca2+) ion flows across the cell membrane and organelles are vital components of signaling networks controlling cardiac cell activities [12]. From the first to the last heartbeat, that flow of Ca2+ is orchestrated by membrane transporters and channels, which coordinate processes of Ca2+ uptake, storage, and release during each excitation-contraction coupling cycle [2, 12]. When Ca2+ transients deviate from physiological patterns, both cardiac functions and even cardiomyocyte survival may be compromised [15]. In particular, during ischemia abnormal Ca2+ handling ignites cardiomyocyte damage that swiftly progresses towards a more extensive myocardial injury even when perfusion is restored, giving rise to the composite ischemia/reperfusion (I/R) injury. Based on the above, strategies that ultimately normalize Ca2+ load have therapeutic potential [16].
The Na+/Ca2+ exchanger 1 (NCX1) is a key modulator of Ca2+ cycling in cardiac cells, both in physiological and pathological settings [1]. NCX1 catalyzes the reversible exchange of 3 Na+ for 1 Ca2+, facilitating either the influx (reverse mode) or the extrusion (forward mode) of Ca2+. The transition from forward to reverse mode exchange primarily depends on the chemical gradients of the substrate ions and membrane potential [3, 43]. Mammals express three different NCX gene products (namely NCX1, NCX2, and NCX3) in a tissue-specific manner. NCX1 is ubiquitously expressed in all tissues, NCX2 is mainly restricted to the brain, and NCX3 is expressed exclusively in the brain and skeletal muscles [48]. Both NCX1 and NCX3 are modified by alternative splicing [33, 48]. These transporters share an overall sequence identity of ~70% [32], adopt a similar architecture of ten transmembrane domains (containing the ion-transport regions), and possess a large cytosolic loop, which is responsible for secondary regulation elicited by several cytoplasmic messengers [32, 43]. The ion-transport rates and secondary regulation can be substantially different among NCX isoforms and their splicing variants [33], and these distinctive properties may adapt the NCX function to cell-specific dynamics of Ca2+ waves and oscillations in health and disease.
2 Role of NCX1 in Hypoxia/Reoxygenation (H/R) and in Ischemic Preconditioning (IPC)
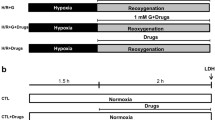
In the heart, NCX1 influences diverse functions of cardiac cells, including excitation-contraction coupling [40], nodal pace-maker activity [14, 56] and cell metabolism [25, 29]. During an ischemic event, a shortage of oxygen and substrates supply will inevitably impair energy production, and consequently lead to Na+ accumulation and membrane depolarization [18]. In this scenario, Ca2+ entry through the reverse-mode activity of NCX1 is enhanced. During reperfusion, the abrupt alleviation of tissue acidosis and washout of extracellular H+ establish a favorable gradient for Na+ influx via the Na+/H+ exchanger. Such Na+ accumulation further increases Ca2+ entry or decreases Ca2+ extrusion via NCX1, and the dramatic gain in intracellular Ca2+ load further aggravates the pre-existing injury towards more severe contractile dysfunction, electrical instability and death of cardiac cells [6, 22, 47]. In the last few years, our research group made great efforts in confirming the deleterious role of NCX1 in cardiac I/R injury, and different experimental models have been developed to this purpose. For instance, in rat adult cardiomyocytes and in the whole heart exposed to specific hypoxia/reoxygenation (H/R) protocols [5], we found that the benzyloxyphenyl derivative SN-6 (Niu et al. 2007)—an inhibitor with increased selectivity for NCX1 in condition of ATP depletion [17]—significantly ameliorates the cell damage occurring after H/R challenge [5]. We also established an in vitro model of H/R based on the rat cardiomyoblast H9c2 cell line. With the intent to emphasize the exchanger role within this pathological context, we used two different clones: H9c2 wild-type (H9c2-WT), not expressing endogenous NCX1, and H9c2-NCX1, generated from H9c2-WT and stably expressing canine NCX1 [27]. While in both phenotypes cell viability was significantly affected by H/R challenge, we interestingly observed that in H9c2-NCX1 cells injury was of a much greater extent than in H9c2-WT cells. This result reflects the tendency of NCX to work in a Ca2+-influx mode under hypoxic conditions, thereby favoring a deleterious intracellular Ca2+ accumulation. The increased NCX1 expression and reverse-mode activity observed after H/R challenge lend further support to this hypothesis. It is widely described that, in this setting, strategies that ultimately inhibit the exchanger can improve cell survival and cardiac functions [6, 37, 53]. However, our experimental experience also indicates that NCX activity may be essential to drive the cells towards survival pathways, leading to the concept that the exchanger role depends on the pathophysiological context within which it is operating. It is well known that short periods of subcritical ischemic stimuli preceding the index ischemia—also known as ischemic preconditioning (IPC)—can confer protection from lethal injury [36]. Pieces of laboratory experience indicate that transient and reversible raises in intracellular Ca2+ levels can reproduce the protective effect of the IPC [30, 34]. In our experience, NCX1 pharmacological inhibition, during a series of brief hypoxia-reoxigenation cycles, not only abolishes IPC cardioprotective effect, but also causes an exacerbation of the H/R-induced cardiomyocytes injury [5].
Overall, the findings reported above lead us to conclude that NCX1 may play a dual role in ischemic settings: on one hand, its inhibition during I/R may be crucial to cell survival, on the other hand, its activity during IPC may serve as a trigger for the induction of ischemic tolerance.
3 Metabolic Role of NCX1 During H/R: The Interplay with Glutamate and the Excitatory Amino Acids Transporters (EAATs)
The heart is capable of consuming a number of different substrates, therefore it is well known as a “metabolic omnivore” [11]. During ischemia, the reduction of blood flow causes a restriction in both supplies and oxygen to the heart, leading to significant alterations of the myocardial metabolism. The continuous deficiency of oxygen shifts cardiac metabolism towards anaerobic glycolysis and disrupts ATP generation through the mitochondrial oxidative phosphorylation, ultimately leading to ionic imbalance and cell damage. Although reperfusion may be detrimental, a prompt restoration of blood flow is crucial for the conversion from reversible to irreversible injury of a population of cardiomyocytes that have been severely impaired during the prior period of ischemia. Indeed, the restoration of the oxygen flow is a pre-requisite to recover oxidative metabolism, thereby favoring cell survival. This may be accomplished by supplying energy substrates to the ischemic tissue during the reperfusion phase. For instance, glutamate has been recognized as a critical compound that can be preferentially used as anaplerotic substrate in the tricarboxylic acid (TCA) cycle during anoxia and ischemia [11]. In this regard, over the last thirty years, several studies have outlined the cardioprotective effect of glutamate supplementation under ischemic conditions [23, 46, 55, 59].
One of the main finding that our research group has pointed out is that, under physiological conditions, in purified mitochondria from different tissues and in the whole cell, glutamate significantly stimulates ATP de novo synthesis. Even more importantly, in this setting, glutamate entry into the mitochondria does not rely on the activity of the well-known aspartate/glutamate carriers [13, 41], but rather on the activity of the Na+-dependent Excitatory Amino Acid Transporters (EAATs) [7, 25, 26], whose activity we have found to be strongly related to NCX. The pathophysiological significance and metabolic relevance of such interaction will be further discussed in the following sections.
3.1 NCX-EAAT Interplay Under Normoxic Conditions
EAATs are secondary active transporters that couple the accumulation of glutamate in the cytoplasm to downhill movement of co-transported ions along their concentration gradient [7]. Specifically, the co-transport of three Na+ ions and one H+ drives EAATs glutamate uptake, as well as the counter-transport of one K+ ion. To date, five EAATs subtypes (1–5) have been identified and cloned from mammalian tissues. They include: EAAT1 (rodent homologue: GLAST, GLutamate-ASpartate Transporter), which is highly expressed in the neocortex and cerebellum, especially in astrocytes [38]; EAAT2 (rodent homologue: GLT1, GLutamate Transporter 1), which is the main glutamate transporter found in the forebrain, abundantly expressed in astrocytes and in a limited extent also on presynaptic nerve terminals [31, 38]; EAAT3 (rodent homologue: EAAC1), which appears to be neuron-specific [52]; EAAT4, which is neuron-specific and has an expression profile restricted to Purkinje cells [7, 19]; and finally, EAAT5, selectively expressed at photoreceptor and bipolar cell terminals in the retina [7]. In 2004, for the first time, Ralphe and colleagues described brain EAAT1 localization in cardiac mitochondria [49, 50]. Considering that the transport across membranes expressing EAATs may alter the Na+ gradient used to move glutamate, there should be a mechanism able to restore and maintain the Na+ driving force for efficient substrate translocation. It has been already proposed that glutamate and Na+ entry via EAAT induces a Ca2+ response due to the reverse mode of plasma membrane NCX [21]. However, our group for the first time showed a selective interaction between a specific EAAT subtype, EAAT3/EAAC1, and a specific NCX subtype, NCX1 both at the cytosolic and mitochondrial level. Their physical association, disclosed by colocalization, coimmunoprecipitation and mutual activity dependency, emphasizes the high selectivity of this interaction, which represents a novel and complementary mechanism enhancing cell metabolism to meet the increased energy demand in neuronal, glial and cardiac models [25, 26, 28].
As mentioned above, our earlier studies indicate that, under physiological conditions, glutamate supplementation significantly stimulates cell metabolism, leading to a rise in ATP content. The most interesting finding is that the metabolic response evoked by glutamate is strictly dependent on EAAT (in particular on EAAT3/EAAC1) activity. However, this transport system cannot ensure by itself an effective glutamate uptake capable to “drive” ATP synthesis: its activity should be functionally supported by NCX1 reverse-mode activity, which balances intracellular Na+ levels after glutamate uptake. As a consequence, the cytoplasmic concentrations of Ca2+ may increase and a parallel rise in mitochondrial Ca2+ concentrations may occur, thus activating the intramitochondrial Ca2+-sensitive dehydrogenases [8]. The activation of these enzymes is important in the stimulation of the respiratory chain and hence ATP supply under conditions of increased energy demand. In this connection, the anaplerotic use of glutamate may contribute to boost energy metabolism with a concomitant increase in ATP synthesis.
Overall, our studies outline an alternative metabolic pathway in which glutamate serves as a fuel to produce energy in an EAAT-NCX dependent-fashion. Thus, the EAAT3/EAAC1-NCX1 dependent influx pathway, which plays a crucial role in the glutamate-dependent metabolic response in physiological conditions [25, 26, 28], may also have important implications in pathological settings (i.e. ischemia/reperfusion), where substantial changes in energy metabolism occur as a consequence of the reduced oxygen availability.
3.2 NCX-EAAT Interplay in Cardiac Hypoxia/Reoxygenation Injury
As aforementioned, several studies indicate that glutamate supplementation during early post-ischemic reperfusion may ameliorate cardiomyocytes survival and cardiac functions. Our preliminary studies on the metabolic significance of the NCX-EAAT interplay in normoxia encouraged us to get on with the following issues: (1) to explore the mechanisms underlying the protective effect of glutamate in ischemic settings (2) to evaluate the possible involvement of the EAAT-NCX coupling [29]. The availability of reliable cell models (i.e. H9c2 cells and rat adult cardiomyocytes) has been crucial to properly address these issues.
We report that glutamate administration, at the onset of the reoxygenation phase, fully prevents H/R damage and normalizes the exchanger reverse mode-activity. The mechanism underlying the glutamate-induced cardioprotection has been shown to be related to its ability to improve oxidative metabolism and to be closely linked to the presence of NCX1. Indeed, when NCX1 is pharmacologically inhibited, glutamate fails to exert any beneficial effect. The inability of glutamate to protect H9c2-WT from H/R damage further confirms this finding. More interestingly, glutamate protection also occurs in an EAAT-dependent manner, since the pharmacological inhibition of EAAT fully prevents glutamate actions, reinforcing the hypothesis that the interplay between EAAT and NCX is crucial to allow glutamate to be properly driven into the cells, as already reported under normoxic conditions.
Noteworthy, the same results were observed in the primary culture of rat adult cardiomyocytes, which endogenously express NCX1. In this scenario, it appears that glutamate fate is to be metabolically used to fuel cell metabolism, finally improving cell survival. It is worthwhile to mention that other complementary mechanisms may come into play. For instance, it has been recently proposed that the activation of cardiac mGluR1 at the onset of reperfusion may induce cardioprotection through the activation of the PI3Kinase/Akt survival pathway [57]. Furthermore, in an ischemic setting, glutamate improvement of cell survival may also partially depend on the ability of glutamate to improve the synthesis of scavenging molecules against reactive oxygen species, whose levels increase as the molecular oxygen is reintroduced during the recovery of blood flow [29]. Indeed, the preservation of free radical scavengers and the restoration of energetic metabolism may act as synergistic components of glutamate-induced protection.
By enhancing ATP synthesis, glutamate can exert a plethora of effects that may ultimately impact on NCX1 activity, possibly establishing a virtuous cycle. During H/R, the increased reverse-mode activity of the exchanger contributes to elevate intracellular Ca2+ levels, which may consequently activate intracellular proteolytic enzymes and cell death programs [39]. In our experience, we found that glutamate supplementation normalizes the exchanger activity. Although this was not mechanistically explored and requires a further investigation, we hypothesize that two main events may take place: first, the increased ATP production may contribute to re-establish the ionic homeostasis by supporting both Na+–K+ and Ca2+-ATPase, limiting the exchanger reverse-mode of action that is over-activated during H/R; second, the increased ATP levels triggered by glutamate, in the presence of Ca2+ transients, may evoke a rapid massive endocytosis [24] removing NCX1 from the cell surface, thereby limiting its activity. Further studies are needed to better understand the precise mechanism underlying the protection exerted by glutamate.
The role played by NCX in cardiac I/R injury is substantially different from what occurs in other pathological settings, such as in neuronal ischemia [1, 35, 45]. However, these findings led us to investigate the potential beneficial effect of glutamate also in this setting, with the purpose to shed new light on the injurious role historically ascribed to this compound [28].
3.3 NCX-EAAT Interplay in Neuronal Hypoxia/Reoxygenation Injury
Glutamate is the major excitatory amino acid in the central nervous system. It has been known for several years that, under pathological conditions (i.e. ischemia) glutamate has a neurotoxic role leading to cell death through its excessive release [58]. Indeed, the dysfunction of glutamatergic signaling is related to many debilitating diseases, therefore proper coordination and fidelity of release, activation, and reuptake of this neurotransmitter are paramount for total system homeostasis [7, 10].
The failure of clinical trials of several neuroprotective strategies, most of them targeting the excitotoxicity cascade, suggests that glutamate may have a dual and time-dependent effect in ischemic settings. Although it may be detrimental in the early phase, when physiological conditions are restored, and oxygen flow is reintroduced, glutamate may contribute to cells functional recovery through its known physiological functions. Under energy-depleted conditions, alternative energy source could be used to face the brain bioenergetic imbalance, and glutamate has proven to be an ideal substrate to fuel mitochondrial activity and rescue cells from energy impairment [42]. Thus, tight control of glutamate handling in the brain is crucial to the maintenance of cell integrity.
As mentioned above, glutamate can get access into the cells through EAATs, which primarily regulate glutamatergic neurotransmission. They accomplish these processes through a dynamic coupling of bioenergetics of the transport process and the localization of the transporters themselves. The consequence of this coupling is the creation of complex spatiotemporal profiles that modulate extracellular glutamate levels [10, 54]. The finding that EAATs also enable glutamate entry into the mitochondria points out the concept that glutamate release and recycling are part of a major metabolic pathway that cannot be distinguished from the neurotransmission activity [60].
Our previous evidence showing the functional interplay between EAAT and NCX in sustaining the metabolic use of glutamate in neuronal and glial cells [25, 26]—as well as the key role of these transporters in mediating the survival benefits provided by glutamate in cardiac cells after ischemia [29]—set the background for the results presented in this paragraph. In particular, we tried to “subvert” the traditional role of glutamate as a neurotoxic factor and explored its potential as a “survival” factor in neuronal ischemic settings. Thus, we established an in vitro neuronal model of H/R by using human SH-SY5Y neuroblastoma cells differentiated into a neuron-like state.
We interestingly observed that glutamate supplementation at the onset of the reoxygenation phase does not affect cell viability and induces a significant decrease in H/R-induced cell death [28, 44]. This protective effect of glutamate may rely on its ability to boost the oxidative phosphorylation, leading to an increase in ATP content. In this model, as well as in cardiac H/R injury, glutamate beneficial effects strictly depend on the functional and physical interaction between EAAT3/EAAC1 and NCX. Both NCX1 and EAAT3 inhibition—obtained by using both pharmacological and RNA interference approaches—prevents the beneficial effects of glutamate in terms of cell protection, recovery of ATP production and normalization of NCX reverse mode activity, which was affected by H/R challenge. Remarkably, the hypothesis of glutamate utilization as an alternative energy source is in line with recent approaches addressed to metabolically recycle the excess of glutamate released during the early phase of ischemia. It has been shown that the correction of hypoxia by supplemental oxygen during ischemic brain injury can induce the expression of the glutamate-metabolizing enzyme “glutamate oxaloacetate transaminase” (GOT) [51]. This enzyme can metabolize the otherwise extracellular neurotoxic glutamate by enabling its utilization to support survival in the face of ischemia-induced hypoglycemia [51]. As a transaminase, GOT catalyzes the transfer of the amino group from glutamate to oxaloacetate, to generate aspartate and alpha-ketoglutarate, the latter fueling the TCA cycle and sustaining cell viability. The modulation of the glutamate dehydrogenase (GDH) enzyme is a strategy that has been proposed as well. GDH is a TCA cycle enzyme that converts glutamate to alpha-ketoglutarate improving overall bioenergetics. Under energy-depleted conditions (i.e., I/R and oxygen-glucose deprivation), the modulation of GDH activity towards the utilization of glutamate seems to enhance ATP synthesis and to positively affect neuronal survival [20]. One possible explanation is that the activation of GDH may increase the influx of alpha-ketoglutarate in the TCA cycle, thereby reducing the extracellular glutamate release. The stimulation of the N-methyl-D-aspartate receptors (NMDAR) has also been recently proposed to be beneficial during the recovery period after stroke, most likely through the enhancement of neuroplasticity [9]. We believe that this is a relevant issue, as NMDAR are considered the main determinants of glutamate receptor-mediated excitotoxic mechanisms.
4 Conclusion and Future Perspectives
Overall, these new approaches reveal the potentiality of glutamate to be transformed into a “survival” factor. In this scenario, the essential role played by the EAAT3/EAAC1-NCX1 complex represents the main novelty, which further strengths our initial hypothesis considering EAAT3/EAAC1-NCX1 a dynamic interplay which supports an alternative metabolic route for glutamate utilization under stressful conditions [25, 26]. Furthermore, our findings also highlight the dual role played by Ca2+ ions: on one hand, Ca2+ may be essential to sustain ATP synthesis, on the other hand, it can be harmful, through the activation of specific cell death pathways [39]. In this scenario, NCX is the main actor. Its regulation specifically affects critical cell functions and contributes to delineate the critical point representing the boundary between Ca2+-related cytoprotective and cytotoxic effects.
We believe that our studies could also break new ground in the context of the neurodegenerative diseases [28]. During the last few years, it has become evident that metabolic alterations strongly influence the instigation and progression of many neurodegenerative disorders [4]. Decreases in glucose and oxygen metabolic rates of brain cells occur during normal aging and are further exacerbated in disorders such as Alzheimer’s, amyotrophic lateral sclerosis, Parkinson’s, and Huntington’s diseases [4]. Further studies will be needed to evaluate the potentiality of glutamate to exert beneficial actions also in these settings. This is a challenge that our research group is starting to address taking advantage of national and international partners, which already collaborate with our group. The intent is to get new insights into novel disease-modifying treatments for these irreversible, progressive neurodegenerative disorders.
References
Annunziato L, Pignataro G, Di Renzo GF (2004) Pharmacology of brain Na+/Ca2+ exchanger: from molecular biology to therapeutic perspectives. Pharmacol Rev 56:633–654
Bers DM (2008) Calcium cycling and signaling in cardiac myocytes. Annu Rev Physiol 70:23–49
Blaustein MP, Lederer WJ (1999) Sodium/calcium exchange: its physiological implications. Physiol Rev 79:763–854
Camandola S, Mattson MP (2017) Brain metabolism in health, aging, and neurodegeneration. EMBO J 36:1474–1492
Castaldo P, Macri ML, Lariccia V, Matteucci A, Maiolino M, Gratteri S, Amoroso S, Magi S (2017) Na+/Ca2+ exchanger 1 inhibition abolishes ischemic tolerance induced by ischemic preconditioning in different cardiac models. Eur J Pharmacol 794:246–256
Chen S, Li S (2012) The Na+/Ca2+ exchanger in cardiac ischemia/reperfusion injury. Med Sci Monit 18: RA161-165
Danbolt NC (2001) Glutamate uptake. Prog Neurobiol 65:1–105
Denton RM (2009) Regulation of mitochondrial dehydrogenases by calcium ions. Biochim Biophys Acta 1787:1309–1316
Dhawan J, Benveniste H, Luo Z, Nawrocky M, Smith SD, Biegon A (2011) A new look at glutamate and ischemia: NMDA agonist improves long-term functional outcome in a rat model of stroke. Future Neurol 6:823–834
Divito CB, Underhill SM (2014) Excitatory amino acid transporters: roles in glutamatergic neurotransmission. Neurochem Int 73:172–180
Drake KJ, Sidorov VY, McGuinness OP, Wasserman DH, Wikswo JP (2012) Amino acids as metabolic substrates during cardiac ischemia. Exp Biol Med (Maywood) 237:1369–1378
Fearnley CJ, Roderick HL, Bootman MD (2011) Calcium signaling in cardiac myocytes. Cold Spring Harb Perspect Biol 3:a004242
Fiermonte G, Palmieri L, Todisco S, Agrimi G, Palmieri F, Walker JE (2002) Identification of the mitochondrial glutamate transporter. Bacterial expression, reconstitution, functional characterization, and tissue distribution of two human isoforms. J Biol Chem 277:19289–19294
Gao Z, Rasmussen TP, Li Y, Kutschke W, Koval OM, Wu Y, Hall DD, Joiner ML, Wu XQ, Swaminathan PD, Purohit A, Zimmerman K, Weiss RM, Philipson KD, Song LS, Hund TJ, Anderson ME (2013) Genetic inhibition of Na+/Ca2+ exchanger current disables fight or flight sinoatrial node activity without affecting resting heart rate. Circ Res 112:309–317
Garcia-Dorado D, Ruiz-Meana M, Inserte J, Rodriguez-Sinovas A, Piper HM (2012) Calcium-mediated cell death during myocardial reperfusion. Cardiovasc Res 94:168–180
Ibanez B, Heusch G, Ovize M, Van de Werf F (2015) Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol 65:1454–1471
Iwamoto T, Kita S, Uehara A, Imanaga I, Matsuda T, Baba A, Katsuragi T (2004) Molecular determinants of Na+/Ca2+ exchange (NCX1) inhibition by SEA0400. J Biol Chem 279:7544–7553
Kalogeris T, Baines CP, Krenz M, Korthuis RJ (2012) Cell biology of ischemia/reperfusion injury. Int Rev Cell Mol Biol 298:229–317
Kanai Y, Clemencon B, Simonin A, Leuenberger M, Lochner M, Weisstanner M, Hediger MA (2013) The SLC1 high-affinity glutamate and neutral amino acid transporter family. Mol Aspects Med 34:108–120
Kim AY, Jeong KH, Lee JH, Kang Y, Lee SH, Baik EJ (2017) Glutamate dehydrogenase as a neuroprotective target against brain ischemia and reperfusion. Neuroscience 340:487–500
Kirischuk S, Kettenmann H, Verkhratsky A (2007) Membrane currents and cytoplasmic sodium transients generated by glutamate transport in Bergmann glial cells. Pflugers Arch 454:245–252
Kohajda Z, Farkas-Morvay N, Jost N, Nagy N, Geramipour A, Horvath A, Varga RS, Hornyik T, Corici C, Acsai K, Horvath B, Prorok J, Ordog B, Deri S, Toth D, Levijoki J, Pollesello P, Koskelainen T, Otsomaa L, Toth A, Baczko I, Lepran I, Nanasi PP, Papp JG, Varro A, Virag L (2016) The effect of a novel highly selective inhibitor of the sodium/calcium exchanger (NCX) on cardiac arrhythmias in in vitro and in vivo experiments. PLoS ONE 11:e0166041
Kristiansen SB, Lofgren B, Stottrup NB, Kimose HH, Nielsen-Kudsk JE, Botker HE, Nielsen TT (2008) Cardioprotection by L-glutamate during postischemic reperfusion: reduced infarct size and enhanced glycogen resynthesis in a rat insulin-free heart model. Clin Exp Pharmacol Physiol 35:884–888
Lariccia V, Fine M, Magi S, Lin MJ, Yaradanakul A, Llaguno MC, Hilgemann DW (2011) Massive calcium-activated endocytosis without involvement of classical endocytic proteins. J Gen Physiol 137:111–132
Magi S, Arcangeli S, Castaldo P, Nasti AA, Berrino L, Piegari E, Bernardini R, Amoroso S, Lariccia V (2013) Glutamate-induced ATP synthesis: relationship between plasma membrane Na+/Ca2+ exchanger and excitatory amino acid transporters in brain and heart cell models. Mol Pharmacol 84:603–614
Magi S, Lariccia V, Castaldo P, Arcangeli S, Nasti AA, Giordano A, Amoroso S (2012) Physical and functional interaction of NCX1 and EAAC1 transporters leading to glutamate-enhanced ATP production in brain mitochondria. PLoS ONE 7:e34015
Magi S, Nasti AA, Gratteri S, Castaldo P, Bompadre S, Amoroso S, Lariccia V (2015) Gram-negative endotoxin lipopolysaccharide induces cardiac hypertrophy: detrimental role of Na+/Ca2+ exchanger. Eur J Pharmacol 746:31–40
Magi S, Piccirillo S, Amoroso S (2019) The dual face of glutamate: from a neurotoxin to a potential survival factor-metabolic implications in health and disease. Cell Mol Life Sci: CMLS
Maiolino M, Castaldo P, Lariccia V, Piccirillo S, Amoroso S, Magi S (2017) Essential role of the Na+/Ca2+ exchanger (NCX) in glutamate-enhanced cell survival in cardiac cells exposed to hypoxia/reoxygenation. Sci Rep 7:13073
Meldrum DR, Cleveland JC Jr, Sheridan BC, Rowland RT, Banerjee A, Harken AH (1996) Cardiac preconditioning with calcium: clinically accessible myocardial protection. J Thorac Cardiovasc Surg 112:778–786
Mennerick S, Dhond RP, Benz A, Xu W, Rothstein JD, Danbolt NC, Isenberg KE, Zorumski CF (1998) Neuronal expression of the glutamate transporter GLT-1 in hippocampal microcultures. J Neurosci 18:4490–4499
Michel LY, Hoenderop JG, Bindels RJ (2015) Towards understanding the role of the Na+/Ca2+ exchanger isoform 3. Rev Physiol Biochem Pharmacol 168:31–57
Michel LY, Verkaart S, Koopman WJ, Willems PH, Hoenderop JG, Bindels RJ (2014) Function and regulation of the Na+/Ca2+ exchanger NCX3 splice variants in brain and skeletal muscle. J Biol Chem 289:11293–11303
Miyawaki H, Ashraf M (1997) Ca2+ as a mediator of ischemic preconditioning. Circ Res 80:790–799
Molinaro P, Cuomo O, Pignataro G, Boscia F, Sirabella R, Pannaccione A, Secondo A, Scorziello A, Adornetto A, Gala R, Viggiano D, Sokolow S, Herchuelz A, Schurmans S, Di Renzo G, Annunziato L (2008) Targeted disruption of Na+/Ca2+ exchanger 3 (NCX3) gene leads to a worsening of ischemic brain damage. J Neurosci 28:1179–1184
Murry CE, Jennings RB, Reimer KA (1986) Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 74:1124–1136
Namekata I, Shimada H, Kawanishi T, Tanaka H, Shigenobu K (2006) Reduction by SEA0400 of myocardial ischemia-induced cytoplasmic and mitochondrial Ca2+ overload. Eur J Pharmacol 543:108–115
Niciu MJ, Kelmendi B, Sanacora G (2012) Overview of glutamatergic neurotransmission in the nervous system. Pharmacol Biochem Behav 100:656–664
Orrenius S, Zhivotovsky B, Nicotera P (2003) Regulation of cell death: the calcium-apoptosis link. Nat Rev Mol Cell Biol 4:552–565
Ottolia M, Torres N, Bridge JH, Philipson KD, Goldhaber JI (2013) Na+/Ca2+ exchange and contraction of the heart. J Mol Cell Cardiol 61:28–33
Palmieri L, Pardo B, Lasorsa FM, del Arco A, Kobayashi K, Iijima M, Runswick MJ, Walker JE, Saheki T, Satrustegui J, Palmieri F (2001) Citrin and aralar 1 are Ca2+-stimulated aspartate/glutamate transporters in mitochondria. EMBO J 20:5060–5069
Pascual JM, Carceller F, Roda JM, Cerdan S (1998) Glutamate, glutamine, and GABA as substrates for the neuronal and glial compartments after focal cerebral ischemia in rats. Stroke 29:1048–1056; Discussion 1056–1047
Philipson KD, Nicoll DA (2000) Sodium-calcium exchange: a molecular perspective. Annu Rev Physiol 62:111–133
Piccirillo S, Castaldo P, Macri ML, Amoroso S, Magi S (2018) Glutamate as a potential “survival factor” in an in vitro model of neuronal hypoxia/reoxygenation injury: leading role of the Na+/Ca2+ exchanger. Cell Death Dis 9:731
Pignataro G, Tortiglione A, Scorziello A, Giaccio L, Secondo A, Severino B, Santagada V, Caliendo G, Amoroso S, Di Renzo G, Annunziato L (2004) Evidence for a protective role played by the Na+/Ca2+ exchanger in cerebral ischemia induced by middle cerebral artery occlusion in male rats. Neuropharmacology 46:439–448
Pisarenko OI, Lepilin MG, Ivanov VE (1986) Cardiac metabolism and performance during L-glutamic acid infusion in postoperative cardiac failure. Clin Sci (Lond) 70:7–12
Pott C, Eckardt L, Goldhaber JI (2011) Triple threat: the Na+/Ca2+ exchanger in the pathophysiology of cardiac arrhythmia, ischemia and heart failure. Curr Drug Targets 12:737–747
Quednau BD, Nicoll DA, Philipson KD (1997) Tissue specificity and alternative splicing of the Na+/Ca2+ exchanger isoforms NCX1, NCX2, and NCX3 in rat. Am J Physiol 272:C1250–C1261
Ralphe JC, Bedell K, Segar JL, Scholz TD (2005) Correlation between myocardial malate/aspartate shuttle activity and EAAT1 protein expression in hyper- and hypothyroidism. Am J Physiol Heart Circ Physiol 288:H2521–H2526
Ralphe JC, Segar JL, Schutte BC, Scholz TD (2004) Localization and function of the brain excitatory amino acid transporter type 1 in cardiac mitochondria. J Mol Cell Cardiol 37:33–41
Rink C, Gnyawali S, Stewart R, Teplitsky S, Harris H, Roy S, Sen CK, Khanna S (2017) Glutamate oxaloacetate transaminase enables anaplerotic refilling of TCA cycle intermediates in stroke-affected brain. FASEB J 31:1709–1718
Rothstein JD, Martin L, Levey AI, Dykes-Hoberg M, Jin L, Wu D, Nash N, Kuncl RW (1994) Localization of neuronal and glial glutamate transporters. Neuron 13:713–725
Seki S, Taniguchi M, Takeda H, Nagai M, Taniguchi I, Mochizuki S (2002) Inhibition by KB-r7943 of the reverse mode of the Na+/Ca2+ exchanger reduces Ca2+ overload in ischemic-reperfused rat hearts. Circ J 66:390–396
Shigeri Y, Seal RP, Shimamoto K (2004) Molecular pharmacology of glutamate transporters, EAATs and VGLUTs. Brain Res Brain Res Rev 45:250–265
Svedjeholm R, Vanhanen I, Hakanson E, Joachimsson PO, Jorfeldt L, Nilsson L (1996) Metabolic and hemodynamic effects of intravenous glutamate infusion early after coronary operations. J Thorac Cardiovasc Surg 112:1468–1477
Torrente AG, Zhang R, Zaini A, Giani JF, Kang J, Lamp ST, Philipson KD, Goldhaber JI (2015) Burst pacemaker activity of the sinoatrial node in sodium-calcium exchanger knockout mice. Proc Natl Acad Sci U S A 112:9769–9774
Vincent A, Sportouch C, Covinhes A, Barrere C, Gallot L, Delgado-Betancourt V, Lattuca B, Solecki K, Boisguerin P, Piot C, Nargeot J, Barrere-Lemaire S (2017) Cardiac mGluR1 metabotropic receptors in cardioprotection. Cardiovasc Res 113:644–655
Whetsell WO Jr, Shapira NA (1993) Neuroexcitation, excitotoxicity and human neurological disease. Lab Invest 68:372–387
Williams H, King N, Griffiths EJ, Suleiman MS (2001) Glutamate-loading stimulates metabolic flux and improves cell recovery following chemical hypoxia in isolated cardiomyocytes. J Mol Cell Cardiol 33:2109–2119
Zemek RL, Grool AM, Rodriguez Duque D, DeMatteo C, Rothman L, Benchimol EI, Guttmann A, Macpherson AK (2017) Annual and seasonal trends in ambulatory visits for pediatric concussion in ontario between 2003 and 2013. J Pediatr 181(222–228):e222
Acknowledgements
We are grateful to Gerardo Galeazzi, Carlo Alfredo Violet, Franco Pettinari for their invaluable technical assistance.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Magi, S., Castaldo, P., Lariccia, V., Piccirillo, S., Maiolino, M., Amoroso, S. (2020). Intracellular Calcium and Ischemic Damage: Dual Role of the Na+/Ca2+ Exchanger. In: Longhi, S., et al. The First Outstanding 50 Years of “Università Politecnica delle Marche”. Springer, Cham. https://doi.org/10.1007/978-3-030-33832-9_24
Download citation
DOI: https://doi.org/10.1007/978-3-030-33832-9_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-33831-2
Online ISBN: 978-3-030-33832-9
eBook Packages: EducationEducation (R0)