Abstract
Pulmonary hypertension (PH) is a heterogeneous disorder that encompasses multiple different etiologies with complex pathobiology. The current classification of PH is based primarily on clinical characteristics and hemodynamics. Accurate characterization of PH using advanced hemodynamic analyses, exercise testing, improved imaging techniques, and innovative biomarkers provide the opportunity to define novel phenotypes. These approaches are paving the way to a personalized medicine approach in the evaluation and management of patients with PH.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pulmonary hypertension
- Exercise testing
- Metabolomics
- Cardiopulmonary imaging
- Cardiac MRI
- Computed tomography or CT chest
Introduction
Pulmonary hypertension (PH) is defined by an elevated mean pulmonary arterial pressure of greater than or equal to 25 mmHg at rest as measured by pulmonary arterial catheterization. Importantly, this hemodynamic criterion incorporates a heterogeneous group of diseases characterized by distinct etiologies, pathophysiologies, and management strategies. Currently, patients diagnosed with PH are subclassified into one of five World Health Organization (WHO) groups on the basis of hemodynamic measurements and medical comorbidities (Table 16.1). Regardless of the underlying etiology, elevated pulmonary artery pressures confer an increased risk of morbidity and mortality [1].
WHO Group 1 pulmonary arterial hypertension (PAH) is defined clinically by an elevated pulmonary vascular resistance and pathologically as a primary pulmonary vasculopathy resulting from a number of complex pathophysiologic processes (Table 16.1). Despite recent therapeutic advances, the prognosis of PAH remains poor [2] which likely reflects, in part, delayed detection of the disease [3] and, in part, the heterogeneity of the underlying pathophysiology. Indeed, the current clinical classification scheme places all PAH patients together into the same treatment algorithm whether the cause is heritable, toxin-induced, or associated with connective tissue disease (Table 16.1). While the notion of precision medicine in pulmonary vascular disease dates to the recognition of the value of pulmonary vasodilator testing in selection of patients for calcium channel blocker therapy, the future diagnosis and management of patients with pulmonary vascular disease will rely on a more sophisticated diagnostic and treatment paradigms based on each patient’s disease phenotype. This chapter reviews the evolving approaches to sub-phenotype patients with PH based on clinical, imaging, and molecular signatures that will form the basis of personalized clinical classification schemes and management strategies.
Resting Hemodynamic Phenotyping
All patients suspected of having PH should be referred for pulmonary arterial catheterization for diagnosis. Pulmonary arterial catheterization allows direct measurements of pulmonary artery pressures from which the mean pulmonary artery pressure (mPAP) , left atrial filling pressures by balloon occlusion of distal pulmonary arteries (pulmonary artery wedge pressure [PAWP] ), and cardiac output (CO) by thermodilution or the Fick equation are determined. From these parameters, the pulmonary vascular resistance (PVR) may be calculated according to the ohmic Starling resistor model [4]:
Pulmonary arterial hypertension (PAH) is defined by both an increased mPAP and an increased PVR >3 Wood units. Increased PVR is a consequence of proliferative remodeling of the small pulmonary arterial resistance vessels [5]. This remodeling process involves all three layers of the vessel wall (intima, media, and adventitia) and is the consequence of cellular hypertrophy, hyperplasia, inflammation, abnormal cellular metabolism, defects in cellular differentiation and apoptosis, excessive migration, and accumulation of extracellular matrix components [6]. This pro-proliferative and anti-apoptotic phenotype reduces vessel distensibility and causes luminal narrowing, impairing the ability of pulmonary vasculature to accommodate increases in pulmonary blood flow.
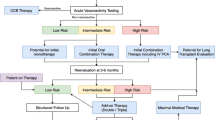
Once the diagnosis of PAH is made during pulmonary arterial catheterization study, all patients undergo vasoreactivity testing. This involves the acute administration of a short-acting pulmonary arterial vasodilator such as inhaled nitric oxide or intravenous adenosine followed by repeat measurement of the hemodynamic response. Patients are considered vasoreactive if, following acute vasodilator testing, there is a reduction in mPAP by 10 mmHg to a value less than 40 mmHg with an increase or no change in cardiac output [7]. The main purpose of vasoreactivity testing is to identify a phenotype of PAH patients who are candidates for calcium channel blocker therapy. The use of calcium channel blockers in PAH is associated with a significant survival benefit compared to patients who are not vasoreactive [8].
The diagnosis of PH due to left heart disease (WHO Group 2) is defined by both an increased mPAP greater than or equal to 25 mmHg and a PAWP greater than or equal to 15 mmHg. Hemodynamic phenotyping in PH due to left heart disease is challenging because of the uncertainty surrounding the best measure to differentiate between isolated retrograde transmission of elevated PAWP, known as passive or isolated post-capillary PH (IpC-PH), and the concomitant development of pre-capillary pulmonary vascular disease, known as combined pre- and post-capillary PH (CpC-PH) [9,10,11].
Why is the distinction between Ipc-PH and Cpc-PH important? One of the major determinants of the poor outcome observed in patients with PH due to left heart disease is the presence of RV dysfunction [12]. Patients with CpC-PH are more likely to have a significantly higher RV afterload that is comparable to patients with idiopathic PAH [13] and have worse RV function compared to their IpC-PH counterparts [14]. Therefore, the ability to distinctly phenotype and ascertain the relative contributions of PAWP (or pulsatile RV afterload) and PVR (or resistive RV afterload) is an intriguing prospect that would allow for dedicated interventions directed at either the left heart or the remodeled pre-capillary pulmonary vasculature. However, the use of PAH-specific therapies in PH due to left heart disease thus far has yielded mixed results [15,16,17,18].
There have been a number of hemodynamic parameters implemented to help distinguish between IpC-PH and CpC-PH . These include the trans-pulmonary gradient (i.e., TPG = mean pulmonary artery pressure – PAWP) and the diastolic pressure gradient (i.e., DPG = diastolic pulmonary artery pressure – PAWP). In the setting of IpC-PH, the elevated PAWP can spuriously increase the TPG without any coexistent pulmonary vascular remodeling or vasoconstriction [19]. The DPG, therefore, may be more preferable as it is less sensitive to changes in PA compliance, stroke volume, and PAWP [19]. However, studies utilizing DPG for a diagnosis of CpC-PH have yielded mixed prognostic results. These discrepancies can be explained by inaccuracies in the measurement of diastolic pulmonary arterial pressure owing to motion artifacts, the influence of large v-waves on DPG values, and insufficient or excessive flushing of the fluid-filled catheter system [19, 20]. Previous studies have shown that PVR strongly predicts outcomes in PH due to left heart disease [21, 22]. Accordingly, recent guidelines have reincorporated PVR into the CpC-PH definition . In the latest iteration of the European Society of Cardiology / European Respiratory Society guidelines, CpC-PH was defined as DPG ≥7 mmHg, mPAP ≥25 mmHg, and PVR >3 Wood units (WU) [10].
Exercise Hemodynamic Phenotyping
Exercise intolerance is one of the earliest manifestations of PAH, and reduced exercise capacity has important implications for prognosis and mortality in PAH [23]. Since the essential stress of exercise imposed on the pulmonary circulation is an increase in pulmonary blood flow, provocative testing such as the cardiopulmonary exercise test (CPET) is able to demonstrate early [24,25,26,27,28] and reproducible [29, 30] abnormalities seen in PH. Additionally, factors that contribute to exercise intolerance in PAH are not simply confined to the central cardiopulmonary system and include peripheral factors such as impaired mitochondrial and respiratory muscle function (Fig. 16.1). In fact, pharmacotherapies such as dicholoroacetate [31] and ranolazine [32] that restitute mitochondrial oxidative metabolism have shown promise in the management of PAH.
CPET provides a comprehensive and dynamic assessment, integrating the cardiovascular, pulmonary, muscular, and cellular oxidative metabolism systems during exercise . The two modalities of CPET are noninvasive (niCPET) and invasive CPET (iCPET). The former is equipped with continuous 12-lead electrocardiogram, cuff blood pressure monitoring, breath-by-breath gas exchange assessment, and pulse oximetry while the latter also includes systemic and pulmonary arterial catheters for continuous systemic and pulmonary arterial, and right ventricular (RV) pressure measurements as well as intermittent measurement of PAWP [33]. Combining exercise hemodynamics with CPET is gaining prominence, particularly for its ability to potentially identify with early pulmonary vascular disease such as exercise PH.
Exercise PH is increasingly being recognized as an early phase of PH that is a potential target for PAH-specific therapy [34,35,36] (Table 16.2). Although further studies are needed to refine its diagnosis, exercise PH has been shown to be a major risk factor for the development of PAH in patients with systemic sclerosis [27, 28] and in healthy carriers of the bone morphogenetic receptor-2 (BMPR2) mutation [38]. In addition, patients with systemic sclerosis and exercise PH have a similarly reduced transplant-free survival compared to patients with established PAH [26].
Exercise PH is typically diagnosed in patients with exertional dyspnea or exercise intolerance without obvious underlying pulmonary or cardiac etiology. In patients with exercise PH, the data gathered from iCPET demonstrates an inverse relationship between the slope of mPAP-CO with a depressed maximal O2 uptake, suggesting impaired RV adaptation to increasing afterload with resulting reduced aerobic exercise capacity [39]. Recently, cumulative evidence from invasive as well as noninvasive studies have shown that the slope of linearized mPAP–CO relationship should not exceed 3 mmHg.L−1.min−1. Hence, an mPAP/CO slope of >3 mmHg.L−1.min−1 may be used to define exercise PH (Fig. 16.2). Similarly, a PAWP/CO slope of 2 mmHg/L/min can be used to define the potential contribution from left-sided heart disease [40, 41].
Relationship between exercise mean pulmonary artery pressure (mPAP) and cardiac output (CO). Individual data points represent mPAP and CO reached at maximal exercise stratified by subjects with pulmonary vascular disease (PVD), left heart disease (LHD), control subjects and historical healthy volunteers. It can be seen that the total pulmonary resistance (TPR) line with a slope of 3 Wood units (WU) differentiated the diseased (PVD and LHD) and non-diseased groups (controls and historical volunteers). (Reproduced with permission of the © ERS 2019: Herve et al. [103], Published 31 August 2015)
CPET can also be used to extract individualized parameters related to pulmonary vascular remodeling. Using CPET, the ability of the pulmonary vasculature to distend and accommodate the ejected RV stroke volume can be quantified by estimating the resistive vessel distensibility coefficient, α [42]. α or pulmonary distensibility is an intrinsic mechanical property of the vasculature and is defined as the percent change in vessel diameter per unit mmHg increase in distending pressure. By including different pressure and flow measurements during exercise, this assessment of pulmonary vascular distensibility accounts for the significant variation in pulmonary pressures and flow encountered during exercise [42]:
Invasive studies and noninvasive echocardiography have shown that the normal value of α is between 1% and 2% per mmHg [39]. Reduced vessel distensibility has been demonstrated in patients with early PH (i.e., those with normal resting pulmonary hemodynamics who later evolve into resting PAH or have lung biopsy consistent with pulmonary vascular disease) [43] and in healthy carriers of the BMPR2 mutation [44].
Another use of CPET is to quantify the degree of RV dysfunction which is closely linked to survival in patients with PH [45]. Exercise hemodynamics allows for dynamic assessment of RV contractile function (termed Ees, end-systolic elastance) to its afterload (termed Ea, arterial elastance). The matching of RV contractility (Ees) and RV afterload (Ea) describes RV–PA coupling, and a normal RV Ees to Ea ratio (Ees/Ea) of between 1.5 and 2.0 allows for optimal RV functioning at minimal energy cost while a value of <0.8 is associated with RV failure [46]. RV-PA coupling can be determined using single-beat pressure waveform analysis or multi-beat pressure volume loop analysis (Figs. 16.3 and 16.4).
Single-beat methods to estimate right ventricle–pulmonary artery (RV-PA) coupling . In the (a) volumetric method and (b) pressure method, pulmonary arterial elastance (Ea) is calculated from the ratio of RV end-systolic pressure (RVESP) to stroke volume (SV). The mean PA pressure can be used as surrogates for the RV-ESP. End-systolic elastance (Ees) in the volume method is estimated by the ratio of RV-ESP to end-systolic volume. The Ees/Ea is, therefore, simplified as SV/ESV. In the pressure method, Pmax was estimated by nonlinear extrapolation of early and late isovolumic portions of an RV pressure curve from the point of maximum (dp/dt max) and minimum (dp/dt min) pressure derivation. End-systolic elastance is then determined by a tangent from Pmax to the RV-ESP point. Ees/Ea in the pressure method is then determined by the ratio of (Pmax-RVESP) divided by SV or (Pmax/ESP – 1)
Multi-beat method to estimate right ventricle–pulmonary artery (RV-PA) coupling . End-systolic elastance (Ees) is determined by a tangent fitted on the end-systolic portions of a series of pressure–volume loops produced by alteration in venous return or preload. Pulmonary arterial elastance (Ea) is calculated from the ratio of the RV-end systolic pressure to stroke volume. RV-PA coupling is then determined from the ratio of Ees to Ea (Ees/Ea)
The initial response of the RV to an increased afterload is to increase its contractility (Ees) to match the increasing afterload (Ea). When the RV no longer is able to augment its contractility in the face of increasing afterload, RV–PA uncoupling ensues. The RV then relies on volumetric adaptation (i.e., Frank Starling’s mechanism ) to sustain its flow output in response to increasing metabolic demand leading to RV dilatation and associated poor prognosis [47, 48].
Exercise hemodynamics may play an important role in identifying early pulmonary vascular disease in subjects who are at risk of overt PAH due to established risk factors such as systemic sclerosis or BMPR2 mutation. It can be used to examine the relative contribution of pulmonary vascular remodeling and left-sided heart disease to exercise impairment. Additionally, it allows to identify maladaptive RV phenotype response during exercise in patients with established PAH and exercise PH . This may prove useful in harnessing therapies aimed at improving RV contractility and potentially serve as endpoints for clinical prevention trials.
Phenotyping by Cardiopulmonary Imaging
Imaging can be used to quantify structural and functional changes to the pulmonary circulation allowing for detection, classification, and monitoring of PH. Thus, significant efforts have focused on utilizing imaging in defining individualized parameters of PH that have clinical utility.
Although the initial insult in PAH implicates the pulmonary vasculature, the functional state, exercise capacity, and survival of patients with PAH is closely linked to RV function [45]. While right heart catheterization provides important information about the hemodynamic impact of PH and the ability of the heart to provide cardiac output in that context, RV imaging using echocardiogram and cMRI provide significant information about the structure and function of the heart. Echocardiography remains the most important tool for screening patients for PH and monitoring RV function in no small part because of its relative availability, owing mainly to low cost of deployment [49]. Echocardiography can be used to estimate RV systolic pressures and evaluate RV systolic function [50]. It additionally provides information about other structural cardiac issues such as valvular dysfunction and left-sided heart failure, all of which have a very important impact on RV function. Beyond these well-established methods , current development is focusing on 3D reconstruction of RV geometry and estimation of the strain on the RV [51, 52], which can be combined together to aid with prognostication [53].
Cardiac magnetic resonance imaging (cMRI) provides a versatile set of tools with which many structural and functional parameters of the RV and its interactions with the proximal pulmonary artery can be measured [54]. As a noninvasive modality, cMRI is an attractive tool for monitoring patients with PAH. Standard cMRI imaging provides accurate information about changes in RV mass and volumes, RV function, as well as RV/LV interactions [49, 51, 54]. cMRI measures of ventricular volume and mass have been shown to be reproducible and superior to standard echocardiography [55]. Furthermore, specific techniques applied in the context of cMRI can provide information about cardiac mechanics and cardiac tissue remodeling. For example, the presence of late gadolinium enhancement can be used to assess degree of RV fibrosis [56] while phase-contrast imaging can be used to study cardiac output and assess PA stiffness and pulsatility [55,56,58]. Additionally, fluid dynamics models can utilize imaging data to study the impact of the remodeling of the proximal pulmonary circulation on vorticity of flow [59].
Computed tomography (CT) imaging has long been used as a screening tool for PH. Dilation of the pulmonary artery has been appreciated as a sign of pulmonary vascular disease [60]. Additionally, measurements of the size and dimensions of the chambers of the heart from CT imaging have potential utility in screening for PH [61] and distinguishing subtypes of PH [61,62,64]. Remodeling and loss of distal vascular volume have been quantified as markers of disease using CT imaging in multiple etiologies of PH [64,65,66,68]. Furthermore, changes in intraparenchymal blood vessel volumes have been noted with interventions [69]. Given the ubiquity of CT imaging in most patients with shortness of breath, as well as smokers, derived predictive models for PH are a promising tool for screening and evaluating patients prior to invasive measures [70].
Perfusion, which conceptually represents the flow of blood through the lung microvasculature, has also been the subject of great interest in PH given that the extent and spatial heterogeneity may provide insight into disease stage and phenotype. Nuclear imaging has been used to assess perfusion patterns in PH [70,71,73]. For example, utilizing 3′-deoxy-3′-[18F]-fluorothymidine positron emission tomography (18FLT-PET) imaging technique allows for the identification of a hyperproliferative PH phenotype. Unlike 2-deoxy-2-[18F]-fluoro-D-glucose (18F-FDG), which reports both inflammation and cellular proliferation, 18FLT serves primarily as a marker of cell proliferation and can be used as a direct measure of pulmonary endothelial cell growth and, therefore, can be used to assess disease activity directly. In fact, treatment with anti-proliferative agents such as dichloroacetate and the tyrosine kinase inhibitor imatinib has been shown to attenuate 18FLT uptake on PET imaging [74].
While MRI often lacks the spatial resolution of CT scan in the lung parenchyma, functional data and the ability to distinguish between materials permit spatial quantification of perfusion. These properties have been used to study perfusion in chronic thromboembolic pulmonary hypertension (CTEPH) [75] as well as in chronic obstructive pulmonary disease (COPD) [76]. Dual-energy computed tomography (DECT) utilizes multiple X-ray sources to help quantify molecular density without significant exposure to additional radiation. The spatial density of iodine tracer can then be derived from DECT, giving a high-resolution spatial map related to perfusion. This has been deployed largely in the study of CTEPH [77, 78] and can be used to study impact of intervention [71]. Recent studies have also evaluated its use in the detection of parenchymal perfusion in PAH [79].
In summary, imaging methods have been well established for individualized diagnosis, subtyping, and prognostication in pulmonary hypertension. Improved resolutions, image processing, and quantification algorithms along with development of new methods of marking the site of disease continue to expand the initial role of each imaging into better understanding of the entirety of the pulmonary circulation.
Molecular Phenotyping
Genetics
A “familial tendency” for the development of PAH was first suggested in 1954 [80] and, subsequently, mutations in the gene encoding BMPR2, a member of the transforming growth factor β (TGF-β) family of receptors, were linked to several families with heritable PAH in 2000 [81, 82]. Approximately 70% of patients with familial PAH carry mutations in BMPR2, which confer only a 20% lifetime risk for the development of the disease (14% for males and 42% for females). Remarkably, up to 25% of patients with non-heritable PAH also carry somatic mutations in BMPR2 [83]. Since the identification of BMPR2 mutations, approximately 20 other genes have been implicated in the development of PAH, including several additional members of the BMP/TGF receptor signaling family (BMPR2, ACVRL1, CAV1, ENG, SMAD9) [84]. More recently, autosomal recessive inheritance of EIF2AK4 mutations encoding for eukaryotic translation initiation factor 2 alpha kinase 4 predisposes to pulmonary veno-occlusive disease (PVOD) / pulmonary capillary hemangiomatosis (PCH) [85].
PAH patients with BMPR2 mutations develop the disease approximately 7–10 years earlier than noncarriers, have more severe hemodynamic compromise at time of diagnosis, and are less likely to respond to calcium channel blocker therapy [86]. Furthermore, in patients with idiopathic, anorexigen-associated, and heritable PAH , the presence of BMPR2 mutation is associated with increased risk of death or lung transplantation [87]. In contrast to BMPR2 mutation carriers, patients with ALK1 mutations tend to be younger and have less severe hemodynamic changes at time of diagnosis. However, ALK1 mutations are associated with poorer survival compared to noncarriers despite receiving similar treatment [88].
In the future, genetic testing in PAH may play an important role in guiding a phenotypic management strategy. In patients with heritable and idiopathic PAH, genetic testing allows for early detection of a progressive disease phenotype . This would allow for early implementation of specific pharmacotherapies, which has been shown to improve clinical outcomes and prevent deterioration in patients with PAH [88,89,91]. For example, low-dose tacrolimus, a potent BMPR2 activator has been shown to reverse experimental PAH [92] and improve clinical and functional outcomes in a small cohort of PAH patients with advanced disease [93]. In a Phase 2a safety and tolerability trial, tacrolimus was shown to be well tolerated. Although the trial was under-powered for outcomes assessment, some patients demonstrated marked improvement in functional capacity as measured by 6-minute walk distance. Importantly, those patients with improved functional capacity tended to have larger increases in leukocyte BMPR2 expression in response to tacrolimus [94]. This suggests that tacrolimus therapy may be tailored to patient subsets based on the recruitment of BMPR2 signaling.
Genetic testing also allows to distinguish PVOD/PCH from PAH in patients with pre-capillary pulmonary vascular disease, a distinction that is challenging given the similarities in clinical and hemodynamic presentation between these two diseases. Patients with PVOD/PCH have a poor prognosis compared to those patients with PAH, respond poorly to PAH-specific therapies, and lung transplantation is the only curative treatment. Early diagnosis by genetic testing allows timely referral for patients with PVOD/PCH [95] for lung transplant evaluation.
Omics
The advent of omics-based technologies has provided a means to measure tens of thousands of parameters that can be utilized to provide a molecular signature of disease. While most omics studies in PAH have focused on identifying novel features of disease pathobiology or characterizing patients at-risk for developing the disease [96], investigators have recently begun to apply these technologies to address important clinical questions related to outcomes. For example, whole-exome sequencing of PAH patients with and without vasodilator response identified enrichment of vascular smooth muscle cell contraction pathways in vasodilator-responsive patients [97]. Similarly, a single-nucleotide polymorphism (SNP) in the G protein γ subunit 2 gene, GNG2, was associated with functional improvement among patients treated with an endothelin receptor antagonist [98]. A recent trial of dichloroacetate in PAH demonstrated that a lack of clinical response to the drug was associated with functional variants of SIRT3 and UCP2 [31]. In addition to providing meaningful pathobiological insights, these three studies demonstrate the value of genomic approaches to subclassifying PAH patients based on responsiveness to specific therapies. While genetic testing is unlikely to supplant clinical vasodilator testing, once prospectively validated, it may be very helpful to tailor current medical therapy or guide enrollment in clinical trials of novel agents.
In addition to genomics, proteomic and metabolomic approaches have been employed to identify circulating biomarkers to aid in the diagnosis and prognosis of patients with PAH. Using an aptamer-based assay of 1129 plasma proteins, Rhodes and colleagues identified a panel of nine circulating proteins that identifies PAH patients with a high risk of mortality, independent of existing clinical assessments [99]. Similarly, iTRAQ proteomics identified decreases in plasma carbamoyl-phosphate synthetase I and complement factor H-related protein associated with PAH in patients with congenital heart disease [100]. Plasma metabolomics has also identified circulating small molecules that distinguish PAH patients from healthy subjects and prognosticate outcomes [101]. At the present moment, these findings may have more impact by directing further investigation of novel disease mechanisms rather than guiding clinical management of PAH patients; however, as the therapeutic armamentarium increases in size, these approaches will become invaluable for customizing treatment.
Future Directions
As with many areas of medicine, the foundations are currently being poured for the implementation of sophisticated clinical, imaging, and molecular phenotyping of patients with PAH. Two limitations of the studies described above, however, are the relatively small sample sizes studied and the incorporation of relatively limited clinical data. Moreover, how these disparate datasets can be meaningfully synthesized is a critical issue for leveraging their full potential. These areas may be addressed by the ongoing Redefining Pulmonary Hypertension through Pulmonary Vascular Disease Phenomics (PVDomics) sponsored by the National Heart, Lung, and Blood Institute of the National Institutes of Health [102]. This clinical trial seeks to enroll 1500 incident cases of PH who undergo a battery of diagnostic testing, including pulmonary artery catheterization, polysomnography, pulmonary function tests, exercise testing, echocardiography, cMRI, lung imaging, ventilation/perfusion scanning, and plasma omic profiling (genome, transcriptome, proteome, and metabolome), the results of which are linked to clinical parameters such as medical history, exam, vital signs, and quality-of-life survey results. The goal of this program is to use all of these parameters to define new subclassifications of PH patients, leveraging the tools of systems biology and network medicine to facilitate earlier diagnosis, more targeted at-risk screening, and personalized approaches for intervention. Certainly, the field has come a long way since its first foray into personalized medicine with pulmonary vasodilator testing with many exciting new discoveries on the horizon.
References
Maron BA, Hess E, Maddox TM, Opotowsky AR, Tedford RJ, Lahm T, et al. Association of borderline pulmonary hypertension with mortality and hospitalization in a large patient cohort: insights from the veterans affairs clinical assessment, reporting, and tracking program. Circulation. 2016;133(13):1240–8.
Benza RL, Miller DP, Barst RJ, Badesch DB, Frost AE, McGoon MD. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the REVEAL Registry. Chest. 2012;142(2):448–56.
Badesch DB, Raskob GE, Elliott CG, Krichman AM, Farber HW, Frost AE, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest. 2010;137(2):376–87.
Singh I, Ma KC, Berlin DA. Pathophysiology of pulmonary hypertension in chronic parenchymal lung disease. Am J Med. 2016;129(4):366–71.
Bloodworth NC, West JD, Merryman WD. Microvessel mechanobiology in pulmonary arterial hypertension: cause and effect. Hypertension. 2015;65(3):483–9.
Guignabert C, Tu L, Le Hiress M, Ricard N, Sattler C, Seferian A, et al. Pathogenesis of pulmonary arterial hypertension: lessons from cancer. Eur Respir Rev. 2013;22(130):543–51.
McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on expert consensus documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009;53(17):1573–619.
Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med. 1992;327(2):76–81.
Vachiery JL, Adir Y, Barbera JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62(25 Suppl):D100–8.
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Kardiol Pol. 2015;73(12):1127–206.
Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiery JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37(12):942–54.
Gorter TM, Hoendermis ES, van Veldhuisen DJ, Voors AA, Lam CS, Geelhoed B, et al. Right ventricular dysfunction in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail. 2016;18(12):1472–87.
Gerges C, Gerges M, Fesler P, Pistritto AM, Konowitz NP, Jakowitsch J, et al. In-depth haemodynamic phenotyping of pulmonary hypertension due to left heart disease. Eur Respir J. 2018;51(5):1800067.
Gerges M, Gerges C, Pistritto AM, Lang MB, Trip P, Jakowitsch J, et al. Pulmonary hypertension in heart failure. Epidemiology, right ventricular function, and survival. Am J Respir Crit Care Med. 2015;192(10):1234–46.
Guazzi M, Vicenzi M, Arena R, Guazzi MD. Pulmonary hypertension in heart failure with preserved ejection fraction: a target of phosphodiesterase-5 inhibition in a 1-year study. Circulation. 2011;124(2):164–74.
Lewis GD, Lachmann J, Camuso J, Lepore JJ, Shin J, Martinovic ME, et al. Sildenafil improves exercise hemodynamics and oxygen uptake in patients with systolic heart failure. Circulation. 2007;115(1):59–66.
Hussain I, Mohammed SF, Forfia PR, Lewis GD, Borlaug BA, Gallup DS, et al. Impaired right ventricular-pulmonary arterial coupling and effect of sildenafil in heart failure with preserved ejection fraction: an ancillary analysis from the phosphodiesterase-5 inhibition to improve clinical status and exercise capacity in diastolic heart failure (RELAX) trial. Circ Heart Fail. 2016;9(4):e002729.
Vachiery JL, Delcroix M, Al-Hiti H, Efficace M, Hutyra M, Lack G, et al. Macitentan in pulmonary hypertension due to left ventricular dysfunction. Eur Respir J. 2018;51(2):1701886.
Naeije R, Vachiery JL, Yerly P, Vanderpool R. The transpulmonary pressure gradient for the diagnosis of pulmonary vascular disease. Eur Respir J. 2013;41(1):217–23.
Tampakakis E, Tedford RJ. Balancing the positives and negatives of the diastolic pulmonary gradient. Eur J Heart Fail. 2017;19(1):98–100.
Khush KK, Tasissa G, Butler J, McGlothlin D, De Marco T, Investigators E. Effect of pulmonary hypertension on clinical outcomes in advanced heart failure: analysis of the evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness (ESCAPE) database. Am Heart J. 2009;157(6):1026–34.
Aronson D, Eitan A, Dragu R, Burger AJ. Relationship between reactive pulmonary hypertension and mortality in patients with acute decompensated heart failure. Circ Heart Fail. 2011;4(5):644–50.
Weatherald J, Farina S, Bruno N, Laveneziana P. Cardiopulmonary exercise testing in pulmonary hypertension. Ann Am Thorac Soc. 2017;14(Supplement_1):S84–92.
Tolle JJ, Waxman AB, Van Horn TL, Pappagianopoulos PP, Systrom DM. Exercise-induced pulmonary arterial hypertension. Circulation. 2008;118(21):2183–9.
Steen V, Chou M, Shanmugam V, Mathias M, Kuru T, Morrissey R. Exercise-induced pulmonary arterial hypertension in patients with systemic sclerosis. Chest. 2008;134(1):146–51.
Stamm A, Saxer S, Lichtblau M, Hasler ED, Jordan S, Huber LC, et al. Exercise pulmonary haemodynamics predict outcome in patients with systemic sclerosis. Eur Respir J. 2016;48(6):1658–67.
Saggar R, Khanna D, Furst DE, Shapiro S, Maranian P, Belperio JA, et al. Exercise-induced pulmonary hypertension associated with systemic sclerosis: four distinct entities. Arthritis Rheum. 2010;62(12):3741–50.
Condliffe R, Kiely DG, Peacock AJ, Corris PA, Gibbs JS, Vrapi F, et al. Connective tissue disease-associated pulmonary arterial hypertension in the modern treatment era. Am J Respir Crit Care Med. 2009;179(2):151–7.
Barron A, Dhutia N, Mayet J, Hughes AD, Francis DP, Wensel R. Test-retest repeatability of cardiopulmonary exercise test variables in patients with cardiac or respiratory disease. Eur J Prev Cardiol. 2014;21(4):445–53.
Hansen JE, Sun XG, Yasunobu Y, Garafano RP, Gates G, Barst RJ, et al. Reproducibility of cardiopulmonary exercise measurements in patients with pulmonary arterial hypertension. Chest. 2004;126(3):816–24.
Michelakis ED, Gurtu V, Webster L, Barnes G, Watson G, Howard L, et al. Inhibition of pyruvate dehydrogenase kinase improves pulmonary arterial hypertension in genetically susceptible patients. Sci Transl Med. 2017;9(413):eaao4583.
Gomberg-Maitland M, Schilz R, Mediratta A, Addetia K, Coslet S, Thomeas V, et al. Phase I safety study of ranolazine in pulmonary arterial hypertension. Pulm Circ. 2015;5(4):691–700.
Maron BA, Cockrill BA, Waxman AB, Systrom DM. The invasive cardiopulmonary exercise test. Circulation. 2013;127(10):1157–64.
Segrera SA, Lawler L, Opotowsky AR, Systrom D, Waxman AB. Open label study of ambrisentan in patients with exercise pulmonary hypertension. Pulm Circ. 2017;7(2):531–8.
Saggar R, Khanna D, Shapiro S, Furst DE, Maranian P, Clements P, et al. Brief report: effect of ambrisentan treatment on exercise-induced pulmonary hypertension in systemic sclerosis: a prospective single-center, open-label pilot study. Arthritis Rheum. 2012;64(12):4072–7.
Wallace WD, Nouraie M, Chan SY, Risbano MG. Treatment of exercise pulmonary hypertension improves pulmonary vascular distensibility. Pulm Circ. 2018;8(3):2045894018787381.
Oliveira RKF, Faria-Urbina M, Maron BA, Santos M, Waxman AB, Systrom DM. Functional impact of exercise pulmonary hypertension in patients with borderline resting pulmonary arterial pressure. Pulm Circ. 2017;7(3):654–65.
Hinderhofer K, Fischer C, Pfarr N, Szamalek-Hoegel J, Lichtblau M, Nagel C, et al. Identification of a new intronic BMPR2-mutation and early diagnosis of heritable pulmonary arterial hypertension in a large family with mean clinical follow-up of 12 years. PLoS One. 2014;9(3):e91374.
Naeije R, Saggar R, Badesch D, Rajagopalan S, Gargani L, Rischard F, et al. Exercise-induced pulmonary hypertension: translating pathophysiological concepts into clinical practice. Chest. 2018;154(1):10–5.
Esfandiari S, Wright SP, Goodman JM, Sasson Z, Mak S. Pulmonary artery wedge pressure relative to exercise work rate in older men and women. Med Sci Sports Exerc. 2017;49(7):1297–304.
Eisman AS, Shah RV, Dhakal BP, Pappagianopoulos PP, Wooster L, Bailey C, et al. Pulmonary capillary wedge pressure patterns during exercise predict exercise capacity and incident heart failure. Circ Heart Fail. 2018;11(5):e004750.
Reeves JT, Linehan JH, Stenmark KR. Distensibility of the normal human lung circulation during exercise. Am J Physiol Lung Cell Mol Physiol. 2005;288(3):L419–25.
Lau EMT, Chemla D, Godinas L, Zhu K, Sitbon O, Savale L, et al. Loss of vascular distensibility during exercise is an early hemodynamic marker of pulmonary vascular disease. Chest. 2016;149(2):353–61.
Pavelescu A, Vanderpool R, Vachiery JL, Grunig E, Naeije R. Echocardiography of pulmonary vascular function in asymptomatic carriers of BMPR2 mutations. Eur Respir J. 2012;40(5):1287–9.
Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62(25 Suppl):D22–33.
Tello K, Dalmer A, Axmann J, Vanderpool R, Ghofrani HA, Naeije R, et al. Reserve of right ventricular-arterial coupling in the setting of chronic overload. Circ Heart Fail. 2019;12(1):e005512.
Spruijt OA, de Man FS, Groepenhoff H, Oosterveer F, Westerhof N, Vonk-Noordegraaf A, et al. The effects of exercise on right ventricular contractility and right ventricular-arterial coupling in pulmonary hypertension. Am J Respir Crit Care Med. 2015;191(9):1050–7.
Hsu S, Houston BA, Tampakakis E, Bacher AC, Rhodes PS, Mathai SC, et al. Right ventricular functional reserve in pulmonary arterial hypertension. Circulation. 2016;133(24):2413–22.
Grunig E, Peacock AJ. Imaging the heart in pulmonary hypertension: an update. Eur Respir Rev. 2015;24(138):653–64.
Bossone E, D’Andrea A, D'Alto M, Citro R, Argiento P, Ferrara F, et al. Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr. 2013;26(1):1–14.
Rengier F, Melzig C, Derlin T, Marra AM, Vogel-Claussen J. Advanced imaging in pulmonary hypertension: emerging techniques and applications. Int J Cardiovasc Imaging. 2019;35:1407–20.
Sachdev A, Villarraga HR, Frantz RP, McGoon MD, Hsiao JF, Maalouf JF, et al. Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest. 2011;139(6):1299–309.
Vitarelli A, Mangieri E, Terzano C, Gaudio C, Salsano F, Rosato E, et al. Three-dimensional echocardiography and 2D-3D speckle-tracking imaging in chronic pulmonary hypertension: diagnostic accuracy in detecting hemodynamic signs of right ventricular (RV) failure. J Am Heart Assoc. 2015;4(3):e001584.
Freed BH, Collins JD, Francois CJ, Barker AJ, Cuttica MJ, Chesler NC, et al. MR and CT imaging for the evaluation of pulmonary hypertension. JACC Cardiovasc Imaging. 2016;9(6):715–32.
Peacock AJ, Vonk Noordegraaf A. Cardiac magnetic resonance imaging in pulmonary arterial hypertension. Eur Respir Rev. 2013;22(130):526–34.
Dellegrottaglie S, Ostenfeld E, Sanz J, Scatteia A, Perrone-Filardi P, Bossone E. Imaging the right heart-pulmonary circulation unit: The role of MRI and computed tomography. Heart Fail Clin. 2018;14(3):377–91.
Ray JC, Burger C, Mergo P, Safford R, Blackshear J, Austin C, et al. Pulmonary arterial stiffness assessed by cardiovascular magnetic resonance imaging is a predictor of mild pulmonary arterial hypertension. Int J Cardiovasc Imaging. 2018;35(10):1881–92.
Schafer M, Myers C, Brown RD, Frid MG, Tan W, Hunter K, et al. Pulmonary arterial stiffness: toward a new paradigm in pulmonary arterial hypertension pathophysiology and assessment. Curr Hypertens Rep. 2016;18(1):4.
Reiter G, Reiter U, Kovacs G, Olschewski H, Fuchsjager M. Blood flow vortices along the main pulmonary artery measured with MR imaging for diagnosis of pulmonary hypertension. Radiology. 2015;275(1):71–9.
Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999;14(4):270–8.
Rahaghi FN, Vegas-Sanchez-Ferrero G, Minhas JK, Come CE, De La Bruere I, Wells JM, et al. Ventricular geometry from non-contrast non-ECG-gated CT scans: an imaging marker of cardiopulmonary disease in smokers. Acad Radiol. 2017;24(5):594–602.
Colin GC, Gerber BL, de Meester de Ravenstein C, Byl D, Dietz A, Kamga M, et al. Pulmonary hypertension due to left heart disease: diagnostic and prognostic value of CT in chronic systolic heart failure. Eur Radiol 2018, 28, 4643.
Currie BJ, Johns C, Chin M, Charalampopolous T, Elliot CA, Garg P, et al. CT derived left atrial size identifies left heart disease in suspected pulmonary hypertension: derivation and validation of predictive thresholds. Int J Cardiol. 2018;260:172–7.
Aviram G, Rozenbaum Z, Ziv-Baran T, Berliner S, Topilsky Y, Fleischmann D, et al. Identification of pulmonary hypertension caused by left-sided heart disease (World Health Organization Group 2) based on cardiac chamber volumes derived from chest CT imaging. Chest. 2017;152(4):792–9.
Rahaghi FN, Ross JC, Agarwal M, Gonzalez G, Come CE, Diaz AA, et al. Pulmonary vascular morphology as an imaging biomarker in chronic thromboembolic pulmonary hypertension. Pulm Circ. 2016;6(1):70–81.
Matsuoka S, Washko GR, Yamashiro T, Estepar RS, Diaz A, Silverman EK, et al. Pulmonary hypertension and computed tomography measurement of small pulmonary vessels in severe emphysema. Am J Respir Crit Care Med. 2010;181(3):218–25.
Helmberger M, Pienn M, Urschler M, Kullnig P, Stollberger R, Kovacs G, et al. Quantification of tortuosity and fractal dimension of the lung vessels in pulmonary hypertension patients. PLoS One. 2014;9(1):e87515.
Moledina S, de Bruyn A, Schievano S, Owens CM, Young C, Haworth SG, et al. Fractal branching quantifies vascular changes and predicts survival in pulmonary hypertension: a proof of principle study. Heart. 2011;97(15):1245–9.
Rahaghi FN, Winkler T, Kohli P, Nardelli P, Marti-Fuster B, Ross JC, et al. Quantification of the pulmonary vascular response to inhaled nitric oxide using noncontrast computed tomography imaging. Circ Cardiovasc Imaging. 2019;12(1):e008338.
Aviram G, Shmueli H, Adam SZ, Bendet A, Ziv-Baran T, Steinvil A, et al. Pulmonary hypertension: a nomogram based on CT pulmonary angiographic data for prediction in patients without pulmonary embolism. Radiology. 2015;277(1):236–46.
Koike H, Sueyoshi E, Sakamoto I, Uetani M, Nakata T, Maemura K. Comparative clinical and predictive value of lung perfusion blood volume CT, lung perfusion SPECT and catheter pulmonary angiography images in patients with chronic thromboembolic pulmonary hypertension before and after balloon pulmonary angioplasty. Eur Radiol. 2018;28(12):5091–9.
Marsboom G, Wietholt C, Haney CR, Toth PT, Ryan JJ, Morrow E, et al. Lung (1)(8)F-fluorodeoxyglucose positron emission tomography for diagnosis and monitoring of pulmonary arterial hypertension. Am J Respir Crit Care Med. 2012;185(6):670–9.
Zhao L, Ashek A, Wang L, Fang W, Dabral S, Dubois O, et al. Heterogeneity in lung (18)FDG uptake in pulmonary arterial hypertension: potential of dynamic (18)FDG positron emission tomography with kinetic analysis as a bridging biomarker for pulmonary vascular remodeling targeted treatments. Circulation. 2013;128(11):1214–24.
Ashek A, Spruijt OA, Harms HJ, Lammertsma AA, Cupitt J, Dubois O, et al. 3′-deoxy-3′-[18F]fluorothymidine positron emission tomography depicts heterogeneous proliferation pathology in idiopathic pulmonary arterial hypertension patient lung. Circ Cardiovasc Imaging. 2018;11(8):e007402.
Schoenfeld C, Cebotari S, Hinrichs J, Renne J, Kaireit T, Olsson KM, et al. MR imaging-derived regional pulmonary parenchymal perfusion and cardiac function for monitoring patients with chronic thromboembolic pulmonary hypertension before and after pulmonary endarterectomy. Radiology. 2016;279(3):925–34.
Hueper K, Parikh MA, Prince MR, Schoenfeld C, Liu C, Bluemke DA, et al. Quantitative and semiquantitative measures of regional pulmonary microvascular perfusion by magnetic resonance imaging and their relationships to global lung perfusion and lung diffusing capacity: the multiethnic study of atherosclerosis chronic obstructive pulmonary disease study. Investig Radiol. 2013;48(4):223–30.
Nallasamy N, Bullen J, Karim W, Heresi GA, Renapurkar RD. Evaluation of vascular parameters in patients with pulmonary thromboembolic disease using dual-energy computed tomography. J Thorac Imaging. 2019;4(6):367–72.
Renapurkar RD, Bolen MA, Shrikanthan S, Bullen J, Karim W, Primak A, et al. Comparative assessment of qualitative and quantitative perfusion with dual-energy CT and planar and SPECT-CT V/Q scanning in patients with chronic thromboembolic pulmonary hypertension. Cardiovasc Diagn Ther. 2018;8(4):414–22.
Ameli-Renani S, Ramsay L, Bacon JL, Rahman F, Nair A, Smith V, et al. Dual-energy computed tomography in the assessment of vascular and parenchymal enhancement in suspected pulmonary hypertension. J Thorac Imaging. 2014;29(2):98–106.
Dresdale DT, Michtom RJ, Schultz M. Recent studies in primary pulmonary hypertension, including pharmacodynamic observations on pulmonary vascular resistance. Bull N Y Acad Med. 1954;30(3):195–207.
Deng Z, Morse JH, Slager SL, Cuervo N, Moore KJ, Venetos G, et al. Familial primary pulmonary hypertension (gene PPH1) is caused by mutations in the bone morphogenetic protein receptor-II gene. Am J Hum Genet. 2000;67(3):737–44.
International PPHC, Lane KB, Machado RD, Pauciulo MW, Thomson JR, Phillips JA 3rd, et al. Heterozygous germline mutations in BMPR2, encoding a TGF-beta receptor, cause familial primary pulmonary hypertension. Nat Genet. 2000;26(1):81–4.
Thomson JR, Machado RD, Pauciulo MW, Morgan NV, Humbert M, Elliott GC, et al. Sporadic primary pulmonary hypertension is associated with germline mutations of the gene encoding BMPR-II, a receptor member of the TGF-beta family. J Med Genet. 2000;37(10):741–5.
Garcia-Rivas G, Jerjes-Sanchez C, Rodriguez D, Garcia-Pelaez J, Trevino V. A systematic review of genetic mutations in pulmonary arterial hypertension. BMC Med Genet. 2017;18(1):82.
Aldred MA, Comhair SA, Varella-Garcia M, Asosingh K, Xu W, Noon GP, et al. Somatic chromosome abnormalities in the lungs of patients with pulmonary arterial hypertension. Am J Respir Crit Care Med. 2010;182(9):1153–60.
Rosenzweig EB, Morse JH, Knowles JA, Chada KK, Khan AM, Roberts KE, et al. Clinical implications of determining BMPR2 mutation status in a large cohort of children and adults with pulmonary arterial hypertension. J Heart Lung Transplant. 2008;27(6):668–74.
Evans JD, Girerd B, Montani D, Wang XJ, Galie N, Austin ED, et al. BMPR2 mutations and survival in pulmonary arterial hypertension: an individual participant data meta-analysis. Lancet Respir Med. 2016;4(2):129–37.
Girerd B, Montani D, Coulet F, Sztrymf B, Yaici A, Jais X, et al. Clinical outcomes of pulmonary arterial hypertension in patients carrying an ACVRL1 (ALK1) mutation. Am J Respir Crit Care Med. 2010;181(8):851–61.
Galie N, Barbera JA, Frost AE, Ghofrani HA, Hoeper MM, McLaughlin VV, et al. Initial use of ambrisentan plus tadalafil in pulmonary arterial hypertension. N Engl J Med. 2015;373(9):834–44.
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation. 2010;122(2):156–63.
Galie N, Rubin L, Hoeper M, Jansa P, Al-Hiti H, Meyer G, et al. Treatment of patients with mildly symptomatic pulmonary arterial hypertension with bosentan (EARLY study): a double-blind, randomised controlled trial. Lancet. 2008;371(9630):2093–100.
Spiekerkoetter E, Tian X, Cai J, Hopper RK, Sudheendra D, Li CG, et al. FK506 activates BMPR2, rescues endothelial dysfunction, and reverses pulmonary hypertension. J Clin Invest. 2013;123(8):3600–13.
Spiekerkoetter E, Sung YK, Sudheendra D, Bill M, Aldred MA, van de Veerdonk MC, et al. Low-dose FK506 (tacrolimus) in end-stage pulmonary arterial hypertension. Am J Respir Crit Care Med. 2015;192(2):254–7.
Spiekerkoetter E, Sung YK, Sudheendra D, Scott V, Del Rosario P, Bill M, et al. Randomised placebo-controlled safety and tolerability trial of FK506 (tacrolimus) for pulmonary arterial hypertension. Eur Respir J. 2017;50(3):1602449.
Montani D, Jais X, Price LC, Achouh L, Degano B, Mercier O, et al. Cautious epoprostenol therapy is a safe bridge to lung transplantation in pulmonary veno-occlusive disease. Eur Respir J. 2009;34(6):1348–56.
Rhodes CJ, Batai K, Bleda M, Haimel M, Southgate L, Germain M, et al. Genetic determinants of risk in pulmonary arterial hypertension: international genome-wide association studies and meta-analysis. Lancet Respir Med. 2019;7:227–38.
Hemnes AR, Zhao M, West J, Newman JH, Rich S, Archer SL, et al. Critical genomic networks and vasoreactive variants in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med. 2016;194(4):464–75.
Benza RL, Gomberg-Maitland M, Demarco T, Frost AE, Torbicki A, Langleben D, et al. Endothelin-1 pathway polymorphisms and outcomes in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2015;192(11):1345–54.
Rhodes CJ, Wharton J, Ghataorhe P, Watson G, Girerd B, Howard LS, et al. Plasma proteome analysis in patients with pulmonary arterial hypertension: an observational cohort study. Lancet Respir Med. 2017;5(9):717–26.
Zhang X, Hou HT, Wang J, Liu XC, Yang Q, He GW. Plasma proteomic study in pulmonary arterial hypertension associated with congenital heart diseases. Sci Rep. 2016;6:36541.
Rhodes CJ, Ghataorhe P, Wharton J, Rue-Albrecht KC, Hadinnapola C, Watson G, et al. Plasma metabolomics implicate modified transfer RNAs and altered bioenergetics in the outcome of pulmonary arterial hypertension. Circulation. 2017;135:460–75.
Hemnes AR, Beck GJ, Newman JH, Abidov A, Aldred MA, Barnard J, et al. PVDOMICS: a multi-center study to improve understanding of pulmonary vascular disease through phenomics. Circ Res. 2017;121(10):1136–9.
Herve P, Lau EM, Sitbon O, Savale L, Montani D, Godinas L, Lador F, Jaïs X, Parent F, Günther S, Humbert M, Simonneau G, Chemla D. Criteria for diagnosis of exercise pulmonary hypertension. Eur Respir J. 2015;46(3):728–37. https://doi.org/10.1183/09031936.00021915.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Singh, I., Oldham, W.M., Rahaghi, F.N. (2020). Precision Medicine in Pulmonary Hypertension. In: Gomez, J., Himes, B., Kaminski, N. (eds) Precision in Pulmonary, Critical Care, and Sleep Medicine. Respiratory Medicine. Humana, Cham. https://doi.org/10.1007/978-3-030-31507-8_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-31507-8_16
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-31506-1
Online ISBN: 978-3-030-31507-8
eBook Packages: MedicineMedicine (R0)