Abstract
Oral cancer is a serious health problem and appears to be amenable to screening. The oral cavity is easy to examine, and studies have shown that healthcare workers can detect oral potentially malignant lesions with a sensitivity and specificity similar to that found to be acceptable in other screening programs. However, there remain considerable barriers to the implementation of screening programs. The criteria for a positive test may not detect the lesions that are most likely to be malignant or that will progress to malignancy, and there is a lack of evidence to show that a screening program will reduce mortality. Studies have suggested that opportunistic screening of high-risk groups may be effective and cost-effective, but further research is needed to refine the criteria for a positive screen and to determine the best methods for identifying and targeting high-risk groups.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Oral cancer is a serious health problem and appears to be amenable to screening. The oral cavity is easy to examine, and studies have shown that healthcare workers can detect oral potentially malignant lesions with a sensitivity and specificity similar to that found to be acceptable in other screening programs. However, there remain considerable barriers to the implementation of screening programs. The criteria for a positive test may not detect the lesions that are most likely to be malignant or that will progress to malignancy, and there is a lack of evidence to show that a screening program will reduce mortality. Studies have suggested that opportunistic screening of high-risk groups may be effective and cost-effective, but further research is needed to refine the criteria for a positive screen and to determine the best methods for identifying and targeting high-risk groups.
16.1 Definition and Principles of Cancer Screening
16.1.1 Definitions
Early detection and prevention of cancer is a major component of cancer control programs worldwide and is an important part of the World Health Organization’s efforts to reduce mortality and morbidity from cancer [1, 2]. Cancer prevention encompasses a range of interventions that can be divided into three main groups, referred to as primary , secondary, and tertiary prevention . Primary prevention aims to prevent disease before it occurs, by reducing or eliminating exposure to causative agents. In the case of oral cancer, this may involve programs to reduce tobacco and alcohol use, either through health education or by fiscal measures. Tertiary prevention aims to reduce the impact of established disease, using measures to improve quality of life through better treatment or by rehabilitation and long-term care of survivors. Cancer screening is a component of secondary prevention , which aims to detect disease early when it can be effectively treated. Cancer screening must be distinguished from early diagnosis or case-finding, which involves detecting and diagnosing disease in symptomatic people, as early as possible, so that effective treatment can be implemented while there is still a good chance of a cure. Programs aimed at early diagnosis often include health education to encourage the public and health professionals to recognize the early signs and symptoms of disease.
In contrast, screening involves early detection of cancer in asymptomatic people. Screening has long been defined as the identification of unrecognized disease by the application of a test to people who are asymptomatic, in order to identify those who probably have the disease and to distinguish them from those who probably do not [3]. It is important to note that a screening test is not intended to be diagnostic but aims to identify changes that are associated with an increased likelihood of cancer, initiating the application of more specific diagnostic procedures. Therefore, a screening test may be designed to detect premalignant changes as well as evidence of early malignancy. This, for example, is the underlying principle of the “smear” test for cervical cancer, which identifies atypical cells that may be associated with premalignancy or with actual cancer.
16.1.2 Principles and Criteria for Screening
Screening is an ongoing process of testing well people at regular intervals and must include methods for identifying the target population and provision for onward referral for diagnosis and treatment. Implementation of a screening program therefore has significant resource implications as well as a number of potential disadvantages. It is now more than 50 years since Wilson and Jungner [3] established ten principles that should be met for the implementation of a successful screening program. With some contemporary rewording, these are shown in ◘ Table 16.1. These principles have been adapted and expanded over the years, to reflect the higher standards of evidence required to prove effectiveness and to address increasing concerns about ethical issues and overdiagnosis whereby subjects may be over-investigated or overtreated without gaining benefit (see ► Section 16.2.1). For example, the National Screening Committee of the United Kingdom now lists 20 criteria that must be considered before a screening program can be funded and implemented [4]. As well as the ten basic principles, the criteria include evidence of adequate test performance, evidence from randomized trials that screening will reduce mortality or morbidity in the population, provisions for genetic testing, and that all primary preventive programs have been implemented wherever possible. Agencies in the United States have similar criteria [5, 6]. Importantly, these criteria also require that the benefits and advantages of screening outweigh the disadvantages and any potential physical or psychological harm to subjects. The potential advantages and disadvantages of a screening program are summarized in ◘ Table 16.2. The disadvantages are particularly important and may be insurmountable, meaning that a program cannot be implemented. In the United Kingdom, 30 screening programs have been implemented, but only 3 are for cancers: cervical cancer, breast cancer, and bowel cancer. Worldwide, few cancer screening programs have been introduced, and no country has yet organized a national screening program for oral cancer [7]. The reasons for this will be considered in the context of oral cancer later in this chapter.
Key Features of a Cancer Screening Program
-
Early detection of disease in people who are otherwise asymptomatic.
-
Uses a test to detect early stages of cancer or changes of precancer.
-
The test identifies those who probably have the disease, to distinguish them from those who probably do not.
-
The screening test is not diagnostic. Those screened positive are referred for more specific diagnostic tests.
-
Screening is an ongoing process repeated at intervals and includes protocols for managing people who screen positive and must include effective treatment of screen-detected disease.
-
The outcome must be a reduction in mortality in the whole population offered screening. If the screening test also aims to detect precancer, then a further expected outcome will be reduced incidence of invasive cancer.
16.2 Evaluation of Screening
16.2.1 Evaluation of a Screening Test
The validity or accuracy of a test is determined by the proportion of the results that are confirmed as truly positive or negative by an acceptable diagnostic procedure – often referred to as the “gold-standard” diagnosis. An ideal screening test would correctly identify all individuals in the screened population with the disease as positive and all individuals without the disease as negative. However, this never happens and, therefore, there must be a balance between how well the screening test correctly classifies people with the disease (sensitivity) and how well it classifies people without the disease (specificity). The possible outcomes of a test are illustrated in ◘ Fig. 16.1, and definitions of these and the metrics used to evaluate a test are shown in ◘ Tables 16.3 and 16.4. The most widely used metrics are the sensitivity and specificity , and in general the calculation of these parameters is regarded as essential in the evaluation of a test. However, obtaining the data to do this can be very difficult because it is necessary to determine the number of true (TN) and false (FN) negatives. This means that all individuals subjected to the screening test who are negative must also be subjected to the gold-standard diagnostic test to prove they are truly negative. In large studies, where a disease may be of low prevalence, this can be a difficult or impossible undertaking and may be too expensive to justify funding. In this case, the PPV may be used as an acceptable substitute .
There is no agreed definition for what constitutes an acceptable test, and there must always be a “trade-off” between sensitivity and specificity . While it is important that the test records a low number of false positives (FP), to prevent unnecessary overdiagnosis and anxiety, it is also important that the number of false negatives (FN) is kept as low as possible so that disease is not missed. Acceptable tests generally have a sensitivity and specificity of 0.8 or more, but in order to capture and treat as many cancers as possible, a higher sensitivity is preferable – but this will result in more false positives and may come at extra cost .
16.2.2 Lead-Time Bias
A major unintentional consequence of early detection of cancer is that it may result in overdiagnosis of disease and cause many people to receive unnecessary treatment. This is called lead-time bias and refers to a situation where a screening test detects disease which may be asymptomatic but is already so far advanced that treatment is not effective and will not prolong life (◘ Fig. 16.2). For example, screening tests for lung cancer proved ineffective, because when disease was detected, even in asymptomatic patients, it was already advanced and treatment would not prolong life [8]. ◘ Figure 16.2 shows that the earlier diagnosis due to a positive screen results in an apparent increase in survival, but in reality, life is not prolonged and the patient dies at the same age. The outcome for the patient does not change, but they are subjected to unnecessary treatment after the screen and to the psychological trauma of living with cancer for a longer period than is necessary. ◘ Figure 16.3 illustrates an effective screening program, such as cervical cancer screening. In this case, subject (b) benefits from a positive screen early in life, and effective treatment results in a prolongation of life and a true increase in survival compared to subject (a), whose cancer presents late with symptoms and dies soon after .
A phenomenon similar to lead-time bias is referred to as length-time bias. In this situation, a sensitive screening test detects small slow-growing cancers, which may be less aggressive and may not have killed the patient or even become clinically apparent within their natural lifetime. In this case, the screening results in unnecessary treatment as well as the psychological trauma of being diagnosed with a disease that, in the absence of the screen, the patient may never have known about. This scenario applies to prostate cancer where the PSA test (for prostate-specific antigen) may be too sensitive and may also lack specificity .
16.2.3 Evaluation of a Screening Program
Although a test may have adequate sensitivity and specificity , it must also be demonstrated that it is able to detect relevant lesions in the context of a screening program and that the program achieves the desired objectives for successful implementation (◘ Table 16.1) [3, 4]. In particular, it is expected that a screening program for cancer will reduce mortality and morbidity, and ideally this should be tested in a prospective randomized controlled trial (RCT). In such a project, populations are randomized to a screened and non-screened group and the mortality is compared [9]. The primary outcome is a significant reduction in mortality in the whole population that was offered screening. In reality, RCTs of this scale are very difficult to carry out, since they must often involve hundreds of thousands of subjects with follow-up long enough to determine mortality – usually for about 10 years. The number of participants needed is greater for cancers with a low prevalence such as oral cancer. Few RCTs of this nature have been undertaken, but one, in the context of oral cancer, will be discussed in a subsequent section. Alternative research methods include retrospective cohort studies, where the incidence of disease and mortality in a population that has been offered screening are compared to a population that has not been screened. A similar study design may compare the same population before and after the implementation of the screening program. Cervical cancer is of relatively low incidence , and the effectiveness of screening programs has mostly been determined in retrospective cohort studies. Breast and bowel cancer screening however have been evaluated in RCTs, since the diseases have high incidence and the number of subjects required may be less than 100,000 [10]. RCTs for prostate cancer screening are currently ongoing [11].
Once a screening program has been introduced, or is under evaluation, a number of interim or surrogate measures can be applied that can suggest whether or not the program is likely to bring about a satisfactory outcome [9, 12] (◘ Table 16.5).
16.3 Screening for Oral Cancer
16.3.1 Is Oral Cancer an Important Health Problem?
Worldwide, there are an estimated 300,000 new cases of oral cancer per annum and145,400 deaths, making it one of the most common cancers [13, 14]. Although there are wide variations in incidence , overall about two-thirds of cases occur in the developing world [14]. There is also good evidence that oral cancer is increasing in incidence throughout the world [13] with significant increases in younger people. In recent decades, there have been some major advances in treatment, but despite this, the 5-year survival rate has not improved and remains at about 50%. The most important reason for this, even in developed countries, is diagnostic delay , with more than 60% of patients presenting with late-stage disease (stages III/IV) [15], when complex multimodality therapy may be needed. Cancers detected when they are small or at an early stage however can be treated by simple surgery, with a good chance of cure. For example, in a UK study, the 5-year survival for stage I oral cancer was 96%, while patients presenting at stage IV had only 57% survival [16].
The majority of oral cancers are preceded by a clinically detectable potentially malignant lesion, the most common of which is a white patch or leukoplakia [17]. This suggests that a screening program to detect preinvasive disease may also be feasible and may reduce the incidence of established lesions of oral cancer.
Taken together, these data show that oral cancer is a significant health problem and that screening is feasible since there is good evidence for a detectable premalignant lesion and early detection of established cancers should result in improved survival. The disease appears to meet the first four principles suggested by Wilson and Jungner (◘ Table 16.1) [3].
16.3.2 Evaluation of a Screening Test for Oral Cancer
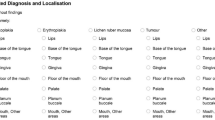
The efficacy of a screening test is ideally determined by measures of sensitivity and specificity, as discussed in ► Section 16.2.1. The most widely studied test for oral cancer screening has been a conventional oral examination. However, only nine studies have been reported that have properly determined the sensitivity and specificity by retesting negative cases against the gold-standard diagnosis [18,19,20,21,22,23,24,25,26]. These are summarized in ◘ Table 16.6. In all studies, the criterion for a positive screen was the finding of a persistent red or white lesion or ulcer, which encompassed a range of lesions regarded as potentially malignant, including leukoplakia, erythroplakia, lichen planus, and submucous fibrosis. However, other nonrelevant lesions, for example, benign hyperkeratotic lesions, may have been regarded as positive. In most studies, the screen was carried out by a dental professional, but some used trained nonmedical or non-dental healthcare workers [23,24,25], with similar results.
Walsh et al. [27] undertook a Cochrane systematic review of test accuracy that reviewed a number of these studies [18,19,20,21,22,23,24,25] and found a variable degree of sensitivity (0.50 to 0.99) but a consistently high value for specificity (greater than 0.80). They also examined vital staining, light-based detection (including fluorescence), biomarkers, and mouth self-examination as potential screening tests but found insufficient evidence to determine their test accuracy. A meta-analysis of some of these studies [28] found pooled values of sensitivity of 0.85 (95%CI; 0.73–0.92) and specificity of 0.97 (95%CI; 0.93–0.98).
These analyses have shown that an oral examination can correctly identify oral lesions with a sensitivity and specificity of 0.8 or greater, which is regarded as acceptable and is similar to the test performance in established screening programs [9]. These data further support the view that oral cancer screening may be feasible and that both dentists and trained healthcare workers can accurately detect oral lesions (◘ Table 16.6).
16.3.3 Application of an Oral Examination as a Screening Test
Although an oral examination may show a satisfactory degree of accuracy and reproducibility, the use of this as a test in a real-world screening scenario is controversial. As discussed above, most research studies have reported using the presence of an oral potentially malignant disorder or early oral cancer as the criteria for a positive screen. The lesion most often detected in screening studies is a white patch or leukoplakia, which is a common lesion with an estimated global prevalence of 2.6% [17, 29], but its natural history is not fully understood since progression to cancer is not predictable and it is almost impossible to clearly categorize which lesions will transform to cancer [30]. In addition, the overall malignant transformation rate is estimated to be less than 5% [31]. Lesions at the highest risk may have a nonhomogeneous surface and show evidence of epithelial dysplasia on biopsy [31,32,33], but these features may not be evident on screening and may not be suitable for a screening test. In real terms, up to 95% of the lesions detected by oral examination may not progress to malignancy and a white patch cannot therefore be used as the criteria for a positive test that should only detect lesions with the highest probability of progressing to cancer. It is not economically feasible to treat all screen-detected white patches in the hope that the less than 5% that may have progressed will be included. This is a major barrier for the implementation of an oral cancer screening program, since principle 7 (◘ Table 16.1) is not met and therefore principles 4 and 5 are also in doubt. There is therefore an urgent need to find a new test for oral cancer screening that will detect only lesions that are most likely to progress to cancer. At the present time, no biomarkers have been shown to accurately predict which oral potentially malignant lesions may progress to cancer, and none have been found suitable for a screening test [32,33,34].
There are many recent studies that have described a number of new tests or adjunctive techniques designed to assist clinical diagnosis, including vital staining (toluidine blue), light-based techniques (usually using fluorescence), mouth self-examination, and some cytological methods. However, most have been used as diagnostic aids in secondary care environments, but none have been evaluated for use in subjects who are otherwise asymptomatic or evaluated in the context of oral cancer screening [35]. A Cochrane systematic review found that none of the adjunctive tests were suitable for use as a screening test or can be used as a substitute for the current diagnostic standard of a biopsy and histological examination [36]. Lingen et al. [37] have updated this Cochrane review on behalf of the American Dental Association. They undertook a detailed review and meta-analysis of 46 studies that evaluated the diagnostic test accuracy of more than ten different adjunctive methods for use in primary care settings. They found that, with the exception of cytological studies, adjunctive tests showed pooled sensitivities of 0.00 to 0.90 and specificities of 0.31 to 0.76. The authors concluded that the overall low specificities and high rate of false positives raised doubts about the potential benefits of adjunctive tests. They did however suggest that cytology had potential as a test for both innocuous and suspicious lesions with pooled sensitivities of 0.95 (CI: 0.86–0.99) and 0.90 (CI: 0.86–0.98), respectively. Corresponding specificities were 0.90 (CI: 0.79–0.97) and 0.94 (CI: 0.88–0.99). However, the quality of the evidence was low, and it should be noted that none of the methods were evaluated as potential screening tests for use on otherwise symptomless individuals. These date show that none of these adjuncts have been found to have adequate diagnostic test accuracy for the routine evaluation of oral potentially malignant lesions, and they have not been recommended for use in routine clinical practice [38] or for screening [39].
At the present time therefore, although it is possible to accurately detect oral lesions, the criteria for a positive oral examination are not suitable to detect those lesions with the highest probability of progressing to malignancy. A major research priority is to further understand the natural history of the progression of oral lesions to cancer and to find biomarkers or clinical tests that can be used to identify truly premalignant oral lesions. A further challenge will be to find a test that can be applied to apparently clinically normal subjects for the detection of potentially malignant lesions or occult oral cancers.
16.3.4 Screening Programs for Oral Cancer
Screening programs for oral cancer have been the subject of a number of research projects, but only two countries, Taiwan and Cuba, have implemented any sort of formally organized oral cancer control programs. Cuba recognizes that oral cancer screening may not reduce mortality [40] but nevertheless have introduced a national oral cancer case-finding program [41]. The strategy involves an annual oral examination and teaching oral self-examination for the whole population and opportunistic case-finding for high-risk individuals over 35 years [40]. Originally, the program recruited all individuals over age 15 years, but there have been no published evaluations since 1997 [41, 42]. Between 1982 and 1990, over ten million people were examined and 30,478 (0.3%) were referred with an oral abnormality. Only 27% (8259) complied, but the yield of lesions included 481 squamous cell carcinomas and 127 other oral malignancies. There were also 3220 oral potentially malignant lesions including 2367 leukoplakias. The only reported outcome measure was a stage shift (◘ Table 16.5) with the proportion of lesions detected at stage I increasing from 22.8% in 1982 to 48.2% in 1988 [41]. Although this suggests a successful program, the improvement in stage was only analyzed in the cases detected from within the program, and not for the population as a whole. Others have noted [42] that the program only actually identified 16% of the incident oral cancers over the period and that there was no overall change in mortality or morbidity in Cuba. No data has been published since 1997, and it is not possible to assess the ongoing status of the program [40].
Taiwan has a very high prevalence of oral potentially malignant disorders, in particular oral submucous fibrosis, as a result of the common habit of chewing betel quid (areca nut) [43]. Over a 3-year period, 1999–2001, a large project evaluated a multiple disease screening program in Keelung County, Taiwan, which included an oral examination for oral submucous fibrosis or leukoplakia [44]. About 10,500 subjects who used betel quid , tobacco, or alcohol received an oral examination, and in 285 (2.7%), a lesion was detected. After referral, a total of 116 lesions (1.08%) were diagnosed, including 2 cases of oral cancer, 23 oral submucous fibrosis, and 86 leukoplakias. Following this trial, national screening programs for cervical, breast, oral, and colorectal cancer were introduced and are ongoing [45]. A fuller evaluation of the oral cancer screening outcomes was reported in 2016 and will be discussed in the following section.
16.3.5 Evaluation of Oral Cancer Screening Programs
The ideal test of the effectiveness of a screening program is a randomized controlled trial with a primary outcome measure of reduced mortality . In a Cochrane systematic review, Brocklehurst et al. [46] found 30 potentially eligible studies investigating oral cancer screening, but only one of these was a controlled trial that met the inclusion criteria. All other studies were uncontrolled, were observational only, or were reviews. Thus, to date, there has only ever been one properly conducted randomized controlled trial to evaluate the effectiveness of an oral cancer screening program.
This oral cancer screening trial was undertaken in Kerala, India, and has been reported in a series of papers [47,48,49,50,51]. From 1994 to 2009, the investigators carried out four rounds of screening in a community-based trial where 13 municipalities were randomized to give an intervention (screened) population and a control (not screened) population, each of almost 100,000 subjects. Healthy residents 35 years of age or over were examined by trained nonmedical university graduates who carried out a visual oral examination of each subject. The criteria for a positive screen were the presence of a potentially malignant disorder (including white/red lesions, oral submucous fibrosis, and lichen planus) or of an ulcer suspected to be malignant.
After three rounds of screening, it was reported that 87,655 (91%) subjects in the intervention group were screened at least once and 6.55% were found to be positive [48]. Overall 205 oral cancers were diagnosed in the intervention group (131 screen-detected, 59 interval cancers, and 15 nonparticipants), compared to 158 in the control group. They found that 5-year survival was significantly different between the two groups with 50% in the intervention arm and 34% in the control arm. They also found evidence of a significant stage shift, with 42% of cases in the intervention arm diagnosed early (in stages I and II), compared to only 23% in the control arm. However, there was no significant reduction in mortality in the population as a whole. Deaths from oral cancer were 37.6% in the intervention arm (77 individuals) and 55% (87 individuals) in the control arm, but this difference was not significant. The authors further analyzed their data to determine the outcome if only high-risk groups had been screened. They found a significant reduction in mortality , from 42.9% to 24.6%, in males who used tobacco and/or alcohol . Among females there was no significant reduction in mortality .
After four rounds of screening, completed in 2009 [50], there was a significant improvement in 5- and 10-year survival rates and in early detection (stage shift). However, there was still no significant reduction in death rates or reduced mortality in the population. This suggests that the improvements in survival were due to lead-time bias (see ► Section 16.2.2) and that the overall screening program had not been effective. However, the authors did find a significant reduction in mortality among those subjects who had attended all four cycles of screening. The death rate in the intervention arm was 17.1 per 100,000 and reduced to 3.0 per 100,000 in the control arm. In the high-risk group, the corresponding rates were 39 per 100,000 and 7.1 per 100,000. The authors suggested that targeted or opportunistic screening of high-risk groups may be effective. However, the fact that only 19,288 subjects (20%) completed all four cycles of the program means that the effect on oral cancer incidence or mortality on the population as a whole was slight.
The authors of the Kerala study concluded that opportunistic screening of high-risk groups should be considered as an effective intervention to reduce incidence and mortality of oral cancer [50, 51]. The Cochrane review [46] acknowledged the significant findings of the Kerala study but, on critical examination, found a number of methodological weaknesses that reduced the validity of the findings. They concluded that there was insufficient evidence to recommend population-based screening programs for oral cancer.
Alternatives to a full randomized controlled trial include retrospective analyses or evaluation of demonstration studies (► Section 16.2.3). Following the implementation of screening in Taiwan (► Section 16.3.4 [44, 45]), the program was evaluated by comparing the outcomes in the population cohort who attended for screening with those who did not attend [52]. Between 2004 and 2009, a total of more than 4.2 million individuals aged 18 years or over, who were smokers and/or betel quid users, were invited for a biennial oral examination by a trained dentist or physician. Fifty-five percent (2,334,299 individuals) attended for screening, and 18,116 (0.8%) were found to have a positive lesion including 4110 oral cancers at the first screen. The main outcome measures relevant to a screening program were yield of lesions, incidence of invasive cancers, stage shift, and mortality . In the screened group (“attendees”; n = 2,334,299), the yield of lesions was directly observed, but other parameters, including incidence of interval cancers, stage at presentation, and survival, were obtained from the national registries of cancer or deaths, with a median follow-up period of 4.5 years. The non-screened group comprised those individuals who had not accepted the invitation to be examined (“non-attendees”; n = 1,900,094). However, because information was not available to confirm the high-risk habits of this group, the expected incidence of disease, stage of presentation, and mortality rates were calculated from cancer registry data, based on an estimate that 90% of oral cancers arose in those who smoked or chewed betel quid . The effectiveness of the program was then estimated using the observed values in the screened group and the expected values of the non-screened group. Overall, the data showed good evidence that the screening program was effective. The total number of oral cancers in the screened group, including cases detected at subsequent screens and interval cases, was 8033 with an annual incidence of 133.4 per 100,000. This was significantly lower than the incidence in the non-screened group (190.9 per 100,000). There was evidence of a significant stage shift, with 46.5% of cases presenting in stages I and II in the screened group compared to 39.6% in the non-screened group. The study also showed a 26% reduction in mortality in the screened group (RR vs. non-screened: 0.74; CI, 0.72–0.77).
The results of this Taiwan study support the findings from the Kerala project and provide further evidence that screening may reduce mortality from oral cancer among high-risk groups. The study also presents important new data showing that the screened population had a reduced incidence of invasive oral cancers after only 5 years. This suggests that the early detection and treatment of potentially malignant lesions may prevent malignant transformation . The potentially malignant lesions included as positive were leukoplakia, erythroleukoplakia, erythroplakia, oral submucous fibrosis, and verrucous hyperplasia, but the authors do not indicate how the lesions were treated.
Neither study was able to show that a national screening program is able to reduce mortally from oral cancer in the population as a whole. Further RCTs may be needed to provide more robust evidence to support oral cancer screening, but as can be seen from these studies and from the previous discussion (► Section 16.2.3), this is a major undertaking requiring significant resource and large numbers of subjects followed over a long period. Few funding bodies or governments are likely to support a project of the standard and scale of the Kerala study .
16.4 Cost-Effectiveness of Cancer Screening
16.4.1 Principles of Cost-Effectiveness Analysis and Thresholds
When considering the implementation of a screening program, a major consideration (principle 9 in ◘ Table 16.1) is that it should be cost-effective. The most common method used to determine the value of a new healthcare intervention is to undertake a cost-effectiveness analysis. This assesses if the health benefits obtained from the intervention are sufficient to justify the costs. When evaluating a cancer screening program, the benefits are measured in the number of lives saved, but in order to be able to give a reproducible and comparable measure, the lives saved are expressed in the number of years adjusted using a measure of perceived quality of life (health-state utilities [53]) and are expressed as quality-adjusted life years (QALYs) [54]. In a screened population, the total number of additional QALYs gained as a result of early detection can be compared to the number of QALYs in the non-screened population and can be costed. The resulting measure is called the incremental cost-effectiveness ratio (ICER) and represents the additional cost for each QALY saved in the population. There is no expectation that the ICER will be zero or negative, but it is expected that the cost of saving lives through screening will be within the resources available and will have a beneficial effect on the health system as a whole. Thus, a government may set a cost-effectiveness threshold on what they (or the taxpayer) are prepared to spend on a new healthcare intervention [55]. This threshold is likely to be lower in low- and middle-income countries than in high-income countries [55]. In the United Kingdom and the United States, the thresholds are set at about £20,000 to £30,000 and $50,000, respectively [56, 57].
16.4.2 Cost-Effectiveness of Oral Cancer Screening Programs
In the Kerala screening study, the research group undertook a detailed analysis of the costs of the program and was able to calculate the ICER [51]. They showed that the screening program produced a benefit of 270 life years saved per 100,000 for the whole population and 1438 life years for the high-risk groups. The incremental cost per life-year saved was US$835 for the whole screened population, but it decreased to US$156 for the high-risk group only. This cost is within the range considered acceptable in a low-middle-income country and suggests that opportunistic screening of high-risk groups may be feasible and cost-effective [50, 51]. However, it must be noted that there has not been an RCT or formal cost-effectiveness analysis in any high-income country or low-prevalence population.
An alternative to a fully costed clinical trial is to simulate a screening program using computer modeling. Speight et al. [58] used simulation modeling to evaluate the outcome of screening on a population of 100,000 people over the age of 40 years. The model was a decision tree analysis informed by published NHS costs and using data on disease prevalence, malignant transformation, and test performance from previously published research. The modeling showed that whole-population screening was unlikely to be cost-effective but that targeting high-risk groups for opportunistic screening in medical or dental primary care may be cost-effective. They found that the ICER for an opportunistic high-risk screen was £22,850 by primary care dentist and £23,728 by a general medical practitioner. These costs assumed that detection and treatment of potentially malignant lesions would have no effect on disease progression. If the model assumed malignant transformation was reduced by 10% or 20%, the ICERs for opportunistic screening by a dentist were reduced to £18,919 and £15,790, respectively. These costs are below the cost-effectiveness threshold set by the United Kingdom and the United States [56, 57] and suggest that opportunistic high-risk screening in primary dental or medical care settings may be a cost-effective strategy.
However, the simulation model assumed that detection of potentially malignant lesions may prevent further disease progression and reduce the incidence of invasive cancers. In their literature reviews, Speight et al. [58] found little evidence that this is the case and undertook a value of information analysis, which estimates the value of future research that could be undertaken to reduce the uncertainty in the data. The analysis showed that the most valuable research should be directed at studies of the natural history of the oral cancer – in particular to determine the exact malignant transformation rates of individual potentially malignant disorders and the rate of disease progression of established lesions of oral cancer. Further research was also needed on cancer referral pathways from primary to secondary care and the identification of sources of delay and how to prevent them.
16.4.3 Opportunistic Screening for Oral Cancer
The evidence discussed in ► Sections 16.3.5 and 16.4.2 suggests that opportunistic screening of the oral cavity by visual examination in high-risk groups may be cost-effective and may provide an effective strategy for oral cancer screening. However, there are few studies on the ideal environment for undertaking opportunistic screening. In their simulation modeling, Speight et al. [58] suggested that patients attending either a medical or dental practitioner could be effectively screened, but these estimates were based on attendance rates and disease prevalence. They did not account for the additional training that would be necessary to enable medical practitioners to examine the oral cavity. Since dentists are already trained, it seems intuitive that opportunistic screening in dental primary care, when a patient attends for a routine “checkup,” would be the most effective strategy. However, there is evidence that those thought to be at the highest risk of oral cancer, especially males over 40 who smoke and/or drink, are the least likely to attend for regular dental checkups [59]. Yusof et al. [60] analyzed patterns of attendance for regular dental checkups over a 10-year period and found that males over 40 years, who belonged to lower socioeconomic groups, and who were heavy smokers were less likely to attend than females, younger people, nonsmokers, and those from a higher socioeconomic class. These studies concluded that opportunistic screening is unlikely to be an effective strategy for early detection or prevention of oral cancer. Further research is needed to more fully understand the patient pathway to secondary care and to establish the frequency and nature of contacts that patients with oral cancer have had with a full range of healthcare professionals. This may identify more ideal sites for opportunistic screening by a wider range of healthcare workers. Integration of oral cancer screening with general health screening or with other cancer screening programs was found to be effective in Taiwan [44, 45, 52], but when trialed in a Japanese population, it was associated with low compliance among the elderly and a low yield of lesions, and regular smokers were less likely to attend for rescreening [26, 61, 62]. The Japanese screening program did however find that annual screening could detect new oral potentially malignant lesions in the screened population. Poor attendance for screening or regular checkups may also be related to a lack of awareness of the signs of oral cancer and its causes, meaning that individuals may not be aware that they are at high risk [63] and may not appreciate the importance of regular attendance. Research on attendance patterns may be helpful, but more health education on risk factors and the importance of oral health is needed. There is good evidence that health promotion aimed at smoking cessation may be effective in reducing the incidence of oral cancer [64] but also that regular dental attendance is associated with diagnosis of oral cancer at an earlier stage [65].
16.5 Conclusion and Future Perspectives
Overall, it appears clear that oral cancer is a significant health problem and that screening for oral cancer and for potentially malignant lesions is feasible. However, there are considerable barriers to the implementation of any sort of formal screening program. Although principle 1 suggested by Wilson and Jungner (◘ Table 16.1) [3] is met, the evidence for the other key principles is lacking or inconclusive. The main barriers and potential solutions and research priorities are summarized in ◘ Table 16.7.
16.5.1 The Natural History of Oral Cancer and Precancer
Although there is good evidence that an oral examination can detect potentially malignant lesions with a sensitivity and specificity sufficient to justify it as a screening test, the currently used criteria for a positive test are not sufficiently specific to identify only those lesions that have the highest probability of progression to cancer, since only about 5% of the most commonly detected lesions (leukoplakia) are expected to transform [30,31,32]. Even for those that will progress, studies have shown that the main source of uncertainty in determining the outcomes of an oral cancer screening program was a lack of knowledge of malignant transformation rates and disease progression [58].Currently, there are no biomarkers or accurate indicators of which lesions are most likely to progress (► Section 16.3.3). Further research is needed on the natural history of oral cancer, the development of biomarkers, and the feasibility of commercially available clinical tests and adjunctive aids, all of which will help to inform the development of more accurate tests.
16.5.2 The Management of Screen-Detected Lesions
A further consideration is principle 2 (◘ Table 16.1). Although there are well established protocols for the management of oral cancer, the treatment for potentially malignant disorders remains controversial. Holmstrup et al. [66, 67] showed that surgical removal of potentially malignant lesions did not prevent the development of oral cancer and suggested that this was because the clinically detectable lesion only represents one small part of a whole field of altered oral mucosa, any area of which could progress to malignancy. A systematic review of interventions for treating leukoplakia [68] found few randomized controlled trials and a lack of evidence that any treatment options, including surgical intervention and preventive chemotherapy, are effective in reducing progression to oral cancer. A further systematic review on the surgical management of lesions shown to be dysplastic found evidence that surgery reduces malignant transformation rates [69], but the authors could not find any properly conducted trials. Holmstrup [70, 71] has highlighted this lack of evidence for the effectiveness of surgery for the treatment of oral precancer and has drawn attention to the urgent need for randomized controlled trials with long-term follow-up to establish optimal treatment protocols.
16.5.3 Identification of High-Risk Groups and the Potential of mHealth
It also remains to be determined who should be screened and where. The evidence discussed in ► Section 16.4.3 suggests that opportunistic screening of high-risk groups may be cost-effective and may provide an effective strategy for oral cancer screening, but it is not certain that opportunistic screening would be effective in a primary care setting. To make opportunistic screening more effective, methods are needed for the easy identification of high-risk groups so that dentists can appropriately target those most likely to have lesions. Apart from issues of health education [63, 64], this could be done using a simple patient checklist that enquires about tobacco and alcohol habits [72, 73]. Lim et al. [73] conducted a demonstration project of opportunistic screening in a group of selected general dental practices and used a patient checklist, which showed a strong correlation between self-reported habits of tobacco and alcohol use and the presence of oral potentially malignant lesions.
Another effective way of identifying high-risk individuals may be to use artificial intelligence (AI) systems. These have been developed to support oral cancer screening and have been shown to be effective in identifying those at the highest risk of having lesions [74, 75]. An advantage of using AI is that it can be embedded into a standard computerized system for medical history taking and internal algorithms can accurately flag patients at different levels of risk [75]. Such a system could also be used in any setting (e.g., in a pharmacy or any waiting area) or be made available as a smartphone app, allowing patients to anonymously self-identify as high risk and seek advice. The use of mobile phones (“mHealth”) is providing many new opportunities in the delivery of healthcare, especially in low- and middle-income countries and “last-mile” rural communities [76]. It is estimated that 97% of the world’s population live within reach of a mobile phone signal and mobile phones are increasingly being used to support cancer control programs by improving communications, enhancing attendance and compliance, and facilitating data collection and decision support [76].
Birur et al. [77] have described a mobile phone-based oral cancer detection program using a hub and node model based on Bangalore, India. The mHealth system enabled remote dentists and frontline healthcare workers to input demographic and risk factor data and clinical photographs into a mobile phone app, linked directly to oral cancer specialist at a cancer center. Built-in algorithms identified high-risk patients for targeted examinations and follow-up, and any lesions detected were photographed and uploaded for interpretation by the center specialists. If a lesion met the criteria for a potentially malignant or malignant lesion, the specialist sent instructions for referral and follow-up. Two thousand patients were targeted for examination by healthcare workers, and 1440 were examined opportunistically by dentists, with a yield of 130 (6.5%) and 106 (7.36%) lesions in each group, respectively. The remote diagnosis was confirmed by the oral cancer specialist in 45% of cases photographed by the healthcare workers and in 100% of cases photographed by the dentists. However, of a total of 129 patients referred for biopsy and histological evaluation, only 62 attended: 1 (4%) from the targeted population and 61 (57%) referred by the dentists. Of the 61 lesions referred by the dentists, there was a high rate of true positives, with 49 shown to be dysplastic and 5 proving to be squamous cell carcinomas. A similar study in Malaysia [78] evaluated mobile phone imaging for early detection of oral cancer in 16 individuals. Lesions and normal areas of mucosa were photographed, and diagnoses on the images were compared to a gold-standard clinical examination by a specialist. Sensitivity exceeded 70% and specificity was 100%. Together, these studies show the potential of mHealth systems to support cancer screening and to improve the efficiency of early detection of oral potentially malignant or malignant lesions.
16.6 Conclusion
This chapter reviews the principles of cancer screening and discusses the currently available evidence for the effectiveness of oral cancer screening programs. It is noted that no oral cancer screening program has yet been shown to be effective and no country has formally introduced a national program. Much work, however, has been done and there is evidence that screening is feasible. More research is needed to refine screening tests and to determine the optimal screening environment and ways to target appropriate population groups.
References
World Health Organization. National cancer control programmes: policies and managerial guidelines. 2nd ed. WHO; 2002. www.who.int/cancer/media/en/408.pdf.
Petersen PE. Oral cancer prevention and control – the approach of the World Health Organization. Oral Oncol. 2009;45:454–60.
Wilson JMG, Jungner G. Principles and practice of screening for disease. Geneva: WHO; 1968.
UK National Screening Committee. Criteria for appraising the viability, effectiveness and appropriateness of a screening programme. London, UK: National Screening Committee, 2003. Updated 2015: https://www.gov.uk/government/publications/evidence-review-criteria-national-screening-programmes.
Oral cancer Screening. National Cancer Institute: U.S. National Institutes of Health. http://www.cancer.gov/cancertopics/pdq/screening/oral/healthprofessional.
U.S. Preventive Services Task Force: Screening for Oral Cancer: Recommendation Statement. Rockville: U.S. Preventive Services Task Force, 2004. http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/oral-cancer-screening1.
Speight PM, Epstein J, Kujan O, Lingen MW, Nagao T, Ranganathan K, Vargas P. Screening for oral cancer – a perspective from the Global Oral Cancer Forum. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;123:680–7.
Parkin DM, Moss SM. Lung cancer screening: improved survival but no reduction in deaths–the role of “overdiagnosis”. Cancer. 2000;89(11 Suppl):2369–76.
Chamberlain J, Moss S, editors. Evaluation of cancer screening. London: Springer; 1996.
Vermeer NC, Snijders HS, Holman FA, Liefers GJ, Bastiaannet E, van de Velde CJ, Peeters KC. Colorectal cancer screening: systematic review of screen-related morbidity and mortality. Cancer Treat Rev. 2017;54:87–98.
de Koning HJ, Gulati R, Moss SM, Hugosson J, Pinsky PF, Berg CD, Auvinen A, Andriole GL, Roobol MJ, Crawford ED, Nelen V, Kwiatkowski M, Zappa M, Luján M, Villers A, de Carvalho TM, Feuer EJ, Tsodikov A, Mariotto AB, Heijnsdijk EAM, Etzioni R. The efficacy of prostate-specific antigen screening: impact of key components in the ERSPC and PLCO trials. Cancer. 2018;124:1197–206.
Chamberlain J. Evaluation of screening for cancer. Community Dent Health. 1993;10(Suppl 1):5–11.
Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45:309–16.
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Seoane J, Alvarez-Novoa P, Gomez I, et al. Early oral cancer diagnosis: The Aarhus statement perspective. A systematic review and meta-analysis. Head Neck. 2016;38(Suppl 1):E2182–9.
Rogers SN, Brown JS, Woolgar JA, et al. Survival following primary surgery for oral cancer. Oral Oncol. 2009;45:201–11.
Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36(10):575–80.
Chang IH, Jiang RS, Wong YK, Wu SH, Chen FJ, Liu SA. Visual screening of oral cavity cancer in a male population: experience from a medical center. J Chin Med Assoc. 2011;74:561–6.
Downer MC, Evans AW, Hughes Hallett CM, Jullien JA, Speight PM, Zakrzewska JM. Evaluation of screening for oral cancer and precancer in a company headquarters. Community Dent Oral Epidemiol. 1995;23:84–8.
Ikeda N, Downer MC, Ishii T, Fukano H, Nagao T, Inoue K. Annual screening for oral cancer and precancer by invitation to 60 year-old residents of a city in Japan. Community Dent Health. 1995;12:133–7.
Jullien JA, Downer MC, Zakrzewska JM, Speight PM. Evaluation of a screening test for the early detection of oral cancer and precancer. Community Dent Health. 1995;12:3–7.
Mathew B, Sankaranarayanan R, Sunilkumar KB, Kuruvila B, Pisani P, Nair MK. Reproducibility and validity of oral visual inspection by trained health workers in the detection of oral precancer and cancer. Brit J Cancer. 1997;76:390–4.
Mehta FS, Gupta PC, Bhonsle RB, et al. Detection of oral cancer using basic health workers in an area of high oral cancer incidence in India. Cancer Detect Prev. 1986;9:219–25.
Warnakulasuriya S, Pindborg JJ. Reliability of oral precancer screening by primary health care workers in Sri Lanka. Community Dent Health. 1990;7:73–9.
Monteiro LS, Salazar F, Pacheco JJ, Martins M, Warnakulasuriya S. Outcomes of invitational and opportunistic oral cancer screening initiatives in Oporto, Portugal. J Oral Pathol Med. 2015 Feb;44:145–52.
Nagao T, Ikeda N, Fukano H, Miyazaki H, Yano M, Warnakulasuriya S. Outcome following a population screening programme for oral cancer and precancer in Japan. Oral Oncol. 2000 Jul;36:340–6.
Walsh T, Liu JL, Brocklehurst P, Glenny AM, Lingen M, Kerr AR, et al. Clinical assessment to screen for the detection of oral cavity cancer and potentially malignant disorders in apparently healthy adults. Cochrane Database Syst Rev. 2013;11:CD010173.
Downer MC, Moles DR, Palmer S, Speight PM. A systematic review of test performance in screening for oral cancer and precancer. Oral Oncol. 2004;40:264–73.
Petti S. Pooled estimate of world leukoplakia prevalence: a systematic review. Oral Oncol. 2003;39:770–80.
Napier SS, Speight PM. Natural history of potentially malignant oral lesions and conditions: an overview of the literature. J Oral Pathol Med. 2008;37:1–10.
Warnakulasuriya S, Ariyawardana A. Malignant transformation of oral leukoplakia: a systematic review of observational studies. J Oral Pathol Med. 2016;45:155–66.
Speight PM, Khurram SA, Kujan O. Oral potentially malignant disorders: risk of progression to malignancy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;. pii: S2212-4403(17)31248-8.
Warnakulasuriya S, Reibel J, Bouquot J, Dabelsteen E. Oral epithelial dysplasia classification systems: predictive value, utility, weaknesses and scope for improvement. J Oral Pathol Med. 2008;3:127–33.
Warnakulasuriya S. Lack of molecular markers to predict malignant potential of oral precancer. J Pathol. 2000;190:407–9.
Lingen MW, Kalmar JR, Karrison T, Speight PM. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008;44:10–22.
Macey R, Walsh T, Brocklehurst P, Kerr AR, Liu JL, Lingen MW, et al. Diagnostic tests for oral cancer and potentially malignant disorders in patients presenting with clinically evident lesions. Cochrane Database Syst Rev. 2015;5:CD010276.
Lingen MW, Tampi MP, Urquhart O, Abt E, Agrawal N, Chaturvedi AK, Cohen E, D'Souza G, Gurenlian J, Kalmar JR, Kerr AR, Lambert PM, Patton LL, Sollecito TP, Truelove E, Banfield L, Carrasco-Labra A. Adjuncts for the evaluation of potentially malignant disorders in the oral cavity: diagnostic test accuracy systematic review and meta-analysis-a report of the American Dental Association. J Am Dent Assoc. 2017;148:797–813.
Lingen MW, Abt E, Agrawal N, Chaturvedi AK, Cohen E, D'Souza G, Gurenlian J, Kalmar JR, Kerr AR, Lambert PM, Patton LL, Sollecito TP, Truelove E, Tampi MP, Urquhart O, Banfield L, Carrasco-Labra A. Evidence-based clinical practice guideline for the evaluation of potentially malignant disorders in the oral cavity: a report of the American Dental Association. J Am Dent Assoc. 2017;148:712–27.
Rethman MP, Carpenter W, Cohen EE, Epstein J, Evans CA, Flaitz CM, et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc. 2010;141:509–20.
González RS. Cancer screening: global debates and Cuban experience. MEDICC Rev. 2014;16:73–7.
Santana JC, Delgado L, Miranda J, Sánchez M. Oral Cancer Case Finding Program (OCCFP). Oral Oncol. 1997;33:10–2.
Frenández Garrote L, Sankaranarayanan R, Lence Anta JJ, Rodriguez Salvá A, Maxwell Parkin D. An evaluation of the oral cancer control program in Cuba. Epidemiology. 1995;6:428–31.
Yen AM, Chen SC, Chen TH. Dose-response relationships of oral habits associated with the risk of oral pre-malignant lesions among men who chew betel quid. Oral Oncol. 2007;43:634–8.
Chen TH, Chiu YH, Luh DL, et al. Community-based multiple screening model: design, implementation, and analysis of 42,387 participants. Cancer. 2004;100:1734–43.
Taiwan Breast cancer, Oral cancer and Colorectal cancer Screening Programs. Taiwan Ministry of Health and Welfare. https://www.hpa.gov.tw/EngPages/Detail.aspx?nodeid=1051&pid=5957. Accessed May 2018.
Brocklehurst P, Kujan O, O’Malley LA, Ogden G, Shepherd S, Glenny AM. Screening programmes for the early detection and prevention of oral cancer. Cochrane Database Syst Rev. 2013;11:CD004150.
Sankaranarayanan R, Mathew B, Jacob BJ, Thomas G, Somanathan T, Pisani P, Pandey M, Ramadas K, Najeeb K, Abraham E. Early findings from a community-based, cluster-randomized, controlled oral cancer screening trial in Kerala, India. The Trivandrum Oral Cancer Screening Study Group. Cancer. 2000;88:664–73.
Ramadas K, Sankaranarayanan R, Jacob BJ, Thomas G, Somanathan T, Mahe C, Pandey M, Abraham E, Najeeb S, Mathew B, Parkin DM, Nair MK. Interim results from a cluster randomized controlled oral cancer screening trial in Kerala, India. Oral Oncol. 2003;39:580–8.
Sankaranarayanan R, Ramadas K, Thomas G, Muwonge R, Thara S, Mathew B, Rajan B, Trivandrum Oral Cancer Screening Study Group. Effect of screening on oral cancer mortality in Kerala, India: a cluster-randomised controlled trial. Lancet. 2005;365:1927–33.
Sankaranarayanan R, Ramadas K, Thara S, Muwonge R, Thomas G, Anju G, Mathew B. Long term effect of visual screening on oral cancer incidence and mortality in a randomized trial in Kerala, India. Oral Oncol. 2013;49:314–21.
Subramanian S, Sankaranarayanan R, Bapat B, Somanathan T, Thomas G, Mathew B, Vinoda J, Ramadas K. Cost-effectiveness of oral cancer screening: results from a cluster randomized controlled trial in India. Bull World Health Organ. 2009;87:200–6.
Chuang SL, Su WW, Chen SL, Yen AM, Wang CP, Fann JC, Chiu SY, Lee YC, Chiu HM, Chang DC, Jou YY, Wu CY, Chen HH, Chen MK, Chiou ST. Population-based screening program for reducing oral cancer mortality in 2,334,299 Taiwanese cigarette smokers and/or betel quid chewers. Cancer. 2017;123:1597–609.
Downer MC, Jullien JA, Speight PM. An interim determination of health gain from oral cancer and precancer screening: 1. Obtaining health state utilities. Community Dent Health. 1997;14:139–42.
Downer MC, Jullien JA, Speight PM. An interim determination of health gain from oral cancer and precancer screening: 2. Developing a model of population screening. Community Dent Health. 1997;14:227–32.
Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health. 2016;19:929–35.
National Institute for Health and Care Excellence (NICE). Carrying NICE over the threshold. https://www.nice.org.uk/news/blog/carrying-nice-over-the-threshold. Accessed May 2018.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796–7.
Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, Augustovski F. The cost-effectiveness of screening for oral cancer in primary care. Health Technol Assess. 2006;10:1–144.
Netuveli G, Sheiham A, Watt RG. Does the ‘inverse screening law’ apply to oral cancer screening and regular dental check-ups? J Med Screen. 2006;13:47–50.
Yusof ZY, Netuveli G, Ramli AS, Sheiham A. Is opportunistic oral cancer screening by dentists feasible? An analysis of the patterns of dental attendance of a nationally representative sample over 10 years. Oral Health Prev Dent. 2006;4:165–71.
Nagao T, Warnakulasuriya S, Ikeda N, Fukano H, Fujiwara K, Miyazaki H. Oral cancer screening as an integral part of general health screening in Tokoname City, Japan. J Med Screen. 2000;7:203–8.
Nagao T, Warnakulasuriya S. Annual screening for oral cancer detection. Cancer Detect Prev. 2003;27:333–7.
Warnakulasuriya KA, Harris CK, Scarrott DM, Watt R, Gelbier S, Peters TJ, Johnson NW. An alarming lack of public awareness towards oral cancer. Br Dent J. 1999;187:319–22.
van der Waal I. Are we able to reduce the mortality and morbidity of oral cancer; some considerations. Med Oral Patol Oral Cir Bucal. 2013;18:e33–7.
Langevin SM, Michaud DS, Eliot M, Peters ES, McClean MD, Kelsey KT. Regular dental visits are associated with earlier stage at diagnosis for oral and pharyngeal cancer. Cancer Causes Control. 2012;23:1821–9.
Holmstrup P, Vedtofte P, Reibel J, Stoltze K. Long-term treatment outcome of oral premalignant lesions. Oral Oncol. 2006;42:461–74.
Holmstrup P, Vedtofte P, Reibel J, Stoltze K. Oral premalignant lesions: is a biopsy reliable? J Oral Pathol Med. 2007;36:262–6.
Lodi G, Franchini R, Warnakulasuriya S, et al. Interventions for treating oral leukoplakia to prevent oral cancer. Cochrane Database Syst Rev. 2016;7:CD001829.
Mehanna HM, Rattay T, Smith J, McConkey CC. Treatment and follow-up of oral dysplasia – a systematic review and meta-analysis. Head Neck. 2009;31:1600–9.
Holmstrup P. Can we prevent malignancy by treating premalignant lesions? Oral Oncol. 2009;45:549–50.
Holmstrup P, Dabelsteen E. Oral leukoplakia-to treat or not to treat. Oral Dis. 2016;22:494–7.
McGurk M, Scott SE. The reality of identifying early oral cancer in the general dental practice. Br Dent J. 2010;208:347–51.
Lim K, Moles DR, Downer MC, Speight PM. Opportunistic screening for oral cancer and precancer in general dental practice: results of a demonstration study. Br Dent J. 2003;194:497–502.
Speight PM, Elliott AE, Jullien JA, Downer MC, Zakzrewska JM. The use of artificial intelligence to identify people at risk of oral cancer and precancer. Br Dent J. 1995;179:382–7.
Speight PM, Hammond P. The use of machine learning in screening for oral cancer. In: Naguib RNG, Sherbet GV, editors. Artificial neural networks in cancer diagnosis, prognosis, and patient management. Boca Raton: CRC Press; 2001.
Bhatt S, Evans J. Mobile healthcare for cancer care and control in low- and middle-income countries. In: Finkel ML, editor. Cancer screening in the developing world. New England: Dartmouth College Press; 2018.
Birur PN, Sunny SP, Jena S, Kandasarma U, Raghavan S, Ramaswamy B, Shanmugam SP, Patrick S, Kuriakose R, Mallaiah J, Suresh A, Chigurupati R, Desai R, Kuriakose MA. Mobile health application for remote oral cancer surveillance. J Am Dent Assoc. 2015;146:886–94.
Haron N, Zain RB, Nabillah WM, Saleh A, Kallarakkal TG, Ramanathan A, Sinon SH, Razak IA, Cheong SC. Mobile phone imaging in low resource settings for early detection of oral cancer and concordance with clinical oral examination. Telemed J E Health. 2017;23:192–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Speight, P.M. (2020). Screening for Oral Cancer. In: Warnakulasuriya, S., Greenspan, J. (eds) Textbook of Oral Cancer. Textbooks in Contemporary Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-030-32316-5_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-32316-5_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32315-8
Online ISBN: 978-3-030-32316-5
eBook Packages: MedicineMedicine (R0)