Abstract
Lumbar medial branch diagnostic injection and radiofrequency ablation are commonly performed for chronic lumbar facet-related back pain. This chapter provides a step-by-step guide on how to perform this intervention safely and shows all the relevant C-arm and needle positions that need to be demonstrated during the Fellow of Interventional Pain Practice (FIPP) exam administered by the World Institute of Pain (WIP). Both native and edited high-quality images are included, so the fluoroscopy anatomy is more easily understood.
Possible complications of the procedures and common reasons for failure at the FIPP exam are also outlined. Evidence for the procedure is provided based on the available literature reviewed by the Benelux section of WIP and also by the American Society of Interventional Pain Physicians (ASIPP).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Lumbar medial branch block
- lumbar MBB
- lumbar facet-related pain
- lumbago
- radiofrequency ablation
- FIPP exam
- fluoroscopic needle placement
Equipment and Monitoring
-
Standard ASA monitoring
-
Fluoroscopy
-
Sterile prep, and drape
-
Local anesthesia prior to any needle larger than 25G (unless sedation is used)
-
Coaxial view is always used to advance needle, unless otherwise specified
-
CPR equipment and medications available
For Diagnostic Block
-
22–25G, 3.5 inch (100 mm) – 6 inch (150 mm) needle, tip curved to facilitate steering 150-mm
For Radiofrequency Ablation (RFA)
-
18–20 G RF cannula(s), 10 mm active tip (preferably curved tip), 3.5–5 inch (90–130 mm) depending on body habitus
-
RF generator with capacity for unipolar and bipolar lesions
-
Local anesthetic
-
Grounding pad
Anatomy
-
The innervation of each facet joint is via the medial branches of contiguous dorsal rami; because of the additional cervical nerve (C8), each lumbar facet joint innervation is shifted one level cephalic such that, for example, the L4/5 facet joint is innervated by the L3 and L4 medial branches
-
Furthermore, the L5/S1 facet joint is innervated from above by the medial branch of the L4 dorsal ramus and the L5 dorsal ramus from below
-
The medial branches of the L1–4 dorsal rami , which innervate the facet joints and multifidus, run caudally and dorsally, lying against bone at the junction of the root of the transverse process with the root of the superior articular process from where they pass through a fibro-osseous tissue, covered by the mamillo-accessory ligament. The articular branches arise from this region
-
The L5 dorsal ramus passes dorsally over the ala of the sacrum, lying against bone in a groove formed by the junction of the ala with the root of the superior articular process (SAP) of the sacrum. Opposite the caudal aspect of the L5/S1 facet joint, the L5 dorsal ramus divides into a medial and a lateral branch; the medial branch hooks medially around the joint, which it supplies, and then ramifies into the multifidus muscle. The lateral branch runs caudally to communicate with the lateral branch of the S1 dorsal ramus
Structures to Keep in Mind and Possible Complications
-
Nerve root → paresthesia, sensory/motor dysfunction, sensory/motor loss
-
Disc → discitis
-
Dura → postdural puncture headache, spinal cord lesion
-
Intravascular injection, bleeding, retroperitoneal hematoma
-
Infection, epidural abscess, vertebral osteomyelitis
-
Postprocedure pain
-
Vasovagal reaction
-
Allergic reaction
Fluoroscopy Technique, Target Localization - Diagnostic Block
Sandra A. S. van den Heuvel
-
Prone position; reduce lumbar lordosis with a pillow underneath the lower abdomen
-
Anteroposterior (AP) view. Identify level and square off endplates (Fig. 16.1a–c)
-
Oblique (approximately 15°), until the joint line between the SAP and inferior articular process (IAP) opens. The C-arm can be turned less oblique (0–10°) for L5 (Fig. 16.2a–c)
-
Mark entry point on the skin, which should be at the junction of SAP and the transverse process (TP) or SAP of S1 and sacral ala (SA)
AP view of the lumbar spine. Cannulas are placed at the L3 and L4 medial branches and L5 dorsal ramus for diagnostic medial branch block. Vertebral bodies are squared off at L3–4 level. Orange = spinous process and lamina; purple = vertebral body and sacrum; yellow = transverse process; dark blue = pedicle. Complete Anatomy image (a), and native (b) and edited fluoroscopy image (c)
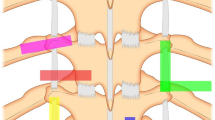
Oblique view of the lumbar spine. Vertebral bodies are squared off at L3–4 level; C-arm is obliqued 20° toward the side of interest. Needles are placed at the L3 and L4 medial branches and L5 dorsal ramus for a diagnostic medial branch block. Orange = spinous process and lamina; yellow = transverse process; dark green = superior articular process; light green = inferior articular process; dark blue = pedicle. Complete Anatomy image (a), and native (b) and edited fluoroscopy image (c)
Procedure Steps - Diagnostic Block
-
Oblique view: Advance the needle in coaxial view to touch bone at the junction of the SAP and TP (Fig. 16.2a–c)
-
Lateral view: The needle should be at the base of the SAP, dorsal to the posterior border intervertebral foramen (Fig. 16.3a–c)
-
AP view to confirm needle position: It should touch the SAP (Fig. 16.1a–c)
-
Aspiration should be negative. Contrast confirms lack of vascular uptake (Fig. 16.4)
-
Limit local anesthetic to 0.5 ml per level
Lateral view of the lumbar spine . Sacrum and ilium faded (a). Needles are placed at the L3 and L4 medial branches and L5 dorsal ramus for a diagnostic block. Dark green = superior articular process; light green = inferior articular process; red = intervertebral foramen; purple = vertebral body. Complete Anatomy image (a) and native (b) and edited (c) fluoroscopy images
Fluoroscopy Technique, Target Localization - Radiofrequency Ablation
David Vivian and Paul Verrills
L1–4 Medial Branches
-
Start as described above for diagnostic block (Figs. 16.1a–c and 16.2a–c)
-
Caudad tilt of the C-arm will enable the needle to project from a caudad approach; this is typically about 30° of caudad tilt (Fig. 16.5a–c)
L5 Dorsal Ramus
-
One may follow the exact same method as the L1–4 medial branches, bearing in mind that the oblique angle may need a slight adjustment to remove the ilium from needle trajectory
L4 medial branch radiofrequency ablation. C-arm is slightly obliqued to the ipsilateral side, then tilted caudally. Orange = spinous process and lamina; yellow = transverse process; dark green = superior articular process; dark blue = pedicle; pink = ilium. Complete Anatomy image (a), native (b) and edited fluoroscopy image (c)
OR
-
AP view of the lumbar spine
-
Caudad tilt of the C-arm will enable the needle to project from a caudad to the junction of the SAP and SA (sacral ala) of S1; this is typically about 30° of caudad tilt (Fig. 16.6a–c)
L5 dorsal ramus radiofrequency ablation. C-arm tilted caudally. Needle at the junction of the S1 SAP and SA. Orange = spinous process and lamina; yellow = transverse process; dark green = superior articular process; purple = sacrum; pink = ilium. Complete Anatomy image (a), and native (b) and edited fluoroscopy image (c)
Procedure Steps - Radiofrequency Ablation
-
Insert cannula and advance it in a coaxial view, aiming at the intended target point: the junction of the SAP and the TP (Figs. 16.5a–c and 16.6a–c)
-
Once on bone, and before the cannula advances past the cephalic aspect of the transverse process, assess the anterior position by using a lateral C-arm view (Fig. 16.7a–d)
-
True lateral views are identified when the iliopectineal lines are overlapped on lateral imaging (Figs. 16.7a, b and 16.8b)
-
Inject local anesthetic and perform lesion
-
Bipolar (Fig. 16.8a–c) or unipolar lesions can be performed; the former provides larger lesions
-
If unipolar, place the grounding pad as close to the actual lesion as possible, particularly if metal is present around the site; the closer the pad is to the lesion site, the lower the impedance
-
Try to keep the electrical pathway remote from metal; if there is metallic spinal fusion above the intended target, place the pad below the lesion so that metal is more distant (the metal acts as an electron sink)
-
-
During the lesioning, monitor the temperatures (typically 80–90 °C is required)
-
If impedance rises, check machine and leads, and consider injecting saline around the cannula tip
-
Saline can lower impedance and improve the lesion size, and it can be injected as the lesion is performed
-
Lateral view of the lumbar spine. Cannulas are placed to the L3 medial branches (a, b) and L5 dorsal ramus for RFA (c, d). The iliopectineal lines overlap, showing a true lateral image. Dark green = superior articular process; red = intervertebral foramen; yellow = transverse process, purple = vertebral body; pink = iliopectineal lines. Native (a, c) and edited (b, d) fluoroscopy image
Clinical Pearls
-
The needle is always directed cephalad and medially from a point caudad to the fluoroscopically optimized vertebra being targeted
-
Obtain a true lateral image (iliopectineal lines superimposed) to be able to assess the depth
-
Ensure that the trajectory of the needle is kept over bone as it is advanced to ensure that the spinal canal or spinal nerve is not compromised
-
Regularly use lateral, oblique, and AP views to ensure safe and accurate needle manipulation
-
In older patients, in particular, the anatomy can be difficult to assess; take care and do not perform the procedure if there is any chance of malposition
-
As the medial branches are potentially insulated from the RF lesion by the mamillo-accessory ligament, there is an added need for very accurate needle placement
Unacceptable, Potentially Harmful Needle Placement on Exam
-
Failing to check AP and lateral views
-
Rough manipulation of the needle
-
Needle compromised intraspinal space or exiting nerve root
-
Any proof of lack of understanding of lumbar spine anatomy, for example, the needle left far posterior between spinous processes and believing it is in the right place
Unacceptable, But Not Harmful Needle Placement on Exam
-
The procedure was abandoned after unsuccessful attempts, but it was clear that the examinee was cognizant of the safety aspects of the procedure, the needle did not compromise vital structures, did not reach the epidural space and there was no cord compromise
Evidence
Suggested Reading
Manchikanti L, Kaye AD, Soin A et al. Comprehensive evidence-based guidelines for facet joint interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines Facet Joint Interventions 2020 Guidelines. Pain Physician. 2020;23(3S):S1–S127.
Dreyfuss P, et al. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine (Phila Pa 1976). 2000;25:1270–7. https://www.sciencedirect.com/book/9781416037798/pain-procedures-in-clinical-practice#book-info.
Falco FJE, et al. An update of the effectiveness of therapeutic lumbar facet joint interventions. Pain Physician. 2012;15(6):E909–53.
King W, Borowcyzk J. Zygapophysial joint pain: procedures for diagnosis and treatment. In: Pain procedures in clinical practice. Elsevier Saunders; 2010. p. 357–90.
MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2013;14:639–45.
Manchikanti L, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013;16:S49–283.
Cohen SP, Bhaskar A, Bhatia A, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Regional Anesthesia & Pain Medicine:rapm-2019-101243.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
The Lumbar Medial Branch and RFA chapter was reviewed by Athmaja Thottungal; Harvey Finkelstein; Alan Berkman; Amit Gulati; Andrea M. Trescot; Milan Stojanovic; Peter S. Staats; Agnes R. Stogicza; Andre M. Mansano; Athmaja Thottungal and Raja Reddy.
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
van den Heuvel, S.A.S., Vivian, D.G., Verrills, P. (2020). Lumbar Medial Branch Block and Radiofrequency Ablation. In: Stogicza, A.R., Mansano, A.M., Trescot, A.M., Staats, P.S. (eds) Interventional Pain . Springer, Cham. https://doi.org/10.1007/978-3-030-31741-6_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-31741-6_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31740-9
Online ISBN: 978-3-030-31741-6
eBook Packages: MedicineMedicine (R0)