Abstract
In ultrasound therapies with HITU applications, the temperature reached in the tissue depends both on the properties of the tissue to be treated and on the ultrasonic parameters. Ultrasonic attenuation (α) is one such parameters since it plays a fundamental role in the thermal source term of the biothermic equation. The study addresses the behavior of α by subjecting an ex vivo muscle to continuous heating-cooling cycles (15–50 °C). Using the transmission technique of ultrasonic pulse (PU) and a controlled thermal bath, the evolution of the pulses was obtained as a function of temperature. It was observed that, for the first three cycles, the evolution of the attenuation presents a non-reversible behavior. Then, the cycle becomes reversible, but at values very different from the initial value. Disregarding this behavior in the planning of a therapeutic session will result in an over or underestimation of the temperature, and, therefore, compromising the limits of safety and in the effectiveness of the application.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The goal of ultrasonic therapies (UT) is to complement or even replace standard therapies [1]. In addition, it has evolved for new therapies such as the administration of medications through the blood-brain barrier [2]. The safety of UT and the accuracy of their treatment plans as well as their devices are crucial [3] for patient safety. A major limitation of thermal therapies is the lack of detailed temperature information available to guide therapy. Temperatures are routinely measured in an invasive manner, but only limited measurements can be made [4]. The limited number of measurements may result in less information than is necessary to produce satisfactory temperature distributions to adequately assess thermal dosimetry.
Efforts have been made to obtain objective safety criteria during treatment, for example, based on the thermal index [5], the maximum temperature allowed on the surface of the transducer [6]. However, there is a lack of standards to allow predicting the quality of the therapy, or of a single treatment session, before its execution, because there is no reliable way to calculate the doses and estimate the side effects [7]. These facts make the reproducibility of treatment sessions and the comparability of clinical studies virtually impossible [8].
The use of ultrasound to estimate the temperature is not new [9] and its accuracy has been improved successively. Methods of temperature estimation are generally divided into three categories: (1) those that analyze the changes in the thermal expansion of the tissues and the speed of sound [10], (2) those that use the acoustic attenuation coefficient [11] and (3) those that explore the change in backscattered energy in the tissue [12]. To obtain a reliable estimate of the temperature, in each stage of treatment, one must have a correct knowledge of the properties of the tissue under study. In biological tissues the absolute value of the speed of the ultrasound and its dependence on temperature are closely related to the particular composition of the tissue [13]. The stiffness of the tissue changes significantly and irreversibly after thermal ablation [14, 15] and above 60 °C the changes become irreversible due to the denaturation of collagen [16].
Although the dependence of ultrasonic tissue parameters on temperature from in vitro analysis of the characteristics of ultrasonic tissues has been widely reported [17], the analysis of these parameters has not been addressed when the tissue under study is subjected to repeated and continuous cycles of temperature change.
This study explores the changes in the ultrasonic attenuation originated in ex vivo tissue when subjected to continuous heating-cooling cycles within the temperature range of the ultrasonic therapies.
2 Methodology
2.1 Sample Preparation
Samples of bovine muscle tissue were kept submerged in 0.9% saline at room temperature. They were placed in a vacuum chamber until no air bubbles were released from the tissue, by visual inspection. This method has been successfully tested in the elimination of air inclusions in the liver tissue [18]. The attenuation measures were taken immediately after this procedure to avoid changes in attenuation [19].
The transfer of the tissue sample from the vacuum chamber to the water bath was performed submerged in degassed saline solution to minimize exposure to the air.
For the measurements of attenuation in the muscle tissue sample, the muscle fibers were oriented perpendicular to the ultrasonic beam. The presence of interfaces (fat) in the path of ultrasound is avoided.
2.2 Attenuation Measurement System
The measured attenuation coefficient was based on the transmission and reception method described in the literature [20]. Two non-focused circular immersion transducers (Harisonic I3-0108S, 1 MHz) were aligned along the central axis of the transducers. The separation between them is given by the thickness of the sample (see Fig. 1). The ultrasonic pulse is generated from a generator-receiver (FG) (Olympus NDT, MA, USA; 5073PR, rise time <2 ns). The pulse width is <0.2 μs, with repetition frequency of 1 kHz providing an adequate temporal resolution. The time base of the oscilloscope is synchronized with the FG trigger (Tektronix, INC, USA, TDS-2024B). The transducers with the sample in the middle were submerged in a degassed saline bath.
A heat exchanger was submerged in the bath to vary the tissue temperature. The exchanger is connected to a thermal bath with adjustable temperature control, the temperature range used is 15–50 °C with a step of 0.5 °C. A Type-J thermocouple was inserted in the tissue away from the ultrasonic path and another in the saline bath. A high-speed multiplexer (NI, National Instruments, NI9213) was used to record temperatures. When the bath and sample temperatures differ by ≤0.05 °C, the acquisition is proceeded. Next, control of the thermal bath is increased (decreased) by 1 °C in the case of heating (cooling) at a rate of 0.1 °C per min. The oscilloscope, multiplexer and thermal bath control are all commanded by a program developed in MatLab® platform.
Finally, the data was stored on a computer. The signal that passes through the sample is captured, and based on the decrease in the intensity of the received signal, the behavior of the attenuation as a function of temperature is analyzed. Care was taken to ensure that the attenuation of the ultrasonic pulse was not related to air bubbles, tissue interfaces (fat) or other unwanted inclusions within the ultrasonic path.
The behavior of the attenuation with temperature is evidenced when analyzing the evolution of the amplitude spectrum.
3 Results
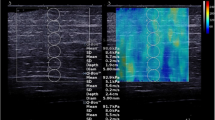
Figure 2 shows the time evolution of the ultrasonic pulses (US) as a function of the temperature for the heating stage of the second cycle. As the sample of muscle tissue increases (decreases) its temperature the US presents a temporary shift and change in amplitude.
To analyze the evolution of the attenuation, the behavior of the maximum of the amplitude spectrum is followed (Fig. 3).
Figures 4, 5, 6 and 7 show the evolution of the attenuation for the four heating-cooling cycles. The curve in red corresponds to the heating stage and in the blue the cooling stage.
4 Discussion
It can be seen that the attenuation of the skeletal muscle tissue depends on the temperature in a non-reversible manner for the first three heating-cooling cycles. Such behavior is not present for the fourth cycle. The non-cyclic behavior of the ultrasonic attenuation, for the studied temperature range, is not expected in that temperature range [15, 16]. One possible explanation is that there is a cumulative effect of temperature on the structures and proteins that compose the tissue, despite not achieving high temperatures. This effect is intrinsically linked to the denaturation of proteins, as well as the behavior of elastin associated with the phenomenon called Reverse Transition with Temperature (ITT). It should be noted that the possible denaturation takes place in the range 40–50 °C. The behavior of the attenuation becomes reversible for the fourth cycle can be explained by the total denaturation of proteins that undergo lysis at temperatures lower than 50 °C. A fifth cycle was started, but which was discarded due to a change in the orientation of the muscle fibers and ultrasonic beam during the heating process.
The range of therapeutic applications in humans is 37–45 °C. US attenuation (absorption and scattering) is a fundamental parameter in the determination of temperature [21], therefore, it has a direct effect on the thermal dose, as well as on the planning of the therapy. This fact indicates that the “new” properties of the tissue must be taken into consideration in each treatment session planning with ultrasound. This care should be considered especially in high intensity applications. It can be observed that, once a HITU application has been made, the new value of the attenuation must be estimated not to commit an over (or under) exposure of the patient.
5 Conclusion
The changing of ultrasonic attenuation of the tissue with repeated application of heating-cooling cycles was evidenced despite not reaching temperatures that generate denaturation of the collagen.
Experimentally, there was a cumulative effect of temperature on the protein structures, which caused a non-reversible behavior. Apparently, once the total denaturation of proteins is achieved, the attenuation behavior becomes reversible. Such behavior should be considered in the planning of therapeutic sessions so to avoid over or underestimation of the temperature, and thus, keeping the limits of safety and effectiveness of the application.
More experiences with other types of biological tissues are necessary to confirm and find a relationship between the attenuation-temperature and amount of heating-cooling cycle applied.
References
ter Haar, G.: Therapeutic ultrasound. Eur. J. Ultrasound 9(1), 3–9 (1999)
Aryal, M., Arvanitis, C., Alexander, P., McDannold, N.: Ultrasound-mediated blood–brain barrier disruption for targeted drug delivery in the central nervous system. Adv. Drug Deliv. Rev. 72, 94–109 (2014)
Izadifar, Z., Babyn, P., Chapman, D.: Applications and safety of therapeutic ultrasound: current trends and future potential. Clin. Res. Open Access 3(1) (2017)
Arthur, R., Straube, W., Trobaughi, J., Moros, E.: Non-invasive estimation of hyperthermia temperatures with ultrasound. Int. J. Hyperthermia 21(6), 589–600 (2005)
IEC 62359: Ultrasonics–Field characterization–Test methods for the determination of thermal and mechanical indices related to medical diagnostic ultrasonic fields, 2nd edn. International Electrotechnical Commission, Geneva (2010)
IEC 60601-2-37: Medical electrical equipment : Particular requirements for the basic safety and essential performance of ultrasonic medical diagnostic and monitoring equipment, 1st edn. International Electrotechnical Commission, Geneva (2015)
Shaw, A., Martin, E., Haller, J., ter Haar, G.: Equipment, measurement and dose—a survey for therapeutic ultrasound. J. Ther. Ultrasound 4(1), 1–7 (2016)
ter Haar, G., Shaw, A., Pye, S., Ward, B., Bottomley, F., Nolan, R., Coady, A.: Guidance on reporting ultrasound exposure conditions for bio-effects studies. Ultrasound Med. Biol. 37(2), 177–183 (2011)
Seip, R., VanBaren, P., Cain, P., Ebbini, E.: Noninvasive real-time multipoint temperature control for ultrasound phased array treatments. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 43(6), 1063–1073 (1996)
Seip, R., Ebbini, E.: Noninvasive estimation of tissue temperature response to heating fields using diagnostic ultrasound. IEEE Trans. Biomed. Eng. 42(8), 828–839 (1995)
Bamber, J., Hill, C.: Ultrasonic attenuation and propagation speed in mammalian tissues as a function of temperature. Ultrasound Med. Biol. 5(2), 149–157 (1979)
Teixeira, C., Pastrana-Chalco, M., Simões, R., Pedrosa, A., von Kruger, M., Alvarenga, A.V., Fontes-Pereira, A., Pereira, W.: On the feasibility of ultrasound imaging enrichment by medium temperature changes. Ultrason. Imaging 41(1), 17–34 (2019)
Simon, C., VanBaren, P., Ebbini, E.: Two-dimensional temperature estimation using diagnostic ultrasound. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 45(4), 1088–1099 (1998)
Benech, N., Negreira, C.: Monitoring heat-induced changes in soft tissues with 1D transient elastography. Phys. Med. Biol. 55(6), 1753–1765 (2010)
Sapin, E., Gennisson, J., Pernot, M., Fink, M., Tanter, M.: Temperature dependence of the shear modulus of soft tissues assessed by ultrasound. Phys. Med. Biol. 55(6), 1701–1718 (2010)
Wu, T., Felmlee, J., Greenleaf, J., Riederer, S., Ehman, R.: Assessment of thermal tissue ablation with MR elastography. Magn. Reson. Med. 45(1), 80–87 (2001)
Shore, D., Miles, C.: Attenuation of ultrasound in homogenates of bovine skeletal muscle and other tissues. Ultrasonics 26, 218–222 (1988)
Bamber, J., Nassiri, D.: Effect of gaseous inclusions on the frequency dependence of ultrasonic attenuation in liver. Ultrasound Med. Biol. 11, 293–298 (1985)
Frizzell, L., Cartensen, E., Davis, D.: Ultrasonic absorption in liver tissue. J. Acoust. Soc. Am. 65, 1309–1312 (1979)
Kossoff, G., Kelly-Fry, E., Jellins, J.: Average velocity of ultrasound in the human female breast. J. Acoust. Soc. Am. 53, 1730–1736 (1973)
Cortela, G., Pereira, W., Negreira, C.: Ex vivo determined experimental correction factor for the ultrasonic source term in the bioheat equation. Ultrasonics 82, 72–78 (2017)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this paper
Cite this paper
Cortela, G., Negreira, C., Pereira, W.C.A. (2020). Effect of Continuous Application of Heating-Cooling Cycles on Ultrasonic Attenuation of Muscle Tissue. In: Henriques, J., Neves, N., de Carvalho, P. (eds) XV Mediterranean Conference on Medical and Biological Engineering and Computing – MEDICON 2019. MEDICON 2019. IFMBE Proceedings, vol 76. Springer, Cham. https://doi.org/10.1007/978-3-030-31635-8_160
Download citation
DOI: https://doi.org/10.1007/978-3-030-31635-8_160
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31634-1
Online ISBN: 978-3-030-31635-8
eBook Packages: EngineeringEngineering (R0)