Abstract
Before the introduction of combination chemotherapy, more than 95% of patients with advanced classical Hodgkin lymphoma (cHL) succumbed to their disease within 5 years. Thus, remission rates in excess of 50% achieved with MOPP (mechlorethamine, vincristine, procarbazine, and prednisone) were a major breakthrough in oncology when first seen over 40 years ago. Systematic searches for more effective regimens have replaced MOPP by ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) and BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone). With today’s high survival rates exceeding 90%, it is important to balance cure against short- and long-term adverse effects of treatment. Consequently, response-adapted approaches, mainly using 18-fluorodeoxyglucose-positron emission tomography-computer tomography (FDG-PET-CT), have been introduced as the standard of care allowing for individualized tailored treatment. After many years without new drugs, research has been energized by the possible introduction of novel agents, that is, the antibody-drug conjugate brentuximab vedotin and programmed death receptor-1 inhibitory antibodies, which are increasingly being tested as components of initial therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Multidrug regimen
- Randomized trials
- Overall survival
- Positron emission tomography
- Brentuximab vedotin
- Programmed death receptor-1
1 Introduction and Early History of Combination Chemotherapy
The definition of advanced stage in Hodgkin lymphoma (HL) has evolved over time. Megavoltage radiotherapy (RT) techniques proved efficacious in stage I and IIA disease in the 1950s and 1960s, whereas only few patients with stage III disease were cured by RT alone, despite extended fields of treatment [1]. At the time, more than 95% of patients with stage IV HL succumbed to their disease within 5 years. The first encouraging trials on combination chemotherapy included patients with stages III and IV. Thus, from a historical perspective, advanced disease may be defined by risk groups where curative combination chemotherapy is planned as the primary treatment, while RT is either not used or not the major component. The definition of advanced disease has therefore varied between academic study groups and between trials. This should be borne in mind when evaluating treatment recommendations and results from trials. For most studies, stages IIB, III, and IV are considered advanced disease, while stage IIA is sometimes included, but only in the presence of other risk factors such as bulky disease or multiple sites of involvement.
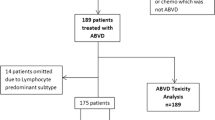
With the advent of more exact diagnostic tools and targeted treatment, the distinction between classical HL (cHL) and nodular lymphocyte-predominant HL has become more robust and more important for treatment. The current chapter covers the development of treatment for cHL only, recognizing that in the past this distinction was not as clear as it is today.
The introduction by DeVita and coworkers of the MOPP regimen to treat patients with advanced HL was a milestone in oncology [2, 3]. MOPP resulted in long-term remission in nearly 50% of patients with stage III and IV disease and has been used for than 40 years. Bonadonna and coworkers were the first to report on the importance of anthracyclines in developing ABVD [4]. ABVD replaced MOPP as the preferred first-line treatment worldwide as the result of a series of randomized trials comparing ABVD, MOPP, and/or MOPP/ABVD alternating, sequential, or hybrid regimens [5,6,7,8,9,10]. The results were better for ABVD or ABVD-containing regimens than for MOPP alone, with failure-free (FFS) or event-free survival (EFS) rates at 5–10 years of 50–80% for ABVD-containing regimens, compared to 35.9% for MOPP in Bonadonna’s original trial and 50% in the Cancer and Leukemia Group B (CALGB) trial reported by Canellos in 1992 (Table 13.1).
The acceptance of ABVD over MOPP and MOPP-like regimens during the 1980s and 1990s was not only motivated by its greater efficacy but also by concerns about toxicity. Follow-up of the early trials showed that irreversible gonadal dysfunction as well as acute leukemia occurred far more often in patients treated with MOPP and MOPP-like regimens. With improved control of the lymphoma, there was an increasing need to balance the likelihood of cure and the risk of serious or fatal complications from treatment. This balance has since been a key concept in the development of better treatment options for advanced-stage cHL.
ABVD is a safe outpatient regimen without the need for close white blood cell monitoring, is feasible in most adult patients up to the age of 60, and can be administered in less-developed healthcare systems [11]. However, bleomycin may cause fatal lung toxicity, especially in older patients, and a long-term higher risk of cardiac morbidity has been reported for patients treated with 6–8 cycles of ABVD [12, 13]. Furthermore, Canellos and coworkers reported the long-term outcome for 123 patients treated with ABVD for advanced cHL in the CALGB trial with a FFS of only 47% and overall survival (OS) 59% after 14 years [14]. Therefore, alternative approaches were developed to improve these results.
2 Fourth-Generation Regimens
2.1 Hybrid and Alternating Regimens
Several academic groups developed combination regimens containing different drugs with known efficacy in HL, and many of these fourth-generation regimens were tested in randomized trials against ABVD [15,16,17,18,19,20,21,22]. According to standards of the time, most of these trials used consolidation RT as part of first-line treatment in a varying proportion of patients (Table 13.2
). None of these studies has established any regimen as superior to ABVD, with the notable exception of the BEACOPP escalated regimen developed by the German Hodgkin Study Group (GHSG).
2.2 BEACOPP Escalated
The development of BEACOPP was motivated by the recognition that dose intensity plays a role in chemotherapy of advanced HL. Hasenclever and coworkers developed a statistical model of dose-response characteristics for drugs used in 706 patients treated with COPP (cyclophosphamide, vincristine, procarbazine, prednisone)/ABVD-like regimens [23]. The model was then used to simulate the effect of dose escalation and changes of schedule and architecture of COPP-ABVD and to design the BEACOPP regimen. G-CSF was mandatory to compensate for the myelotoxic effects. In a phase II study, the optimal doses of the BEACOPP baseline and BEACOPP escalated regimens were determined [24]. The subsequent HD9 trial of the GHSG found the predicted dose-response curve to be correct when comparing the original COPP/ABVD to BEACOPP baseline and BEACOPP escalated [20]. Results from 1195 randomized patients showed a clear superiority of 8 cycles of BEACOPP escalated over BEACOPP baseline and COPP/ABVD at 5 years. Importantly, follow-up data at 10 years confirmed these results: with a median follow-up of 112 months, freedom from treatment failure (FFTF) and OS rates were 64 and 75% in the COPP/ABVD group, 70 and 80% in the BEACOPP baseline group, and 82 and 86% in the BEACOPP escalated group, respectively [25].
However, BEACOPP escalated is associated with higher rates of acute and long-term toxicity. The high rate of secondary malignancies, including myelodysplastic syndrome (MDS) or acute myelogenous leukemia (AML) and solid cancers, and high rates of infertility could be attributed to the higher doses of alkylating agents and the frequent use of RT in the HD9 trial [20, 25]. The subsequent GHSG HD12 trial aimed at de-escalating treatment by comparing four courses of BEACOPP escalated with four courses of escalated and four courses of baseline BEACOPP (“4 + 4”) [21]. The role of RT was tested by a second randomization of consolidating radiation to initial bulky and residual disease versus no RT. At 5 years, OS was 91%, FFTF 85.5%, and progression-free survival (PFS) 86.2% with no statistical difference between 8 cycles of BEACOPP escalated and the 4 + 4 arm but no apparent benefit in terms of toxicity with the reduced regimen. Because a number of patients randomized to the arm without RT were in fact irradiated based on recommendations by a blinded expert panel, the conclusions to be drawn from this part of the trial are limited. Since there was no relevant benefit in terms of toxicity in the 4 + 4 treated patients, 8 cycles of BEACOPP escalated remained standard for advanced-stage HL patients in the GHSG. Recent long-term updates of both the HD9 and 12 trials confirm the superior initial results for BEACOPP escalated [26].
The subsequent HD15 study also tested de-escalation of chemotherapy with a reduction in the number of cycles from 8 to 6 and the introduction of a dose-dense BEACOPP baseline regimen (BEACOPP-14) [22]. In addition, PET-guided omission of RT to residual disease was investigated. A total of 2182 patients were randomized among the 3 study arms. Surprisingly, when comparing 6 cycles of BEACOPP escalated with 8 cycles, both PFS (90.3% versus 85.6%) and OS (95.3% versus 91.9%) were significantly better with the reduced number of cycles. With omission of RT in cases of PET-negative residual masses, only 11% of all patients received additional RT without compromising tumor control, and the negative predictive value for the end of treatment PET at 12 months was 94.1% [27]. In summary, HD15 established six cycles of BEACOPP escalated as a new standard of care to be tested further in PET response-adapted trials (see below).
With extensive evidence from clinical trials, BEACOPP escalated is a highly effective regimen for patients with advanced HL. Acute toxicity requires monitoring of patients between cycles, hospitalization in around one third of patients, and vigilance for potentially lethal neutropenic infections. Special attention should be paid to patients above the age of 50 years and patients of poor performance status at start of treatment. With the reduction of cycle numbers and less use of consolidation RT, rates of secondary malignancies seem to be decreasing, but determining the true rate of such complications will need longer observation [26]. Infertility in both women and men treated with BEACOPP is still a concern [28].
3 ABVD or BEACOPP Escalated as Standard First-Line Treatment?
These developments led to the emergence of two alternative strategies for the treatment of advanced HL: balancing cure rates and toxicity, the first strategy proposed ABVD as the standard front line regimen, with salvage treatment, high-dose chemotherapy (HDCT), and autologous stem cell transplantation (ASCT) for those patients failing initial therapy. With this strategy, the majority of patients could be cured with ABVD without exposing them to the toxicity of BEACOPP. The second strategy used BEACOPP escalated as first-line treatment, aiming to cure as many patients as possible with first-line therapy, but accepting more toxicity for those patients who might have been cured with a less intensive approach. Data are now available from direct comparative trails and from meta-analyses to address this question.
Four studies have been conducted comparing these two approaches, all smaller and so far with shorter follow-up than the HD9 trial. All studies compare four escalated BEACOPP followed by two or four baseline BEACOPP with six to eight cycles of ABVD (Table 13.3
).
The Italian HD2000 trial enrolled 307 patients in 3 different treatment arms showing a significant superiority of BEACOPP (4+2 fashion) over 6 cycles of ABVD in terms of PFS but not for OS [29]. At 5 years, the PFS rate was 68% for ABVD and 81% for BEACOPP: OS was 84% for ABVD and 92% for BEACOPP, respectively. The data of this trial were updated at 10 years follow-up, and the authors were not able to confirm the superiority of BEACOPP over ABVD in terms of PFS, mainly because of higher mortality from second malignancies observed after BEACOPP [33].
The Michelangelo Foundation, the Gruppo Italiano di Terapie Innovative nei Linfomi (GITIL), and the Intergruppo Italiano Linfomi (IIL) study compared 6–8 courses of ABVD and BEACOPP given in 4 + 4 fashion plus preplanned salvage with HDCT [30]. Patients with a higher risk profile based on international prognostic score (IPS) of 3 and more were included. Two thirds of the patients also received RT. The final analysis showed a 7-year rate of freedom from first progression (FFFP) of 85% in patients who received initial treatment with BEACOPP and 73% for those who received ABVD (p = 0.004). A total of 65 patients (20 in the BEACOPP group and 45 in the ABVD group) needed HDCT. After completion of the planned treatment including salvage therapy, the 7-year OS rates were 89 and 84%, respectively (p = 0.39). This trial was not powered to detect differences in OS, and the conclusion on overall treatment outcome should be cautioned.
The slightly larger intergroup trial organized by the EORTC had a similar design as the Michelangelo-GITIL-IIL study [31]; 8 courses of ABVD were compared to BEACOPP 4 + 4 with no RT allowed. With a median follow-up of 3.6 years at the time of the final report, the 4-year rates for EFS and OS were similar in ABVD-treated (63.7% and 86.7%, respectively) and BEACOPP-treated patients (69.3% and 91.5%). However, the secondary endpoint, PFS, was significantly lower in the ABVD than in the BEACOPP arm (72.8% versus 83.4%, p = 0.0052). There were no clear differences in toxicity between the two arms.
Patients with low-risk advanced-stage disease (IPS 0–2) were enrolled in the H34 trial conducted by the Lymphoma Study Association (LYSA) [32]. With 150 patients randomized in this trial, the complete remission rate was 85% for ABVD and 90% for BEACOPP. With a median follow-up of 5.5 years, 7 patients died: 6 treated with ABVD and 1 with BEACOPP. The PFS at 5 years was 75% and 93% (p = 0.007) and the OS 92% and 99% (p = 0.06) for ABVD- and BEACOPP-treated patients. Although the number of patients recruited in this trial was rather small, these results suggest that BEACOPP is also more effective than ABVD in advanced-stage patients with lower risk.
All trials comparing ABVD and BEACOPP directly are smaller than the GHSG trials and evaluated different numbers of BEACOPP escalated (4 + 4 or 4 + 2, escalated, and baseline, respectively). 6 cycles of escalated BEACOPP have been shown by the GHSG to represent the most effective strategy. Since there was uncertainty regarding the difference in OS between ABVD and BEACOPP, a network meta-analysis was performed to indirectly compare these and other regimens [34]. The final analysis included nearly 10,000 patients from 14 different trials. Reconstructed survival data suggested that 6 cycles of BEACOPP escalated have a 10% advantage over ABVD in terms of OS at 5 years (95% confidence interval 3–15%), offering advanced-stage HL patients the highest chance of cure. Another more recent meta-analysis with data from four of the trials mentioned above (and including one trial comparing ABVD and BEACOPP in early unfavorable disease) confirmed the superiority of BEACOPP escalated over ABVD in term of PFS and OS [35]. There was a significantly increased occurrence of MDS or AML in BEACOPP-based strategies (relative risk 3.90, p = 0.02), but not for second malignancies in total. The risk of infertility could not be assessed by these meta-analyses due to lack of data.
4 Outcome Prediction
4.1 The International Prognostic Score
With the choice between ABVD and BEACOPP, it would be preferable to treat each advanced cHL patient according to their individual risk in order to balance efficacy and toxicity. The development of the IPS paralleled the quest for more effective regimens than ABVD and was aimed to further assess each patient’s risk of treatment failure under ABVD- and ABVD-like regimens [36].
The score was derived from 5141 patients who had been treated with ABVD-like regimens with or without RT. Seven factors had similar independent prognostic effects: serum albumin of less than 4 g/dL, hemoglobin level of less than 10.5 g/dL, male sex, age of 45 years or older, stage IV disease (according to the Ann Arbor classification), leukocytosis (white cell count of at least 15 × 10−9 L), and lymphocytopenia (lymphocyte count of less than 0.6 × 10−9 or less than 8% of white-cell count). As outlined, several studies evaluating BEACOPP escalated have selected patients not only based on stage and B symptoms, but also on a higher IPS. It is assumed that the more intensive treatment will have the greatest effect in high-risk patients. This is in part supported by the results of the HD9 trial, where the absolute benefit in terms of improved OS in those treated with BEACOPP escalated seems greater in intermediate risk than in low-risk patients, although not in the high-risk group [25]. The LYSA H34 results in low-risk patients suggest a significant 18% benefit in PFS rates and a borderline significant improvement in OS of 9%, both at 5 years, but this requires confirmation [32].
4.2 Positron Emission Tomography
Assessment of the risk of treatment failure by IPS has been partly displaced by early response evaluation. To determine the optimal amount of treatment needed, functional imaging in the form of FDG-PET has been developed to provide an early indication of chemosensitivity in HL. PET is discussed in detail elsewhere in this book (see Chap. 7). In patients with mostly advanced disease, retrospective studies showed that the early PET response (after two cycles of ABVD) overshadowed the prognostic value of the IPS and thus could be an important tool for response-adapted treatment planning in advanced HL [37]. The utility of FDG-PET has been facilitated by development of a highly reproducible 5-point scale, the Deauville scale, for reporting results [38].
Several recent studies have tested early response evaluation by FDG-PET as a means of adjusting subsequent therapy according to the response to initial treatment. Strategies based on initial ABVD or BEACOPP have helped to define new standards of care in which each patient receives as much therapy as deemed necessary.
5 Response-Adapted Therapy
5.1 De-escalation of Therapy in Early Responders
Groups using either ABVD or BEACOPP as initial therapy have aimed to reduce treatment intensity in patients with a negative interim PET, by omitting potentially toxic components of the regimens, by reducing the number of cycles, or by omitting RT (Table 13.4
).
In the international RATHL trial, all patients initially received two cycles of ABVD [39]. Using a Deauville score cut-off between 3 and 4, 83.7% of the patients were interim PET negative and were randomized. In the experimental arm, bleomycin was not given in the remaining four cycles. The results showed 3-year PFS rates of 85.7% and 84.4%, respectively, in the standard ABVD and AVD groups. Pulmonary toxicity was reduced in patients treated with AVD in cycles 3 through 6. Thus, bleomycin is redundant in advanced-stage patients who have achieved a complete metabolic response after two cycles of chemotherapy.
In patients with advanced HL who have a negative PET, defined as Deauville scores 1–3, after two and six cycles of ABVD, the GITIL/Fondazione Italiana Linfomi (FIL) HD0607 trial demonstrated that consolidation RT to initially bulky lesions can be omitted without a decrease in tumor control at 3 years [40]. The 3-year PFS was 87% in the interim PET-negative group.
The proportions of interim PET-negative patients in the RATHL and GITL/FIL HD0607 studies and 3-year PFS rates are remarkably similar. They are comparable to other prospective phase II trials using the same approach [42, 43]. However, the negative predictive value of interim PET-CT in these prospective trials appears lower than anticipated from previous retrospective studies using non-standardized criteria for reporting PET results. This means that the largest number of treatment failures in advanced-stage HL treated initially with ABVD will occur in the interim PET-negative group.
Interim PET-CT has also been used to de-escalate therapy in early responders to BEACOPP escalated. Using the FDG uptake in the mediastinal blood pool as reference, corresponding to Deauville scores of 1 and 2, the randomized GHSG HD18 trial demonstrated that the number of cycles of BEACOPP could be reduced from six to four in patients with a negative interim PET after two cycles [41]. With 1005 out of 1945 randomized patients (52%) having a negative interim PET by these criteria, the HD18 trial indicated an excellent 5-year OS rate of 95% and a significant reduction of severe acute hematological and non-hematological toxicities. The GHSG later provided post hoc evidence that the excellent outcome of PET-negative patients also holds for those with an interim Deauville score of 3, and despite the fact that these had all received six cycles of BEACOPP escalated in the trail, a total of four escalated BEACOPPs to patients with an interim score of 1–3 are currently recommended [44].
The randomized LYSA AHL2011 trial evaluated whether a PET-driven strategy allows for a tailored shift from BEACOPP escalated to ABVD in advanced HL [45]. In the experimental arm, patients with a negative PET after two cycles of BEACOPP escalated completed treatment with four cycles of ABVD, while the interim PET-positive patients continued with four cycles of BEACOPP escalated. Patients assigned to the standard arm received a total of six cycles of BEACOPP escalated. After a median observation time of 50 months, 5-year PFS rates did not differ, 86.5% and 85.7% in the standard and experimental arms, respectively. Using a Deauville score cut-off between 3 and 4 in the experimental arm, 84% of patients received 2 escalated BEACOPP and 4 ABVD with a significant reduction in toxicity. Thus, it appears possible to switch to ABVD on the basis of a negative interim PET after two cycles of escalated BEACOPP without loss of tumor control. By extrapolation from the RATHL study, it may be possible to switch to AVD and thereby avoid the risk of continued bleomycin exposure. The LYSA AHL2011 used a modified Deauville score for assessment of interim PET-CT defining score 4 and 5 as a residual lesion uptake equal or higher than 140% and 200% of the liver uptake, respectively. These more stringent criteria may explain the lower rate of interim PET-positive patients in the AHL2011 (12.6%) than in the HD18 trial (24%) and the higher treatment failure rate in the PET-positive group in AHL2011 compared to HD18 study.
5.2 Escalation of Therapy in Early Nonresponders
Several groups tested prospectively the approach of escalating treatment in patients not responding to two cycles of ABVD as defined by PET positivity (Table 13.4). With the limitations mentioned above, based on the historical data, these patients have a very poor outcome with ABVD or ABVD-like therapy. The 2- or 3-year PFS is reported between 6% and 38% [46]. Most investigators have therefore considered it unethical in these patients to compare any experimental therapy to ABVD in a randomized fashion.
The RATHL trial tested the escalation to either BEACOPP escalated four cycles or BEACOPP-14 six cycles in interim PET-positive patients [39]. Of the 182 patients with positive findings on interim PET-CT scans according to protocol, 94 received BEACOPP-14 and 78 received escalated BEACOPP. The results of a third PET-CT scan were available for 160 patients, of whom 119 (74.4%) had negative findings. The 3-year PFS rate for the group as a whole was 67.5%, and the OS rate was 87.8%.
Similar results were reported in the GITIL/FIL HD0607 trial [40]. 149 of 150 patients with interim PET-positive results continued on BEACOPP (4 escalated and 4 baseline) with or without the addition of rituximab. After four BEACOPP escalated, a PET evaluation was performed in 136 patients. At the time of the report, disease progression was registered in 27 of 108 PET-negative scans compared with 25 of 28 PET-positive scans. The 3-year PFS rate was 60%, and the 3-year OS rate was 89% in the interim PET-positive group.
The American South West Oncology Group (SWOG) followed the same principles of escalating to six cycles of BEACOPP escalated after ABVD with similar results for the interim PET-positive group compared to RATHL and GITIL/FIL HD0607 trials [42]. Escalation to an alternative regimen consisting of ifosfamide, gemcitabine and vinorelbine (IGEV) followed by HDCT was pursued in the Italian HD0801 study [43]. In an intention-to-treat analysis, the authors reported for the PET-positive patients (excluding those with Deauville score 3) a 2-year PFS of 75%.
Taking together the shift from ABVD to BEACOPP escalated or variants thereof seems justified in interim PET-positive patients. Whether other salvage regimens including HDCT might improve the outcomes further is unknown at present. Nonetheless, the results remain suboptimal, and further improvements, possibly by incorporation of novel drugs, are needed.
Following the success with initial BEACOPP escalated in the HD9, HD12, and HD15 trials, the GHSG tested whether it might be possible to improve the results by adding rituximab, a monoclonal antibody binding to CD-20 on the surface of B cells, in patients with interim PET-positive disease [47]. The rationale is derived from the recognition of a minority of cHL cases with CD-20-positive Hodgkin or Reed-Sternberg cells and the possible benefit of targeting normal B cell in the tumor microenvironment. In the HD18 trial, patients with interim PET-positive disease (Deauville score 3–5) after two cycles of escalated BEACOPP were randomized to six further cycles with or without rituximab. The PFS rates at 3 years for PET-positive patients were 93.0% and 91.4% with or without rituximab, respectively, better than expected from the previous HD15 trial and without any benefit of adding rituximab.
Patients with an interim Deauville score 4 (post hoc analysis of HD18) or 4–5 (LYSA AHL2011) after 2 BEACOPP escalated have reduced PFS rates compared to interim PET-negative patients with a score of 1–3. As mentioned, a later post hoc analysis of the HD18 study showed that in patients receiving 6 cycles of BEACOPP escalated, 3-year PFS rates were 92.2%, 95.9%, and 87.6% with interim PET scores of 1–2, 3, and 4, respectively [44]. The univariate hazard ratio (HR) for PFS in patients with score 4 versus score 1–3 was 2.3 (p = 0.002). Deauville score of 4 was the only factor remaining significant for PFS in a multivariate analysis including the associated baseline risk factors. In the LYSA AHL 2011 trial, using more stringent definitions of Deauville score 4 and 5, interim PET positivity was associated to a higher risk of relapse or progression with 5-year PFS of 70.7% versus 88.9% and a HR = 3.59 (p < 0.0001). Whether these results for interim PET-positive patients after initial BEACOPP therapy can be improved, i.e., by the incorporation of novel drugs, has not been tested yet.
The concept of response-adapted therapy in advanced-stage HL has considerably changed the way in which patients are treated. Unfortunately, there is no direct comparison of strategies starting with ABVD and escalating in poor responders versus starting with BEACOPP escalated and reducing treatment in the early responders.
6 Introduction of Brentuximab Vedotin into First-Line Treatment
With the approval of brentuximab vedotin (BV) for relapsed and refractory disease (see Chap. 21), a novel targeted drug has been introduced into the treatment of cHL. This has shown an excellent balance of efficacy and tolerability in persistent or recurrent disease [48]. Therefore, BV is an ideal candidate to improve both the ABVD and the BEACOPP regimens.
BV was initially combined with ABVD in a phase I study; however, life-threatening pulmonary toxicity in this bleomycin-containing combination was observed [49]. BV at a fixed dose (1.2 mg/kg body weight) was given safely with bleomycin-deleted AVD (given the name A+AVD, as Adcetris, the proprietory name for BV) to 26 patients. 25 of the 26 (96%) had complete response after treatment. Neuropathy, probably as a result of coadministration of two microtubule-disrupting agents (monomethyl auristatin E and vinblastine), neutropenia and complications thereof, including the need to add growth factors in a number of patients, were noted as relevant toxicities. In a recent update on long-term outcome, the 5-year FFS and OS were 79% and 92% after ABVD plus BV and 92% and 100% after A+AVD, respectively [50].
After the initial encouraging results with A+AVD, this regimen has been tested in a large company-sponsored trial, comparing the new regimen to ABVD [51]. Patients with stage III and IV disease were entered and interim PET-CT after two cycles guided an optional switch to alternative frontline therapy at the treating physician’s discretion, but only for patients with a Deauville score of 5. The primary endpoint was modified PFS, defined as time to disease progression, death, or modified progression (with the latter defined as evidence of non-complete response after completion of frontline therapy according to review by an independent committee, followed by subsequent anticancer therapy). With 1334 randomized patients and a median follow-up of 24.6 months, the 2-year modified PFS rates in the A+AVD and ABVD groups were 82.1% and 77.2%, respectively, a difference of 4.9 percentage points (p = 0.04). There was higher rate of febrile neutropenia in the A+AVD group, and growth factor support was introduced as mandatory during the course of the trial. There was also more severe neuropathy in the experimental arm, but as reported for other BV trials, this appeared to be reversible in most patients. As expected from the omission of bleomycin, lung toxicity was reduced. These results produced a debate as to whether A+AVD should be accepted as a new standard of care. Follow-up is short, and the new endpoint, incorporating into the definition of progression any treatment given to patients with residual PET-positive disease (Deauville scores 3–5), hampers comparison with other trials. With a modest difference between treatment arms, increased toxicity, and the absence of a documented survival benefit, the same principles as in the debate over ABVD and BEACOPP will apply. Another consideration is the considerable drug cost of BV and expense of the necessary growth factors.
An interesting aspect of the Echelon-1 trial is the prospective less stringent approach to PET-guided adaptation, where patients with an interim PET-CT of 4 or 5 were either planned to continue treatment with A+AVD or ABVD (Deauville score 4) or allowed to do so as an alternative to intensive chemotherapy (Deauville score 5). The data thus reflect the outcome of ABVD-treated interim PET-positive patients in the modern era, using PET-CT in a prospective way and with uniform criteria comparable to other studies [52]. PET positivity rates were strikingly lower than in other similar studies, with Deauville ≥4 found in 7% (47/644) in the A+AVD arm and 9% (58/670) with ABVD; 5 patients with a Deauville score of 5 switched to alternative frontline therapy. Subgroup analyses of the ABVD arm showed a 2-year modified PFS rate of 80.9% versus 42.0% for interim PET-negative and PET-positive patients, respectively.
Following the aim to improve tolerability while maintaining efficacy, the GHSG has modified the BEACOPP regimen and introduced BV. A randomized phase II trial testing six cycles of two variants of BEACOPP was published recently: in one arm, vincristine was replaced by BV and bleomycin omitted (BrECAPP) [53]. A more experimental regimen additionally replaced dacarbazine for procarbazine and short-term dexamethasone instead of long-term prednisone (BrECADD). 104 patients were enrolled to the study (52 were assigned to each study arm). Complete responses were seen at completion of BrECAPP and BrECADD in 86% and 88% of patients, respectively. Particularly, the BrECADD regimen was associated with a more favorable toxicity profile and therefore selected for comparison to standard BEACOPP escalated in advanced cHL in the ongoing HD21 trial (NCT02661503). This trial is testing 4/6 cycles of escalated BEACOPP (in a PET response-adapted design) against 4/6 cycles of BrECADD.
7 Introducing Programmed-Death-1 Inhibitors into First-Line Treatment
The second class of drugs recently introduced for relapsed and refractory cHL is the checkpoint inhibitors targeting programmed-death receptor (PD) 1, on the surface of cells in the microenvironment of cHL. It appears that Hodgkin and Reed-Sternberg cells by expression of the PD-ligand (PD-L)-1 and PD-L2 orchestrate the tissue microenvironment for tumor survival and growth (reviewed in Chap. 22). These mechanisms seem to be operable also in previously untreated cases [54]. Studies are underway to explore the effect of PD-1 inhibition also in the context of first-line treatment of advanced disease. So far, no results are reported. An initial study using nivolumab as sole initial therapy prior to the addition of AVD showed a response rate of 69% for monotherapy and promising short term outcomes, with PFS of 92% at 9 months [55].
8 The Role of Radiotherapy
The use of RT in advanced-stage HL has evolved over time, from subtotal or total nodal RT (i.e., treating also areas of initial possible microscopic disease) to involved-field RT (i.e., treating only areas of initial macroscopic disease) or as RT in situations associated with a higher risk of local relapse (most often site of initial bulky lesions or residual macroscopic disease possibly representing active tumor). The role of consolidation RT for advanced HL also depends on the efficacy of the prior chemotherapy (see Chap. 9 for further details).
After MOPP or MOPP-like regimens, there appeared to be a potential advantage of IFRT in a meta-analysis of 16 randomized studies, whereas this advantage is not evident after ABVD or ABVD-like regimens [56, 57]. A randomized EORTC study demonstrated that consolidation IFRT did not improve outcomes in patients in complete remission after six to eight courses of MOPP-ABV, but potentially improved the outcome of patients with a partial response [58]. A randomized Groupe d’Etude des Lymphomes de l’Adulte (GELA) trial showed that consolidation with subtotal or total nodal RT for patients in remission after doxorubicin-containing systemic treatment was not superior to two additional cycles of chemotherapy [59]. Thus, patients achieving a complete radiological response with ABVD or ABVD-like regimens do not need consolidation RT.
In current treatment algorithms, the chemosensitivity and quality of remission in each individual patient are assessed by FDG-PET, either as an interim PET during or a PET done at the end of treatment. PET results may be especially helpful in assessing the need for consolidation in situations with residual fibrotic masses after chemotherapy. The GITIL/FIL HD0607 trial randomized patients with advanced HL with a large nodal mass at diagnosis (≥5 cm) and a negative PET after two and six cycles of ABVD to RT of the site of the initial large mass or observation alone [40]. In 296 randomized patients, there was no significant PFS improvement at 3 years, 97% versus 93%, respectively (p = 0.29). Together, patients treated with ABVD that are in complete remission by radiological criteria or PET negative after two cycles can safely omit RT, even in presence of residual masses. Whether certain patients with residual masses that are PET negative at the end of treatment (in the absence of any interim PET) or patients with interim or end of treatment positive PET in the context of ABVD benefit from the addition of RT has not been analyzed systematically.
The HD15 trial prospectively analyzed the omission of RT in cases of PET-negative residual masses after six or eight cycles of BEACOPP [27]. All patients with residual disease of ≥2.5 cm after chemotherapy were evaluated using additional PET and based on the criteria at the time; those with a PET-positive result were irradiated to the site of residual disease. Only 11% of all patients received additional RT without compromising tumor control, and the negative predictive value for the end of treatment PET at 12 months was 94.1%. PFS at 4 years was similar for patients without residual disease and patients with PET-negative residuals, 92.1% and 92.6%, respectively, showing that RT can be safely omitted in both situations. PFS for PET-negative or PET-positive patients was 92.6% and 86.2% at 48 months (p = 0.022). Thus, a positive PET after chemotherapy was associated with higher risk of subsequent treatment failure, even though PET-positive patients were treated with additional RT. The frequency and pattern of relapses still suggest that local RT to PET-positive residual disease is sufficient for these patients [60].
9 Summary
Advanced-stage HL has become a curable disease for the majority of patients, and treatment decisions need to take into account the risk of serious long-term consequences of therapy. After a decade of debate whether first-line treatment with six to eight cycles of ABVD or BEACOPP escalated best balances the likelihood of cure and risk of complications, individualized treatment based on early response to chemotherapy has now become a standard in many developed countries. Starting with ABVD, de-escalation by omission of bleomycin and/or RT is possible in interim PET-negative patients. In case of an inadequate response, a shift to BEACOPP escalated may still cure a reasonable number of patients, subjecting only a minority of patients to the increased toxicity associated with BEACOPP. Similarly, the total number of cycles can be reduced from six to four or therapy switched to four ABVD in patients with interim negative PET results after two cycles of BEACOPP escalated. RT can be safely omitted in BEACOPP-treated patients with an end of treatment negative PET. With still short follow-up, the OS in either approach is excellent, with the interim PET-positive group after ABVD representing a candidate group for implementation of novel approaches. Apart from these more personalized treatment strategies, early results from a combination of BV with AVD show modest improvements in disease control but increased toxicity and costs. BV is also tested in the context of a modified BEACOPP regimen to enhance tolerability. After decades of substantial but slow advances in the treatment of advanced-stage HL, personalized treatment strategies have resulted in better treatment options for our patients. Targeted and immunological approaches may improve results further in the near future.
References
Kaplan HS (1972) Hodgkin’s disease. Harvard University Press, Cambridge, MA. 452 p
Devita VT Jr, Serpick AA, Carbone PP (1970) Combination chemotherapy in the treatment of advanced Hodgkin’s disease. Ann Intern Med 73(6):881–895
DeVita VT Jr, Simon RM, Hubbard SM, Young RC, Berard CW, Moxley JH 3rd et al (1980) Curability of advanced Hodgkin’s disease with chemotherapy. Long-term follow-up of MOPP-treated patients at the National Cancer Institute. Ann Intern Med 92(5):587–595
Bonadonna G, Zucali R, Monfardini S, De Lena M, Uslenghi C (1975) Combination chemotherapy of Hodgkin’s disease with adriamycin, bleomycin, vinblastine, and imidazole carboxamide versus MOPP. Cancer 36(1):252–259
Bonadonna G, Valagussa P, Santoro A (1986) Alternating non-cross-resistant combination chemotherapy or MOPP in stage IV Hodgkin’s disease. A report of 8-year results. Ann Intern Med 104(6):739–746
Santoro A, Bonadonna G, Valagussa P, Zucali R, Viviani S, Villani F et al (1987) Long-term results of combined chemotherapy-radiotherapy approach in Hodgkin’s disease: superiority of ABVD plus radiotherapy versus MOPP plus radiotherapy. J Clin Oncol 5(1):27–37
Duggan DB, Petroni GR, Johnson JL, Glick JH, Fisher RI, Connors JM et al (2003) Randomized comparison of ABVD and MOPP/ABV hybrid for the treatment of advanced Hodgkin’s disease: report of an intergroup trial. J Clin Oncol 21(4):607–614
Viviani S, Bonadonna G, Santoro A, Bonfante V, Zanini M, Devizzi L et al (1996) Alternating versus hybrid MOPP and ABVD combinations in advanced Hodgkin’s disease: ten-year results. J Clin Oncol 14(5):1421–1430
Connors JM, Klimo P, Adams G, Burns BF, Cooper I, Meyer RM et al (1997) Treatment of advanced Hodgkin’s disease with chemotherapy--comparison of MOPP/ABV hybrid regimen with alternating courses of MOPP and ABVD: a report from the National Cancer Institute of Canada clinical trials group. J Clin Oncol 15(4):1638–1645
Canellos GP, Anderson JR, Propert KJ, Nissen N, Cooper MR, Henderson ES et al (1992) Chemotherapy of advanced Hodgkin’s disease with MOPP, ABVD, or MOPP alternating with ABVD. New Engl J Med 327(21):1478–1484
Geel JA, Chirwa TC, Rowe B, Eyal KC, Omar F, Stones DK et al (2017) Treatment outcomes of children with Hodgkin lymphoma between 2000 and 2010: First report by the South African Children’s Cancer Study Group. Pediatr Blood Cancer 64:10
Myrehaug S, Pintilie M, Tsang R, Mackenzie R, Crump M, Chen Z et al (2008) Cardiac morbidity following modern treatment for Hodgkin lymphoma: supra-additive cardiotoxicity of doxorubicin and radiation therapy. Leukemia Lymphoma 49(8):1486–1493
Evens AM, Hong F, Gordon LI, Fisher RI, Bartlett NL, Connors JM et al (2013) The efficacy and tolerability of adriamycin, bleomycin, vinblastine, dacarbazine and Stanford V in older Hodgkin lymphoma patients: a comprehensive analysis from the North American intergroup trial E2496. Brit J Haematol 161(1):76–86
Canellos GP, Niedzwiecki D (2002) Long-term follow-up of Hodgkin’s disease trial. New Engl J Med 346(18):1417–1418
Sieber M, Tesch H, Pfistner B, Rueffer U, Paulus U, Munker R et al (2004) Treatment of advanced Hodgkin’s disease with COPP/ABV/IMEP versus COPP/ABVD and consolidating radiotherapy: final results of the German Hodgkin’s Lymphoma Study Group HD6 trial. Ann Oncol 15(2):276–282
Gobbi PG, Levis A, Chisesi T, Broglia C, Vitolo U, Stelitano C et al (2005) ABVD versus modified Stanford V versus MOPPEBVCAD with optional and limited radiotherapy in intermediate- and advanced-stage Hodgkin’s lymphoma: final results of a multicenter randomized trial by the Intergruppo Italiano Linfomi. J Clin Oncol 23(36):9198–9207
Johnson PW, Radford JA, Cullen MH, Sydes MR, Walewski J, Jack AS et al (2005) Comparison of ABVD and alternating or hybrid multidrug regimens for the treatment of advanced Hodgkin’s lymphoma: results of the United Kingdom Lymphoma Group LY09 Trial (ISRCTN97144519). J Clin Oncol 23(36):9208–9218
Radford JA, Rohatiner AZ, Ryder WD, Deakin DP, Barbui T, Lucie NP et al (2002) ChlVPP/EVA hybrid versus the weekly VAPEC-B regimen for previously untreated Hodgkin’s disease. J Clin Oncol 20(13):2988–2994
Hoskin PJ, Lowry L, Horwich A, Jack A, Mead B, Hancock BW et al (2009) Randomized comparison of the Stanford V regimen and ABVD in the treatment of advanced Hodgkin’s Lymphoma: United Kingdom National Cancer Research Institute Lymphoma Group Study ISRCTN 64141244. J Clin Oncol 27(32):5390–5396
Diehl V, Franklin J, Pfreundschuh M, Lathan B, Paulus U, Hasenclever D et al (2003) Standard and increased-dose BEACOPP chemotherapy compared with COPP-ABVD for advanced Hodgkin’s disease. New Engl J Med 348(24):2386–2395
Borchmann P, Haverkamp H, Diehl V, Cerny T, Markova J, Ho AD et al (2011) Eight cycles of escalated-dose BEACOPP compared with four cycles of escalated-dose BEACOPP followed by four cycles of baseline-dose BEACOPP with or without radiotherapy in patients with advanced-stage Hodgkin’s lymphoma: final analysis of the HD12 trial of the German Hodgkin Study Group. J Clin Oncol 29(32):4234–4242
Engert A, Haverkamp H, Kobe C, Markova J, Renner C, Ho A et al (2012) Reduced-intensity chemotherapy and PET-guided radiotherapy in patients with advanced stage Hodgkin’s lymphoma (HD15 trial): a randomised, open-label, phase 3 non-inferiority trial. Lancet 379(9828):1791–1799
Hasenclever D, Loeffler M, Diehl V (1996) Rationale for dose escalation of first line conventional chemotherapy in advanced Hodgkin’s disease. German Hodgkin’s Lymphoma Study Group. Ann Oncol 7(Suppl 4):95–98
Tesch H, Diehl V, Lathan B, Hasenclever D, Sieber M, Ruffer U et al (1998) Moderate dose escalation for advanced stage Hodgkin’s disease using the bleomycin, etoposide, adriamycin, cyclophosphamide, vincristine, procarbazine, and prednisone scheme and adjuvant radiotherapy: a study of the German Hodgkin’s Lymphoma Study Group. Blood 92(12):4560–4567
Engert A, Diehl V, Franklin J, Lohri A, Dörken B, Ludwig W-D et al (2009) Escalated-Dose BEACOPP in the treatment of patients with advanced-stage Hodgkin’s lymphoma: 10 years of follow-up of the GHSG HD9 study. J Clin Oncol 27(27):4548–4554
von Tresckow B, Kreissl S, Goergen H, Brockelmann PJ, Pabst T, Fridrik M et al (2018) Intensive treatment strategies in advanced-stage Hodgkin’s lymphoma (HD9 and HD12): analysis of long-term survival in two randomised trials. Lancet Haematol 5(10):e462–ee73
Kobe C, Dietlein M, Franklin J, Markova J, Lohri A, Amthauer H et al (2008) Positron emission tomography has a high negative predictive value for progression or early relapse for patients with residual disease after first-line chemotherapy in advanced-stage Hodgkin lymphoma. Blood 112(10):3989–3994
Behringer K, Mueller H, Goergen H, Thielen I, Eibl AD, Stumpf V et al (2013) Gonadal function and fertility in survivors after Hodgkin lymphoma treatment within the German Hodgkin Study Group HD13 to HD15 trials. J Clin Oncol 31(2):231–239
Federico M, Luminari S, Iannitto E, Polimeno G, Marcheselli L, Montanini A et al (2009) ABVD compared with BEACOPP compared with CEC for the initial treatment of patients with advanced Hodgkin’s lymphoma: results from the HD2000 Gruppo Italiano per lo Studio dei Linfomi Trial. J Clin Oncol 27(5):805–811
Viviani S, Zinzani PL, Rambaldi A, Brusamolino E, Levis A, Bonfante V et al (2011) ABVD versus BEACOPP for Hodgkin’s lymphoma when high-dose salvage is planned. New Engl J Med 365(3):203–212
Carde P, Karrasch M, Fortpied C, Brice P, Khaled H, Casasnovas O et al (2016) Eight cycles of ABVD versus four cycles of BEACOPP escalated plus four cycles of BEACOPP baseline in stage III to IV, International prognostic score >/= 3, high-risk Hodgkin lymphoma: first results of the phase III EORTC 20012 intergroup trial. J Clin Oncol 34(17):2028–2036
Mounier N, Brice P, Bologna S, Briere J, Gaillard I, Heczko M et al (2014) ABVD (8 cycles) versus BEACOPP (4 escalated cycles >/= 4 baseline): final results in stage III–IV low-risk Hodgkin lymphoma (IPS 0-2) of the LYSA H34 randomized trial. Ann Oncol 25(8):1622–1628
Merli F, Luminari S, Gobbi PG, Cascavilla N, Mammi C, Ilariucci F et al (2016) Long-term results of the HD2000 trial comparing ABVD versus BEACOPP versus COPP-EBV-CAD in untreated patients with advanced Hodgkin lymphoma: a study by Fondazione Italiana Linfomi. J Clin Oncol 34(11):1175–1181
Skoetz N, Trelle S, Rancea M, Haverkamp H, Diehl V, Engert A et al (2013) Effect of initial treatment strategy on survival of patients with advanced-stage Hodgkin’s lymphoma: a systematic review and network meta-analysis. Lancet Oncol 14(10):943–952
Skoetz N, Will A, Monsef I, Brillant C, Engert A, von Tresckow B (2017) Comparison of first-line chemotherapy including escalated BEACOPP versus chemotherapy including ABVD for people with early unfavourable or advanced stage Hodgkin lymphoma. Cochr Datab Syst Rev 5:CD007941. https://doi.org/10.1002/14651858
Hasenclever D, Diehl V (1998) A prognostic score for advanced Hodgkin’s disease. International Prognostic Factors Project on Advanced Hodgkin’s Disease. New Engl J Med 339(21):1506–1514
Gallamini A, Hutchings M, Rigacci L, Specht L, Merli F, Hansen M et al (2007) Early interim 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography is prognostically superior to international prognostic score in advanced-stage Hodgkin’s lymphoma: a report from a joint Italian-Danish study. J Clin Oncol 25(24):3746–3752
Meignan M, Gallamini A, Meignan M, Gallamini A, Haioun C (2009) Report on the First International Workshop on Interim-PET-Scan in Lymphoma. Leukemia Lymphoma 50(8):1257–1260
Johnson P, Federico M, Kirkwood A, Fossa A, Berkahn L, Carella A et al (2016) Adapted treatment guided by interim PET-CT scan in advanced Hodgkin’s Lymphoma. New Engl J Med 374(25):2419–2429
Gallamini A, Tarella C, Viviani S, Rossi A, Patti C, Mule A et al (2018) Early chemotherapy intensification with escalated BEACOPP in patients with advanced-stage Hodgkin lymphoma with a positive interim positron emission tomography/computed tomography scan after two ABVD cycles: long-term results of the GITIL/FIL HD 0607 trial. J Clin Oncol 36(5):454–462
Borchmann P, Goergen H, Kobe C, Lohri A, Greil R, Eichenauer DA et al (2018) PET-guided treatment in patients with advanced-stage Hodgkin’s lymphoma (HD18): final results of an open-label, international, randomised phase 3 trial by the German Hodgkin Study Group. Lancet 390(10114):2790–2802
Press OW, Li H, Schoder H, Straus DJ, Moskowitz CH, LeBlanc M et al (2016) US intergroup trial of response-adapted therapy for stage III to IV Hodgkin lymphoma using early interim fluorodeoxyglucose-positron emission tomography imaging: Southwest Oncology Group S0816. J Clin Oncol 34(17):2020–2027
Zinzani PL, Broccoli A, Gioia DM, Castagnoli A, Ciccone G, Evangelista A et al (2016) Interim positron emission tomography response-adapted therapy in advanced-stage Hodgkin lymphoma: final results of the phase II part of the HD0801 Study. J Clin Oncol 34(12):1376–1385
Kobe C, Goergen H, Baues C, Kuhnert G, Voltin CA, Zijlstra J et al (2018) Outcome-based interpretation of early interim PET in advanced-stage Hodgkin lymphoma. Blood 132(21):2273–2279. https://doi.org/10.1182/blood-2018-05-852129
Casasnovas RO, Brice P, Lazarovici J, Ghesquieres H, Stamatoullas A, Dupuis J et al (2019) PET-adapted treatment of patients with advanced Hodgkin lymphoma (AHL2011): final results of a randomised, multi-centre, phase 3 study. Lancet 20(2):202–215
Biggi A, Gallamini A, Chauvie S, Hutchings M, Kostakoglu L, Gregianin M et al (2013) International validation study for interim PET in ABVD-treated, advanced-stage Hodgkin lymphoma: interpretation criteria and concordance rate among reviewers. J Nucl Med 54(5):683–690
Borchmann P, Haverkamp H, Lohri A, Mey U, Kreissl S, Greil R et al (2017) Progression-free survival of early interim PET-positive patients with advanced stage Hodgkin’s lymphoma treated with BEACOPP escalated alone or in combination with rituximab (HD18): an open-label, international, randomised phase 3 study by the German Hodgkin Study Group. Lancet Oncol 18(4):454–463
Younes A, Gopal AK, Smith SE, Ansell SM, Rosenblatt JD, Savage KJ et al (2012) Results of a pivotal phase II study of brentuximab vedotin for patients with relapsed or refractory Hodgkin’s lymphoma. J Clin Oncol 30(18):2183–2189
Younes A, Connors JM, Park SI, Fanale M, O’Meara MM, Hunder NN et al (2013) Brentuximab vedotin combined with ABVD or AVD for patients with newly diagnosed Hodgkin’s lymphoma: a phase 1, open-label, dose-escalation study. Lancet Oncol 14(13):1348–1356
Connors JM, Ansell SM, Fanale M, Park SI, Younes A (2017) Five-year follow-up of brentuximab vedotin combined with ABVD or AVD for advanced-stage classical Hodgkin lymphoma. Blood 130(11):1375–1377
Connors JM, Jurczak W, Straus DJ, Ansell SM, Kim WS, Gallamini A et al (2018) Brentuximab vedotin with chemotherapy for stage III or IV Hodgkin’s Lymphoma. New Eng J Med 378(4):331–344
Chen RW, Gallamini A, Connors JM, Savage KJ, Collins GP, Grigg A et al (2018) Brentuximab vedotin with chemotherapy for stage III or IV Hodgkin lymphoma (HL): Impact of cycle 2 PET result on modified progression-free survival (mPFS). J Clin Oncol 36:abstr 7539
Eichenauer DA, Plutschow A, Kreissl S, Sokler M, Hellmuth JC, Meissner J et al (2017) Incorporation of brentuximab vedotin into first-line treatment of advanced classical Hodgkin’s lymphoma: final analysis of a phase 2 randomised trial by the German Hodgkin Study Group. Lancet Oncol 18(12):1680–1687
Roemer MG, Advani RH, Ligon AH, Natkunam Y, Redd RA, Homer H et al (2016) PD-L1 and PD-L2 genetic alterations define classical Hodgkin lymphoma and predict outcome. J Clin Oncol. 34(23):2690–2697
Ramchandren R, Domingo-Domènech E, Rueda A, Trněný M, Feldman TA, Lee HJ et al (2019) Nivolumab for newly diagnosed advanced-stage classic Hodgkin lymphoma: safety and efficacy in the phase II checkmate 205 study. J Clin Oncol 37(23):1997–2007. https://doi.org/10.1200/JCO.19.00315. PMID: 31112476
Loeffler M, Brosteanu O, Hasenclever D, Sextro M, Assouline D, Bartolucci AA et al (1998) Meta-analysis of chemotherapy versus combined modality treatment trials in Hodgkin’s disease. International Database on Hodgkin’s Disease Overview Study Group. J Clin Oncol 16(3):818–829
Andrieu JM, Yilmaz U, Colonna P, Loeffler M, Brosteanu O, Hasenclever D (1999) MOPP versus ABVD and low-dose versus high-dose irradiation in Hodgkin’s disease at intermediate and advanced stages: analysis of a meta-analysis by clinicians. J Clin Oncol 17(2):730–732
Aleman BM, Raemaekers JM, Tirelli U, Bortolus R, van’t Veer MB, Lybeert ML et al (2003) Involved-field radiotherapy for advanced Hodgkin’s lymphoma. New Engl J Med 348(24):2396–2406
Ferme C, Mounier N, Casasnovas O, Brice P, Divine M, Sonet A et al (2006) Long-term results and competing risk analysis of the H89 trial in patients with advanced-stage Hodgkin lymphoma: a study by the Groupe d'Etude des Lymphomes de l'Adulte (GELA). Blood 107(12):4636–4642
Kriz J, Reinartz G, Dietlein M, Kobe C, Kuhnert G, Haverkamp H et al (2015) Relapse analysis of irradiated patients within the HD15 trial of the German Hodgkin Study Group. Int J Radiat Oncol 92(1):46–53
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fosså, A., Casasnovas, RO., Johnson, P.W.M. (2020). Treatment of Advanced-Stage Hodgkin Lymphoma. In: Engert, A., Younes, A. (eds) Hodgkin Lymphoma. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-32482-7_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-32482-7_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32481-0
Online ISBN: 978-3-030-32482-7
eBook Packages: MedicineMedicine (R0)