Abstract
Radiology as a specialty came into being due to a series of significant discoveries in the field of physics. A succession of innovators has taken novel scientific phenomena, and from them developed strategies to image the human body.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Radiology as a specialty came into being due to a series of significant discoveries in the field of physics. A succession of innovators has taken novel scientific phenomena, and from them developed strategies to image the human body.
Paediatric radiology as a separate subspecialty is relatively new, although the first clinical X-ray taken in America, on 3 February 1896, was of a 14-year-old boy’s wrist. The first book specifically concerned with paediatric radiology was published in 1910.
In the 1940s, John Caffey described the association of multiple long bone fractures and chronic subdural haematomas, creating the debate that first established the existence of physical child abuse. Radiology continues to have a prominent role in the investigation of this condition. Caffey published his landmark textbook Pediatric X-Ray Diagnosis in 1945, which now continues in 2018 in its thirteenth edition.
The Society for Pediatric Radiology (SPR) was founded in America in 1958, electing Edward Neuhauser as its president, and was followed by the establishment of the European Society of Paediatric Radiology (ESPR) in 1963. Paediatric neuroradiology emerged as the first formal subspecialty of paediatric radiology during the late 1960s.
1.2 Discovery of the X-Ray
X-rays were discovered on 8 November 1895 by Wilhelm Conrad Röntgen, working in Wurzburg, Germany. Perhaps appropriately for the father of radiology, the discovery was made in a darkened room. He was performing experiments with cathode ray tubes, where streams of electrons pass across a vacuum, colliding forcefully with the metal of the anode. The tubes were entirely covered so that no light could escape, but nonetheless Röntgen observed that a screen several feet from the tube began to fluoresce when the current was applied.
It was apparent that some sort of invisible ray was being emitted by the tube and shining upon the screen. These he termed X-rays; the designation “x” was intended to be a temporary name, indicating that the nature of the ray was unknown. He immediately began to investigate the properties of this new form of ray. His earliest experiments investigated the ability of the X-rays to cast a shadow from various objects interposed between the tube and the screen, and recorded the results upon a photographic plate. Rather than stopping all of the X-rays, objects were shown to be variably transparent. Paper, wood, and cloth were penetrated easily, as were, to differing degrees, various metals.
One of the first recorded X-rays of a living human was performed on the hand of Röntgen’s wife Anna-Bertha. Due to the low output of the unmodified tube, the exposure time was in the region of 30 min. By contrast, a modern hand X-ray exposure time is in the region of milliseconds. These early X-rays immediately showed their potential in medical investigation, successfully localising glass and metallic foreign bodies in various patients and facilitating their removal.
Röntgen’s paper entitled “On a New Kind of Rays” (Übereineneue Art von Strahlen) was immediately published in December 1895. News of his discovery quickly spread, and Röntgen became famous and bestowed with many honours, including the Nobel Prize for Physics in 1901.
What is believed to be the first medical X-ray department in the world was set up in Glasgow Royal Infirmary, Scotland, in March 1896, by Dr. John Macintyre. Röntgen had sent a copy of his paper to Lord Kelvin in Glasgow in early 1896, who passed it on to Macintyre’s group, along with necessary apparatus. Some of the examinations attributed to this department include the first X-ray depictions of a bullet, and another of a coin in the oesophagus (Figs. 1.1, 1.2, and 1.3)
Due to the long exposure times, early radiographs were much more successful in imaging the peripheral skeleton than the chest or abdomen, where movement artefact and the thickness of the tissues spoiled the images. Improvements in X-ray tube design allowed for shorter exposures, as did advances in the construction of the film plates. Fluoroscopy was achieved by the examiner holding a fluorescent screen between his eyes and the patient, all the time directly in the path of the primary X-ray beam!
Although there were many early reports of skin damage, the harmful effects of radiation were not initially fully appreciated. Many early X-ray workers suffered burns, lost fingers, hands, or eyes, or succumbed to radiation-induced cancers. The Martyrs Memorial to 169 who lost their lives was dedicated in 1936 outside the Röntgen Institute of St. George’s Hospital in Hamburg.
Modern X-ray set ups still use X-ray tubes based on the same design. They are, however, heavily shielded, and include collimators to enable the area irradiated to be minimized. Films have been replaced with digital sensors, and the processed images are sent electronically to picture archiving and communications systems (PACS). The images are then immediately available for reviewing at multiple geographically separate locations. Currently a National PACS system is installed and accessible across the whole of Scotland, on which all imaging modalities are stored.
1.3 Ultrasound
Medical ultrasound has its roots in the development of SONAR (Sound navigation and ranging). In the First World War, experiments were underway to develop sonar for submarines. It was known that bats could navigate by listening for the echoes of the high frequency sound waves they produced, and it was hoped to replicate this principle underwater. The sinking of the RMS Titanic after it struck an iceberg in 1912 had added impetus to the project.
An early system developed in 1914 by Fessenden was partially successful, but its direction-finding ability was limited owing to the low frequency of the sound waves it used. High-frequency sound waves (hence ultra sound) were produced with quartz crystals glued between steel plates by the French physicist Paul Langévin, using the piezoelectric effect. This is where crystals are caused to change size and vibrate by passing electrical currents through them and vice versa (the inverse piezoelectric effect). This produced a short “chirp” of high-frequency sound underwater. By timing how long it took the echo to return, and knowing the speed of sound in water, it was possible to determine the distance from the source of the sound to the source of the echo. In practice, this gave the distance from the ship to the submarine/seabed/iceberg. The pulse echo technique was developed using radio waves rather than sound waves in the development of RADAR (radio detection and ranging).
A parallel field of study was in the use of ultrasound to detect otherwise invisible flaws in metal. During the Second World War, several groups were investigating the technique at the same time in different countries. Wartime also proved the catalyst for further sonar development.
The application of ultrasound to medicine was initially confined to attempts at therapy, rather than diagnosis. High-frequency ultrasound generated heat, which was used in many conditions as symptomatic treatment. The destructive force of high-energy sound waves was also used as a neurosurgical tool for ablation of parts of the brain.
Working in America in the late 1940s, George Ludwig began animal experiments using metal flaw-detector equipment to identify foreign bodies, such as gallstones that had been surgically implanted into dogs. His work established many fundamental concepts of diagnostic ultrasonography.
Ian Donald, an obstetrician and gynaecologist working in Glasgow, Scotland, conducted experiments on tumours freshly removed from human patients. The ultrasound device was provided by a local boilermaker, where it was used to check the integrity of metal welds. It was immediately apparent that different traces were produced by different masses, and further experiments on in vivo tumours were planned. Difficulties were encountered in transferring the industrial equipment to clinical usage. Initially a small bucket of water with a latex bottom was placed on the patient’s abdomen, which itself was smeared with lubricating jelly to exclude air. The ultrasound probe was then applied to the surface of the water. Subsequently, direct application of the probe to the skin, with olive oil as a coupling film, proved less hazardous. There was an early clinical success: a middle-aged woman thought to be dying of a gastric carcinoma with ascites, was instead shown to have an enormous ovarian cyst. This was removed, and the patient made a full recovery. Donald notes in his memoir, however, that after this success he was “inflicted with horrid specimens of [the patient’s] grandchild’s attempts at cooking by way of an expression of gratitude.”
Donald went on to publish a landmark paper in the Lancet of 7 June 1958, “Investigation of abdominal masses by pulsed ultrasound.” His co-worker James Willocks went on to establish the utility of biparietal measurement of the fetal skull to measure growth (Figs. 1.4 and 1.5).
From the mid-1960s there was a rapid increase in the use of diagnostic ultrasound, matched with great enhancements in the scanning machines. Early commercial machines were large and cumbersome, with either large fixed gantries or articulated probe arms. Original (A mode) scan displays were simply blips on an oscilloscope trace, although accurate measurements with these systems were possible. More advanced electronics needed to be developed before cross-sectional (B mode) images with grey scale could be produced. The next major innovation was that of real-time scanning, which relied upon mechanical rotating or oscillating transducers to quickly sweep back and forth across the area of interest, building up a moving picture. These in turn have been superseded by electronic phased array transducers. Doppler techniques have developed in parallel to grey scale imaging, and from the outset have allowed investigation of the movement of heart valves, and the flow of blood in peripheral vessels. The increasing processing power of newer computers has enabled the addition of 3D scanning, which uses advanced surface shading and volume rendering (Fig. 1.6). Further developments in ultrasound elastography, and contrast agent imaging are gaining widespread clinical use.
1.4 Computed Tomography
Sir Godfrey Hounsfield, an English engineer, invented the computed tomography (CT) scanner. During the Second World War he joined the Royal Air Force as a radar mechanic instructor. Joining EMI in 1951, he initially continued his work on radar and guided weapons. He subsequently led the design team building the first all-transistor computer to be built in Britain.
During a walk in the countryside in 1967, Hounsfield had the germ of the idea that was to become computerised tomography. He realized that “you could determine what was in a box simply by taking readings at all angles through it.” In practice, this required a minicomputer to reconstruct a picture from X-ray measurements taken through the body at a multitude of different angles. The computer was essential because hundreds of thousands of calculations would need to be made.
Initial tests with gamma rays were too slow, but even switching to X-rays still required a scanning time of 9 h. The first scan of human tissue was performed on a preserved human brain from a local hospital museum, and successfully showed differentiation of grey and white matter. Fearing that the preservation process had enhanced the images, Hounsfield substituted fresh bullocks’ brains. In scanning through the carcasses of pigs, problems were encountered as each picture took a day to acquire, during which gas bubbles formed and expanded within the tissues.
Faster prototypes were produced, and the first patient was scanned on 1 October 1971 at Atkinson Morley’s Hospital in South London. The patient had a suspected brain lesion, and the scan demonstrated a frontal cyst. The next step was a machine capable of scanning the body, and a larger and faster scanner was produced capable of taking a picture in 18 s. The first body images produced in the body prototype were of Hounsfield himself.
Hounsfield proposed a scale for measuring the relative absorption values in CT, from 1,000 for bone, 20–40 for tissue, 0 for water and −1000 for air. These Hounsfield units remain the standard unit for CT imaging density. He was awarded the Nobel Prize in Physiology or Medicine in 1979, sharing the honour with Allan Cormack, a South African physicist of Scottish descent.
1.5 Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is a complicated imaging technique, and the history of its development is no less complex. In many ways it is well suited to investigate children, giving fantastically detailed images with unparalleled soft-tissue contrast. However, the machine is expensive and apt to induce claustrophobia, and the long scan times may require sedation or general anaesthetic for younger patients. The use of strong magnetic fields precludes scanning of patients with certain metallic implants, but the absence of ionizing radiation secures it a place in the arsenal of the paediatric radiologist.
Expressed simply, placing the body in a strong magnetic field causes the hydrogen nuclei of the water molecules found throughout the body to line up. A brief radio wave is applied, which pushes these protons out of alignment. When the protons flick back into line, they release energy, which is detected and localised by the scanner. Areas with lots of water release relatively more energy, and the scanner builds up a cross-sectional picture of the body, depending upon the amount of water, and therefore the amounts of energy released.
MRI was initially termed Nuclear Magnetic Resonance (NMR). Working independently in the 1940s, Felix Bloch at Stanford University and Edward Purcell at Harvard University found that some nuclei in a magnetic field absorbed radiofrequency range energy and emitted this energy upon returning to their original state. Their discoveries in nuclear magnetic absorption earned them each a share of the Nobel Prize in Physics in 1952. NMR spectroscopy was used by physicists to investigate the properties of small samples in high-strength magnetic fields, not to produce anatomical images.
In the early 1970s, Raymond Damadian found that normal and cancerous tissue could be separated in vitro according to different physical parameters using NMR. This raised the possibility of non-invasive tumour characterisation, and in 1974 Damadian constructed a scanner with the intention of analysing the whole body.
In 1973 Paul Lauterbur, a professor of chemistry at the State University of New York, published a paper in Nature describing an imaging technique for the spatial localization of two capillary tubes of water inside a narrow tube of heavy water. The introduction of gradients allowed two-dimensional images to be produced. Reportedly, he was eating a hamburger at the time when the idea occurred, and he jotted it down on a napkin. The development of this idea resulted in the award of the 2003 Nobel Prize in Physiology or Medicine, shared with Sir Peter Mansfield. Mansfield is a British physicist who further developed the utilisation of gradients and showed how the signals could be mathematically analysed to develop a useful imaging technique. He discovered how fast imaging could be performed with the echo planar technique, and laid the basis for functional MRI.
By 1980, Edelstein and Hutchison at the University of Aberdeen in Scotland had developed a practical two-dimensional imaging technique, dubbed “spin-warp imaging,” and the world’s first clinical diagnostic MRI service was started at the Aberdeen Royal Infirmary in August of that year.
1.6 Nuclear Medicine
Nuclear medicine uses radioactive isotopes to image the body and to treat disease. As the isotopes can be attached to various pharmaceutical compounds, analysis of a wide range of physiological function and anatomy is possible. Two important applications of nuclear medicine in the field of paediatric radiology are imaging of the renal tract and oncology.
The 1903 Nobel Prize for Physics was shared by Henri Becquerel and Marie and Pierre Curie for their work in the discovery of radioactivity. Whilst investigating a possible connection between Röntgen’s X-rays and natural phosphorescence in 1896, Bequerel discovered by chance that uranium emitted radiation that exposed photographic film. Marie and Pierre Curie continued his work, discovering polonium (named after Marie’s native Poland) and radium.
Unfortunately, some early applications of radioactivity included the addition of radioactive compounds to water as a cure-all, and to toothpaste promising “radioactive brilliance.”
The use of radioactivity in imaging required the use of tracers with a short half-life, to limit the potential for side effects. In 1937 iodine-131 was created, followed by the production of technetium-99m in 1938, which remains the most commonly used isotope in nuclear medicine. These and many other isotopes were created using a cyclotron, an apparatus that accelerates charged particles to great speed in a vacuum chamber and fires them at a target. The cyclotron was invented and developed by Ernest Lawrence, later to receive the Nobel Prize in Physics for his work (and to have the element lawrencium named in his honour).
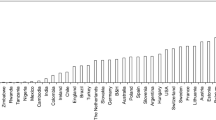
The use of isotopes in imaging was revolutionised in the1950s by the invention and development of the first clinically successful scintillation camera by Hal Anger at the University of California at Berkeley. The design principle of his gamma camera was so successful that it is still the basis of most of those used today. The technology has evolved to form the basis of single photon-emission computed tomography (SPECT) and positron emission tomography (PET), which permit cross-sectional imaging, analogous to CT. SPECT uses standard nuclear medicine tracers, but PET uses a different class of short-lived tracers that emit positrons, also produced in a cyclotron. The necessity of an accessible cyclotron has slowed the introduction of PET. As of 2008 there were approximately 1500 PET centres in the United States of America, while in the United Kingdom the modality was only emerging as a highly specialized regional service. The most widely used PET tracer is currently fluorine-18 fluoro-deoxy-glucose (FDG), which produces images of tissue metabolism.
The images produced in nuclear medicine are generally of low resolution, and these can now be enhanced by combining the images with high resolution CT techniques, hence SPECT/CT and PET/CT. The fused images produced by these complementary techniques combine functional information with anatomical detail, and these can be used to improve the localization of certain disease processes and enhance diagnostic accuracy. The primary application of PET in children is in oncology, where it particularly useful for the diagnosis and staging of disease, as well as for assessing the response of individual treatments.
1.7 Dose Considerations and ALARA
ALARA stands for “as low as reasonably achievable,” and this is the guiding principle where ionising radiation is being used. The most effective way to reduce dose is to not perform the examination at all! X-rays, fluoroscopy, CT scans, nuclear medicine studies, and PET all use ionising radiation, and consideration should be given as to whether the information sought could be obtained using ultrasound or MRI scanning. If not, then the examination should be tailored to use the minimum radiation dose necessary to produce diagnostic images. To an extent, the risks of relatively low levels of radiation are unknown. Nonetheless, it is prudent and responsible to minimise any chance of potential iatrogenic injury to our patients. Children’s tissues are inherently more radiosensitive than those of adults, and children also have longer to live and develop delayed (stochastic) effects of radiation.
Good communication between the surgeon and radiologist is vital to allow a collaborative approach to dose reduction. A close working relationship reduces errors and, particularly in emergency situations, the surgeon will often be present during the study.
Further Reading
Anger HO. A new instrument for mapping gamma-ray emitters. Biol Med Quart Rep. 1957;3653:38.
Burrows EH. Pioneers and early years: history of British radiology. Alderney: Colophon; 1986.
Coley BD. Caffey’s Pediatric Diagnostic Imaging. 13th ed. Elsevier; 2018.
Donald I, MacVicar J, Brown TG. Investigation of abdominal masses by pulsed ultrasound. Lancet. 1958;271(7032):1188–95.
Griscom NT. History of pediatric radiology in the United States and Canada: images and trends. Radiographics. 1995;15(6):1399–422.
Hong J-Y, Han K, Jung J-H, Kim JS. Association of exposure to diagnostic low-dose ionizing radiation with risk of cancer among youths in South Korea. JAMA Network Open. 2019;2(9):e1910584.
Kirks DR. Eugene W. Caldwell lecture. Pediatric imaging: the oldest radiological subspecialty comes of age. Am J Roentgenol. 1999;172(2):291–9.
Rosenbusch G, Oudkerk M, Ammann E, Winter PF. Radiology in medical diagnostics: evolution of X-ray applications 1895–1995. Oxford: Blackwell Science; 1995.
Rotch TM. Living anatomy and pathology: the diagnosis of diseases in early life by the roentgen method. Philadelphia, PA: Lippincott; 1910.
Slovis I. Caffey’s pediatric diagnostic imaging. 11th ed. Philadelphia, PA: Mosby; 2007.
The Nobel Prize. Wilhelm Conrad Röntgen. Biographical. https://www.nobelprize.org/prizes/physics/1901/rontgen/biographical/. Accessed 21 Oct 2018.
The Nobel Prize. Godfrey N. Hounsfield. Biographical. https://www.nobelprize.org/prizes/medicine/1979/hounsfield/auto-biography/. Accessed 21 Oct 2018.
Willocks J, Barr W. Ian Donald: a memoir. London: RCOG Press; 2004.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Irwin, G.J. (2020). Introduction: Paediatric Radiology. In: Carachi, R. (eds) Atlas of Paediatric Surgical Imaging. Springer, Cham. https://doi.org/10.1007/978-3-030-32384-4_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-32384-4_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32383-7
Online ISBN: 978-3-030-32384-4
eBook Packages: MedicineMedicine (R0)