Abstract
Diagnostic imaging, including magnetic resonance (MR) imaging, plays an important role in diagnosing pancreatic disease in the pediatric population. MR cholangiopancreatography (MRCP) is a valuable noninvasive method for evaluating the pancreas and pancreaticobiliary tree. While MR imaging remains challenging in children, in recent years, novel pulse sequences have greatly improved image quality by increasing the speed of image acquisition and decreasing/compensating for motion and respiratory artifacts.
This chapter reviews the up-to-date and fundamental basics of pediatric pancreatic MR imaging protocols. Familiarity with the normal development and appearance of the pancreas allows radiologists to provide accurate and timely diagnoses. Therefore, this chapter discusses pancreatic embryology and common and less common congenital anomalies, including pancreas divisum, annular pancreas, agenesis and hypoplasia of the pancreas, and pancreatic ectopia. Next, congenital disorders which affect the pancreas are reviewed, including von Hippel-Lindau disease syndrome, cystic fibrosis, and Shwachman-Diamond syndrome. In these disorders, the pancreas undergoes cystic or fatty degeneration.
Pancreatitis is the most common pancreatic disease in children and may cause significant morbidity and mortality. MR imaging may play an important role in diagnosis and prognosis, as nearly a quarter of children eventually develop severe complications. The imaging features of acute pancreatitis, its complications, and chronic pancreatitis are described in this chapter.
Pancreatic neoplasms are fortunately uncommon in children. Even the most common pancreatic tumor, pancreaticoblastoma, is quite rare. The typical imaging and demographic features of pancreaticoblastoma and other pediatric pancreatic tumors are discussed, including solid pseudopapillary tumor, islet cell tumors, and lymphoma.
Lastly, this chapter also briefly discusses pancreatic traumatic injury, which may occur with seatbelt-type injuries or non-accidental trauma.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pancreas
- Magnetic resonance cholangiopancreatography (MRCP)
- Pancreatic divisum
- Annular pancreas
- Cystic fibrosis
- Pancreatitis
- Pancreaticoblastoma
- Solid pseudopapillary tumor
- Pancreatic traumatic injury
Introduction
The discovery of the pancreas is attributed to the ancient Greek physician Herophilus (335–380 BC). Unlike other larger abdominal organs, such as the liver, the pancreas was largely ignored in early medicine, relegated as a “cushion of the stomach and pad supporting the vessels” [1]. In 1642, the German surgeon Johann Georg Wirsung discovered the main pancreatic duct, and subsequent experiments established that the pancreas was a complex and essential organ whose dysfunction could lead to illness and death [1]. Today, the pancreas is known to serve vital roles in the both the digestive and endocrine systems. Pancreatic disease has a lower incidence in children compared to adults, but pathologies such as pancreatitis have been increasing in the pediatric population and are associated with significant morbidity and mortality [2].
Diagnostic imaging plays an important role in evaluating pancreatic disorders in children and adolescents. Ultrasound and magnetic resonance (MR) imaging are preferred modalities over computed tomography (CT), in large part because both methods avoid ionizing radiation. MR imaging, in particular, offers additional advantages including multiplanar imaging capability and superior soft tissue contrast. Technologic advancements have made diagnostic-quality MR imaging examinations faster and more feasible for pediatric patients.
The adept radiologist should be familiar with the normal development of the pancreas and the various manifestations of disease that are seen in and often unique to children. Some pathologies (e.g., acute pancreatitis) are similar in imaging appearance to their adult counterparts, but often have different etiologies. Meanwhile, some congenital anomalies and certain neoplasms are almost exclusively seen in children.
The overarching goal of this chapter is to discuss the up-to-date and fundamental basics of pediatric pancreatic MR imaging protocols, the normal and abnormal development of the pancreas, and MR imaging features of pancreatic disorders in the pediatric population.
Magentic Resonance Imaging Techniques
In recent years, MR imaging has become increasingly useful for evaluating pancreatitis and pancreatic tumors in the pediatric population. The superior soft tissue contrast and its ability to image the pancreas in multiple contrast-enhanced phases make MR imaging ideally suited to evaluating both diffuse and focal pancreatic pathology. MR cholangiopancreatography (MRCP) is a specialized MR imaging technique that provides excellent noninvasive evaluation of the pancreaticobiliary tree and often serves as an imaging alternative to endoscopic retrograde cholangiopancreatography (ERCP), which is invasive and often requires general anesthesia when performed in the pediatric population. Secretin is a hormone that is produced by the duodenum and stimulates pancreatic exocrine secretion. Synthetic secretin-enhanced MRCP is a technique that improves sensitivity for visualizing pancreatic duct abnormalities due to secretin-induced ductal dilatation [3]. Pancreatic exocrine function can also be assessed by secretin MRCP by visualizing or quantifying secretin-induced duodenal fluid [3].
Patient Preparation
As with all pediatric studies, MR imaging of the pancreas should be tailored to the clinical question and the patient’s age, size, and ability to cooperate. MR imaging of the pancreas is challenging in young children because of potential image quality degradation from respiratory motion and patient movements. During the examination, child life specialists, engagement and education of patients and families, and distraction techniques like music and video goggles can help relax pediatric patients and decrease motion artifacts [4]. These environmental factors and faster MR imaging sequences often reduce the need for anesthesia, thus making examinations faster and safer for pediatric patients. Deep sedation or general anesthesia may be required, particularly for young children between 6 months and 6 years of age [4].
No specific patient preparation is required for pancreatic MR imaging, although fasting 3–5 hours before an MRCP is beneficial to empty the stomach, decrease bowel motility, and fully distend the gallbladder and biliary tree [2]. Secretin, if used, is administered using a weight-based protocol at a dose of 0.2 mg/kg as a slow infusion over 1 minute [3]. Negative oral contrast agents that decrease the signal intensity of stomach and duodenal contents on T2-weighted images can also improve visualization of the pancreatic duct and ampulla on MRCP [2]. Pediatric patients who require sedation or anesthesia for MR imaging needs to adhere to institutional specific guidelines for NPO (nothing per oral) status to minimize the risk of aspiration.
MR Imaging Pulse Sequences and Protocols
The pancreas is intrinsically hyperintense on T1-weighted images due the high amounts of protein and paramagnetic ions (e.g., manganese) within pancreatic cells [5]. Therefore, the pancreas is well-evaluated on T1-weighted fat-suppressed images, even in the absence of intravenous contrast. Most pancreatic parenchymal abnormalities result in low signal intensity on T1-weighted fat-suppressed images. The normal pancreas enhances avidly on arterial and venous phases and appears similar to the liver on delayed imaging (Fig. 9.1).
Normal pancreas in a 13-year-old boy. Axial T1-weighted MR image (a) shows a uniformly hyperintense pancreas (arrows). T2 signal intensity is uniform and similar to the liver on the axial single-shot image (b, arrows). Post-contrast, the pancreas demonstrates early arterial enhancement (c, arrows) and appears similar in intensity to the liver on delayed imaging (d, arrows)
Unlike adult exams, pediatric MR imaging must be tailored to the size of the patient and may require a reduced field of view and smaller slice thickness. MR imaging of the pancreas is usually performed using a multi-channel phased-array cardiac or body coil, depending on the size of the child. The smallest coil that fits the anatomic region should be used, as this permits a smaller field of view and better resolution [6].
The standard pediatric pancreatic protocol includes T1-weighted in- and opposed-phase breath-hold and T2-weighted fat-suppressed fast-spin echo respiratory-triggered sequences to evaluate the pancreas and adjacent abdominal organs. Volumetric T1-weighted fat-suppressed gradient echo sequences can be acquired in a single breath-hold acquisition (10–20 seconds) and are helpful for evaluating the pancreatic parenchyma for both focal and diffuse abnormalities [2]. This same sequence (also known as VIBE/LAVA/eTHRIVE) can be used for multi-phase post-contrast evaluation of the pancreas, which increases sensitivity for detecting subtle pancreatic lesions, pancreatic vascularity in cases of suspected necrosis in the setting of pancreatitis, and peripancreatic inflammatory changes [7]. Signal averaging is often used for T1-weighted sequences in infants and young children who are unable to suspend respiration. Additional sequences in a pancreatic MR imaging protocol include balanced steady-state free precession (bSSFP) sequences that provide excellent visualization of peripancreatic inflammatory changes, as well as diffusion-weighted imaging (DWI) with B-values up to 800–1000 s/mm2 that are useful for focal lesion detection as well as abscesses associated with pancreatitis [7, 8].
The optimal timing for pancreatic evaluation is late arterial (35–55 seconds post-injection), as the pancreaticoduodenal arteries are end branches of the celiac and superior mesenteric arteries. Additional post-contrast imaging time points include portal venous (60–70 seconds) and delayed venous (2–3 minutes) phases [2, 6].
MRCP consists of a heavily T2-weighted pulse sequence with a long echo time (TE range 500–1000 ms), which increases the conspicuity of bile in the pancreaticobiliary tree while suppressing background signal from soft tissues and vascular structures. Typically, MRCP is a 3D volumetric fast-spin echo sequence, acquired with respiratory triggering in the coronal oblique plane, designed to view the pancreatic duct in its entirety. In secretin MRCP, coronal oblique single-shot T2-weighted images that include the entire pancreatic duct are acquired every 30–60 seconds after secretin administration for a period of 5–10 minutes, with peak pancreatic duct dilatation typically occurring at 3–5 minutes [9]. In children who are breathing fast or irregularly, MRCP image quality can be degraded and thick-slab single-shot T2-weighted imaging can be performed instead to freeze motion [7].
Non-Cartesian radial pulse sequences can also be used to reduce respiratory motion artifacts on T2-weighted and T1-weighted fat-suppressed post-contrast imaging [7, 10]. In these sequences, in-plane K-space is acquired in a spoke-wheel fashion, which leads to oversampling of the center and undersampling of the periphery of K-space. Oversampling the center of k-space, which encodes for image contrast, results in high signal-to-noise and contrast-to-noise ratios. Because the phase-encoding direction shifts with the rotating lines of radial k-space acquisition, respiratory motion is dispersed over multiple axes, leading to less reduction in visual image quality compared with standard Cartesian sequences [7]. These sequences are particularly helpful for young children who are unable to suspend respiration.
Anatomy
Embryology
The pancreas emerges at approximately 3–4 weeks gestation [11]. Pancreatic development begins with formation of ventral and dorsal pancreatic buds or anlagen (Fig. 9.2a), which originate from the endodermal lining of the duodenum. The dorsal pancreatic bud or anlage forms below the greater curvature of the stomach, eventually becoming the neck, body, and tail of the pancreas. At the same time, the ventral bud becomes the head and uncinate process. The dorsal bud initially drains into the dorsal duct of Santorini and then into the minor papilla of the duodenum, above the insertion site of the common bile duct (CBD). The ventral bud is drained by the ventral duct of Wirsung into the major papilla of the duodenum, at the same level as the CBD [12].
Early development of the pancreas . At approximately 3–4 weeks gestation (a), the ventral and dorsal anlagen or buds develop from the endodermal lining of the duodenum, which arises at the junction between the foregut and midgut. At about 7 weeks gestation (b), the stomach and duodenum rotate, pulling the ventral anlage posteriorly and inferiorly, and the dorsal bud anteriorly and superiorly. (Images: Susanne L. Loomis, MS, FBCA; Department of Radiology, Massachusetts General Hospital, Boston, Massachusetts, USA)
At about 7 weeks gestation, the stomach and duodenum rotate, pulling the ventral bud posteriorly and inferiorly, while the dorsal bud moves anteriorly and superiorly, resulting in the final position of the pancreas (Fig. 9.2b). The ventral and dorsal ducts fuse in the pancreatic head [11].
Normal Development and Anatomy
The pancreas is a retroperitoneal organ, located posterior to the lesser sac (Fig. 9.3). The pancreas is divided into the head, uncinate process, neck, body, and tail. The head is the thickest part of the pancreas, surrounded by the duodenum, and to the right of the superior mesenteric artery (SMA) and superior mesenteric vein (SMV). The uncinate process emerges from the back of the pancreatic head, posterior to the SMA and SMV. The neck, between the head and body, is the thinnest part of the pancreas and lies in front of the SMA and SMV, anterior to the portosplenic confluence. The body is the largest portion. The tail abuts the splenic hilum.
Normal MR imaging pancreatic anatomy in a 16-year-old girl. Normal appearance of the pancreatic head, uncinate process, and surrounding structures (labeled). The pancreatic body and tail are not visualized on this image. SMV, superior mesenteric vein; SMA, superior mesenteric artery; IVC, inferior vena cava
The pancreas has both endocrine and exocrine functions. The endocrine glands are composed of discrete units called islets of Langerhans, which secrete hormones, including insulin, glucagon, somatostatin. The exocrine glands, a network of acinar cells, secrete pancreatic fluid into the duodenum via the pancreatic duct; bicarbonate neutralizes gastric acid and enzymes aid with digestion [11, 12].
Anatomic Variants
Anatomic anomalies of the pancreas arise due to failed fusion of the ventral and dorsal buds or abnormal rotation. Often, these are incidental discoveries in asymptomatic pediatric patients. However, it is important to recognize these structural anomalies as some lead to pathology, such as recurrent pancreatitis or duodenal obstruction, and may require surgical correction. MRCP demonstrates the course and drainage pattern of the pancreatic duct and is helpful in diagnosing developmental anomalies. In recent years, MRCP has replaced ERCP as the primary diagnostic tool for evaluating pancreatic ductal anatomy in pediatric patients.
Pancreas Divisum
Pancreas divisum is the most common congenital pancreatic abnormality, seen in about 10% of the population [13]. It is caused by non-fusion of the ventral and dorsal pancreatic ducts, which retain their primitive drainage patterns (Fig. 9.4). This is identified on MRCP by the “crossing” sign, when the common bile duct crosses the dorsal pancreatic duct as it courses to join the ventral duct [12].
Pancreas divisum anatomy. In pancreas divisum (a), the ventral and dorsal ducts do not fuse, retaining their early drainage patterns. The normal drainage pattern is shown as comparison (b). (Images: Susanne L. Loomis, MS, FBCA; Department of Radiology, Massachusetts General Hospital, Boston, Massachusetts, USA)
In complete pancreas divisum, the main (dorsal) pancreatic duct drains into the minor papilla without communicating with the ventral duct (Fig. 9.5). Complete pancreas divisum may be a cause of recurrent pancreatitis in pediatric patients. In incomplete divisum, some communication remains between the dorsal and ventral ducts [12]. Incomplete pancreas divisum is considered a normal anatomic variant and not associated with pathology [13].
Pancreas divisum in an 18-year-old female with ulcerative colitis and primary sclerosing cholangitis. 3D thick maximum intensity projection MR image demonstrates the crossing sign of pancreas divisum. The main pancreatic duct (arrow) crosses over the common bile duct (arrowhead) into drains into the minor papilla via the dorsal duct of Santorini. Note the additional beading of the intrahepatic bile ducts, characteristic of primary sclerosing cholangitis
Annular Pancreas
Annular pancreas is rare and occurs when the ventral bud does not fully rotate and a part of the pancreas wraps around the second portion of duodenum [11] (Fig. 9.6). There are two types of annular pancreas: extramural and intramural. In the extramural type, the ventral duct encircles the duodenum and joins the main duct. This presents with duodenal obstruction in infancy and is one etiology of the classic “double-bubble” sign in neonates. In the intramural type, pancreatic tissue is within the walls of the duodenum, and small ducts drain directly into the duodenum. These children may present with peptic ulcer disease, without duodenal obstruction [12]. One-half to two-thirds of all patients with annular pancreas are asymptomatic [14].
Pancreatic Agenesis and Hypoplasia (Congenital Short Pancreas)
Complete agenesis of the pancreas is rare and lethal. Partial agenesis is still very rare but compatible with life and usually involves the dorsal rather than ventral pancreas. In dorsal agenesis or hypoplasia, the pancreatic head appears enlarged and widened, with a partially or completely absent pancreatic body and tail [12] (Fig. 9.7). Patients with dorsal pancreatic agenesis are at risk of developing abdominal pain, hypoglycemia, and pancreatitis related to problems with pancreatic drainage [15].
Ectopic Pancreas
Residual primitive cells from the ventral and dorsal buds can migrate to nearby structures and mature, leading to ectopic pancreatic tissue in locations such as the gastric antrum or duodenum (Fig. 9.8). Ectopic pancreatic tissue is subject to the same inflammatory and neoplastic processes affecting the orthotropic pancreas. Rarely, cystic dystrophy can occur, which represents cystic dilatation of the ectopic ducts and occurs most often in the second portion of the duodenum [12, 13].
Ectopic pancreas in a 17-year-old girl with abdominal pain and vomiting. Coronal single-shot T2-weighted (a) and T1-weighted fat-suppressed pre- (b) and post-contrast (c) MR images demonstrate a T2-weighted hypointense, T1-weighted hyperintense, mildly enhancing lesion (arrows) in the stomach. The lesion consistent with ectopic pancreas on biopsy. Incidental note is made of a hepatic mass found to be a focal nodular hyperplasia
Intrapancreatic Splenic Tissue
Accessory spleens, or splenules, are congenital foci of normal splenic tissue separate from the main spleen. These are distinguished from splenosis, which is autotransplantation of splenic tissue, usually after splenectomy or trauma. The tail of the pancreas is the second most common site of an accessory spleen (the splenic hilum is the most common location). This is usually an incidental finding on CT or MR imaging and is important not to mistake for a mass. The accessory spleen typically has the same signal characteristics as the spleen on all MR pulse sequences (Fig. 9.9) [12].
Pancreatic Cyst
A true congenital pancreatic cyst is very rare. As opposed to cystic dilatation of the pancreatic duct or pseudocysts, true pancreatic cysts are lined by epithelium and do not communicate with the pancreatic ducts. These may be idiopathic or associated with systemic diseases like von Hippel-Lindau disease, Beckwith-Wiedemann syndrome, or polycystic kidney disease [12].
Spectrum of Pancreatic Disorders
Congenital Pancreatic Disorders
von Hippel-Lindau Disease
von Hippel-Lindau (VHL) disease is a rare autosomal dominant disorder caused by a mutation in the VHL tumor suppressor gene on chromosome 3. Patients with VHL are at high risk for various malignancies, including neuroendocrine tumors and serous cystadenomas in the pancreas. The disease is also associated with bilateral or multifocal renal cell carcinomas, adrenal pheochromocytomas, skull base endolymphatic sac tumors, and hemangioblastomas involving the brainstem, cerebellum, and spinal cord. Numerous cysts can be seen in the kidneys, pancreas, and liver [12].
Cystic Fibrosis
Cystic fibrosis (CF) is an autosomal recessive disease caused by a gene defect encoding the CF transmembrane conductance regulator (CFTR), which is a chloride and bicarbonate channel. Abnormal chloride metabolism causes glands to produce abnormally thick, viscous material. This is mostly seen in the exocrine glands of the tracheobronchial tree, pancreas, sweat glands, and seminal vesicles of boys. The pancreas is one of the organs earliest affected by CF [12, 16].
In patients with CF, thickened secretions result in plugging of the proximal pancreatic ducts, leading to exocrine insufficiency, which is seen in approximately 85–90% of CF patients. Endocrine dysfunction is seen in about 30–50% of patients [16]. Fatty infiltration is the most common manifestation of CF in the pancreas, usually seen in adolescence or early adulthood. This can progress to complete pancreatic lipomatosis (Fig. 9.10). Pancreatic cystosis can also be seen, which is diffuse replacement of the pancreas with cysts of varying sizes (Fig. 9.11). On MR imaging, the cysts demonstrate typical low T1-weighted and high T2-weighted signal [16]. Various abnormalities of the ducts can occur, including strictures, dilatation, and obstruction [17].
Shwachman-Diamond Syndrome
Shwachman-Diamond syndrome is a rare, autosomal recessive disease, caused by a mutation in the Shwachman-Bodian-Diamond gene, the function of which is unknown. It is a multisystem disease, which involves the bones, bone marrow, and pancreas, often manifesting as pancreatic exocrine insufficiency, neutropenia, and bone dysplasia [18]. It is the second most common cause of childhood pancreatic atrophy, following CF [12]. The characteristic imaging feature is fatty replacement of the pancreas, which is well-visualized on MR imaging using paired T1-weighted or T2-weighted sequences with and without fat suppression. Unlike other causes of fatty pancreatic atrophy, the pancreas in Shwachman-Diamond syndrome is normal in size [18].
Congenital Hyperinsulinism
Congenital hyperinsulinism (CHI), otherwise known as persistent hyperinsulinemic hypoglycemia of infancy , is an uncommon (1:50,0000 live births) but important cause of severe neonatal hypoglycemia. CHI was previously known as nesidioblastosis, meaning the persistence of nesidioblasts, which are fetal pancreatic cells [12]. CHI is attributable to a range of mutations that regulate insulin secretion, resulting in proliferation of B islet cells and pancreatic ducts. CHI is typically sporadic but can be associated with genetic conditions, including Beckwith-Wiedemann and Sotos syndromes [19].
Affected patients typically present with recurrent hypoglycemia refractory to feeds. CHI can be either diffuse or focal, with MRI being helpful to identify the extent of parenchymal enlargement, usually without an identifiable discrete mass [12] (Fig. 9.12), although MR imaging may not be definitive. As much, it is important to know that the diagnosis of CHI is usually made by F-DOPA PET imaging. It is important to distinguish the two forms of CHI because the focal form typically is treated by subtotal pancreatectomy, while diffuse CHI is typically managed medically [20].
Inflammatory Pancreatic Disorders
Acute Pancreatitis
Pancreatitis, which is defined as inflammation of the pancreas, is the most common pancreatic disorder in children and adults. Three categories of pancreatitis have been defined: acute pancreatitis, acute recurrent pancreatitis, and chronic pancreatitis, based on the number of pancreatitis episodes and the presence or absence of irreversible features of pancreatitis [21]. Acute pancreatitis is diagnosed clinically when two of the following are present: abdominal pain compatible with acute pancreatitis, serum amylase or lipase more than three times the upper limit of normal, and imaging findings consistent with acute pancreatitis [22]. The incidence of acute pancreatitis has increased in the pediatric population, which may be related to increased frequency of testing and childhood obesity. Pancreatitis occurs in all age groups, including infants, although studies have shown that it is more common in children more than 5 years old [2].
Pancreatitis in children is associated with significant morbidity and mortality. About one-quarter of children develop severe complications and the mortality rate is estimated to be 4% [2, 22]. Therefore, it is important for radiologists to have a broad awareness of pancreatitis in children in order to help guide appropriate treatment.
Imaging has a pivotal role in diagnosing pancreatitis. For children, ultrasound is the primary imaging modality of choice, although CT is also widely used. MR imaging with MRCP is becoming increasingly helpful and may soon replace CT, as it is able to provide exquisite anatomic delineation of the pancreatic parenchyma and pancreaticobiliary duct system. Acute pancreatitis in children looks similar to that in adults. The most common imaging feature of acute pancreatitis is an edematous enlarged pancreas, which in early or mild cases may be identified only as a subtle contour abnormality or increased signal intensity on T2-weighted imaging [23, 24]. The pancreas demonstrates loss of its intrinsic T1-weighted signal intensity, instead becoming heterogeneous and hypointense. Peripancreatic edema and fluid collections are often seen [2, 23] (Fig. 9.13).
Acute pancreatitis in an 18-year-old male who presented with acute abdominal pain. Axial single-shot T2-weighted MR image (a) demonstrates a swollen pancreas with small peripancreatic fluid collections (arrows). Fat-suppressed T1-weighted MR image (b) demonstrates areas of low signal intensity within the pancreatic body (arrowhead) consistent with edema in the context of acute pancreatitis
Complications of Acute Pancreatitis
Pseudocysts are the most common complication of acute pancreatitis, and the most common lesions seen within the pancreas. They are T2-weighted hyperintense and may have high T1-weighted signal intensity due to internal debris or hemorrhage. There may be peripheral enhancement surrounding the cyst but no internal enhancement (Fig. 9.14), which would suggest a mass [2].
Pancreatic pseudocyst in a 13-year-old boy with a history of acute pancreatitis. A lobulated cystic lesion (arrow) is seen in the pancreatic tail on an axial T2-weighted fat-suppressed MR image (a). This demonstrates a rim of enhancement (arrow) on a T1-weighted fat-suppressed post-contrast MR image (b). The patient’s history of acute pancreatitis favors a diagnosis of a pseudocyst, which was confirmed when the lesion resolved on subsequent imaging
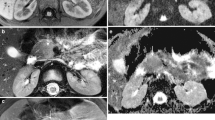
Necrotizing pancreatitis is uncommon in children but is important to be aware of because it is associated with increased morbidity and mortality [25]. Classic MR imaging features include focal areas of non-enhancement on post-contrast sequences that typically show high signal intensity on T1-weighted imaging. Gas can also be a feature of more severe necrotizing pancreatitis and can be difficult to identify on MR imaging, appearing as punctate low signal foci on T1- and T2-weighted images. Gradient recalled echo imaging (such as T1-weighted fat-suppressed pre-contrast imaging) can be helpful to identify susceptibility artifact from air associated with pancreatic necrosis [2, 24, 25]. Hemorrhagic changes may also be seen in necrotizing pancreatitis, which may affect the pancreas itself or surrounding fatty tissue (Fig. 9.15).
Pancreaticopleural fistulas are extremely rare, occurring in less than 1% of patients with pancreatitis. This complication should be considered if the patient has large, recurrent pleural effusions despite resolution of his or her acute symptoms. T2-weighted and contrast-enhanced sequences may show a fistulous connection between the pancreatic duct and pleural space. The diagnosis can be confirmed by high amylase levels in the pleural fluid aspirate [2].
Vascular complications, including splenic vein thrombosis or splenic artery pseudoaneurysms, arise due to the close proximity of these vascular structures to inflamed pancreatic tissue. These are best detected on sequential contrast-enhanced T1-weighted fat-suppressed sequences [2, 23].
Causes of Pancreatitis
About 10–20% of pediatric patients have recurrent episodes of pancreatitis. Many of these causes are treatable and thus it is important to identify on imaging if possible. Biliary disease is one of the most common causes of acute pancreatitis in children, accounting for approximately 10–30% of cases (although compared to more than 80% of adult pancreatitis). Obesity is both a risk factor for developing gallstones and an independent risk factor for developing gallstone pancreatitis. Pancreaticobiliary anomalies, including pancreas divisum, have been associated with recurrent pancreatitis. Approximately 50% of patients with acute recurrent pancreatitis have genetic pancreatitis predisposition mutations, with mutations in cystic fibrosis transmembrane conductance regulator (CFTR) and pancreatic secretory trypsin inhibitor (SPINK1) being among the most common [26]. Other less common but important causes of acute pancreatitis in children include trauma, autoimmune disorders, medications (e.g., valproic acid, prednisone, L-asparaginase, and 6-mercaptopurine), and certain systemic diseases like CF, chronic renal failure, and diabetes [2, 27].
Chronic Pancreatitis
Chronic pancreatitis is relatively uncommon in children compared to adults. Children with chronic pancreatitis usually have genetic risk factors or congenital anomalies leading to chronic obstruction (e.g., pancreas divisum). Chronic pancreas can be debilitating in children and associated with significant morbidity, including chronic pain, frequent emergency room visits, hospitalizations, as well as lost time from school [28].
On MR imaging, the afflicted pancreas demonstrates low T1-weighted signal intensity and atrophy (Fig. 9.16), with MRCP ideally suited to show pancreatic duct tortuosity and dilatation (Fig. 9.17) as well as increased visibility of pancreatic duct side branches [23, 24]. Parenchymal calcifications associated with chronic pancreatitis are difficult to identify on MR imaging but appear as punctate foci of low signal intensity on T1-weighted and T2-weighted images causing susceptibility artifact on GRE imaging (similar to air). Acute on chronic pancreatitis has features of acute pancreatitis (edema, peripancreatic fluid) superimposed on chronic changes (abnormal duct morphology) (Fig. 9.18).
Chronic pancreatitis and pseudocyst in an 11-year-old boy. Axial T2-weighted fat-suppressed MR images demonstrate a pseudocyst (a, b; arrows) anterior to an atrophic pancreas. The main pancreatic duct can be seen posterior to the pseudocyst and is dilated and beaded in appearance (b; arrowhead). Overall these findings are consistent with chronic pancreatitis
Acute on chronic pancreatitis in a 15-year-old girl with abdominal pain. The main pancreatic duct is markedly dilated with a gradual transition at the pancreatic neck, as seen on this single-shot T2-weighted MR image. There is peripancreatic edema (note blurred parenchymal margins). Findings are consistent with acute on chronic pancreatitis
Autoimmune Pancreatitis
Autoimmune pancreatitis is a rare entity in adults, and even more uncommon in children, although the disease is increasing being recognized in both demographic groups. Unlike the adult form, autoimmune pancreatitis in children is less frequently associated with an elevated IgG4, seen in 22% of children with the disease [29]. On MR imaging, the pancreas typically demonstrates low signal intensity on T1-weighted images and be globally or focally enlarged. Focal or segmental autoimmune pancreatitis may mimic a pancreatic mass. Other imaging features to look out for in the setting of autoimmune pancreatitis include irregularity of the main pancreatic duct and narrowing of the common bile duct, which are seen in the majority of cases [23, 29]. Most children respond well to steroids, with accompanying normalization of the pancreas on imaging.
Neoplastic Pancreatic Disorders
Pancreatic tumors are relatively rare in children compared with adults. In general, they have distinct histologic patterns and fortunately better prognoses compared to their adult counterparts. Pancreatic neoplasms can be divided into those of epithelial origin and those of non-epithelial origin (Table 9.1).
Pancreatic neoplasms in general occur less frequently in children compared with adults. This section focuses on pancreatic neoplasms that are most likely to occur in pediatric patients, acknowledging that several of these tumors are very rare and MRI is often not the primary imaging modality for diagnosis.
Epithelial Pancreatic Neoplasms
Pancreatoblastoma
Pancreatoblastoma , formerly infantile pancreatic carcinoma, is the most common pancreatic tumor in children, representing approximately 25% of pancreatic tumors. However, this tumor is still extremely rare, with an incidence of less than 1 per 1,000,000 children [30]. Pancreatoblastoma may be slightly more common in males and usually occurs in the first decade of life (mean age is 5 years old). The tumor is often quite large (2–20 cm) at diagnosis, and clinical presentation is variable based on mass effect, ranging from abdominal pain and nausea and vomiting to jaundice. Alpha-fetoprotein (AFP) is usually elevated. While there is some association with Beckwith-Wiedemann syndrome, most cases are sporadic [30].
On MR imaging, pancreatoblastomas are usually large mixed solid-cystic masses with well-defined margins. They usually arise from the pancreatic head and tend to protrude into the lesser sac (Fig. 9.19). Pancreatoblastomas demonstrate low to intermediate T1-weighted signal intensity and heterogeneously increased T2-weighted signal intensity due to hemorrhage and necrosis [31]. Calcifications are often present and better seen on CT. About one-third of patients have metastases at presentation, usually to the liver [30].
Pancreatoblastoma in a 4-year-old boy. Axial T2-weighted (a) and T1-weighted (b) fat-suppressed MR images demonstrate a large, well-circumscribed low signal mass originating from the pancreatic head/neck, protruding into the lesser sac. The mass demonstrates enhancement on arterial and venous phase T1-weighted fat-suppressed post-contrast MR images (c, d) and was shown to be a pancreatoblastoma on histology
Solid Pseudopapillary Tumor
In contrast to pancreatoblastomas, which are usually seen in male children less than 10 years old, solid pseudopapillary tumors (SPT; also known as solid pseudopapillary epithelial neoplasms) are more common in young women in their second or third decade of life. Affected patients may present with abdominal pain but are often asymptomatic [30].
SPN is a mixed solid and cystic, slow-growing tumor, often large at diagnosis (>5 cm). The most common location is the pancreatic head. Key imaging features include a fibrous capsule and internal hemorrhage. The fibrous capsule typically demonstrates low signal intensity on T1-weighted and T2-weighted imaging (Fig. 9.20). The solid components can demonstrate hemorrhage, particularly at larger sizes [30, 31]. Although usually benign, the tumor has malignant potential and therefore is treated with surgical resection. Vascular invasion and capsule disruption are aggressive features. Metastases are uncommon and are most common in the liver [30].
Pancreatic solid pseudopapillary tumor and liver metastasis in an 18-year-old female. Axial T1-weighted (a) and T2-weighted (b) MR images demonstrate a large, well-circumscribed, heterogeneous, mass originating from the pancreatic body/tail (arrowheads; a–d). Intrinsic T1-weighted hyperintensity likely represents hemorrhage. T1-weighted fat-suppressed pre- (c) and post-contrast (d) images show heterogeneous enhancement of the mass. There is also a hypoenhancing hepatic lesion (arrows; a–d) consistent with a hepatic metastasis
Neuroendocrine (Islet Cell) Tumors
Islet cell tumors are neuroendocrine tumors seen in older children. In general, tumors that are large at presentation are typically non-functioning as they do not cause symptoms until they compress adjacent structures. Conversely, hormonally active neuroendocrine cell tumors are often small at diagnosis. Clinical features of islet cell tumors are summarized in Table 9.2.
The most common islet cell tumor is the insulinoma, accounting for approximately 50% of cases. These tumors often present at a very small size due to their clinical symptoms related to hypoglycemia. Insulinomas are often seen in the body or tail of the pancreas [30]. Gastrinomas are the second most common islet cell tumor, representing 30% of cases. These tend to occur in the “gastrinoma triangle,” between the junction of the cystic duct and CBD, duodenum, and neck and body of the pancreas [30]. While the majority of islet cell tumors arising in children occur sporadically, there is an association with genetic conditions such as multiple endocrine neoplasia type 1 and von Hippel-Lindau syndrome [23]. More recently, an association has been established with tuberous sclerosis complex in which nonfunctional pancreatic islet cells are incidentally discovered during renal imaging surveillance. The current data suggest that the islet cell tumors arising in this context are indolent [32].
On MR imaging, islet cell tumors are typically solid, hypervascular masses that avidly enhance on arterial-phase sequences (Fig. 9.21). They can be inconspicuous to background parenchyma on delayed sequences, which emphasizes the importance of arterial phase imaging. They often demonstrate heterogeneous signal intensity on T2-weighted images, including central areas of necrosis when the tumors become large in size [30, 31].
Pancreatic insulinoma in an 8-year-old girl who presented with hypoglycemia. Axial T1-weighted fat-suppressed MR image (a) shows a hypointense lesion (arrows) in the tail of the pancreas, with avid arterial enhancement post-contrast (b), in keeping with a neuroendocrine tumor. Pathology was compatible with an insulinoma
Non-epithelial Pancreatic Neoplasms
Lymphoma
Pancreatic involvement of lymphoma is the most common non-epithelial tumor of the pancreas. Although very rare, most cases of pancreatic lymphoma are non-Hodgkin lymphoma. Burkitt lymphoma , an aggressive B-cell non-Hodgkin lymphoma that is associated with translocation of the MYC oncogene, can present as a rapidly growing pancreatic mass associated with pancreatitis [33]. Primary (isolated to the pancreas) and secondary (present in both the pancreas and lymphatic organs) pancreatic lymphoma have similar imaging features. Presenting symptoms are nonspecific and may include a palpable abdominal mass, weight loss, and obstructive jaundice [30].
Lymphoma of the pancreas has two morphologic patterns: focal and diffuse. The focal form most often involves the pancreatic head, with low T1-weighted signal intensity and intermediate T2-weighted signal intensity (Fig. 9.22). Post-contrast sequences may demonstrate either absent or mild enhancement [30, 31].
The diffuse form leads to glandular enlargement and could mimic acute pancreatitis. There is typically global low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. The pancreas typically demonstrates diffuse enhancement with small foci or decreased or no enhancement. Compression of the biliary tree may be seen [31]. Diffusion restriction on DWI sequences is also characteristic and related to the high nuclear to cytoplasmic ratio of the tumor cells.
Metastases
Non-pancreatic tumors within the pancreas typically occur due to local invasion from contiguous organs, most commonly neuroblastoma from the adrenal gland [30] (Fig. 9.23). Metastases to the pancreas is very rare.
Mimics and Pitfalls of Pancreatic Neoplasms
It is important to understand that non-neoplastic pathologies (e.g., splenules, pseudocysts, focal pancreatitis), discussed earlier in the chapter, may present as mass-like lesions. For example, fatty infiltration of the pancreas can be focal or diffuse and could mimic a neoplasm. In such a case, T1-weighted in- and out-of-phase MR imaging confirms the diagnosis (Fig. 9.24). True pancreatic lesions do not contain fat except for pancreatic lipomas, which are uncommon but benign. Duodenal diverticula are rare in children, but are another potential pitfall. It is important to recognize that air causes inhomogeneities in the magnetic field and blooming artifacts on in-phase images due to their longer TE. Often the clinical presentation (e.g., fever, abdominal pain) would favor pancreas over a mass lesion, although follow-up imaging may be required.
Incidental pancreatic lipoma in an 18-year-old female. Axial T1 fat-suppressed MR image (a) demonstrates a small low signal intensity lesion (arrow) in the tail of the pancreas. T1-weighted chemical shift in-phase (b) and opposed phase (c) MR images demonstrate signal loss on the opposed phase image (c, arrow), at the interface between the lipoma and the surrounding normal pancreas
Inflammatory myofibroblastic tumors (IMTs) , previously known as inflammatory pseudotumors , are unusual pseudosarcomatous lesions that can mimic a malignant mass. Composed of inflammatory myofibroblastic spindle cells, these are most often seen in children and young adults. The lungs and orbits are most often involved, but cases have been reported in nearly every organ [34]. While IMT does not demonstrate aggressive features (Fig. 9.25), imaging cannot currently confidently distinguish IMT from a malignancy, especially in the pancreas where very few cases have been reported. As such, treatment is currently surgical resection.
Myofibroblastic pancreatic tumor in a 17-year-old boy. Axial T2-weighted fat-suppressed (a) and T1-weighted fat-suppressed post-contrast (b) MR images show a well-circumscribed enhancing mass (arrows) in the head of the pancreas. There is no infiltration of surrounding structures. Pathology demonstrated a myofibroblastic tumor, previously known as an inflammatory pseudotumor
Traumatic Pancreatic Injury
Pancreatic injury occurs in 5–10% of children with blunt abdominal trauma and is almost never isolated. The pancreas is vulnerable to injury given its fixed position in the retroperitoneum. Two-thirds of injuries occur in the pancreatic body, which is the largest pancreatic segment. Trauma to the pancreas has a grading system, listed in Table 9.3. Unexplained pancreatic injury, especially in an infant, should raise concern for child abuse [23, 24].
Pancreatic injury is associated with direct blunt force trauma to the abdomen, often handlebar injuries or secondary to child abuse in children. Lacerations and hematoma can be seen (Fig. 9.26). Direct signs of injury (e.g., lacerations) are often subtle and difficult to detect, so it is important to look for secondary signs of injury. These include peripancreatic fluid in the anterior pararenal space or lesser sac and findings of pancreatitis (Fig. 9.27).
Handle bar injury in an 8-year-old boy. Axial T1-weighted fat-suppressed MR image (a) demonstrates a hematoma in the pancreatic body (arrow), on a background of contusion, disrupting the path of the main pancreatic duct. Four months later, axial T2-weighted MR image (b) shows this area had matured into a pseudocyst (asterisk)
Focal pancreatitis in an 18-year-old male with abdominal trauma. Axial single-shot T2-weighted MR image demonstrates swelling and focal high signal in the body of the pancreas (arrows), consistent with focal pancreatitis secondary to trauma. Note the diminished size of the uninvolved pancreatic tail for comparison
Treatment of pancreatic injury is somewhat controversial in children, with the standard of care currently being medical management. Although CT is often the initial imaging modality diagnosing traumatic injury of the pancreas in the setting of blunt abdominal trauma, MRI often plays an important role in assessing for development of peripancreatic fluid collections suggesting pancreatic duct injury, as well as MRCP direct assessment of pancreatic duct integrity [35].
Conclusion
Clear knowledge of normal development and various disorders of the pediatric pancreas is important to allow for generating appropriate differential diagnoses and facilitating optimal care for pediatric patients. In summary, pancreatic disorders are relatively uncommon and often incidental in the pediatric population but are important to recognize as they may cause acute or recurrent symptoms. These are best diagnosed with MR imaging including MRCP. Pancreatitis in children is becoming more common and is important to keep on the differential diagnosis of a pediatric patient with abdominal pain. Pancreatitis can be subtle on imaging and is important to diagnose before complications arise. Pancreatic tumors are very rare in the pediatric population but can often be differentiated on the basis of MR imaging features, patient age/gender, and clinical presentation.
References
Howard JM, Hess W. History of the 9ancreas: mysteries of a hidden organ. 2nd ed. New York: Springer; 2002.
Restrepo R, Hagerott HE, Kulkarni S, Yasrebi M, Lee EY. Acute pancreatitis in pediatric patients: demographics, etiology, and diagnostic imaging. Am J Roentgenol. 2016;206(3):632–44.
Trout AT, Podberesky DJ, Serai SD, Ren Y, Altaye M, Towbin AJ. Does secretin add value in pediatric magnetic resonance cholangiopancreatography? Pediatr Radiol. 2013;43(4):479–86.
Jaimes C, Gee MS. Strategies to minimize sedation in pediatric body magnetic resonance imaging. Pediatr Radiol. 2016;46(6):926–7.
Semelka RC, Ascher SM. MR imaging of the pancreas. Radiology. 1993;188(3):593–602.
Nievelstein RA, Robben SGF, Blickman JG. Hepatobiliary and pancreatic imaging in children—techniques and an overview of neo-neoplastic disease entities. Pediatr Radiol. 2011;41(1):55–75.
Jaimes C, Kirsch JE, Gee MS. Fast, free-breathing and motion-minimized techniques for pediatric body magnetic resonance imaging. Pediatr Radiol. 2018;48(9):1197–208.
Chavhan GB, AlSabban Z, Babyn PS. Diffusion-weighted imaging in pediatric body mr imaging: principles, techniques, and emerging applications. Radiographics. 2014;34(3):E73–88.
Manfredi R, Pozzi Mucelli R. Secretin-enhanced MR imaging of the pancreas. Radiology. 2016;279(1):29–43.
Chavhan GB, Babyn PS, Vasanawala SS. Abdominal MR imaging in children: motion compensation, sequence optimization, and protocol organization. Radiographics. 2013;33(3):703–19.
Sadler TW. Langman’s medical embryology. 11th ed. Philadelphia: Lippincott Williams and Wilkins; 2010.
Borghei P, Sokhandon F, Shirkhoda A, Morgan DE. Anomalies, anatomic variants, and sources of diagnostic pitfalls in pancreatic imaging. Radiology. 2013;266(1):28–36.
Bülow R, Simon P, Thiel R, Thamm P, Messner P, Lerch MM, et al. Anatomic variants of the pancreatic duct and their clinical relevance: an MR-guided study in the general population. Eur Radiol. 2014;24(12):3142–9.
Sandrasegaran K, Patel A, Fogel E, Zyromski NJ, Pitt HA. Annular pancreas in adults. AJR Am J Roentgenol. 2009;193(2):455–60.
Schnedl WJ, Piswanger-Soeklner C, Wallner SJ, Reittner P, Krause R, Lipp RW, et al. Agenesis of the dorsal pancreas and associated diseases. Dig Dis Sci. 2009;54(3):481–7.
Berrocal T, Pajares MP, Zubillaga AF. Pancreatic cystosis in children and young adults with cystic fibrosis: sonographic, CT, and MRI findings. AJR Am J Roentgenol. 2005;184(4):1305–9.
Fields TM, Michel SJ, Butler CL, Kriss VM, Albers SL. Abdominal manifestations of cystic fibrosis in older children and adults. AJR Am J Roentgenol. 2006;187(5):1199–203.
Toivianinen-Salo S, Raade M, Durie PR, Ip W, Marttinen E, Savilahti MO. Magnetic resonance imaging findings of the pancreas with Shwachman-Diamond syndrome and mutations in the SBDS gene. J Pediatr. 2008;152(3):434–6.
Arnoux JB, de Lonlay P, Ribeiro MJ, Hussain K, Blankenstein O, Mohnike K, et al. Congenital hyperinsulinism. Early Hum Dev. 2010;86(5):287–94.
Adzick NS, De Leon DD, States LJ, Lord K, Bhatti TR, Becker SA, Stanley CA. Surgical treatment of congenital hyperinsulinism: results from 500 pancreatectomies in neonates and children. J Pediatr Surg. 2019;54(1):27–32.
Shukla-Udawatta M, Madani S, Kamat D. An update on pediatric pancreatitis. Pediatr Ann. 2017;46(5):e207–11.
Morinville VD, Husain SZ, Bai H, Barth B, Alhosh R, Durie PR, et al. Definitions of pediatric pancreatitis and survey on present clinical practices. J Pediatr Gastroenterol Nutr. 2012;55(3):261–5.
Anupini SA, Chauvin NA, Khwaja A, Biko DM. Magnetic resonance imaging of pancreaticobiliary diseases in children: from technique to practice. Pediatr Radiol. 2016;46(6):778–90.
Thai TC, Riherd DM, Rust KR. MRI manifestations of pancreatic disease, especially pancreatitis, in the pediatric population. AJR Am J Roentgenol. 2013;201(6):W877–92. Review.
Raizner A, Phatak UP, Baker K, Patel MG, Husain SZ, Pashankar DS. Acute necrotizing pancreatitis in children. J Pediatr. 2013;162(4):788–92.
Kumar S, Ooi CY, Werlin S, Abu-El-Haija M, Barth B, Bellin MD, et al. Risk factors associated with pediatric acute recurrent and chronic pancreatitis: lessons from INSPPIRE. JAMA Pediatr. 2016;170(6):562–9.
Bai HX, Lowe ME, Hussain SZ. What have we learned about acute pancreatitis in children? J Pediat Gastroenterol Nutr. 2011;52(3):262–70.
Schwarzenberg SJ, Bellin M, Husain SZ, Monika A, Barth B, Davis H, et al. Pediatric chronic pancreatitis is associated with genetic risk factors and substantial disease burden. J Pediatr. 2015;166(4):890–6.
Scheers I, Palermo JJ, Freedman S, Wilschanski M, Shah U, Abu-El-Haij M, et al. Autoimmune pancreatitis in children: characteristic features, diagnosis, and management. Am J Gastroenterol. 2017;112(10):1604–11.
Chung EM, Travis MD, Conran RM. Pancreatic tumors in children: radiologic-pathologic correlation. Radiographics. 2006;26:1211–38.
Shet NS, Cole BL, Iyer RS. Imaging of pediatric pancreatic neoplasms with radiologic histopathologic correlation. AJR Am J Roentgenol. 2014;202:1337–48.
Koc G, Sugimoto S, Kuperman R, Kammen BF, Karakas SP. Pancreatic tumors in children and young adults with tuberous sclerosis complex. Pediatr Radiol. 2016;47(1):39–45.
Amodio J, Brodsky JE. Pediatric Burkitt lymphoma presenting as acute pancreatitis: MRI characteristics. Pediatr Radiol. 2010;40(5):770–2.
Kim SJ, Kim WS, Cheon JE, Shin SM, Youn BJ, Kim IO, Yeon KM. Inflammatory myofibroblastic tumors of the abdomen as mimickers of malignancy: imaging features in nine children. AJR Am J Roentgenol. 2009;193:1419–24.
Sivit CJ. Imaging children with abdominal trauma. AJR Am J Roentgenol. 2009;192(5):1179–89.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Johnson, M., Anupindi, S.A., Gee, M.S. (2020). Pancreas. In: Lee, E., Liszewski, M., Gee, M., Daltro, P., Restrepo, R. (eds) Pediatric Body MRI. Springer, Cham. https://doi.org/10.1007/978-3-030-31989-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-31989-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31988-5
Online ISBN: 978-3-030-31989-2
eBook Packages: MedicineMedicine (R0)